Abstract
Purpose
Utility of pre-operative MRI for patients undergoing scoliosis correction has expanded to include an MRI classification for identifying patients at increased risk of experiencing intra-operative neuromonitoring (IONM) alerts based on the shape of the spinal cord and circumferential presence of CSF at the apex of the thoracic curve. In the present study, the authors explore the utility of this new MRI classification and multiple X-ray radiographic parameters in identifying the AIS sub-population at high risk of IONM alerts.
Methods
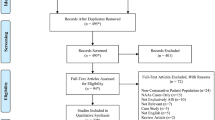
AIS patients < 18 years old who underwent posterior spinal fusion between 2018 and 2022 at a single institution. Imaging reviewed to determine main thoracic (MT) and thoraco-lumbar (TL) Cobb angles, major thoracic Apical Vertebral Translation (AVT) and lumbar/thoraco-lumbar AVT (TL AVT), thoracic kyphosis (TK), coronal main thoracic Deformity Angular Ratio (cDAR), sagittal DAR (sDAR), and MRI to determine the spinal cord type (1, 2, or 3).
Results
A total of 155 AIS patients who met the inclusion criteria between 2018 and 2022 were included. There was a trend to have an increased incidence of Type 3 spinal cord shape both with increase in the MT Cobb angle and MT AVT. There was also a shift toward more IONM alerts in patients with Type 3 (19.5%) spinal cords, AVT ≥ 5 cm (18.9%), and Cobb angle ≥ 650 (28.2%).
Conclusion
Higher magnitude of thoracic Cobb angle and AVT are associated with higher likelihood of type 3 spinal cord at the apex in MRI. Patients with Type 3 spinal cord, Cobb angle ≥ 650, AVT > 5 cm, and cDAR > 10 have higher likelihood to have IONM alerts. Patient with a Type 3 spinal cord and a Cobb angle ≥ 650 (50.0%), cDAR > 10 (43.7%), and AVT > 5 cm (35.2%) have the highest risk of having IONM alerts.


Similar content being viewed by others
Data availability
Data is available upon request from the corresponding author.
References
Diab M et al (2011) Use and outcome of MRI in the surgical treatment of adolescent idiopathic scoliosis. Spine 36(8):667–671
Davids JR, Chamberlin E, Blackhurst DW (2004) Indications for magnetic resonance imaging in presumed adolescent idiopathic scoliosis. JBJS 86(10):2187–2195
Do T, Fras C, Burke S et al (2001) Clinical value of routine preoperative magnetic resonance imaging in adolescent idiopathic scoliosis: a prospective study of three hundred and twenty-seven patients. JBJS 83(4):577
Maiocco B, Deeney VF, Coulon R et al (1997) Adolescent idiopathic scoliosis and the presence of spinal cord abnormalities: preoperative magnetic resonance imaging analysis. Spine 22(21):2537–2541
Shen WJ, McDowell GS, Burke SW et al (1996) Routine preoperative MRI and SEP studies in adolescent idiopathic scoliosis. J Pediatric Orthopaed 16(3):350–353
Sielatycki JA, Cerpa M, Baum G et al (2020) A novel MRI-based classification of spinal cord shape and CSF presence at the curve apex to assess risk of intraoperative neuromonitoring data loss with thoracic spinal deformity correction. Spine Deform 8(4):655–661. https://doi.org/10.1007/s43390-020-00101-9
Mathew SE, Milbrandt TA, Shaughnessy WJ et al (2021) Is the axial spinal cord classification predictive of intraoperative neurological alert for pediatric scoliosis patients? An independent retrospective validation study. Spine Deformity 9:395–401
Nagarajan L, Ghosh S, Dillon D et al (2019) Intraoperative neurophysiology monitoring in scoliosis surgery in children. Clin Neurophysiol Pract 25(4):11–17. https://doi.org/10.1016/j.cnp.2018.12.002.PMID:30828671;PMCID:PMC6383123
Pastorelli F, Di Silvestre M, Plasmati R et al (2011) The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J. https://doi.org/10.1007/s00586-011-1756-z
Shen WJ, McDowell GS, Burke SW et al (1996) Routine preoperative MRI and SEP studies in adolescent idiopathic scoliosis. J Pediatr Orthop 16(3):350–353. https://doi.org/10.1097/00004694-199605000-00011
Richards BS, Sucato DJ, Johnston CE et al (2010) Right thoracic curves in presumed adolescent idiopathic scoliosis: which clinical and radiographic findings correlate with a preoperative abnormal magnetic resonance image? Spine 35(20):1855–1860. https://doi.org/10.1097/BRS.0b013e3181d4f532
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7(1):3–9. https://doi.org/10.1007/s11832-012-0457-4
Wang XB, Lenke LG, Thuet E et al (2016) Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine 41(18):1447–1455
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Contributions
SR, SK, JS, AD, TE, and SG: data acquisition, manuscript preparation, approved the version to be published, and agreed to be accountable for all aspects of work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Thomas J. Errico is a speaker and consultant to Stryker. He also has royalties from Stryker. Dr. Stephen George is a consultant to Globus Medical. Dr. Subaraman Ramchandran, Dr. Sassan Keshavarzi, Dr. Alyssa Dobyns, and Jeffrey Spardy declare that they have no financial or non-financial interests to disclose.
Ethical approval
The manuscript submitted does not contain information about medical device(s).
IRB
The study was conducted under the IRB heading “Secondary analysis of data to study the clinical and radiographic outcomes in pediatric patients undergoing surgery for spinal deformities”. Protocol number: 2019064RI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keshavarzi, S., Ramchandran, S., Spardy, J. et al. Utilization of pre-operative MRI to identify AIS patients at highest risk of intra-operative neuromonitoring alert. Spine Deform 11, 1419–1426 (2023). https://doi.org/10.1007/s43390-023-00710-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00710-0