Abstract
Study design
A group of adult patients with idiopathic scoliosis, diagnosed before the age of ten, at a mean of 26.5 years after treatment with either brace or surgery during childhood and adolescence attended a clinical follow-up.
Objectives
To evaluate the relation between thoracic mobility, rib-cage deformity, and pulmonary function.
Summary of background data
Long-term studies of pulmonary function in relation to thoracic mobility after treatment in this patient group have not been published.
Methods
A total of 106 patients, 57 braced and 49 operated patients, attended the follow-up. We examined thoracic mobility (range of motion of the thoracic spine, thorax expansion, and breathing movements) and rib-cage deformity (curve size and trunk deformity) as well as pulmonary function, especially total lung capacity (TLC). Respiratory muscle strength was evaluated in a subgroup.
Results
Thoracic range of motion was significantly less among the surgically treated patients compared with both the brace-treated and comparison group. Thorax expansion and breathing movements during maximal breathing were significantly reduced in the scoliotic patients compared with the reference values, with no significant differences between the treatment groups. The brace-treated group had better pulmonary function than the operated group, as measured by the TLC, forced vital capacity (FVC), and forced expiratory volume in one second (FEV1) (percentage of predicted values). The respiratory muscle strength was significantly lower only in the surgically treated patients when compared with reference values. The results of a multivariate analysis revealed that the strongest factors explaining TLC percentage of predicted were gender, brace model, and smoking habits.
Conclusions
Thoracic mobility was significantly reduced at mean 26.5 years after completed treatment in both brace-treated and surgically treated patients with early onset scoliosis, compared with the reference values, which did not influence TLC as strongly as gender, brace model, and smoking habits.
Levels of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-term studies have shown that, left untreated, patients with early onset of scoliosis run an increased risk for respiratory failure and premature death [1]. This is probably due to restricted lung development before adulthood resulting in lower number of alveoli [2, 3] and to altered biomechanics of the rib cage.
Early onset scoliosis that increases to a large curve size also results in chest deformity with ensuing reduced chest and lung volume [4]. Furthermore, the distorted chest is thought to lead to reduced thoracic mobility and increased work of breathing. The treatment of scoliosis with full-time brace wearing for several years or with fusion of the spine might also contribute to restricted motion of the rib cage. The mobility and muscle endurance of the spine in adult patients treated for scoliosis during childhood and adolescence has been shown to be reduced [5,6,7]. However, the thoracic mobility and the breathing movements have not been evaluated in these groups of patients, despite the possibility for its evident clinical importance.
Basic pulmonary function has traditionally been measured with spirometry [8]. Other methods exist, but have not been extensively used for scoliosis patients. The respiratory movements consist of abdominal and rib-cage movements [9]. The separate volume changes of the rib cage and abdomen can be measured during breathing, and healthy individuals can breathe with any combination of these locations of breathing [9]. In the sitting position, abdominal breathing dominates, probably because of a more optimal muscle fiber length of the diaphragm leading to a stronger contraction [10], and the rib cage contributes 60% to total ventilation, compared with 35% in the supine position.
Thoracic mobility, that is, the mobility of the thoracic spine and the rib cage, is often measured with a kyphometer [11] and with measurement of the degree of thorax expansion during breathing [12,13,14]. The latter gives a general overview of the maximal range of motion in the upper and the lower part of the rib cage. The measurement of breathing movements [15,16,17], another way to evaluate the rib-cage mobility, has been available for the past 10 years by use of the Respiratory Movement Measuring Instrument (RMMI). Several studies, with patients with ankylosing spondylitis, after cardiac surgery, and those diagnosed with sensory hyperreactivity, have been published [18,19,20].
Breathing movements and maximal range of motion in the rib cage are associated with the strength in the respiratory muscles. For evaluation of respiratory muscle strength, noninvasive measurement of the maximal inspiratory pressure (MIP) and the maximal expiratory pressure (MEP) is used [21, 22].
The aim of this study was to evaluate how thoracic mobility, as measured by different methods, and rib-cage deformity relate to pulmonary function in adult patients treated for early onset idiopathic scoliosis during childhood or adolescence. The total lung capacity (TLC), considered the key measurement for establishment of a restrictive deterioration of the ventilatory capacity when performed in a body plethysmograph, was chosen to represent the pulmonary function.
