Abstract
Endometriosis is one of the gynecological diseases where women suffer from pain, quality of life decreased. The aim of this review was to describe the most common non-medical methods used in the treatment of symptoms associated with endometriosis and to determine their effectiveness. The review was performed in PubMed, Embase and Web of Science databases. Randomized controlled trials, case studies, observational studies, retrospective studies, prospective studies, pilot studies, trails, publications in English or Polish were searched based on the Participant-Intervention-Comparator-Outcomes-Study design (PICOS) format. The criteria used to select studies were: women with endometriosis, no cancer, included any physiotherapeutic or non-medical intervention. 3706 articles were found, however only 26 met the inclusion criteria and were included in the review. Quality of the studies was assessed by Risk of Bias 2 tool and ROBINS-1 tool. The most holistic approach used in the treatment of symptoms of endometriosis include physical therapy, manual therapy, electrophysical agents acupuncture, diet and psychological interventions. Most research has focused on relieving pain and increasing quality of life. Non-medical methods showed reduction of symptoms of endometriosis. Physical activity, manual therapy, electrophysical agents, acupuncture, diet and cognitive behavioral therapy showed no negative side effects and reduced pain, what improved the quality of life and reduced the perceived stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis is a gynecological condition characterized by the presence of estrogen-sensitive tissue resembling the endometrium found outside the uterus [1]. Endometrial glands are typically observed in the pelvic region, including the ovaries, ligaments, peritoneum, intestines, bladder, lymph nodes, and even the lungs, diaphragm, or pericardium [2, 3]. It is estimated that approximately 15% of women of reproductive age experience endometriosis [4]. However, diagnostic difficulties and variations in prevalence across different populations may disturb the correct result of the frequency of this disease [5].
Symptoms of endometriosis vary widely. Some women may remain asymptomatic for years, while others may experience painful menstruation, intermenstrual bleeding, infertility, urinary issues, painful intercourse, painful bowel movements, diarrhoea, or non-menstrual abdominal pain [2, 6, 7]. Nevertheless, the predominant symptom is pain, which can be nociceptive, inflammatory or neuropathic [8]. Chronic pain can lead to central sensitization, which makes pain management difficult, which is noticeable in the population of women with endometriosis [9].
The pain associated with endometriosis involves a complex interplay between peripheral nerve conduction, the peritoneum, and the central nervous system. Increased presence of small unmyelinated nerve fibers and neurotrophic factors near endometriotic lesions suggests their role in pain development. Furthermore, ongoing inflammatory processes cause the release of pro-inflammatory molecules by sensory fibers, which also contributes to increased pain perception. Nerve fiber sensitization due to the pro-inflammatory environment increases pain sensitivity. An impaired immune response to endometrial cells and tissues in patients with endometriosis may contribute to the growth and attachment of endometrial cells, which further worsens pain [8, 10, 11].
Aside from diminishing quality of life, pain contributes to myofascial changes, leading to improper body posture, weakened trunk muscle function, altered spine curvature, and decreased lung function [12, 13]. Patients with endometriosis exhibit thinner abdominal wall muscles, decreased lumbopelvic stability and less resistance in trunk flexor and extensor muscles [14]. Incorrect body posture affects the pelvic floor as well, manifesting as pelvic floor hyperactivity among women with endometriosis, resulting in sexual dysfunction and other pelvic floor dysfunctions like urinary incontinence or constipation [15].
The primary objective of non-medical methods in managing endometriosis is pain relief and pelvic floor function improvement [16], along with post-surgical support [17]. This techniques aim to relax muscles, reduce inflammation, and disrupt the pain cycle, ultimately enhancing quality of life [18]. The aim of this review was to describe the most common physiotherapeutic and non-medical methods used in the treatment of symptoms associated with endometriosis and to determine their effectiveness.
Materials and Methods
The study protocol was prepared following the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) [19]. The research protocol has been approved by PROSPERO no. CRD42023389400 “Physiotherapy in endometriosis - as an effective method of supporting traditional treatment: a systematic review.“ Inclusion criteria were formulated based on the Participant-Intervention-Comparator-Outcomes-Study design (PICOS) format.
Participants: women with endometriosis, no cancer.
