Abstract
Understanding clinical features and risk factors associated with COVID-19 mortality is needed to early identify critically ill patients, initiate treatments and prevent mortality. A retrospective study on COVID-19 patients referred to a tertiary hospital in Iran between March and November 2020 was conducted. COVID-19-related mortality and its association with clinical features including headache, chest pain, symptoms on computerized tomography (CT), hospitalization, time to infection, history of neurological disorders, having a single or multiple risk factors, fever, myalgia, dizziness, seizure, abdominal pain, nausea, vomiting, diarrhoea and anorexia were investigated. Based on the investigation outcome, decision tree and dimension reduction algorithms were used to identify the aforementioned risk factors. Of the 3008 patients (mean age 59.3 ± 18.7 years, 44% women) with COVID-19, 373 died. There was a significant association between COVID-19 mortality and old age, headache, chest pain, low respiratory rate, oxygen saturation < 93%, need for a mechanical ventilator, having symptoms on CT, hospitalization, time to infection, neurological disorders, cardiovascular diseases and having a risk factor or multiple risk factors. In contrast, there was no significant association between mortality and gender, fever, myalgia, dizziness, seizure, abdominal pain, nausea, vomiting, diarrhoea and anorexia. Our results might help identify early symptoms related to COVID-19 and better manage patients according to the extracted decision tree. The proposed ML models identified a number of clinical features and risk factors associated with mortality in COVID-19 patients. These models if implemented in a clinical setting might help to early identify patients needing medical attention and care. However, more studies are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In January 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was discovered [1]. Since then, the virus has spread exponentially and caused immense human suffering worldwide [2,3,4,5,6]. The high number of deaths and the global spread of coronavirus disease (COVID-19) led the World Health Organization to announce it as a pandemic on 12 March 2020 [7, 8]. The world has suffered a high toll from this pandemic regarding increased poverty, economic repercussions and human lives lost to date [9]. A considerable portion of the population is asymptomatic carriers for COVID-19. The most common symptoms include fever (83%), cough (82%) and shortness of breath (31%) [10]. Patients with COVID-19 also demonstrate ground-glass opacity and multiple mottling in patients with pneumonia in chest X-rays.
COVID-19 patients typically yield decreased eosinophils and lymphocyte counts, lower median haemoglobin values, and enhanced neutrophil counts, WBC and serum levels of ALT, AST, LDH and CRP [11]. For severe COVID-19 development, initial CRP serum levels have been considered as an independent predictor [12]. Although the lung is the main target of COVID-19 infection, the widespread distribution of ACE2 receptors in organs [13] may lead to gastrointestinal, liver, kidney, central nervous system, cardiovascular and ocular damage needs to be closely observed [14]. Patients with acute respiratory distress syndrome may deteriorate speedily and die of multiple organ failure [10] induced by the so-called cytokine storm. The severity of COVID-19 is also associated with elevation of D-dimer levels. The elevated D-dimer levels may reflect the risk of disseminated coagulopathy in patients with severe COVID-19, which may require anticoagulant therapy [15].
Early surveillance, contact tracing, testing and strict quarantine strategies have been used by many countries that maintained a low COVID-19 mortality rate [16,17,18]. Many of these countries had adopted digital technology to implement effective strategies and integrate them with healthcare delivery systems [19,20,21]. Pandemic plans are thorny to achieve manually but can be facilitated using digital health technology [22,23,24]. Early flattening of the incidence curve was possible in some countries like South Korea, which had integrated government-coordinated mitigation and containment processes into digital technology [25, 26]. UpCodeto utilized the data generated by the Singapore Ministry of Health to portray infection trends and recovery time [27]. The web-based platform HealthMap and COVID-19 dashboard of Johns Hopkins University provides an up-to-date scenario of COVID-19 deaths and cases across the world [28].
AI algorithms play a vital role in the integration of digital technology with healthcare [29,30,31,32]. For example, Shi et al. [33] analysed the characteristics, risk factors and outcomes for in-hospital mortality of COVID-19 patients with diabetes. They abstracted laboratory, clinical and demographic data of the patients and the risk factors associated with mortality were identified by performing multivariable Cox regression analyses. The outcomes of COVID-19 patients with diabetes were lower than age- and gender-matched patients without diabetes. Yadaw et al. [34] devised a useful prediction model of COVID-19 mortality utilizing unbiased computational techniques and detected the most predictive clinical features. Their machine learning (ML) framework was mainly based on three clinical features: minimum oxygen saturation throughout patients’ medical encounters, age and type of patient encounter. Their COVID-19 mortality prediction model exhibited a competitive accuracy. Although a number of studies have explored the association of mortality with clinical features of COVID-19, those studies did not provide a comprehensive list of clinical features associated with COVID-19 mortality. In addition, most of the predictive COVID-19 ML models were based on Chinese data; hence, it might not be relevant in other parts of the world. In this study, we tried to cover these two weaknesses of previous researches. We aimed to determine the set of clinical features associated with COVID-19 mortality in Iranian cases for the first-time using ML approaches.