Methods
Patients
The Gothenburg Scoliosis Database, which contains information about all patients between 1966 and 1994 with scoliosis at the Department of Orthopaedics at the Sahlgrenska University Hospital, Gothenburg, Sweden, was used to identify the study population. This met the following criteria: (1) diagnosis of idiopathic scoliosis before the age of 10 years; (2) treatment with either a brace (for at least 6 months) or with surgery; (3) no other related disorders or spine anomalies; and (4) > 10 years since maturity or surgical procedure. Details about the treatments have been published earlier (https://doi.org/10.1016/j.jspd.2015.07.007).
The original series of patients consisted of 179 consecutive patients, of which 106 completed this study (Fig. 1). Fifty-seven patients were brace-treated only until maturity, until 1974 with a Milwaukee brace (in 24 patients) and thereafter a Boston brace (33 patients). All together, 49 patients were surgically treated and 31 of those were initially braced but operated before maturity due to curve progression. A further six patients, with a remaining significant curve at maturity or curve progression after maturity, were operated shortly after maturity, before the age of 22 years. The surgical procedure was performed with Harrington instrumentation until 1995 (used in 46 patients) and thereafter with the Isola system (in three patients).
Examination of the curve, pulmonary function, and smoking habits
All patients underwent measurement of rib-cage deformity including trunk deformity by use of Bunnell scoliometer [23]. Full standing posterior–anterior digital roentgenograms were performed at the follow-up, and curve size was measured using the Cobb method [24].
Spirometry by a pressure-differences method (Jaeger MasterScope) was used to measure forced vital capacity (FVC) and forced expiratory volume in one second (FEV1). TLC was measured with a body plethysmograph. Values are presented as the percentage of predicted values related to age, height, and gender according to Quanjer et al. [8] for FVC and FEV1 and Quanjer et al. [25] for TLC and corrected to loss of height due to scoliosis according to Lind [26].
The patients were asked about smoking habits, and they were thereafter classified into either never smokers or current/ex-smokers (“ever-smokers”).
Examination of thoracic mobility with three different methods
Three different methods were used for evaluation of the different aspects of the function of the thoracic cage: (1) range of motion of the thoracic spine [11]; (2) expansion of the thorax during breathing [13, 14]; and (3) breathing movements—respiratory movement measuring instrument (RMMI) [27,28,29,30]. The methods are described in Table 1 and Figs. 2, 3, 4, 5, 6.
Examination of respiratory muscle strength
The respiratory muscle strength was examined in a subgroup of 33 patients (of the 106 in the original study group) three to 5 years after the initial follow-up. The method is described in Table 1 [22]. The mean curve size at follow-up was similar in these two groups, mean 37.2° (brace-treated [BT] group, 36.1°, n = 16; and surgically treated [ST] group, 38°, n = 17; p = 0.6). The number of ever-smokers was 11 (33.3%) (BT group, 7 [43%]; ST group 4 [23%]).
Statistical methods
Distributions of variables are given as means, standard deviations, and ranges. For comparison between the two groups and the groups versus normal/reference values, the Mann–Whitney nonparametric U test was used. For comparison of proportions between two groups, Fisher exact test was used.
Spearman rank correlation coefficient was used for correlation analysis. Correlation was defined as follows: little, if any (rs < 0.25), low (rs = 0.26–0.49), moderate (rs = 0.50–0.69), high (rs = 0.70–0.89), and very high (rs = 0.9–1.00) [31].
A univariate and multivariate analysis was made based on variables possible to explain TLC percent predicted. All significance tests were two-tailed and were conducted at the 5% significance level.
Results of the univariate analysis
Description of demographic data, curve size, trunk deformity, pulmonary function, and smoking habits
Table 2 depicts information about the study group. Mean age at diagnosis and at the present study was 7 years and 41.7 years, respectively, with no significant difference between the braced and the operated patients. Curve size before treatment was significantly larger in the operated group compared with the braced group (57° vs. 28°) and 35 patients (all in the ST group) had a curve size of 50° or more. Curve size at present follow-up did not differ significantly between the groups (ST 37° and BT 35°), and also the number of patients with a curve size of 50° or more was similar (ST 10 patients, BT 12 patients). The mean duration of brace treatment was 4.4 years.
At the present follow-up, operated patients had a larger trunk deformity, 16°, compared with the braced patients, 11° (p < 0.001). Curve apex at present follow-up was located at T9 or above in 86 (81%) of the patients.
