Abstract
Purpose
To assess clinical and safety outcomes associated with different rod materials and diameters in adult spinal deformity (ASD) surgery.
Methods
A systematic literature review and meta-analysis evaluated ASD surgery using pedicle screw fixation systems with rods of different materials and sizes. Postoperative outcomes (i.e., Cobb, sagittal vertical axis, and pelvic tilt angle) and complications (i.e., pseudarthrosis and rod breakage) were assessed. Random effects models (REMs) pooled data for outcomes reported in ≥ 2 studies.
Results
Among 50 studies evaluating ASD surgery using pedicle screw fixation systems, 17 described rod material/diameter. Postoperative outcomes did not statistically differ between cobalt–chromium (CoCr) vs. titanium (Ti) rods (n = 2 studies; mean [95% confidence interval (CI)] sagittal vertical axis angle: CoCr 37.00° [18.58°–55.42°] and Ti 32.58° [24.62°–40.54°]; mean [95% CI] pelvic tilt angle: CoCr 26.20° [22.87°–29.53°] and Ti 20.15° [18.0°–22.31°]). The pooled proportion (95% CI) of pseudarthrosis was 15% (7–22%) for CoCr and 12% (− 8–32%) for stainless steel (SS) (n = 2 studies each; Chi2 = 0.07, p = 0.79). The pooled proportion (95% CI) of broken rods was 12% (1–22%) for Ti (n = 3 studies) and 10% (2–19) for CoCr (n = 1 study). Among 6.0–6.35 mm rods, the pooled (95% CI) postoperative Cobb angle (n = 2) was 12.01° (9.75°–14.28°), sagittal vertical axis angle (n = 4) was 35.32° (30.02°–40.62°), and pelvic tilt angle was 21.11° (18.35°–23.86°).
Conclusions
For ASD patients undergoing posterior fixation and fusion, there are no statistically significant differences in postoperative outcomes or complications among rods of varying materials and diameters. Benchmark postsurgical outcomes and complication rates by rod material and diameter are provided.
Level of Evidence
III
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult spinal deformity (ASD) is a heterogeneous spectrum of abnormalities of the lumbar spine or the thoracolumbar spine that occurs in adult patients [1,2,3]. Specific ASD diagnoses include primary degenerative sagittal imbalance, iatrogenic spinal deformity, and adult spinal scoliosis [1, 2]. Symptoms of ASD include back and leg pain, numbness, tingling, and weakness [1]. These symptoms can result in functional limitations including difficulty standing upright, bending, and lifting, as well as ambulation and exercise intolerance [1]. The most common causes of spinal deformity in adults are iatrogenic flatback and degenerative scoliosis [1]. The global prevalence of adult spinal deformity is estimated to affect between 32–68% of individuals aged > 65 years, and the numbers of patients with ASD is expected to increase with age progression and a rise in life expectancy [4]. ASD may have a profound impact on a patient’s quality of life; however, there is significant variability in patient presentation [5].
The management of ASD usually begins with medical/interventional treatment with the goals of reducing pain and improving function. Operative treatment may be suggested for patients with progressive deformity, neural compromise, pain, and functional limitations which are not responsive to nonoperative conservative treatment [6, 7]. The aim of operative management of ASD is to restore spinal balance, relieve pain, and achieve solid fusion of vertebral segments. Depending on clinical presentation, a combination of surgical options including decompression, correction of deformity using osteotomies, rod manipulation maneuvers, and fusion may be carried out to achieve these goals [8]. Surgical treatment with pedicle screw fixation systems is a definitive management option for patients diagnosed with ASD.
Recent recognition of the importance of restoring sagittal balance [9], along with advances in surgical techniques and instrumentation have improved postoperative outcomes after ASD surgery; however, there are still opportunities for further improvement [10]. Although surgical management has been found to be beneficial for carefully selected patients, there is a risk of complications including dural tears, deep and superficial wound infections, implant complications, pseudarthrosis, adjacent segment disease, and acute and delayed neurological deficits [10, 11].
Multiple factors contribute to the successful correction of ASD and to minimizing the complications that may arise with surgical treatment [12, 13]. Spinal fixation rods are an important component of pedicle screw fixation systems and may play a significant role in the overall surgical outcomes and in the likelihood of complications [12]. Surgeons require rod options that resist rod fracture and breakage and that deliver the optimal alignment and treatment approach to meet the needs of each patient [12,13,14,15,16,17,18]. It is important to gain a better understanding of the rod-specific factors that may contribute to successful surgical and safety outcomes in ASD patients. More specifically, a better understanding of the clinical and economic value of various types of rods available for the surgical management of ASD would help healthcare providers and payers prioritize resource allocation and develop more effective and targeted interventions for the surgical treatment of ASD. Hence, the objectives of this study were to assess current evidence of the postoperative outcomes and complications associated with differing rod materials and dimensions for the operative treatment of ASD. An assessment of the current evidence will identify gaps that will inform priorities for future research.
Methods
Study design and approach
The systematic literature review and meta-analysis compared different rod characteristics for the surgical treatment for ASD. The systematic literature review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19]. The systematic review protocol was registered in the York PROSPERO database (PROSPERO: A registry for systematic review protocols | Augustus C. Long Health Sciences Library [columbia.edu]; PROSPERO 2020).
