Abstract
Purpose
We sought to determine whether the axial spinal cord classification by Sielatycki et al. would be associated with increased intraoperative neuromonitoring (IONM) alerts for pediatric scoliosis patients undergoing posterior spinal fusion (PSF) surgery.
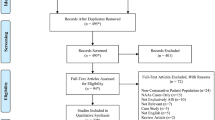
Methods
Children less than age 19 with scoliosis undergoing PSF were retrospectively reviewed. Axial-T2 MRI of the thoracic apex was reviewed for spinal cord/CSF architecture as described by Sielatycki et al.: Type 1—circular cord with visible CSF, Type 2—circular cord but no visible CSF at apical concavity, and Type 3—cord deformed with no intervening CSF. Intraoperative neuromonitoring reports, operative records and preoperative radiographs were reviewed.
Results
90 patients met the inclusion criteria. Rate of neurologic events was Type 1: 2% (1/41 patients), Type 2: 14.3% (4/28), Type 3: 57.1% (12/21) (Type 1 vs 2 p = 0.06; Type 1 vs 3 p < 0.0001; Type 2 vs 3 p = 0.0017). Three patients with a Type 3 cord awoke with significant deficits. In comparison to Type 1 cords, Type 3 and Type 2 spinal cords were associated with increased coronal and total deformity angular ratios (Type 1 vs 3 p = 0.035 and 0.0054 respectively; Type 1 vs 2 p = 0.042 and 0.03 respectively). There was no difference in gender, diagnosis category, age at surgery, Cobb angle or kyphosis between the three groups.
Conclusion
The axial spinal cord classification correlated with IONM alerts and greater severity of spinal deformity in pediatric scoliosis patients.
Level of evidence
IV, retrospective cohort study.


Similar content being viewed by others
References
Fu KM, Smith JS, Polly DW, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp DR, Shaffrey CI, Scoliosis Research Society Morbidity and Mortality Committee (2011) Scoliosis Research Society Morbidity and Mortality Committee Morbidity and mortality associated with spinal surgery in children: a review of the Scoliosis Research Society morbidity and mortality database. J NeurosurgPediatr. 7(1):37–41. https://doi.org/10.3171/2010.10.PEDS10212 (PubMed PMID: 21194285)
Reames DL, Smith JS, Fu KM, Polly DW Jr, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp RD Jr, Heary R, Shaffrey CI (2011) Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 36(18):1484–1491. https://doi.org/10.1097/BRS.0b013e3181f3a326
Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z (2008) Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976). 33(5):519–526. https://doi.org/10.1097/BRS.0b013e3181657d93
Samdani AF, Bennett JT, Ames RJ, Asghar JK, Orlando G, Pahys JM, Yaszay B, Miyanji F, Lonner BS, Lehman RA Jr, Newton PO, Cahill PJ, Betz RR (2016) Reversible intraoperative neurophysiologic monitoring alerts in patients undergoing arthrodesis for adolescent idiopathic scoliosis: what are the outcomes of surgery? J Bone JtSurg Am 98(17):1478–1483. https://doi.org/10.2106/JBJS.15.01379
Vitale MG, Moore DW, Matsumoto H, Emerson RG, Booker WA, Gomez JA, Gallo EJ, Hyman JE, Roye DP Jr (2010) Risk factors for spinal cord injury during surgery for spinal deformity. J Bone JtSurg Am 92(1):64–71. https://doi.org/10.2106/JBJS.H.01839
Wang XB, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M (2016) Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine (Phila Pa 1976). 41(18):1447–1455. https://doi.org/10.1097/BRS.0000000000001547
Lewis ND, Keshen SG, Lenke LG, Zywiel MG, Skaggs DL, Dear TE, Strantzas S, Lewis SJ (2015) The deformity angular ratio: does it correlate with high-risk cases for potential spinal cord monitoring alerts in pediatric 3-column thoracic spinal deformity corrective surgery? Spine (Phila Pa 1976). 40(15):E879–E885. https://doi.org/10.1097/BRS.0000000000000984