Results concerning pulmonary function are also given in Table 2. The mean TLC (% predicted values) was 90%, but with a large individual variation (range 38–121%). The TLC differed significantly between the BT and ST groups with 96% and 84%, respectively, p < 0.001. Thirty-nine percent were ever-smokers, that is, current or ex-smokers, 42% of BT and 35% of ST (nonsignificant).
Thoracic mobility
The range of motion of the thoracic spine, presented in Table 3, showed that the BT group had significantly better range of motion (p < 0.001), and the ST group had significantly reduced values (p < 0.001) compared with the reference values. The ST group had a significantly stiffer thoracic spine than the BT group (p < 0.001).
Both the BT and ST patients were able to expand their chest cage (“thorax expansion”) significantly less (14 and 19 mm) at the level of the xiphoid process, compared with the reference values (p < 0.001). The BT patients and the ST patients did not differ significantly, neither at the level of the xiphoid process (p = 0.07) nor at the level of the fourth rib (p = 0.53) (Table 3).
The respiratory movements (the RMMI tests) during maximal breathing, compared with a reference group of 100 healthy men and women 20–69 years of age [27], were significantly decreased, by mean values of up to 12 mm, in both BT and ST groups, at all locations of the rib cage, compared with the reference values (p < 0.001; Table 3). There were no significant differences between the BT and ST groups (not presented in the table).
Respiratory muscle strength
The respiratory muscle strength was significantly reduced to 67% of MIP and 79% of MEP reference values in the ST group, but this was not found for the BT group (Table 3). Between the two treatment groups, there were no significant differences in either MIP or MEP.
Correlations between mobility of the thoracic spine, pulmonary function, and rib-cage deformity
Correlation analyses between the three modes for measurement of thoracic mobility, pulmonary function, and rib-cage deformity are presented in Table 4.
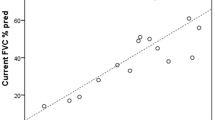
The ability to expand the thorax (expansion tests) correlated little or moderately with the pulmonary function tests (TLC, FVC, and FEV1), r = 0.43–0.64. Neither pulmonary function (TLC, FVC, or FEV1) nor curve (size and trunk deformity) correlated with breathing movements.
Respiratory muscle strength (both MIP and MEP) correlated moderately with all the three pulmonary function tests, TLC, FVC, and FEV1 (r = 0.50–0.61), as well as with thorax expansion (upper, lower, and upper in combination with lower) (r = 0.41–0.63) (Table 5).
Multivariate analysis
A multivariable linear regression model explaining TLC as percentage of predicted was based on significant results of the univariable analysis and results are presented in Table 6. The R-squared value for the multivariable model was 0.619.
An additional analysis was made for the subgroup of 33 patients, who were also examined for respiratory muscle strength. These added variables were not strong enough to further explain the percentage of TLC predicted.
Discussion
This study is the first follow-up of thoracic mobility in previously treated patients with early onset idiopathic scoliosis. The main finding is that both brace-treated and surgically treated patients showed significantly reduced thorax expansion and respiratory movements at a mean of 26.5 years after completed treatment. Our aim was to explore these findings in relation to the pulmonary function, which were previously presented (https://doi.org/10.1016/j.jspd.2015.07.007).
Thoracic mobility
The range of motion of the thoracic spine was measured with a Debrunner Kyphometer and, as expected, the ST group had significantly reduced values compared with the BT group as a result of several fused vertebrae, as in previous studies of adolescent idiopathic scoliosis [5]. The ability for the chest cage to expand the thorax was significantly reduced by 14–19 mm in both groups, compared with the reference values. Two other studies have previously, with other methods, evaluated rib-cage movements in patients with idiopathic scoliosis and found them to be reduced [32, 33]. As information about onset of scoliosis or treatment is lacking in those studies, comparisons are troublesome. The clinical value of the reduction, being less than 20 mm, needs to be established before a proper evaluation on pulmonary function can be made.
Maximal breathing movements during deep breathing were measured with RMMI, and the patients had approximately 10 mm less movement compared with the reference values [27]. No previous studies on individuals with scoliosis exist for comparison. The reduction is likely to be considered small, in relation to the total anteroposterior diameter, and the clinical significance needs to be evaluated with further studies.
Respiratory muscle strength
The possibility for later evaluation of respiratory muscle strength led us to add this examination in a subgroup of 33 patients, as this component is considered to be of high importance for respiration. This subgroup was similar in terms of curve size and ever-smokers.