Literature search strategy
The literature search was conducted on November 20, 2020 by electronic searching of MEDLINE, Embase, KOSMET: Cosmetic Science, APA PsycInfo, and BIOSIS Previews. The search terms and search strategy utilized were: (spine* OR vertebra*) AND (fusion AND stabilization) AND (rods) AND (adults). The types of studies included were randomized controlled trials (RCTs), non-randomized clinical trials or studies, cohort studies, case control studies, registry studies, economic studies (budget impact and cost-effective analyses), and case series. Relevant secondary research with the highest levels of evidence, specifically systematic literature reviews and meta-analyses, was also included. Study types that were excluded were those that were technical articles, animal/cadaver studies, case reports, editorials, commentaries, and letters. Only English language literature was considered for review. The search was restricted to articles published on or after January 1, 2010.
Types of participants and interventions
Studies reporting adult patients aged > 18 years at the time of surgery, who had been diagnosed with any kind of spinal deformity (including congenital, degenerative, idiopathic, iatrogenic spinal deformity, flat back syndrome, failed back syndrome) were considered for the study. Adult spine deformity patients with other comorbid conditions were also eligible and were considered for the study. Studies reporting patients aged ≤ 18 years were excluded. Similarly, studies with patients without any spinal deformity were also excluded from the analysis.
Studies reporting any surgical management for spine deformity using any type of rods were included. While the majority of studies included only or mostly posterior pedicle screw fusion and fixation alone, other approaches included anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF, open or MIS–TLIF) along with the posterior pedicle screw construct. Deformity correction techniques included Ponte osteotomy, Smith–Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), and vertebral column resection (VCR). In addition, studies reporting different types of spine surgeries including primary surgeries, secondary surgeries (i.e., patients who already had previous spine surgeries prior to the surgery done during the actual study), or revision surgeries were also included. Studies involving surgical management of spine deformity but not incorporating rods or pedicle screws were excluded. Studies incorporating other conventional non-pharmacological treatments and experimental treatments were also excluded.
Surgical outcomes
An effort was made to capture and consider major postoperative outcomes and complications in the systematic review and meta-analysis. The postoperative outcomes that were evaluated included postoperative Cobb angle, sagittal vertical axis angle, and pelvic tilt angle. Postoperative complications that were evaluated included pseudarthrosis and rod breakage. Proximal junctional kyphosis (PJK) was not evaluated as there were no studies meeting the inclusion criteria and evaluating specific rod materials and/or diameters that reported PJK.
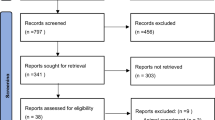
Study selection procedure and data extraction
Two reviewers independently applied the inclusion and exclusion criteria to screen de-duplicated titles and abstracts obtained from the search strategy. Potentially relevant citations were checked in a full-text screening. Disagreements were resolved through discussion and reasons for exclusion were recorded. Figure 1 illustrates the study selection process as a PRISMA flow diagram.
Pre-specified data that were extracted from the relevant studies included the journal citation, study objectives, study design and data source, intervention, comparator, study population (i.e., baseline demographic and clinical characteristics), sample size, duration of follow-up, primary and secondary outcome measures, and author’s conclusions.
Quality assessment of studies
The principles and methodology of Evidence-Based Practice Guidelines [20] were applied to assess the quality of evidence associated with the performance, safety and cost-effectiveness outcomes from the clinical studies and reports included. Studies were appraised for their level of evidence based on the study design and the rigor of methodology used, as well as the ability to prevent and/or control for biases to analyze cause and effect. All included studies were critically appraised and ranked using the Evidence level and Quality Guide from John Hopkins Nursing Evidence-Based Practice [21, 22].
Evidence synthesis and statistical analysis
Both qualitative and quantitative synthesis (using meta-analysis) were performed. Qualitative synthesis included summarizing individual studies and describing their results with respect to the relevant outcomes. For the quantitative synthesis, the data were analyzed using RevMan 5.4 and the meta-analysis was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19]. Pooling and grouping of findings across similar studies and study designs was done. Non-statistical methodology in synthesizing findings across studies of the same level of evidence was applied. Studies that presented and discussed relevant mixed cohort data were analyzed and summarized separately. Meta-analysis was performed for outcomes that were reported in at least two included studies. For continuous outcome measures (length of stay [LOS] and operating room [OR] time), the inverse variance random effects model (REM) was used to estimate the pooled mean difference (MD). The pooled standardized mean difference (SMD) was used for pain scores, since the studies used different pain scales. The mean and standard deviation (SD) were extracted from individual studies or were derived from medians with interquartile ranges or means with p values. For dichotomous outcomes, the Mantel–Haenszel REM was used to estimate the pooled risk ratios (RR). For the pooled summary statistics for each outcome in the surgical and non-surgical intervention groups, inverse variance REMs were used. All effect sizes were reported with 95% confidence intervals (CI). The χ2 test was used to test for statistical heterogeneity (α = 0.05) and heterogeneity was quantitatively evaluated using I2 statistics. Subgroup analyses evaluating the impact of (a) duration of study follow-up; (b) rod material; and (c) rod diameter were also conducted. The statistical significance was set at p value ≤ 0.05.