2 Methods
In this section, the data collection process, the employed ML model and conducted statistical tests are presented. C4.5 decision tree is used as the ML model to predict whether a COVID-19 patient survives or not given his/her symptoms and medical conditions.
2.1 Study Settings, Population and Recruitments
We collected medical reports of all COVID-19 patients (n = 3008) who have been referred to Semnan hospital in Iran between March 2020 to November 2020. Data on sociodemographic features and clinical factors such as gender, age, number of months of infection and hospitalization, inpatient department, fever, myalgia, seizures and dizziness were investigated to determine their effects on the mortality of COVID-19 patients. All of the investigated features are categorical except age, blood pressure and oxygen saturation which are continuous. The dataset collection process has been done under the direct supervision of registered medical experts. Considering that data collection is error prone, samples with suspicious values were corrected if possible and discarded otherwise.
2.2 ML Models
In this research, C4.5 decision tree [35] is used for classification of patients. The C4.5 algorithm makes decisions using a set of training tree data. To do this, to create each node of the decision tree, C4.5 algorithm selects one of the features of training data that can more effectively partition the training samples. This selection is made based on the concept of entropy. Any attribute that can classify samples into purer categories is selected sooner. Then, the train dataset is categorized according to that attribute, and several branches are created. This process is repeated in each branch. If all the instances in the subcategory belong to a class, a leaf node is created for the decision tree and the class of those instances is specified, but if all the instances do not belong to a class and a new attribute cannot be selected for any reason, C4.5 creates a decision node using the expected value of the class. In addition, some dimension reduction algorithms such as PCA [36], PSL [37] and t-SNE [38] were used to show the samples according to important features. Dimension reduction is one of the major tasks for multivariate analysis. PCA as a linear dimension reduction algorithm is applied without considering the correlation between the dependent and the independent variables. However, PLS is applied based on the correlation. On the other hand, t-SNE algorithm estimates a similarity measure between pairs of samples in the high and the low dimensional spaces.
2.3 Ethics Approval
Local ethical committee of the Semnan University of Medical Sciences approved this research. The patients were informed about this research aims, and written consent was obtained before data collection.
2.4 Statistical and ML Analysis
We analysed the dataset features using MATLAB 2018b software. To determine difference between the two patient groups (i.e. alive and dead), Wilcoxon rank‐sum test [39] and Fisher’s exact test [40] were used for continuous and categorical data, respectively. The statistical significance of the two tests was set to P ≤ 0.05. In C4.5, the information gain was employed as the criterion to determine the attributes to be used as tree nodes. At each tree node, the attributes with minimum entropy were selected to form the children of that node. The number of children is equal to the number of possible values that the selected attribute can have. The size of each node \({N}_{i}\) is the number of examples in the sub-tree that has \({N}_{i}\) as its root. Only those nodes were split whose size was greater than or equal to the minimal size for split parameter. In our experiments, the split parameter was set to 4. For C4.5, the size of each leaf node (the number of examples in it) must be set as well. Finally, the last parameter that must be specified is the minimal gain. Only the nodes with gain greater than the minimal gain were considered for split operation. Increasing the minimal gain leads to fewer splits and smaller decision tree.
3 Results
Of the 3008 patients with COVID-19, 94.5% (2844) were of Iranian nationality and 5.5% (164 cases) were Afghan nationals. 56% were men, and 44% were women with an age average (± SD) 59.3 ± 18.7 years (1–100 years). In Fig. 1, the histogram of COVID-19 casualties for different age intervals has been shown. Of the patients who were referred to the hospital during this period, 18.5% were required to be admitted to the intensive care unit and the rest to the isolated and normal wards. Three hundred seventy-three of these 3008 cases were deceased. Three hundred eighty-seven patients (12.9%) with COVID-19 were in contact with the infected person, and 2621 patients (87.1%) declared any contact with the infected person. About 70.4% of patients referred to hospital personally, and 653 (21.7%) of them were conveyed to the hospital by pre-hospital emergency, 199 (6.6%) by private ambulance and 38 (1.3%) by ambulances from other centres.