The surgically treated patients in this subgroup had significantly less muscle strength compared with the reference group, whereas the braced patients had not. In addition, the moderate correlations between respiratory muscle strength and pulmonary variables were found. Muscle strength and function are closely associated with one another and decreased thoracic mobility was found in the scoliotic patients. Whether these findings are results of the scoliotic rib-cage deformity itself or a stiffer spine after surgery or a prolonged brace treatment is unknown. This study evaluates late additive results of both deformity and the treatment of the deformity, and was not designed to evaluate these issues separately.
Respiratory muscle strength has previously been tested in patients with chronic obstructive pulmonary disease [34], cystic fibrosis [35], and ankylosing spondylitis [36] and found to have different levels of associations. In the latter study [36], they found correlations between thorax expansion and MIP and MEP, similar to our findings.
From our results, it is not possible to evaluate whether the diaphragmatic motion is affected, because we have not evaluated its function. Kotani et al. [33], who also found restricted rib-cage movements in patients with idiopathic scoliosis, reported that the diaphragmatic motion was normal. This is contradictory to Chu et al. [37], who found that diaphragmatic heights significantly reduced in patients with severe idiopathic scoliosis when measured by dynamic magnetic resonance imaging.
Correlations between results
The ability for thorax expansion and the respiratory muscle strength correlated (moderately) with the pulmonary function (TLC, FVC, and FEV1), whereas the breathing movements (RMMI) did not show any correlations of significance. Hagman et al. [38] found a strong correlation between measured breathing movements and breathing volumes. They did their measurements, with RMMI and a dynamic spirometer, simultaneously in three different body positions—supine, sitting on a chair, and standing with the back against a wall. In our study, the supine position was used for the breathing movements with RMMI because of the need of a stable position for the measurement of the anteroposterior movements and the fact that the reference values were collected in the supine position [27]. Both the spirometry and the respiratory muscle strength were measured in the sitting position, whereas the expansion of the thorax during breathing was measured in an upright standing position because of the testing position of this reference group [13]. These different body positions during the tests might be an explanation for the lack of correlation.
Further comments on pulmonary function tests and smoking habits
The ventilatory capacity of the patients in this study was evaluated by use of spirometry, with data on FVC and FEV1 as well as by use of body plethysmograph measuring TLC. The pulmonary function tests are presented as percentage predicted values. These are mean values for the normal population adjusted for height, age, and gender, and therefore, normal individual predicted values range from 80 to 120% [25]. The main deterioration of pulmonary function due to scoliosis and its treatment is restrictive ventilation. TLC is the key measurement to evaluate restrictive disorders of ventilation and was, therefore, chosen as the main outcome of the pulmonary function in this study.
The multivariate linear regression model, aimed to explain the TLC percentage predicted, included five variables, of which two belong to the time of the treatment (curve size and type of brace), two to demographics (gender and smoking), and one to the time of the current follow-up (lower thorax expansion). Their level of explanation was an R-squared value of 0.619. Gender, brace model, smoking habits, thorax expansion (xiphoideus), and curve size at start of treatment were strongly associated with TLC percentage predicted.
The impact of gender in lung volumes is well-known, as men in general have larger lung volumes than women. Despite our analyses using the percentage of predicted values, constructed to eliminate the gender difference, the male gender has an association with lower TLC in this study. That the type of brace was of importance can be explained by the use of the stiffer Milwaukee brace compared with the less rigid Boston brace, which is still in use. With more modern braces in use, for instance, the night braces worn for less time, these negative effects might be reduced in the future.
Smoking has a strong association to TLC percentage predicted values, where “ever-smokers” have higher values (96% of predicted) than never-smokers (86% of predicted). This finding presents a possible difficulty in evaluating the effect on the decrease of TLC related to treatment for scoliosis. The higher values in smokers is most probably due to the development of emphysema, which also has been reported to increase TLC in apparently healthy smokers [39]. As the proportion of smokers does not differ between the surgically or brace-treated groups, our interpretation is that smoking does not influence the effect of various treatments for scoliosis, where increasing curve size or decreasing thoracic expansion is related to a low TLC, as a matter of restrictive pulmonary function. Emphysema adds an obstructive component to any restrictive consequence of scoliosis; therefore, avoiding or quitting smoking is a very important advice for patients treated for scoliosis.