Results
Study identification and selection
The literature search yielded 1260 citations which were screened for inclusion. Full texts of 537 of the studies were retrieved for further screening, of which 189 were excluded based on the patient population, 59 based on the intervention, 50 based on the study design, 21 due to lack of relevant outcomes, 11 due to language, and 6 due to duplication of study data. A total of 50 studies evaluating patients aged > 18 years whose surgical management of ASD included pedicle screw and rod systems met the study inclusion criteria and were included in the systematic literature review and meta-analysis (Fig. 1).
Descriptive characterization of studies
Of the 50 studies evaluating the surgical management of ASD using posterior rods and pedicle screws, 17 studies described the rod material type [23,24,25,26,27,28,29,30,31,32,33,34,35]. Fourteen of the 17 studies reported the use of Ti rods either alone [23, 25, 27, 36, 37] or along with other rod materials.[26, 28,29,30,31,32, 35]. Eight studies reported the use of CoCr rods, either alone [24, 26, 28, 36] or along with other rod material [29, 31, 32, 34]. Thirteen studies reported the rod diameter used for the surgical management of ASD [23,24,25,26,27,28,29,30,31,32,33,34,35]. The rod diameter varied from 5.0 mm [35] to 6.35 mm [28, 32, 33], and 5.5 mm rods [27, 29]. Table 1 provides a description of the 50 included studies.
Meta-analyses
Impact of rod material
Clinical and functional outcomes
Sagittal vertical axis One study utilized CoCr posterior rods for ASD surgery and reported the postoperative sagittal vertical axis angle of patients (Fig. 2) [24]. The mean postoperative sagittal vertical axis angle with CoCr rods was 37.00° (95% CI: 18.58°–55.42°) [24]. One eligible study with two subgroups that utilized Ti rods reported a mean postoperative sagittal vertical axis of 32.58° (95% CI: 24.62°–40.54°) [25].
Pelvic tilt angle One study utilized CoCr posterior rods for ASD surgery and reported the postoperative pelvic tilt angle of patients (Fig. 3) [24]. The mean postoperative pelvic tilt angle with CoCr rods was 26.20° (95% CI 22.87°–29.53°) [24]. One eligible study with two subgroups that utilized Ti rods reported the postoperative pelvic tilt angle [25]. The analysis revealed a mean postoperative pelvic tilt angle of 20.15° (95% CI: 18.0°–22.31°).
Postoperative complications
Pseudarthrosis Two studies used CoCr rods and reported at least one case of pseudarthrosis in adult patients who underwent spine deformity surgery with pedicle screw fixation systems (Fig. 4) [26, 46]. The overall pooled proportion for pseudarthrosis was 15% (95% CI 7–22%) in patients receiving CoCr rods. Two studies used stainless steel (SS) rods and reported pseudarthrosis [32, 35]; the overall pooled proportion of pseudarthrosis was found to be 12% (95% CI − 8–32%). Test for subgroup differences showed no significant difference in the proportion of pseudarthrosis between the two rod materials (Chi2 = 0.07, p = 0.79).
Rod breakage Three studies that used Ti rods reported the presence of broken rods in adult patients who underwent spine deformity surgery with pedicle screw fixation systems (Fig. 5) [25, 27, 37]. The pooled subgroup proportion of broken rods was 12% (95% CI 1–22%) in patients that received Ti rods. Only one included study that used CoCr rods reported broken rods in adult patients after spine deformity surgery; the proportion of broken rods was 10% (95% CI 2–19%) [26]. Testing for subgroup differences was not done due to the small number of studies.
Impact of rod diameter
Clinical and functional outcomes
Cobb angle Two eligible studies utilized 6.0–6.35 mm posterior rods for ASD surgery and reported data on the postoperative Cobb angle (Fig. 6) [24, 26]. The overall pooled postoperative Cobb angle with 6.0–6.35 mm rods was 12.01° (95% CI 9.75°–14.28°).
Sagittal vertical axis Four studies utilized 6.0–6.35 mm posterior rods for ASD surgery and reported data on the postoperative sagittal vertical axis angle of patients (Fig. 7) [24,25,26, 28]. The pooled mean postoperative sagittal vertical axis angle with 6.0–6.35 mm rods was 35.32° (95% CI 30.02°–40.62°).
Pelvic tilt angle Three studies utilized 6.0–6.35 mm posterior rods for ASD surgery and reported data on the postoperative pelvic tilt angle of patients (Fig. 8) [24, 25, 28]. The pooled mean postoperative pelvic tilt angle with 6.0–6.35 mm rods was 21.11° (95% CI 18.35°–23.86°). There was a high degree of heterogeneity among included studies (I2 = 80%, p = 0.002).
Postoperative complications
No studies reported postoperative complication rates by rod diameter.
Discussion
The choice of rod used for the correction of deformity is an important consideration in the treatment of ASD. The composition and design of the spinal rod must strike a complex balance: the rod must be flexible enough for the surgeon to bend in the desired curve and have a high enough fatigue strength that it does not fracture or break during the therapeutic lifetime of the implant. The ability to resist damage brought about by contouring will depend on the material used and the diameter and shape of the rod. There have been significant changes in the types of rods and the materials used for rods over the years. Initially, Harrington rods consisted of SS. Present-day rod constructs are more likely to consist of either Ti or CoCr. These materials differ in yield strength and stiffness, with Ti having a lower yield strength and lower stiffness, and CoCr having higher yield strength and higher stiffness.