Of the studied patients, 20 patients (0.7%) had a history of previous infection. Patients admitted to the hospital were associated with symptoms including 32.2% fever, 28% cough, 14% myalgia, 43.3% loss of consciousness, 0.8% loss of sense of smell, 0.5% loss of taste, 0.4% seizures, 4.6% headache, 1.6% dizziness, 0.4% paresis, 0.1% plague, 3.8% chest pain, 3.8% chills, 0.5% sweating, 0.5% dry throat and sore throat, 7.8% weakness and lethargy, 0.2% sputum excretion, 0.2% gastrointestinal bleeding, 2.3% abdominal pain, 5.4% Nausea, 3.8% vomiting, 2.9% diarrhoea and 4.4% anorexia. Other initial symptoms included haemoptysis (in 2 patients), oedema, restlessness, delirium, earache, constipation, palpitations, sudden loss of vision and haematuria (each in one case). Fifty cases (1.7%) were a smoker, and 70 cases (2.3%) were addicted to drugs. Two thousand seven hundred sixty-four patients underwent CT scan, of which 2277 had symptoms, and 244 did not undergo CT scan. One hundred seventy-eight patients (5.9%) needed mechanical ventilation at the beginning of the study, and the others did not. The average (± standard deviation) level of oxygen saturation at referral was 89.3% ± 7.4% (39–100%). 37.2% of patients had more than 93% oxygen saturation.
The number of patients’ respiration per minute were also measured in such a way that 0.3% (9 patients) did not breathe at all, 194 patients (6.4%) with 10–14 breaths, 1068 patients (35.5%) had 14–18 breaths, and 1296 patients (43.1%) showed 18–122 breaths per minute. Indeed, 353 patients (11.8%) had 22–28 breaths, and 88 patients (2.9%) had more than 28 breaths per minute. The average (± SD) of patients’ body temperature at the time of referral was 37.1 ± 0 0.7 °C [35,36,37,38,39,40]. 21.8% of patients had a fever at the time of referral.
The average (± SD) duration of symptoms until referral was 4.7 ± 13.9 days. In these patients, 1670 patients (55.5%) had risk factors or underlying diseases, so that 104 patients (3.5%) had cancer, 16 patients (0.5%) had liver disease, 588 patients (19.5%) with diabetes, 39 (1.3%) with chronic haematological diseases, 15 (0.5%) with immunodeficiency, 586 patients (19.5%) with cardiovascular diseases, 177 patients (5.9%) with kidney diseases, 108 patients (3.6%) with asthma, 99 patients (3.3%) with chronic lung diseases, 127 patients (4.2%) with neurological diseases, 695 patients (23.1%) with hypertension, 26 patients (0.8%) with CVA and stroke, 8 patients (0.2%) with neurosurgery-related problems, 28 patients (0.9%) with hypothyroidism, 43 patients (1.4%) with other neurological diseases, 42 patients (1.3%) with hyperlipidaemia, 15 patients (0.4%) with prostate, 43 patients (1.4%) with psychological diseases, 10 patients (0.3%) with history of veteran chemical warfare and 24 patients (0.7%) had anaemia. Out of 177 patients with kidney disease, 77 were on dialysis.
One thousand three hundred thirty-eight patients (44.5%) had no risk factor and underlying disease. Eight hundred twenty-three (27.4%) and 567 (18.8%) patients had one and two risk factors, respectively. Three and four risk factors were observed in 218 (7.2%) and 52 cases (1.7%), respectively. Nine (0.3%) and one patient (0.05%) had five and six risk factors, respectively. Among 3008 investigated patients, 112 (3.7%) were hospitalized, 2523 (83.9%) were discharged, and also 373 (12.4%) died. The average (± SD) duration of hospitalization was 6.17 ± 6.3 days (1–87 days), of which 236 patients (7.8%) did not need hospitalization, and 2154 patients (71.6%) required 1–7 days of hospitalization. Three hundred seventy-six cases (12.5%) 8–14 days, 137 cases (4.6%) 15–21 days, 59 cases (2%) 22–28 days and 16 cases (0.5%) more than 28 days were hospitalized.
According to these data, the prevalence of COVID-19 infection was high in March 2020 and then had the lowest incidence in May and June and finally reached its peak in October and was associated with the fewer incidence in November (Fig. 2).
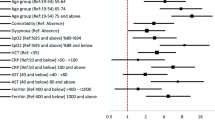
3.1 The Effect of Early Symptoms on the Outcome of Patients’ Deaths
Table 1 shows the effect of different features on the mortality rate. Mortality was not significantly different between men (1684 cases) and women (1324 cases). There was a significant correlation between mortality and age of patients (P < 0.001), infection time (P < 0.001) and the hospitalization ward (isolated ward, intensive care unit, normal ward) (P < 0.001). Symptoms such as fever, myalgia, dizziness, seizure, abdominal pain, nausea, vomiting, diarrhoea and anorexia were occurred without having mortality related to COVID-19 (P > 0.05). There was a significant association between mortality and headache in infected patients (P < 0.011). Chest pain was also associated significantly with COVID-19-related mortality (P < 0.045). Decreased level of consciousness was also significantly associated with COVID-19-related mortality (P < 0.0001). Respiratory distress, oxygen saturation less than 93%, lower respiratory rate and need for mechanical ventilation were associated with COVID-19-related mortality (P < 0.004, P < 0.001, P < 0.001 and P < 0.001, respectively).