Intervention: any physiotherapeutic or non-medical intervention (exercise, manual therapy, physical therapy, diet, psychologic intervention).
Comparasion: no intervention, placebo.
Outcomes: therapy effectiveness assessment, quality of life, pain, pelvic floor, sex life, muscle function.
Study design: studies in Polish and English, no time limit, pilot study, randomized control trial, prospective study, retrospective study, observational study.
The search process involved four researchers independently scouring databases including Medline-Pub Med, Embase, and Web of Science. The following phrase was used to search for articles: endometriosis and (physiotherapy or rehabilitation or electrotherapy or electrophysical agents or exercise or yoga or visceral therapy or acupuncture or manual therapy or physical therapy or massage or trigger points or breathing or biopsychosocial or mindfulness or relaxation or complementary therapy or holistic approach).
Titles and abstracts were initially screened for relevance, with subsequent inclusion of studies addressing endometriosis symptoms such as pain, quality of life, physical function, and infertility. Exclusion criteria comprised studies not published in English or Polish, those describing surgical procedures or animal models, and those involving pediatric or male populations, or primarily mathematical analyses. Discrepancies in study selection were resolved through consensus.
After initial screening, full-text versions of selected articles were obtained and scrutinized for study type, participant demographics, intervention details, outcome assessment methods, questionnaires utilized, and main findings, ensuring alignment with inclusion criteria.
Risk of bias assessment was conducted independently by two researchers using the Risk of Bias 2 tool [20] for randomized studies and ROBINS-I [21] for non-randomized trials, evaluating various domains such as randomization process, handling of missing data, intervention adherence, outcome measurement, and reporting integrity to determine overall study risk levels.
Results
Characteristics of the Studies
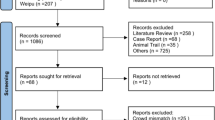
Based on the phrases presented, a total of 3706 works were found. After removing duplicates, 2839 works remained. After analyzing the titles and abstracts, 2770 works were rejected. There were 69 works left to be fully read. 26 works met the final inclusion criteria. A detailed analysis of the individual stages of the review is presented in the PRISMA diagram (Fig. 1).
The studies included into the analysis assess pain (19 studies), quality of life (17 studies), mental health (9 studies), stress (6 studies), dyspareunia (7 studies) among women with endometriosis. The physiotherapeutic interventions that have been described are: physical activity, manual therapy, acupuncture, and physical therapy. The characteristics of the studies included in the review are presented in Table 1.
Risk of Bias of fifteen studies were assessed using RoB 2 tool. Eight studies were assessed as low risk of bias, then seven studies were assessed by moderate risk of bias. Eleven studies were assessed using ROBINS-I tool. Four studies have low risk of bias, seven studies have moderate risk of bias. See Fig. 2; Table 2.
Physical Activity in the Treatment of Endometrial Symptoms
According to Piggin [48], ‘physical activity involves people moving, acting and performing within culturally specific spaces and contexts, and influenced by a unique array of interests, emotions, ideas, instructions and relationships.’ Research on physical activity (PA) among women with endometriosis focuses on alleviating the side effects of drugs and reducing pain while improving quality of life. PA utilized in treating endometriosis symptoms includes breathing exercises, yoga, Pilates, muscle relaxation, and aerobic activities.
Armour et al. [25] estimated that exercises, yoga, Pilates, stretching, and breathing were among the self-management strategies adopted by women with endometriosis. However, women rated these interventions as less effective in reducing pain compared to cannabis, heat, diet, or acupressure. Nonetheless, physical interventions reduced pain on average from 4.5 to 4.9 points on a 0–10 scale (0 being ineffective; 10 being extremely effective). Conversely, after engaging in physical activity, women reported increased pelvic pain (especially cramp pain) and fatigue, particularly after Pilates practice [25].
One of the mind-practice activities is yoga, which integrates meditation, physical exercises, and breathing techniques. Two-hour yoga sessions twice a week in women with endometriosis reduced pain and improved quality of life; however, yoga did not affect or decrease menstrual blood flow [22]. It was emphasized that yoga techniques, particularly breathing exercises, were beneficial in coping with pain, leading to reduced reliance on painkillers. Yoga also fostered self-control, self-awareness, autonomy, improved sleep, better management of panic attacks, and increased self-confidence [23]. Ten sessions combining breathing exercises, individualized stretching and strengthening exercises, massage, transcutaneous electrical nerve stimulation, and psychological intervention reduced salivary cortisol levels, thereby decreasing perceived stress levels and enhancing quality of life [24].
