Abstract
Purpose
The natural history of adolescent idiopathic scoliosis (AIS) has been well documented, but the impact of age at the time of surgical correction is relatively understudied. In this study, we matched patients undergoing surgical correction of adult idiopathic scoliosis (AdIS) with a cohort of AIS patients to compare: (1) coronal and sagittal radiographic correction, (2) operative variables, and (3) postoperative complications.
Methods
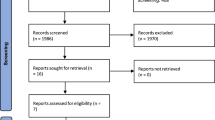
A single-institution scoliosis registry was queried for patients undergoing idiopathic scoliosis surgery from 2000–2017. Inclusion criteria: patients with idiopathic scoliosis, no previous spine surgery, and 2-year follow-up. AdIS patients were matched 1:2 with AIS patients based on Lenke classification and curve characteristics. Independent sample t-test and Chi-square test was used to analyze the data.
Results
31 adults underwent surgical correction of idiopathic scoliosis and were matched with 62 adolescents. Mean age of adults was 26.2 ± 11.05, mean BMI was 25.6 ± 6.0, and 22 (71.0%) were female. Mean age of adolescents was 14.2 ± 1.8, mean BMI was 22.7 ± 5.7, and 41(66.7%) were female. AdIS had significantly less postoperative major Cobb correction (63.9% vs 71.3%, p = 0.006) and final major Cobb correction (60.6% vs 67.9%, p = 0.025). AdIS also had significantly greater postoperative T1PA (11.8 vs 5.8, p = 0.002). AdIS had longer operative times (p = 0.003), higher amounts of pRBCs transfused (p = 0.005), longer LOS (p = 0.016), more ICU requirement (p = 0.013), higher overall complications (p < 0.001), higher rate of pseudarthrosis (p = 0.026), and more neurologic complications (p = 0.013).
Conclusion
Adult patients undergoing surgical correction of idiopathic scoliosis had significantly worse postoperative coronal and sagittal alignment when compared with adolescent patients. Adult patients also had higher rates of complications, longer operative times, and longer hospital stays.
Level of evidence: III.

Similar content being viewed by others
References
Dunn J, Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Lin JS (2018) Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US preventive services task force. JAMA 319(2):173–187. https://doi.org/10.1001/jama.2017.11669
Weinstein SL (2019) The natural history of adolescent idiopathic scoliosis. J Pediatr Orthop 39(6, Suppl 1):S44–S46. https://doi.org/10.1097/BPO.0000000000001350
Agabegi SS, Kazemi N, Sturm PF, Mehlman CT (2015) Natural history of adolescent idiopathic scoliosis in skeletally mature patients: a critical review. J Am Acad Orthop Surg 23(12):714–723. https://doi.org/10.5435/JAAOS-D-14-00037
Weiss HR (2008) Adolescent idiopathic scoliosis (AIS)—an indication for surgery? A systematic review of the literature. Disabil Rehabil 30(10):799–807. https://doi.org/10.1080/09638280801889717
Negrini S (2008) Approach to scoliosis changed due to causes other than evidence: patients call for conservative (rehabilitation) experts to join in team orthopedic surgeons. Disabil Rehabil 30(10):731–741. https://doi.org/10.1080/09638280801889485
Westrick ER, Ward WT (2011) Adolescent idiopathic scoliosis: 5-year to 20-year evidence-based surgical results. J Pediatr Orthop 31(1 Suppl):S61–S68. https://doi.org/10.1097/BPO.0b013e3181fd87d5
Diarbakerli E, Grauers A, Danielsson A, Gerdhem P (2017) Adults with idiopathic scoliosis diagnosed at youth experience similar physical activity and fracture rate as controls. Spine (Phila Pa 1976) 42(7):E404–E410. https://doi.org/10.1097/BRS.0000000000001841
Verla T, Adogwa O, Toche U et al (2016) Impact of increasing age on outcomes of spinal fusion in adult idiopathic scoliosis. World Neurosurg 87:591–597. https://doi.org/10.1016/j.wneu.2015.10.061
Kim YJ, Bridwell KH, Lenke LG, Rinella AS, Edwards C 2nd (2005) Pseudarthrosis in primary fusions for adult idiopathic scoliosis: incidence, risk factors, and outcome analysis [published correction appears in Spine. 2005 Apr 15;30(8):994. Edward, Charles 2nd [corrected to Edwards, Charles 2nd]]. Spine (Phila Pa 1976) 30(4):468–474. https://doi.org/10.1097/01.brs.0000153392.74639.ea
Lonner BS, Ren Y, Bess S et al (2019) Surgery for the adolescent idiopathic scoliosis patients after skeletal maturity: early versus late surgery. Spine Deform 7(1):84–92. https://doi.org/10.1016/j.jspd.2018.05.012