Opium addiction, smoking status, pregnancy, diabetes mellitus, underlying cancer, liver disease, lung disease, asthma, kidney disease, chronic haematological diseases, other chronic diseases and receiving immunosuppressive medicines had no association with COVID-19-related mortality. Underlying cardiovascular disease and neurological diseases were associated with COVID-19-related mortality (P < 0.023, P < 0.003 and P < 0.012, respectively). The presence of CT scan symptoms was significantly related to mortality in COVID-19 cases (P < 0.001). Having a risk factor was significantly correlated with mortality due to COVID-19 (P < 0.003). Having multiple risk factors was significantly correlated with mortality of COVID-19 (P < 0.002). The statistical test results presented above reveal the symptoms with significant relation to COVID-19 mortality. These symptoms can be used as features to form a decision tree for COVID-19 diagnosis. An example of these types of decision trees is shown in Fig. 3. The results of evaluating the prepared decision tree on our dataset are available in Table 2. The evaluation was done based on accuracy [41], sensitivity [42], specificity [43], precision [44] and F1-score [45]. In Fig. 4, the patients are shown according to their important features extracted by PCA, PSL and t-SNE algorithms. According to this figure, although PCA has better performance, it is clear that the cases are not separable well.
4 Discussion
The main findings of our study are the significant association of mortality due to COVID-19 with factors such as age, headache, chest pain, low respiratory rate, oxygen saturation less than 93%, need to a mechanical ventilator, having symptoms on CT, hospitalization in wards and time to infection. Besides, neurological disorders, cardiovascular diseases and having risk factor(s) were associated with COVID-19 mortality. Interestingly, there was no significant association between mortality and gender, fever, myalgia, dizziness, seizure, abdominal pain, nausea, vomiting, diarrhoea and anorexia. As another contribution, this paper is the first to investigate the association of history of neurological disorders, having risk factor(s), dizziness, seizure and abdominal pain with COVID-19-related mortality.
The significant association between age and COVID-19-related mortality in our study is in line with previous studies conducted by Zhou et al. [46], Pettit et al. [47], Chen et al.[48] and Iftime et al. [49] and in contrast to De Smet et al. [50], Sun et al. [51] and Li et al. [52]. Immune impairment and the enhanced possibility of developing cardiovascular and respiratory diseases would be the joint linkage between old age and COVID-19-related mortality [53, 54]. The observed association between the underlying cardiovascular diseases and COVID-19-related mortality in our study was in line with Chen et al. [55], Soares et al. [56] and Ruan et al. [57], but was contrary to Iftimie et al. [58], Li et al. [59] and Ciardullo et al. [60] findings. We found underlying high blood pressure to be associated with COVID-19 mortality, which is in line with Li et al. [59] finding and is in contrast with Rawl et al. [61], Pei et al. [62], Sun et al. [51] and Ciardullo et al. [60] findings. Hospitalization in wards was associated with COVID-19-related mortality, parallel with Chen et al. [59] findings, who found a relationship between ICU admission and mortality. The association between the need for mechanical ventilation and COVID-19-related mortality is in line with Chen et al. [59] and Zhou et al. [46] findings. The association between low oxygen saturation and low respiratory rate with mortality was in contrast with Sun et al. [51] findings.
In our previous study, anorexia, dry cough, anosmia and history of cancer were associated with COVID-19-related mortality [63], but in this study, we observed no relationship between mortality of COVID-19 and cancer that may be due to different populations of the study: two other provinces from one country. Anorexia showed a significant positive relationship with COVID-19-related mortality by Rawl et al. [61]. Regarding comorbidities, finding no significant association between cancer and COVID-19-related mortality is in line with Lee et al. [64] findings but is in contrast with Iftimie et al. [49], Mehta et al. [65], Dai et al. [66], Westblade et al. [67], Melo et al. [68] and Rüthrich et al. [69] findings. Different demographic features could explain this discrepancy. Finding no association between gender and COVID-19-related mortality is the same as Ruan et al. [57], Mehta et al. [65] and Sun et al. [51]. Absence of association between fever and COVID-19-related mortality in our study is the same as our previous research [63], but it contrasts with the findings of Iftime et al. [49]. Myalgia, diarrhoea, nausea and vomiting were not predictors of mortality in our cohort, which contrast with Zhou et al. [46] findings. Some of the typical clinical characteristics of COVID-19 patients with mortality was summarized in Table 3.