Many women use pharmacotherapy to alleviate pain, which may have side effects. PA may play a role in mitigating these effects. Three 30-minute brisk walking sessions and two 1-hour aerobic training sessions per week reduce bone density loss among women with endometriosis undergoing pharmacological treatment with gonadotropin-releasing hormone [26]. Pharmacological treatment can be complemented by progressive muscle relaxation to reduce pain and the side effects of hormone treatment. After 12 weeks, attending group classes twice a week with Jacobson’s relaxation concept and home practice significantly improved overall quality of life [28].
PA is often chosen as a self-management strategy for addressing endometriosis symptoms. It enhances quality of life, reduces pain, and mitigates the effects of pharmacological treatment. The characteristics of studies elucidating the effectiveness of physical activity in treating endometriosis symptoms are presented in Table 3.
Manual Therapy in the Treatment of Endometrial Symptoms
Manual therapy, a treatment method employed by physical therapists, involves a hands-on approach. It encompasses techniques such as joint and soft tissue mobilization, stretching, and acupressure, which have the potential to alleviate pain [49].
Muñoz-Gómez et al. [37] performed comprehensive techniques, including spinal and sacroiliac manipulation, mobilization of the abdominal and broad ligaments, and pelvic diaphragm release. Their manual therapy intervention resulted in a 30.76% reduction in pain after six weeks and led to improvements in control, powerlessness, and emotional well-being among women with endometriosis [37]. Many women with endometriosis have increased pelvic floor muscle tone [30] and adhesions [31]. Some manual techniques can reduce tissue thickening and adhesion, leading to improved mobility in the area, as well as reducing pain, improving quality of life, dyspareunia and dysmenorrchea, as confirmed by Wurn et al. [31]. Certain manual techniques have been shown to decrease tissue thickening and adhesions, thereby enhancing mobility and reducing pain, improving quality of life, dyspareunia, and dysmenorrhea, as confirmed by Wurn et al. [31]. Their intensive therapy sessions, initially lasting 2 h per week for 5 months and progressing to sessions lasting up to 4 h per day for 5 days, resulted in improvements in menstrual cycle, dysmenorrhea, and dyspareunia [31]. Manual therapy can be supported by 3D/4D transperineal ultrasound to precisely identify areas of increased tension and abnormal muscle function [30]. Del Forno et al. [30] performed five 30-minutes session of Thiele massage, supported by 3D/4D transperineal ultrasound, involving stretching and acupressure of the pelvic floor muscles to restore normal tone and induce relaxation. This therapy led to improvements in the Levator Hiatus Area and reductions in both deep and superficial dyspareunia [30]. Additionally, improvements in superficial dyspareunia, chronic pelvic pain, and pelvic floor muscle relaxation were observed after Thiele massage, although del Forno et al. [41] did not confirmed effects on urinary, bowel and sexual function [41]. Another type of manual therapy is Osteopathic Manipulative Therapy (OMT). Darai et al. [29] showed that approximately 1-hour OMT of the mobilisation of uterus, colon, the peritoneum and around the vertebrae L1 and L2 improved physical and mental quality of life women with endometriosis [29]. As well as osteopathic mobilisation of sacroiliac joints, diaphragm, abdominal organ, temporomandibular joints and cervical spine mobilisation and PFM manual relaxation improved symptoms in women with long histories of endometriosis [39].
Physiotherapists frequently employ manual therapy to address pain, with osteopathic techniques becoming increasingly popular. Properly selected techniques have the potential to alleviate pain, enhance functioning, and improve quality of life. The characteristics of studies outlining the effectiveness of manual therapy in treating endometriosis are detailed in Table 4.