This systematic review and meta-analysis identified 50 qualifying studies evaluating the surgical management of ASD using pedicle screw fixation systems; among which 17 studies described the rod material and rod diameter used. Study findings showed that there was no evidence that surgical outcomes differed by rod material. Two studies reported sagittal vertical axis angle and pelvic tilt angle by rod material and did not find statistically significant differences between CoCr vs. Ti rods (mean postoperative sagittal vertical axis angle: CoCr rods 37.00° [95% CI 18.58°–55.42°] and Ti 32.58° [95% CI 24.62°–40.54°]; mean postoperative pelvic tilt angle: CoCr rods 26.20° [95% CI: 22.87°–29.53°] and Ti 20.15° [95% CI 18.0°–22.31°]). There was an absence of evidence evaluating the impact of rod diameter on postoperative outcomes and complications. Among 6.0–6.35 mm rods, the pooled postoperative Cobb angle was 12.01° (95% CI 9.75°–14.28°), the pooled mean postoperative sagittal vertical axis angle was 35.32° (95% CI 30.02°–40.62°), and the pooled mean postoperative pelvic tilt angle was 21.11° (95% CI 18.35°–23.86°).
In regard to complications, the overall pooled proportion of pseudarthrosis with CoCr rods (n = 2 studies) was 15% (95% CI 7.0–22.0%) and with SS rods (n = 2 studies) was 12% [95% CI − 8%–32%) (no significant difference; Chi2 = 0.07, p = 0.79). The pooled proportion of rod breakage with Ti rods (n = 3 studies) was 12% (95% CI 1.0% –22.0%) and CoCr rods (n = 1 study) was 10% (95% CI 2–19%). No studies reported postoperative complication rates by rod diameter.
Pseudarthrosis is one of the most common complications of ASD surgery, and also one of the most common and costly indications for revision surgery [73, 74]. Studies have also increasingly shown a link between pseudarthrosis and rod fracture [10, 34, 75,76,77]. Pseudarthrosis has been found to occur in over half of patients with rod fracture and three-quarters of patients with clinically significant rod fracture [12]. This may be explained by the effect of cyclic loading at a non-fused segment, allowing micro-movements to increase construct strain and risk of instrumentation failure [12]. Patients with radiographic evidence of pseudarthrosis after one year postoperatively may have increased risk of rod fracture and may require more careful observation [12].
Rod fracture is a common, problematic complication of ASD surgery, often requiring reoperation [12]. Similar to our current analysis, another recent meta-analysis found that the overall incidence of rod fracture was 12% [13]. The other meta-analysis did not evaluate rod characteristics associated with rod fracture; however, patient factors found to be associated with rod fracture included advanced age, higher body mass index, previous spine surgery, pedicle subtraction osteotomy, a larger preoperative pelvic tilt, and a larger preoperative thoracic kyphosis [13]. Efforts to reduce the incidence of rod fracture have been made, including the use of CoCr rods and multi-rod constructs; [12,13,14,15,16,17,18]; however, rod fracture continues to be a significant concern with the currently available rod treatment options and constructs [13]. Hence, there is a need for rods with improved fatigue performance so that breakage and, potentially pseudarthrosis, may be minimized.
The systematic review was designed to cover patients with ASD as comprehensively as possible given the published literature. It identified and summarized 50 studies evaluating the surgical management of ASD in which posterior fixation and fusion was part of the treatment plan. The study delineated the paucity of data available, and it is unfortunate how few of the studies directly compared rod materials and/or diameters. PJK was not evaluated in the current analyses as there were no studies meeting the inclusion criteria and evaluating specific rod materials and/or diameters that reported PJK.
A significant limitation of the meta-analysis component of this study is the heterogeneity of the patient populations evaluated, the variability in the surgical techniques and technologies employed, and the definitions of outcomes used in the analyses [78]. Reasons for such heterogeneity include variability in the definitions of ASD used across the available studies, resulting in varying pathologies and patient populations. The inherent complexity of patient needs and comorbidities, along with patient and surgeon treatment choices based on these complexities, further contributed to the variability. The requirements for customized surgical plans and the availability of published data with results for a specific population with a specific surgical technique hinder the accumulation of sufficient numbers of homogeneous cases for meta-analyses. Hence, we did not restrict our review to particular surgical treatments such as pedicle subtraction osteotomies (PSOs) or vertebrectomies or to types of technologies such as the use of interbody devices or specific grafting material. High volume, multi-center studies with shared definitions and consistent methods of documenting variability will be needed to address the knowledge gaps.