Chaudry Z, Anderson JT (2017) Curve flexibility in cerebral palsy-related neuromuscular scoliosis: does the intraoperative prone radiograph reveal more flexibility than preoperative radiographs? Scoliosis 12:15. https://doi.org/10.1186/s13013-017-0122-2
Lavelle W, Kurra S, Hu X, Lieberman I (2020) Clinical outcomes of idiopathic scoliosis surgery: is there a difference between young adult patients and adolescent patients? Cureus 12(5):e8118. https://doi.org/10.7759/cureus.8118 (Published 2020 May 14)
Zhu F, Bao H, Yan P et al (2017) Comparison of surgical outcome of adolescent idiopathic scoliosis and young adult idiopathic scoliosis: a match-pair analysis of 160 patients. Spine (Phila Pa 1976) 42(19):E1133–E1139. https://doi.org/10.1097/BRS.0000000000002106
Ohrt-Nissen S, Bari T, Dahl B, Gehrchen M (2018) Sagittal alignment after surgical treatment of adolescent idiopathic scoliosis-application of the Roussouly classification. Spine Deform 6(5):537–544
Pizones J, Martin MB, Perez-Grueso FJS et al (2019) Impact of adult scoliosis on Roussouly sagittal shape classification. Spine (Phila Pa 1976) 44(4):270–279
de Jonge T, Dubousset JF, Illés T (2002) Sagittal plane correction in idiopathic scoliosis. Spine (Phila Pa 1976) 27(7):754–760
Ritzman TF, Floccari LV (2022) The sagittal plane in spinal fusion for adolescent idiopathic scoliosis. J Am Acad Orthop Surg 30(14):e957–e967
Lonner BS, Ren Y, Newton PO et al (2017) Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis—the pelvis and other considerations. Spine Deform 5(3):181–188
Lowe TG, Lenke L, Betz R et al (2006) Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention. Spine (Phila Pa 1976) 31(3):299–302
Lee GA, Betz RR, Clements III DH et al (1999) Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 24:795–799
Kim YJ, Lenke LG, Bridwell KH et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32(24):2731–2738
Alzakri A, Vergari C, Van den Abbeele M, Gille O, Skalli W, Obeid I (2019) Global sagittal alignment and proximal junctional kyphosis in adolescent idiopathic scoliosis. Spine Deform 7(2):236–244
Roussouly P, Labelle H, Rouissi J, Bodin A (2013) Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J 22(Suppl 2):S203–S215
Yeung KH, Man GCW, Skalli W et al (2021) Global sagittal alignment after surgery of right thoracic idiopathic scoliosis in adolescents and adults with and without thoracic hypokyphosis. Sci Rep 11(1):6294
Nolte MT, Louie PK, Harada GK et al (2020) Sagittal balance in adult idiopathic scoliosis. Clin Spine Surg 33(2):53–61
Garg B, Mehta N, Gupta A et al (2021) Cervical sagittal alignment in Lenke 1 adolescent idiopathic scoliosis and assessment of its alteration with surgery: a retrospective, multi-centric study. Spine Deform 9(6):1559–1568
Lazennec JY, Ramaré S, Arafati N et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Goldstein JA, Macenski MJ, Griffith SL, McAfee PC (2001) Lumbar sagittal alignment after fusion with a threaded interbody cage. Spine (Phila Pa 1976) 26(10):1137–1142
Tribus CB, Belanger TA, Zdeblick TA (1999) The effect of operative position and short-segment fusion on maintenance of sagittal alignment of the lumbar spine. Spine (Phila Pa 1976) 24(1):58–61
Johnson RD, Valore A, Villaminar A, Comisso M, Balsano M (2013) Sagittal balance and pelvic parameters—a paradigm shift in spinal surgery. J Clin Neurosci 20(2):191–196
Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20(Suppl 5):699–703
Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON (2015) Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 76(Suppl 1):S42–S56
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 19(14):1611–1618
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10(4):314–319
Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M (2002) Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 27(1):59–64
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467
Qiao J, Zhu F, Xu L et al (2014) T1 pelvic angle: a new predictor for postoperative sagittal balance and clinical outcomes in adult scoliosis. Spine (Phila Pa 1976) 39(25):2103–2107
Protopsaltis T, Schwab F, Bronsard N et al (2014) TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 96(19):1631–1640
Ryan DJ, Protopsaltis TS, Ames CP et al (2014) T1 pelvic angle (TPA) effectively evaluates sagittal deformity and assesses radiographical surgical outcomes longitudinally. Spine (Phila Pa 1976) 39(15):1203–1210
Rinella A, Bridwell K, Kim Y, et al. Late complications of adult idiopathic scoliosis primary fusions to L4 and above: the effect of age and distal fusion level. Spine (Phila Pa 1976). 2004;29(3):318–325.