The most important strength of this research is investigating impact of some new features on mortality rate of COVID-19 patients. Another important strength of this research is the large amount of data used. However, our results should be interpreted with the following weaknesses. The patients were recruited from a specific region, and our results might not apply in other countries as factors associated with mortality may differ in various regions [70]. Future research is necessary to investigate mortality rate of COVID-19 in patients with heart or kidney diseases with long-term follow-ups.
5 Conclusion
In this research, we investigated the effect of some of the risk factors and symptoms of COVID-19 mortality rate for the first time. Our results show a significant association between mortality and risk factors like old age, headache, chest pain, low respiratory rate, oxygen saturation less than 93%, need to a mechanical ventilator, having symptoms on CT, hospitalization in wards, time to infection, neurological disorders, cardiovascular diseases and having a risk factor or multiple risk factors. In contrast, there is no significant association between mortality and gender, fever, myalgia, dizziness, seizure, abdominal pain, nausea, vomiting, diarrhoea and anorexia. More studies are needed to confirm these findings.
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
Code Availability
Not applicable.
References
Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W et al (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579(7798):270–273
Goldberg D (2010) Critical reviews in clinical laboratory sciences. Crit Rev Clin Lab Sci 47(1):1–4
Sharifrazi D, Alizadehsani R, Roshanzamir M, Joloudari JH, Shoeibi A, Jafari M et al (2021) Fusion of convolution neural network, support vector machine and Sobel filter for accurate detection of COVID-19 patients using X-ray images. Biomed Signal Process Control 68:102622
Alizadehsani R, Sharifrazi D, Izadi NH, Joloudari JH, Shoeibi A, Gorriz JM et al (2021) Uncertainty-aware semi-supervised method using large unlabeled and limited labeled COVID-19 data. ACM Transactions on Multimedia Computing, Communications, and Applications (TOMM) 17(3s):1–24
Joloudari JH, Azizi F, Nodehi I, Nematollahi MA, Kamrannejhad F, Mosavi A et al (2021) DNN-GFE: a deep neural network model combined with global feature extractor for COVID-19 diagnosis based on CT scan images. EasyChair; Report No.: 2516–2314
Ayoobi N, Sharifrazi D, Alizadehsani R, Shoeibi A, Gorriz JM, Moosaei H et al (2021) Time series forecasting of new cases and new deaths rate for COVID-19 using deep learning methods. Results in Physics 27:104495
Khozeimeh F, Sharifrazi D, Izadi NH, Joloudari JH, Shoeibi A, Alizadehsani R et al (2021) Combining a convolutional neural network with autoencoders to predict the survival chance of COVID-19 patients. Sci Rep 11(1):1–18
Shoeibi A, Khodatars M, Alizadehsani R, Ghassemi N, Jafari M, Moridian P et al (2020) Automated detection and forecasting of COVID-19 using deep learning techniques: a review. Preprint at arXiv:200710785
Nasab RZ, Ghamsari MRE, Argha A, Macphillamy C, Beheshti A, Alizadehsani R et al (2022) Deep learning in spatially resolved transcriptomics: a comprehensive technical view. Preprint at arXiv:221004453
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan. China Jama 323(11):1061–1069
Lippi G, Plebani M (2020) The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks. Clin Chem Lab Med (CCLM) 58(7):1063–1069
Bhargava A, Fukushima EA, Levine M, Zhao W, Tanveer F, Szpunar SM et al (2020) Predictors for severe COVID-19 infection. Clin Infect Dis 71(8):1962–1968
Hamming I, Timens W, Bulthuis M, Lely A, Navis G, van Goor H (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 203(2):631–7
Renu K, Prasanna PL, Valsala GA (2020) Coronaviruses pathogenesis, comorbidities and multi-organ damage – a review. Life Sci 255:117839
Lippi G, Favaloro EJ (2020) D-dimer is associated with severity of coronavirus disease 2019: a pooled analysis. Thromb Haemost 120(5):876–878
Whitelaw S, Mamas MA, Topol E, Van Spall HGC (2020) Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit Health 2(8):e435–e440
Alizadehsani R, Eskandarian R, Behjati M, Zahmatkesh M, Roshanzamir M, Izadi NH et al (2022) Factors associated with mortality in hospitalized cardiovascular disease patients infected with COVID-19. Immun Inflamm Dis 10(3):e561