Meta-analysis may offer a way to highlight findings within such heterogeneity, including exposing areas for future research. It also provides a tool for helping to understand the extent of variability [79,80,81]. In the field of spinal procedures, a growing opinion suggests that inclusion of observational studies in meta-analyses might lead to more robust conclusions without compromising the quality of the results [82, 83]. The current study was conducted in line with recommendations available in the literature for the use of real-world evidence in meta-analyses [84]. Statistical heterogeneity was evaluated using Cochran’s Q test (χ2 test) and the I2 statistic. Since Q was significant and I2 was > 50%, it was appropriate to use the random-effects model (REM) to calculate pooled summary estimates. The range of I2 values observed in the current study (0% to 98%) is not inconsistent with the range of those observed in other meta-analyses of observational data. The heterogeneity present suggests that the meta-analysis covered a broad spectrum of patients with ASD, and the findings establish a foundation for future prospective and retrospective research.
Conclusions
For patients with ASD, there is a paucity of data evaluating the impact of rod material and rod diameter on ASD postoperative outcomes and complications. However, the current study provides benchmark measures of outcomes and complications for rods of varying material and diameter. Studies that presented postoperative outcomes and complications of ASD surgery by rod material and/or diameter had sizable complication rates. Technologies with improved fatigue performance (i.e., resisting rod fracture or breakage) could improve clinical and functional outcomes and complications.
References
Diebo BG, Shah NV, Boachie-Adjei O et al (2019) Adult spinal deformity. Lancet 394(10193):160–172. https://doi.org/10.1016/s0140-6736(19)31125-0
Youssef JA, Orndorff DO, Patty CA et al (2013) Current status of adult spinal deformity. Global Spine J 3(1):51–62. https://doi.org/10.1055/s-0032-1326950
Kim HJ, Yang JH, Chang D-G et al (2020) Adult spinal deformity: current concepts and decision-making strategies for management. Asian Spine J 14(6):886–897. https://doi.org/10.31616/asj.2020.0568
Good CR, Auerbach JD, O’Leary PT et al (2011) Adult spine deformity. Curr Rev Musculoskelet Med 4(4):159–167. https://doi.org/10.1007/s12178-011-9101-z
Pellisé F, Vila-Casademunt A, Ferrer M et al (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24(1):3–11. https://doi.org/10.1007/s00586-014-3542-1
Glassman SD, Dimar JR, Puno RM et al (1996) Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine 21(18):2163–2169
Fu KM, Bess S, Shaffrey CI et al (2014) Patients with adult spinal deformity treated operatively report greater baseline pain and disability than patients treated nonoperatively; however, deformities differ between age groups. Spine 39(17):1401–1407. https://doi.org/10.1097/brs.0000000000000414
Cho K-J, Kim Y-T, Shin S-H et al (2014) Surgical treatment of adult degenerative scoliosis. Asian Spine J 8(3):371–381. https://doi.org/10.4184/asj.2014.8.3.371
Cheung JPY (2020) The importance of sagittal balance in adult scoliosis surgery. Ann Transl Med. 8(2):35. https://doi.org/10.21037/atm.2019.10.19
Dinizo M, Dolgalev I, Passias PG et al (2021) Complications after adult spinal deformity surgeries: all are not created equal. Int J Spine Surg 15(1):137–143. https://doi.org/10.14444/8018
Sansur CA, Smith JS, Coe JD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine 36(9):E593–E597. https://doi.org/10.1097/BRS.0b013e3182059bfd
Barton C, Noshchenko A, Patel V et al (2015) Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis 10(1):30. https://doi.org/10.1186/s13013-015-0056-5
Noh SH, Kim KH, Park JY et al (2021) Characteristics and risk factors of rod fracture following adult spinal deformity surgery: a systematic review and meta-analysis. Neurospine 18(3):447–454. https://doi.org/10.14245/ns.2040832.416
Adogwa O, Buchowski JM, Lenke LG et al (2019) Comparison of rod fracture rates in long spinal deformity constructs after transforaminal versus anterior lumbar interbody fusions: a single-institution analysis. J Neurosurg Spine. https://doi.org/10.3171/2019.7.Spine19630
Jung J-m, Hyun S-J, Kim K-J et al (2020) Rod fracture after multiple-rod constructs for adult spinal deformity. J Neurosurg Spine SPI 32(3):407–414. https://doi.org/10.3171/2019.9.SPINE19913
Rabinovich EP, Buell TJ, Wang TR et al (2021) Reduced occurrence of primary rod fracture after adult spinal deformity surgery with accessory supplemental rods: retrospective analysis of 114 patients with minimum 2-year follow-up. J Neurosurg Spine 35(4):504–515. https://doi.org/10.3171/2020.12.Spine201527
Lee KY, Lee JH, Kang KC et al (2021) Strategies for prevention of rod fracture in adult spinal deformity: cobalt chrome rod, accessory rod technique, and lateral lumbar interbody fusion. J Neurosurg Spine. https://doi.org/10.3171/2020.8.Spine201037
Bourghli A, Boissière L, Kieser D et al (2021) Multiple-rod constructs do not reduce pseudarthrosis and rod fracture after pedicle subtraction osteotomy for adult spinal deformity correction but improve quality of life. Neurospine 18(4):816–823. https://doi.org/10.14245/ns.2142596.298
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA): Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Transparent Reporting of Systematic Reviews and Meta-Analyses. http://www.prisma-statement.org/ (2021). Accessed April 18 2021.