Strength and limitations of the study
One advantage of this study is the long follow-up time of a group of 106 patients with early onset scoliosis. The original group of 179 patients is considered a consecutive series of which finally 59% participated. Another advantage is that we have analyzed the mobility of the thoracic cage and its relation to the total lung capacity, which has previously not been studied. A limitation of the study is that we did not compare the results to matched control subjects. To compensate, we used reference values consisting of corresponding groups of healthy individuals of similar age and gender. Another limitation is that the number of patients in the subgroup having measured MIP and MEP is small. However, both brace-treated and surgically treated were evaluated together.
Conclusions
Thoracic mobility was significantly reduced at follow-up (mean 26.5 years after completed treatment) in both brace-treated and surgically treated patients with early onset scoliosis. TLC values as a measurement of pulmonary function were influenced by gender, brace model, smoking habits, thorax expansion, and curve size at the start of treatment. Because smoking is also associated with several additional health problems, patients must be advised to not smoke.
Key points
-
Thoracic mobility, except for the range of motion of the thoracic spine in the brace-treated patients, was significantly reduced at mean 26.5 years after completed treatment.
-
These reductions had limited impact on the total lung capacity.
-
The total lung capacity had strong associations with smoking habits, brace model, gender, thorax expansion (xiphoideus), and curve size at the start of treatment.
-
Individuals with scoliosis must be strongly advised not to smoke.
References
Pehrsson K, Larsson S, Oden A, Nachemson A (1992) Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 17:1091–1096
Davies G, Reid L (1970) Growth of the alveoli and pulmonary arteries in childhood. Thorax 25:669–681
Narayanan M, Owers-Bradley J, Beardsmore CS et al (2012) Alveolarization continues during childhood and adolescence: new evidence from helium-3 magnetic resonance. Am J Respir Crit Care Med 185:186–191
Charles YP, Dimeglio A, Marcoul M et al (2008) Influence of idiopathic scoliosis on three-dimensional thoracic growth. Spine (Phila Pa 1976) 33:1209–1218
Danielsson AJ, Romberg K, Nachemson AL (2006) Spinal range of motion, muscle endurance, and back pain and function at least 20 years after fusion or brace treatment for adolescent idiopathic scoliosis: a case-control study. Spine (Phila Pa 1976) 31:275–283
Grauers A, Topalis C, Moller H et al (2014) Prevalence of back problems in 1069 adults with idiopathic scoliosis and 158 adults without scoliosis. Spine (Phila Pa 1976) 39:886–892
Mahaudens P, Banse X, Mousny M et al (2013) Very short-term effect of brace wearing on gait in adolescent idiopathic scoliosis girls. Eur Spine J 22:2399–2406
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-years age range: the global lung function 2012 equations. Eur Respir J 40:1324–1343
Konno K, Mead J (1967) Measurement of the separate volume changes of rib cage and abdomen during breathing. J Appl Physiol 22:407–422
Lumb AB, Nunn JF (1991) Respiratory function and ribcage contribution to ventilation in body positions commonly used during anesthesia. Anesth Analg 73:422–426
Öhlén G (1989) Spinal sagittal configuration and mobility: a kyphometer study
Moll JM, Wright V (1972) An objective clinical study of chest expansion. Ann Rheum Dis 31:1–8
Finsbäck C, Mannerkorpi K (2005) Spinal and thoracic mobility—age-related values for healthy men and women. Nord Fysioter 9:136–143
Olsén MF, Lindstrand H, Broberg JL, Westerdahl E (2011) Measuring chest expansion: a study comparing two different instructions. Adv Physiother 13:128–132
Banzett RB, Mahan ST, Garner DM et al (1985) A simple and reliable method to calibrate respiratory magnetometers and respitrace. J Appl Physiol 1995(79):2169–2176
Agostoni E, Rahn H (1960) Abdominal and thoracic pressures at different lung volumes. J Appl Physiol 15:1087–1092
Cohn M, Watson H, Weisshaut R et al (eds) (1978) A transducer for non-invasive monitoring of respiration. Proceedings of the Second International Symposium on Ambulatory Monitoring. New York, NY: Academic Press
Ragnarsdottir M, Geirsson AJ, Gudbjornsson B (2008) Rib cage motion in ankylosing spondylitis patients: a pilot study. Spine J 8:505–509
Kristjansdottir A, Ragnarsdottir M, Hannesson P et al (2004) Respiratory movements are altered 3 months and 1 year following cardiac surgery. Scand Cardiovasc J 38:98–103