Asgharnezhad H, Shamsi A, Alizadehsani R, Khosravi A, Nahavandi S, Sani ZA et al (2022) Objective evaluation of deep uncertainty predictions for COVID-19 detection. Sci Rep 12(1):1–11
Alizadehsani R, Hosseini MJ, Boghrati R, Ghandeharioun A, Khozeimeh F, Sani ZA (2012) Exerting cost-sensitive and feature creation algorithms for coronary artery disease diagnosis. Int J Knowl Discov Bioinform (IJKDB) 3(1):59–79
Nahavandi D, Alizadehsani R, Khosravi A, Acharya UR (2022) Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput Methods Programs Biomed 213:106541
Sharifrazi D, Alizadehsani R, Joloudari JH, Shamshirband S, Hussain S, Sani ZA et al (2020) CNN-KCL: Automatic myocarditis diagnosis using convolutional neural network combined with k-means clustering. Math Biosci Eng 19(3):2381–2402
Joloudari JH, Alizadehsani R, Nodehi I, Mojrian S, Fazl F, Shirkharkolaie SK et al (2022) Resource allocation optimization using artificial intelligence methods in various computing paradigms: A Review. Preprint at arXiv:220312315
Joloudari JH, Mojrian S, Nodehi I, Mashmool A, Zadegan ZK, Shirkharkolaie SK et al (2022) Application of artificial intelligence techniques for automated detection of myocardial infarction: a review. Physiol Meas 43(8):08TR01
Joloudari JH, Saadatfar H, GhasemiGol M, Alizadehsani R, Sani ZA, Hasanzadeh F et al (2022) FCM-DNN: diagnosing coronary artery disease by deep accuracy fuzzy C-means clustering model. Preprint at arXiv:220204645
Halpern NA, Tan KS. Society of critical care medicine. US ICU availability for COVID-19. https://sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-U. Accessed 22 Dec 2020
Shoeibi A, Moridian P, Khodatars M, Ghassemi N, Jafari M, Alizadehsani R et al (2022) An overview of deep learning techniques for epileptic seizures detection and prediction based on neuroimaging modalities: methods, challenges, and future works. Comput Biol Med 106053
Dick S. News National. Singapore’s coronavirus temperature screening and tracking are leading the way. https://thenewdaily.com.au/news/national/2020/03/19/singapore-coronavirus-temperature-scans/. Accessed 22 Dec 2020
McCall B (2020) COVID-19 and artificial intelligence: protecting health-care workers and curbing the spread. Lancet Digit Health 2(4):e166–e167
Jafari M, Shoeibi A, Ghassemi N, Heras J, Khosravi A, Ling SH et al (2022) Automatic diagnosis of myocarditis disease in cardiac MRI modality using deep transformers and explainable artificial intelligence. Preprint at arXiv:221014611
Moridian P, Shoeibi A, Khodatars M, Jafari M, Pachori RB, Khadem A et al (2022) Automatic diagnosis of sleep apnea from biomedical signals using artificial intelligence techniques: methods, challenges, and future works. Wiley Interdiscip Rev: Data Min Knowl Discov e1478
Khozeimeh F, Sharifrazi D, Izadi NH, Joloudari JH, Shoeibi A, Alizadehsani R et al (2022) RF-CNN-F: random forest with convolutional neural network features for coronary artery disease diagnosis based on cardiac magnetic resonance. Sci Rep 12(1):1–12
Kakhi K, Alizadehsani R, Kabir HD, Khosravi A, Nahavandi S, Acharya UR (2022) The internet of medical things and artificial intelligence: trends, challenges, and opportunities. Biocybern Biomed Eng 42(3):749–771
Shi Q, Zhang X, Jiang F, Zhang X, Hu N, Bimu C et al (2020) Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care 43(7):1382–1391
Yadaw AS, Li Y-c, Bose S, Iyengar R, Bunyavanich S, Pandey G (2020) Clinical features of COVID-19 mortality: development and validation of a clinical prediction model. Lancet Digit Health 2(10):e516-e25
Joloudari JH, Hussain S, Nematollahi MA, Bagheri R, Fazl F, Alizadehsani R et al (2022) BERT-deep CNN: state-of-the-art for sentiment analysis of COVID-19 tweets. Preprint at arXiv:221109733
Roshanzamir M, Alizadehsani R, Roshanzamir M, Shoeibi A, Gorriz JM, Khosrave A et al (2021) What happens in Face during a facial expression? Using data mining techniques to analyze facial expression motion vectors. Preprint at arXiv:210905457
Sharifrazi D, Alizadehsani R, Hoseini Izadi N, Roshanzamir M, Shoeibi A, Khozeimeh F et al (2021) Hypertrophic cardiomyopathy diagnosis based on cardiovascular magnetic resonance using deep learning techniques. Lancet. https://doi.org/10.2139/ssrn.3855445
Van der Maaten L, Hinton G (2008) Visualizing data using t-SNE. J Mach Learn Res 9(11):2579–2605
Steel RG (1960) A rank sum test for comparing all pairs of treatments. Technometrics 2(2):197–207
Connelly LM (2016) Fisher’s exact test. Medsurg Nurs 25(1):58–60