Dang A, Kaur K (2016) Comparative effectiveness research and its utility in In-clinic practice. Perspect Clin Res 7(1):9–14. https://doi.org/10.4103/2229-3485.173780
Newhouse R, Dearholt S, Poe S et al (2005) Evidence-based practice: a practical approach to implementation. J Nurs Adm 35(1):35–40. https://doi.org/10.1097/00005110-200501000-00013
Dang D, Dearholt SL (2017) Johns Hopkins nursing evidence-based practice: model and guidelines. Sigma Theta Tau
Ohba T, Ebata S, Oda K et al (2021) Utility of a computer-assisted rod bending system to avoid pull-out and loosening of percutaneous pedicle screws. Clin Spine Surg 34(3):E166–E171. https://doi.org/10.1097/bsd.0000000000001099
Buell TJ, Christiansen PA, Nguyen JH et al (2020) Coronal correction using kickstand rods for adult thoracolumbar/lumbar scoliosis: case series with analysis of early outcomes and complications. Oper Neurosurg (Hagerstown) 19(4):403–413. https://doi.org/10.1093/ons/opaa073
Banno T, Hasegawa T, Yamato Y et al (2019) Multi-rod constructs can increase the incidence of iliac screw loosening after surgery for adult spinal deformity. Asian Spine J 13(3):500–510. https://doi.org/10.31616/asj.2018.0209
Gupta S, Eksi MS, Ames CP et al (2018) A Novel 4-Rod technique offers potential to reduce rod breakage and pseudarthrosis in pedicle subtraction osteotomies for adult spinal deformity correction. Oper Neurosurg (Hagerstown) 14(4):449–456. https://doi.org/10.1093/ons/opx151
Shen FH, Qureshi R, Tyger R et al (2018) Use of the “dual construct” for the management of complex spinal reconstructions. Spine J 18(3):482–490. https://doi.org/10.1016/j.spinee.2017.08.235
Banno T, Hasegawa T, Yamato Y et al (2018) Assessment of the change in alignment of fixed segment after adult spinal deformity surgery. Spine 43(4):262–269. https://doi.org/10.1097/brs.0000000000002310
Merrill RK, Kim JS, Leven DM et al (2017) Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Glob Spine J 7(6):514–520. https://doi.org/10.1177/2192568217699392
Theologis AA, Safaee M, Scheer JK et al (2017) Magnitude, location, and factors related to regional and global sagittal alignment change in long adult deformity constructs: report of 183 patients with 2-year follow-up. Clin Spine Surg 30(7):E948–E953. https://doi.org/10.1097/bsd.0000000000000503
Smith JS, Shaffrey E, Klineberg E et al (2014) Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 21(6):994–1003. https://doi.org/10.3171/2014.9.Spine131176
Hyun SJ, Lenke LG, Kim YC et al (2014) Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine 39(22):1899–1904. https://doi.org/10.1097/brs.0000000000000556
Kim YC, Lenke LG, Hyun SJ et al (2014) Results of revision surgery after pedicle subtraction osteotomy for fixed sagittal imbalance with pseudarthrosis at the prior osteotomy site or elsewhere: minimum 5 years post-revision. Spine 39(21):1817–1828. https://doi.org/10.1097/brs.0000000000000526
Smith JS, Shaffrey CI, Ames CP et al (2012) Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 71(4):862–867. https://doi.org/10.1227/NEU.0b013e3182672aab
Soroceanu A, Diebo BG, Burton D et al (2015) Radiographical and Implant-Related Complications in adult spinal deformity surgery: incidence, patient risk factors, and impact on health-related quality of life. Spine 40(18):1414–1421. https://doi.org/10.1097/brs.0000000000001020
Marie-Hardy L, Pascal-Moussellard H, Barnaba A et al (2020) Screw loosening in posterior spine fusion: prevalence and risk factors. Glob Spine J 10(5):598–602. https://doi.org/10.1177/2192568219864341
Akazawa T, Kotani T, Sakuma T et al (2013) Rod fracture after long construct fusion for spinal deformity: clinical and radiographic risk factors. J Orthop Sci 18(6):926–931. https://doi.org/10.1007/s00776-013-0464-4
Echt M, Ranson W, Steinberger J et al (2021) A systematic review of treatment strategies for the prevention of junctional complications after long-segment fusions in the osteoporotic spine. Glob Spine J 11(5):792–801. https://doi.org/10.1177/2192568220939902
Prost S, Pesenti S, Farah K et al (2020) Adult spinal deformities: can patient-specific rods change the preoperative planning into clinical reality? feasibility study and preliminary results about 77 cases. Adv Orthop 2020:6120580. https://doi.org/10.1155/2020/6120580
Daniels AH, Reid DBC, Durand WM et al (2020) Assessment of patient outcomes and proximal junctional failure rate of patients with adult spinal deformity undergoing caudal extension of previous spinal fusion. World Neurosurg 139:e449–e454. https://doi.org/10.1016/j.wneu.2020.04.024
Sebaaly A, Gehrchen M, Silvestre C et al (2020) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 29(4):904–913. https://doi.org/10.1007/s00586-019-06253-1
Lau D, Haddad AF, Deviren V et al (2020) Asymmetrical pedicle subtraction osteotomy for correction of concurrent sagittal-coronal imbalance in adult spinal deformity: a comparative analysis. J Neurosurg Spine. https://doi.org/10.3171/2020.5.Spine20445