Johansson EL, Ternesten-Hasseus E, Olsen MF, Millqvist E (2012) Respiratory movement and pain thresholds in airway environmental sensitivity, asthma and COPD. Respir Med 106:1006–1013
Rochester DF (1985) The diaphragm: contractile properties and fatigue. J Clin Invest 75:1397–1402
Sclauser Pessoa IM, Franco Parreira V, Fregonezi GA et al (2014) Reference values for maximal inspiratory pressure: a systematic review. Can Respir J 21:43–50
Amendt LE, Ause-Ellias KL, Eybers JL et al (1990) Validity and reliability testing of the scoliometer. Phys Ther 70:108–117
Cobb J (1948) Technique for study of scoliosis. AAOS Instructional course lectures. pp 261–75
Quanjer PH, Tammeling GJ, Cotes JE et al (1993) Lung volumes and forced ventilatory flows. Eur Respir J 6(suppl 16):5–40
Lindh M, Bjure J (1975) Lung volumes in scoliosis before and after correction by the Harrington instrumentation method. Acta Orthop Scand 46:934–948
Ragnarsdottir M, Kristinsdottir EK (2006) Breathing movements and breathing patterns among healthy men and women 20–69 years of age. Reference values. Respiration 73:48–54
Cahalin LP, Ragnarsdottir M (2002) Reliability, validity, and clinical utility of a novel respiratory movement measurement instrument (critical care–outcomes: 12: 00 pm–1: 45 pm). Chest 122:207
Gunnesson IL, Olsen MF (2011) Validity in measuring breathing movements with the respiratory movement measuring instrument, RMMI. Clin Physiol Funct Imaging 31:1–4
Olsen MF, Romberg K (2010) Reliability of the respiratory movement measuring instrument, RMMI. Clin Physiol Funct Imaging 30:349–353
Domholdt E (2005) Rehabilitation research: principles and applications. Elsevier Saunders, St. Louis
Leong J, Lu W, Luk K, Karlberg E (1999) Kinematics of the chest cage and spine during breathing in healthy individuals and in patients with adolescent idiopathic scoliosis. Spine 24:1310
Kotani T, Minami S, Takahashi K et al (2004) An analysis of chest wall and diaphragm motions in patients with idiopathic scoliosis using dynamic breathing MRI. Spine 29:298–302
Kim NS, Seo JH, Ko MH et al (2017) Respiratory muscle strength in patients with chronic obstructive pulmonary disease. Ann Rehabil Med 41:659–666
Arikan H, Yatar I, Calik-Kutukcu E et al (2015) A comparison of respiratory and peripheral muscle strength, functional exercise capacity, activities of daily living and physical fitness in patients with cystic fibrosis and healthy subjects. Res Dev Disabil 45(46):147–156
Sahin G, Calikoglu M, Ozge C et al (2004) Respiratory muscle strength but not BASFI score relates to diminished chest expansion in ankylosing spondylitis. Clin Rheumatol 23:199–202
Chu WC, Li AM, Ng BK et al (2006) Dynamic magnetic resonance imaging in assessing lung volumes, chest wall, and diaphragm motions in adolescent idiopathic scoliosis versus normal controls. Spine 31:2243–2249
Hagman C, Janson C, Malinovschi A et al (2016) Measuring breathing patterns and respiratory movements with the respiratory movement measuring instrument. Clin Physiol Funct Imaging 36:414–420
Tylen U, Boijsen M, Ekberg-Jansson A et al (2000) Emphysematous lesions and lung function in healthy smokers 60 years of age. Respir Med 94:38–43
Acknowledgements
Open access funding provided by University of Gothenburg. We wish to thank Anne Dohsé, RN, Department of Orthopaedics, Gothenburg University, for assistance during the study. We would also like to thank Kate Bramley-Moore, PhD, for her English language editing assistance.
Funding
Funds were received as total or partial support for the research in this article from the Gothenburg Medical Society, the Neubergh Foundations, and through “the Agreement concerning research and education of doctors”, the Renée Eander fund and the Norrbacka Eugenia fund. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KR (none), MFO (none), GKW (none), KLH (none), AD (none).
IRB approval
The study was approved by the Human Research Committee at the Medical Faculty, Gothenburg University, Gothenburg, Sweden, # 081/07. The patients were included after verbal and written information and signed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Romberg, K., Fagevik Olsén, M., Kjellby-Wendt, G. et al. Thoracic mobility and its relation to pulmonary function and rib-cage deformity in patients with early onset idiopathic scoliosis: a long-term follow-up. Spine Deform 8, 257–268 (2020). https://doi.org/10.1007/s43390-019-00018-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-019-00018-y