Iqbal MS, Ahmad W, Alizadehsani R, Hussain S, Rehman R (eds) (2022) Breast Cancer Dataset, Classification and Detection Using Deep Learning. Healthcare: MDPI Healthcare: MDPI 10(12):2395
Khalili H, Rismani M, Nematollahi MA, Masoudi MS, Asadollahi A, Taheri R et al (2022) Survival prediction in traumatic brain injury patients using machine learning algorithms. Sci Rep 13:960
Sadeghi D, Shoeibi A, Ghassemi N, Moridian P, Khadem A, Alizadehsani R et al (2022) An overview of artificial intelligence techniques for diagnosis of schizophrenia based on magnetic resonance imaging modalities: Methods, challenges, and future works. Comput Biol Med 105554
Kiss N, Steer B, de van der Schueren M, Loeliger J, Alizadehsani R, Edbrooke L et al (2022) Comparison of the prevalence of 21 GLIM phenotypic and etiologic criteria combinations and association with 30-day outcomes in people with cancer: a retrospective observational study. Clin Nutr 41(5):1102–11
Shoeibi A, Sadeghi D, Moridian P, Ghassemi N, Heras J, Alizadehsani R et al (2021) Automatic diagnosis of schizophrenia in EEG signals using CNN-LSTM models. Front Neuroinform 15:777977
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062
Pettit NN, MacKenzie EL, Ridgway JP, Pursell K, Ash D, Patel B et al (2020) Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19. Obesity 28(10):1806–1810
Chen R, Liang W, Jiang M, Guan W, Zhan C, Wang T et al (2020) Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 158(1):97–105
Iftimie S, López-Azcona AF, Vicente-Miralles M, Descarrega-Reina R, Hernández-Aguilera A, Riu F et al (2020) Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. PloS one 15(9):e0234452
De Smet R, Mellaerts B, Vandewinckele H, Lybeert P, Frans E, Ombelet S et al (2020) Frailty and mortality in hospitalized older adults with COVID-19: retrospective observational study. J Am Med Dir Assoc 21(7):928–32.e1
Sun H, Ning R, Tao Y, Yu C, Deng X, Zhao C et al (2020) Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: a retrospective study. J Am Geriatr Soc 68(6):E19–E23
Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y et al (2020) Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol 146(1):110–118
Nasirzadeh A, Jafarzadeh Maivan MH., Bazeli J, Hajavi J, Yavarmanesh N, Zahedi M, Abounoori M, Razavi A, Maddah MM, Mortazavi P, Moradi M, Heidarzadeh S, Mardaneh J, Shoeibi A, Alizadehsani R, Islam SMS (2021) Inhibiting IL-6 during cytokine storm in COVID-19: Potential role of natural products. Preprints, pp 1–21, 2021060131. https://doi.org/10.20944/preprints202106.0131.v1
Mardaneh J, Nasirzadeh A, Bazeli J, Hajavi J, Zahedi M, Abounoori M, Razavi A, Maddah MM, Mortazavi P, Moradi M, Salehi F, Heidarzadeh S, Jafarzadeh Maivan H, Shoeibi A, Alizadehsani R, Islam SMS (2021) Inhibiting NF-?B during cytokine storm in COVID-19: Potential role of natural products as a promising therapeutic approach. Preprints pp, 1–35, 2021060130. https://doi.org/10.20944/preprints202106.0130.v1
Chen R, Liang W, Jiang M, Guan W, Zhan C, Wang T et al (2020) Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 158(1):97–105
Soares RdCM, Mattos LR, Raposo LM (2020) Risk factors for hospitalization and mortality due to COVID-19 in Espírito Santo State Brazil. Am J Trop Med Hyg 103(3):1184–90
Ruan Q, Yang K, Wang W, Jiang L, Song J (2020) Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan. China Intensive Care Medicine 46(5):846–848
Iftime S, López-Azcona AF, Vicente-Miralles M, Descarrega-Reina R, Hernández-Aguilera A, Riu F et al (2020) Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. bioRxiv
Chen J, Bai H, Liu J, Chen G, Liao Q, Yang J et al (2020) Distinct clinical characteristics and risk factors for mortality in female inpatients with coronavirus disease 2019 (COVID-19): a sex-stratified, large-scale cohort study in Wuhan. China Clinical Infectious Diseases 71(12):3188–3195
Ciardullo S, Zerbini F, Perra S, Muraca E, Cannistraci R, Lauriola M et al (2020) Impact of diabetes on COVID-19-related in-hospital mortality: a retrospective study from Northern Italy. J Endocrinol 44:843–885
Rawle MJ, Bertfield DL, Brill SE (2020) Atypical presentations of COVID-19 in care home residents presenting to secondary care: a UK single centre study. Aging Medicine 3(4):237–244
Pei G, Zhang Z, Peng J, Liu L, Zhang C, Yu C et al (2020) Renal involvement and early prognosis in patients with COVID-19 pneumonia. J Am Soc Nephrol 31(6):1157
Alizadehsani R, Alizadeh Sani Z, Behjati M, Roshanzamir Z, Hussain S, Abedini N et al (2021) Risk factors prediction, clinical outcomes, and mortality in COVID-19 patients. J Med Virol 93(4):2307–2320
