Abstract
Purpose
Children with neuromuscular scoliosis (NMS) undergoing posterior spinal fusion (PSF) have historically been managed post-operatively in the pediatric intensive care unit (PICU) due to institutional tendencies. This study sought to define risk factors for PICU admission when using an enhanced recovery after surgery (ERAS) pathway.
Methods
A retrospective review of children with non-ambulatory (GMFCS 4 or 5) cerebral palsy undergoing PSF for NMS performed at two institutions by 5 surgeons. Both institutions have a pre-existing ERAS pathway for NMS patients consisting of post-surgical transfer to the hospital floor with early reinstitution of feeding and mobilization. PICU admission is used at the discretion of the surgeon and anesthesiologist rather than by institutional decree. Patient and surgical factors were assessed for risk factors of PICU admission.
Results
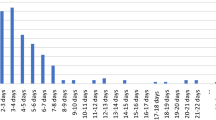
A total of 103 children were included (84% GMFCS 5, mean 14.52 years (± 3.4 years)). Forty children (38.8%) required postoperative PICU admission. PICU admission was associated with seizure disorder (P = 0.09), pre-existing feeding tube (P = 0.003), tracheostomy (P = 0.03), and modified GMFCS-5 subclassification (P = 0.003). Independent predictors of PICU admission include pre-existing feeding (Odd’s ratio = 2.9, P = 0.02) and length of surgery (Odd’s ratio = 2.6, P < 0.001), with surgery lasting ≥ 5.0 h having an 82.5% sensitivity and 63.5% specificity (AUC 0.8, P < 0.001) for post-operative PICU admission.
Conclusion
The majority of children with non-ambulatory cerebral palsy can be successfully managed on the hospital floor following PSF. The extent of central neuromotor impairment is significantly associated with PICU admission along with surgery lasting longer than 5 h.


Similar content being viewed by others
Data availability
Data is maintained by the authors and available pending institutional review and approval.
References
Persson-Bunke M, Hägglund G, Lauge-Pedersen H et al (2012) Scoliosis in a total population of children with cerebral palsy. Spine (Phila Pa 1976) 37(12):708–13
Willoughby KL, Ang SG, Thomason P et al (2022) Epidemiology of scoliosis in cerebral palsy: a population-based study at skeletal maturity. J Paediatr Child Health 58(2):295–301
Shaw KA, Reifsnyder J, Hire JM et al (2019) The effect of spinal arthrodesis on health-related quality of life for patients with nonambulatory cerebral palsy: a critical analysis review. JBJS Rev 7(12):e1
Miller DJ, Flynn JJM, Pasha S et al (2020) Improving health-related quality of life for patients with nonambulatory cerebral palsy: who stands to gain from scoliosis surgery? J Pediatr Orthop 40(3):e186–e192
Miyanji F, Nasto LA, Sponseller PD et al (2018) Assessing the risk-benefit ratio of scoliosis surgery in cerebral palsy: surgery is worth it. J Bone Jt Surg Am 100(7):556–563
Fletcher ND, Bellaire LL, Dilbone ES et al (2020) Variability in length of stay following neuromuscular spinal fusion. Spine Deform 8(4):725–732
Brooks JT, Yaszay B, Bartley CE et al (2019) Do all patients with cerebral palsy require postoperative intensive care admission after spinal fusion? Spine Deform 7(1):112–117
Bellaire LL, Bruce RW Jr, Ward LA et al (2019) Use of an accelerated discharge pathway in patients with severe cerebral palsy undergoing posterior spinal fusion for neuromuscular scoliosis. Spine Deform 7(5):804–811
Jain A, Sponseller PD, Shah SA et al (2016) Subclassification of GMFCS level-5 cerebral palsy as a predictor of complications and health-related quality of life after spinal arthrodesis. J Bone Jt Surg Am 98(21):1821–1828
Fletcher ND, Shourbaji N, Mitchell PM et al (2014) Clinical and economic implications of early discharge following posterior spinal fusion for adolescent idiopathic scoliosis. J Child Orthop 8(3):257–263
Shan LQ, Skaggs DL, Lee C et al (2013) Intensive care unit versus hospital floor: a comparative study of postoperative management of patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am 95(7):e40
Himmelmann K, Beckung E, Hagberg G et al (2006) Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol 48(6):417–423
Sarwahi V, Atlas A, Galina J et al (2022) Ambulatory neuromuscular scoliosis patients have superior perioperative results than nonambulatory neuromuscular scoliosis patients and can approach adolescent idiopathic scoliosis outcomes after posterior spinal fusion. Spine (Phila Pa 1976) 47(5):E159-e68
Funding
No funding was received for the completion of this project.
Author information
Authors and Affiliations
Contributions
KAS: study design, data analysis, data interpretation, manuscript drafting, manuscript approval, accountable. HH: study design, data analysis, data interpretation, manuscript approval, accountable. NS, TR: study design, data analysis, manuscript editing, manuscript approval, accountable. JSM: study design, data interpretation, manuscript editing, manuscript approval, accountable. NDF: study design, data analysis, manuscript editing, manuscript approval, accountable.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Shaw is a committee member for NASS and AAOS; Ms Harris, Sachwani, and Ruska report nothing to disclose; Dr. Murphy reports receiving stock options from Alphatec Spine, is a consultant for Depuy and Orthopediatrics, receives research support from Epic Industries and Orthopediatrics, and is a committee member for POSNA and editorial member for Journal of Pediatric Orthopaedics and Journal of Spine Deformity; Dr. Fletcher reports is a consultant for Medtronic, is a speaker for Medrtonic, Nuvasive, Orthopediatrics, and Zimmer, and is a committee member for SRS and POSNA and an editorial member for JPOSNA.
Ethical approval
Approved by CHOA IRB: 14-030.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shaw, K.A., Harris, H., Sachwani, N. et al. Avoiding PICU admission following PSF for neuromuscular scoliosis in non-ambulatory cerebral palsy managed with ERAS protocol. Spine Deform 11, 671–676 (2023). https://doi.org/10.1007/s43390-022-00635-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00635-0