Kim SM, Kim SH, Seo DW, Lee KW (2013) Intraoperative neurophysiologic monitoring: basic principles and recent update. J Korean Med Sci 28(9):1261–1269. https://doi.org/10.3346/jkms.2013.28.9.1261 (Epub 2013 Aug 28)
Sielatycki JA, Cerpa M, Baum G, Pham M, Thuet E, Lehman RA, Lenke LG (2020) A novel MRI-based classification of spinal cord shape and CSF presence at the curve apex to assess risk of intraoperative neuromonitoring data loss with thoracic spinal deformity correction. Spine Deform 8(4):655–661
Feng B, Qiu G, Shen J, Zhang J, Tian Y, Li S, Zhao H, Zhao Y (2012) Impact of multimodal intraoperative monitoring during surgery for spine deformity and potential risk factors for neurological monitoring changes. J Spinal Disord Tech 25(4):E108–E114. https://doi.org/10.1097/BSD.0b013e31824d2a2f
Nash CL Jr, Lorig RA, Schatzinger LA, Brown RH (1977) Spinal cord monitoring during operative treatment of the spine. ClinOrthopRelat Res 126:100–105
Devlin VJ, Daniel Schwartz DM (2007) Intraoperative neurophysiologic monitoring during spinal surgery. J Am AcadOrthopSurg 15(9):549–560
Kundnani VK, Zhu L, Tak H, Wong H (2010) Multimodal intraoperative neuromonitoring in corrective surgery for adolescent idiopathic scoliosis: evaluation of 354 consecutive cases. Indian J Orthop 44(1):64–72. https://doi.org/10.4103/0019-5413.58608
Vitale MG, Skaggs DL, Pace GI et al (2014) Best practices in intraoperative neuromonitoring in spine deformity surgery: development of an intraoperative checklist to optimize response. Spine Deform 2(5):333–339. https://doi.org/10.1016/j.jspd.2014.05.003
Yang J, Skaggs DL, Chan P et al (2018) Raising mean arterial pressure alone restores 20% of intraoperative neuromonitoring losses. Spine (Phila Pa 1976) 43(13):890–894. https://doi.org/10.1097/BRS.0000000000002461
Schroeder GD, Hjelm N, Vaccaro AR, Weinstein MS, Kepler CK (2016) The effect of increased T2 signal intensity in the spinal cord on the injury severity and early neurological recovery in patients with central cord syndrome. J Neurosurg Spine 24(5):792–796. https://doi.org/10.3171/2015.9.SPINE15661 (Epub 2016 Jan 8)
Morio Y, Yamamoto K, Kuranobu K, Murata M, Tuda K (1994) Does increased signal intensity of the spinal cord on MR images due to cervical myelopathy predict prognosis? Arch Orthop Trauma Surg 113(5):254–259
Funding
There was no funding received for this study.
Author information
Authors and Affiliations
Contributions
SEM, TAM, WJS, AAS and ANL: substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data, drafting the work or critically revising it for important intellectual content, final approval of the version to be published, responsible for content and accuracy of the entire manuscript and the order and inclusion should be decided by consensus among the authors and acknowledged in writing.
Corresponding author
Ethics declarations
Conflict of interest
Outside of the study, Dr. Milbrandt reports consulting activities with Orthopediatrics, Medtronic, Zimmer and stock ownership in Viking Scientific. Dr. Larson reports consulting activities with Orthopediatrics, Medtronic, Zimmer, and Globus. Drs. Mathew, Stans, and Shaughnessy have no conflicts to report.
Ethical approval
Institutional review board approval was obtained for all aspects of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mathew, S.E., Milbrandt, T.A., Shaughnessy, W.J. et al. Is the axial spinal cord classification predictive of intraoperative neurologic alert for pediatric scoliosis patients? An independent retrospective validation study. Spine Deform 9, 395–401 (2021). https://doi.org/10.1007/s43390-020-00241-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00241-y