Hao J, Yan C, Liu S et al (2018) Effect of bone graft granule volume on postoperative fusion after lumber spinal internal fixation: a retrospective analysis of 82 cases. Pak J Med Sci 34(5):1231–1236. https://doi.org/10.12669/pjms.345.14971
Ailon T, Hamilton DK, Klineberg E et al (2018) Radiographic fusion grade does not impact health-related quality of life in the absence of instrumentation failure for patients undergoing posterior instrumented fusion for adult spinal deformity. World Neurosurg 117:e1–e7. https://doi.org/10.1016/j.wneu.2018.04.127
Yamato Y, Hasegawa T, Kobayashi S et al (2018) Treatment strategy for rod fractures following corrective fusion surgery in adult spinal deformity depends on symptoms and local alignment change. J Neurosurg Spine 29(1):59–67. https://doi.org/10.3171/2017.9.Spine17525
Lewis SJ, Mohanty C, Gazendam AM et al (2018) Posterior column reconstruction improves fusion rates at the level of osteotomy in three-column posterior-based osteotomies. Eur Spine J 27(3):636–643. https://doi.org/10.1007/s00586-017-5299-9
Alzakri A, Boissière L, Cawley DT et al (2018) L5 pedicle subtraction osteotomy: indication, surgical technique and specificities. Eur Spine J 27(3):644–651. https://doi.org/10.1007/s00586-017-5403-1
Levin JM, Alentado VJ, Healy AT et al (2018) Superior segment facet joint violation during instrumented lumbar fusion is associated with higher reoperation rates and diminished improvement in quality of life. Clin Spine Surg 31(1):E36-e41. https://doi.org/10.1097/bsd.0000000000000566
Lafage R, Line BG, Gupta S et al (2017) Orientation of the upper-most instrumented segment influences proximal junctional disease following adult spinal deformity surgery. Spine 42(20):1570–1577. https://doi.org/10.1097/brs.0000000000002191
Smith JS, Shaffrey CI, Klineberg E et al (2017) Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 27(4):444–457. https://doi.org/10.3171/2016.10.Spine16849
Park JH, Hyun SJ, Kim KJ et al (2017) Comparative study between pedicle subtraction osteotomy (pso) and closing-opening wedge osteotomy (fish-mouth pso) for sagittal plane deformity correction. Spine 42(15):E899-e905. https://doi.org/10.1097/brs.0000000000002007
Kavadi N, Tallarico RA, Lavelle WF (2017) Analysis of instrumentation failures after three column osteotomies of the spine. Scoliosis Spinal Disord 12:19. https://doi.org/10.1186/s13013-017-0127-x
Wang H, Guo J, Wang S et al (2017) instrumentation failure after posterior vertebral column resection in adult spinal deformity. Spine 42(7):471–478. https://doi.org/10.1097/brs.0000000000001844
Matsumura A, Namikawa T, Kato M et al (2017) Posterior corrective surgery with a multilevel transforaminal lumbar interbody fusion and a rod rotation maneuver for patients with degenerative lumbar kyphoscoliosis. J Neurosurg Spine 26(2):150–157. https://doi.org/10.3171/2016.7.Spine16172
Park SJ, Lee CS, Chung SS et al (2017) different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery 80(2):279–286. https://doi.org/10.1227/neu.0000000000001240
Wu B, Wang Z, Wang Y (2017) Clinical efficacy of expansive pedicle screw in degenerative scoliosis. Biomed Res 28:1325–1328
Kim JS, Phan K, Cheung ZB et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Glob Spine J 9(1):32–40. https://doi.org/10.1177/2192568218761362
Wang MY, Bordon G (2016) Mini-open pedicle subtraction osteotomy as a treatment for severe adult spinal deformities: case series with initial clinical and radiographic outcomes. J Neurosurg Spine 24(5):769–776. https://doi.org/10.3171/2015.7.Spine15188
Ghogawala Z, Dziura J, Butler WE et al (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374(15):1424–1434. https://doi.org/10.1056/NEJMoa1508788
Liu J, Cao L, Guo S et al (2016) Application of one stage posterior approach osteotomy with screw rod fixation and cage inserting anteriorly in late kyphosis deformity. Biomed Res 27(4):991–994
Uddin OM, Haque R, Sugrue PA et al (2015) Cost minimization in treatment of adult degenerative scoliosis. J Neurosurg Spine 23(6):798–806. https://doi.org/10.3171/2015.3.Spine14560
Iida T, Suzuki N, Kono K et al (2015) Minimum 20 Years long-term clinical outcome after spinal fusion and instrumentation for scoliosis: comparison of the srs-22 patient questionnaire with that in nonscoliosis group. Spine 40(16):E922–E928. https://doi.org/10.1097/brs.0000000000000991
Hyun SJ, Lenke LG, Kim YC et al (2015) Long-term radiographic outcomes of a central hook-rod construct for osteotomy closure: minimum 5-year follow-up. Spine 40(7):E428–E432. https://doi.org/10.1097/brs.0000000000000783
Omidi-Kashani F, Hootkani A, Jarahi L et al (2015) Radiologic and clinical outcomes of surgery in high grade spondylolisthesis treated with temporary distraction rod. Clin Orthop Surg 7(1):85–90. https://doi.org/10.4055/cios.2015.7.1.85
Lewis SJ, Goldstein S, Bodrogi A et al (2014) Comparison of pedicle subtraction and Smith-Petersen osteotomies in correcting thoracic kyphosis when closed with a central hook-rod construct. Spine 39(15):1217–1224. https://doi.org/10.1097/brs.0000000000000377