Hariharan AR, Shah SA, Petfield J et al (2022) Complications following surgical treatment of adolescent idiopathic scoliosis: a 10-year prospective follow-up study. Spine Deform 10(5):1097–1105
Glassman SD, Anagnost SC, Parker A et al (2000) Effect of cigarette smoking and smoking cessation on spinal fusion. Spine (Phila Pa 1976) 25(20):2608–2615. https://doi.org/10.1097/00007632-200010150-00011
Brown CW, Orme TJ, Richardson HD (1986) The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine (Phila Pa 1976) 11:942–943. https://doi.org/10.1097/00007632-198611000-00015
Carpenter CT, Dietz JW, Leung KYK et al (1996) Repair of a pseudoarthrosis of the lumbar spine: a functional outcome study. J Bone Joint Surg Am 78(5):712–720. https://doi.org/10.2106/00004623-199605000-00011
Kwiatkowski TC, Hanley EH, Ramp WK (1996) Cigarette smoking and its orthopaedic consequences. Am J Orthop 25:590–597
Funding
This study did not receive funding from any institution or grant.
Author information
Authors and Affiliations
Contributions
MELB: Data curation, drafting the paper, final approval of the version to be published, contributed effort to the study. HC: Data curation, formal analysis, final approval of the version to be published, contributed effort to the study. WHW: Data curation, interpretation of the analysis, final approval of the version to be published, contributed effort to the study. JV: Data curation, interpretation of the analysis, final approval of the version to be published, contributed effort to the study. SJ: Data curation, drafting the paper, final approval of the version to be published, contributed effort to the study. SGR: Design and execution of the formal analysis, final approval of the version to be published, contributed effort to the study. AJC: Data curation, revisions, final approval of the version to be published, contributed effort to the study. AMA: Conducted review and editing, final approval of the version to be published, contributed effort to the study. CRL: Design and execution of the formal analysis, final approval of the version to be published, contributed effort to the study. JEM: Design and execution of the formal analysis, final approval of the version to be published, contributed effort to the study. GAM: Design and execution of the formal analysis, final approval of the version to be published, contributed effort to the study. SLZ: Designed research, data acquisition, conceptualization, interpretation of the analysis, final approval of the version to be published, contributed effort to the study. BFS: Conducted review and editing, final approval of the version to be published, contributed effort to the study.
Corresponding author
Ethics declarations
Conflict of interest
BFS—research support: Stryker Spine. All the authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. The authors have no personal or institutional financial interest in drugs, materials, or devices described in their submissions.
Ethical approval
This study was approved by the IRB committee at Vanderbilt University Medical Center (IRB# 211700). We certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
LaBarge, M.E., Chanbour, H., Waddell, W.H. et al. Clinical and radiographic outcomes following correction of idiopathic scoliosis in adolescence vs young adulthood. Spine Deform 11, 1443–1451 (2023). https://doi.org/10.1007/s43390-023-00708-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00708-8