Lee LYW, Cazier J-B, Starkey T, Briggs SEW, Arnold R, Bisht V et al (2020) COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol 21(10):1309–1316
Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A et al (2020) Case fatality rate of cancer patients with COVID-19 in a New York Hospital System. Cancer Discov 10(7):935–941
Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z et al (2020) Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov 10(6):783–791
Westblade LF, Brar G, Pinheiro LC, Paidoussis D, Rajan M, Martin P et al (2020) SARS-CoV-2 viral load predicts mortality in patients with and without cancer who are hospitalized with COVID-19. Cancer Cell 38(5):661–71.e2
de Melo AC, Thuler LC, da Silva JL, de Albuquerque LZ, Pecego AC, Rodrigues LdO et al (2020) Cancer inpatients with COVID-19: a report from the Brazilian National Cancer Institute. PloS one 15(10):e0241261
Rüthrich MM, Giessen-Jung C, Borgmann S, Classen AY, Dolff S, Grüner B et al (2021) COVID-19 in cancer patients: clinical characteristics and outcome—an analysis of the LEOSS registry. Ann Hematol 100(2):383–393
Alizadehsani R, Khosravi A, Roshanzamir M, Abdar M, Sarrafzadegan N, Shafie D et al (2020) Coronary artery disease detection using artificial intelligence techniques: a survey of trends, geographical differences and diagnostic features 1991–2020. Comput Biol Med 104095
Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A (2021) The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol 93(2):1045–1056
Magfira N, Helda H (2020) Correlation between adult tobacco smoking prevalence and mortality of Coronavirus Disease-19 across the world. Comput Biol Med 128:104095
Mendy A, Apewokin S, Wells AA, Morrow AL (2020) Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 patients. medRxiv. 2020.06.25.20137323
Poloni TE, Carlos AF, Cairati M, Cutaia C, Medici V, Marelli E et al (2020) Prevalence and prognostic value of delirium as the initial presentation of COVID-19 in the elderly with dementia: an Italian retrospective study. EClinicalMedicine 26:100490
Hue S, Beldi-Ferchiou A, Bendib I, Surenaud M, Fourati S, Frapard T et al (2020) Uncontrolled innate and impaired adaptive immune responses in patients with COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med 202(11):1509–1519
Chen Q, Zheng Z, Zhang C (2020) Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou. Infection 48(4):543–551
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ et al (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75(7):1730–41
Homayounieh F, Zhang EW, Babaei R, Karimi Mobin H, Sharifian M, Mohseni I et al (2020) Clinical and imaging features predict mortality in COVID-19 infection in Iran. PLoS ONE 15(9):e0239519
Sorouri M, Kasaeian A, Mojtabavi H, Radmard AR, Kolahdoozan S, Anushiravani A et al (2020) Clinical characteristics, outcomes, and risk factors for mortality in hospitalized patients with COVID-19 and cancer history: a propensity score-matched study. Infect. Agents Cancer 15(1):74
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. SMSI is funded by the National Heart Foundation of Australia (102112) and a National Health and Medical Research Council (NHMRC) Emerging Leadership Fellowship (APP1195406).
Author information
Authors and Affiliations
Contributions
Contributed to prepare the first draft: R.A., M.T.D., M.B., M.R., A.S., F.K. and K.K. Contributed to editing the final draft: S.N., Z.A.S., A.K., S.M.S.I., R.L, J.H.J and R.E. Contributed to all analysis of the data and produced the results accordingly: M.Z., S.M.S.I, A.H., M.R., K.K., S.N., M.T.D. and R.A. Searched for papers and then extracted data: S.H., A.S., M.T.D., M.B., Z.A.S., A.K., R.E. and F.K. Conception or design of the work: S.N., Z.A.S., A.K., S.M.S.I., K.K. and R.E.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Semnan Hospital Ethics Committee.
Consent to Participate
All the patients completed written consent forms before their enrolment in the data collection procedure.
Consent for Publication
The signed consent to publish gives the publisher the permission of the author to publish the work.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eskandarian, R., Alizadehsani, R., Behjati, M. et al. Identification of Clinical Features Associated with Mortality in COVID-19 Patients. Oper. Res. Forum 4, 16 (2023). https://doi.org/10.1007/s43069-022-00191-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43069-022-00191-3