Dickson DD, Lenke LG, Bridwell KH et al (2014) Risk factors for and assessment of symptomatic pseudarthrosis after lumbar pedicle subtraction osteotomy in adult spinal deformity. Spine 39(15):1190–1195. https://doi.org/10.1097/brs.0000000000000380
Zhu Y, Wang B, Wang H et al (2014) Long-term clinical outcomes of selective segmental transforaminal lumbar interbody fusion combined with posterior spinal fusion for degenerative lumbar scoliosis. ANZ J Surg 84(10):781–785. https://doi.org/10.1111/ans.12711
Cho W, Mason JR, Smith JS et al (2013) Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity: clinical and radiographic risk factors: clinical article. J Neurosurg Spine 19(4):445–453. https://doi.org/10.3171/2013.6.Spine121129
Scheer JK, Tang JA, Smith JS et al (2013) Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database: clinical article. J Neurosurg Spine 19(4):464–470. https://doi.org/10.3171/2013.7.Spine12901
Kanayama M (2013) Sagittal plane correction in pedicle subtraction osteotomy using the Xia 3 SUK Direct Vertebral Rotation System: technical note. J Neurosurg Spine 19(4):507–514. https://doi.org/10.3171/2013.7.Spine121162
Crawford CH 3rd, Carreon LY, Bridwell KH et al (2012) Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 21(11):2165–2169. https://doi.org/10.1007/s00586-012-2310-3
Martini C, Langella F, Mazzucchelli L et al (2020) Revision strategies for failed adult spinal deformity surgery. Eur Spine J 29(Suppl 1):116–125. https://doi.org/10.1007/s00586-019-06283-9
Kelly MP, Lenke LG, Bridwell KH et al (2013) Fate of the adult revision spinal deformity patient: a single institution experience. Spine 38(19):E1196–E1200. https://doi.org/10.1097/BRS.0b013e31829e764b
Yeramaneni S, Gum JL, Carreon LY et al (2018) Impact of readmissions in episodic care of adult spinal deformity: event-based cost analysis of 695 consecutive cases. J Bone Joint Surg Am 100(6):487–495. https://doi.org/10.2106/jbjs.16.01589
Yang BP, Ondra SL, Chen LA et al (2006) Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 5(1):9–17. https://doi.org/10.3171/spi.2006.5.1.9
Ikenaga M, Shikata J, Takemoto M et al (2007) Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 6(4):330–336. https://doi.org/10.3171/spi.2007.6.4.8
Charosky S, Guigui P, Blamoutier A et al (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine 37(8):693–700
Higgins J, Thompson S, Deeks J et al (2002) Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy 7(1):51–61. https://doi.org/10.1258/1355819021927674
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012. https://doi.org/10.1001/jama.283.15.2008
Egger M, Schneider M, Davey SG (1998) Spurious precision? Meta-analysis of observational studies. BMJ 316(7125):140–144. https://doi.org/10.1136/bmj.316.7125.140
Huston P, Naylor CD (1996) Health services research: reporting on studies using secondary data sources. CMAJ 155(12):1697–1709
Smeeing DPJ, van der Ven DJC, Hietbrink F et al (2017) Surgical versus nonsurgical treatment for midshaft clavicle fractures in patients aged 16 years and older: a systematic review, meta-analysis, and comparison of randomized controlled trials and observational studies. Am J Sports Med 45(8):1937–1945. https://doi.org/10.1177/0363546516673615
Abraham NS, Byrne CJ, Young JM et al (2010) Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. J Clin Epidemiol 63(3):238–245. https://doi.org/10.1016/j.jclinepi.2009.04.005
Briere JB, Bowrin K, Taieb V et al (2018) Meta-analyses using real-world data to generate clinical and epidemiological evidence: a systematic literature review of existing recommendations. Curr Med Res Opin 34(12):2125–2130. https://doi.org/10.1080/03007995.2018.1524751
Funding
The study was funded by Johnson & Johnson.
Author information
Authors and Affiliations
Contributions
DB, Study conception and design, data collection and analysis, and manuscript preparation, revision, and final approval. AM, Study conception and design, data collection and analysis, and manuscript revision and final approval. MM, Study conception and design, data collection and analysis, and manuscript revision and final approval. SW, Study conception and design, data analysis, and manuscript revision and final approval.
Corresponding author
Ethics declarations
Conflict of interest
DB, AM, MM, and SW are employees of Johnson and Johnson.
Ethics approval
Not required as it is a systematic review and meta-analysis of previously published data.
Informed consent
Not required as it is a systematic review and meta-analysis of previously published data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bowden, D., Michielli, A., Merrill, M. et al. Systematic review and meta-analysis for the impact of rod materials and sizes in the surgical treatment of adult spine deformity. Spine Deform 10, 1265–1278 (2022). https://doi.org/10.1007/s43390-022-00556-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00556-y