Electrophysical Agents in the Treatment of Endometrial Symptoms
Electrophysical agents (EPA) contain the areas of physiotherapy that uses physical factors like cold, heat, electrical stimulation in the treatment process. Electrotherapy has been employed for managing endometriosis pain, utilizing techniques such as electrical neuromuscular stimulation (NMES) [32], and transcutaneous electrical nerve stimulation (TENS) [34]. Women who received NMES for 30 min, 3 times a week for 10 weeks showed decreased of pain endometriosis symptom severity and better results in SF-36 (36-26-item short-form Health Survey) compared to those who did not receive therapy. It is worth emphasizing that NMES was the only form of therapy in this group and has independently demonstrated effectiveness [32]. EPA can also be used as a complement to other therapy. Mira et al. [34] investigated the effects of TENS as an adjunct to hormone therapy for controlling pelvic pain in deep endometriosis. Women who self-administered TENS at home twice daily for 20 min over 8 weeks in the parasacral region experienced significant reductions in chronic pelvic pain and deep dyspareunia, along with notable improvements in quality of life, compared to those solely receiving hormonal treatment [34]. Thabet et al. [35] evaluated the use of Pulsed High-Intensity Laser Therapy (HILT) in addition to hormonal treatment, confirming significant reductions in pain and enhanced quality of life compared to placebo [35].
Furthermore, better treatment outcomes were observed using virtual reality (VR) compared to a standard tablet. Merlot et al. [27] conducted a study where women managing endometriosis pain were treated with a specialized application incorporating auditory and visual sensations. Divided into two groups—one using regular tablets and the other utilizing a VR device—the women in the VR group reported significantly lower pain levels post-treatment compared to the control group [27]. Pain reduction was also noted following thermal biofeedback therapy incorporating relaxation techniques and breathing exercises. Additionally, women acquired pain management skills through this therapy, although caution is warranted in interpreting the results due to the small sample size of the study (n = 5) [33].
Electrophysical agents in studies presents effectiveness alone and combined with other treatment in improve quality of life and pain. The characteristics of studies describing the effectiveness of electrophysical agents in the treatment of endometriosis are presented in Table 5.
Acupuncture in the Treatment of Endometrial Symptoms
Acupuncture is a controversial therapy. Traditional Chinese therapy appeals to non-anatomical structures such as meridians. The analgesic effect of acupuncture may be due to the stimulation of the nerves in the epidermis which, by sending impulses through the spinal cord to the brain, stimulate opioid secretion and decreased pain levels [38].
Rubi-Klein et al. [36] conducted 10 therapeutic acupuncture sessions, with one group receiving authentic treatment and the other receiving a placebo. Following a crossover between the groups, better outcomes were noted in the authentic acupuncture group. Women reported significantly lower pain sensations post-therapy, accompanied by increased quality of life, compared to the placebo group [36]. De Sousa et al. [38] reached similar conclusions. They divided women with endometriosis into two groups, one group receiving acupuncture at appropriate sites and the other group receiving a placebo. After five sessions, marked improvements in pain and quality of life were observed in the authentic acupuncture group compared to the placebo group. These results persisted until the second month post-therapy [38]. Acupuncture also turned out to be more effective in treating menstruation pain in women with endometriosis, compared to women who used pain killers to reduce pain. Acupuncture was applied to specific points on each day of menstruation for 3 cycles. The effect lasted until the second cycle after the end of treatment [40].
Despite many controversies around acupuncture, studies have demonstrated its efficacy in pain relief. However, according to the European Society of Human Reproduction and Embryology, no definitive recommendation can be made regarding its use in women with endometriosis [50]. The characteristics of studies describing the effectiveness of acupuncture in the treatment of endometriosis are presented in Table 6.
Diet and Cognitive Behavioral Therapy in the Treatment of Endometrial Symptoms
Endometriosis as a proinflammatory condition may be managed by diet. Some nutrients may decrease inflammatory factors, which can reduce pain [42]. Cirillo et al. [43] found a strong link between pain relief in endometriosis patients and Mediterranean dietary patterns. A individual Mediterranean diet shows promise for treating endometriosis-related symptoms and could be an effective long-term strategy for managing chronic pain alongside other nonmedical treatments [43]. Nodel et al. [42] confirmed that vitamin D supplementation in adolescents with surgically confirmed endometriosis significantly improved pelvic pain and catastrophic thinking, but these improvements were similar to those seen in the placebo group. Fish oil showed some improvement in VAS pain, but it was not statistically significant and was less effective than the other treatments. The study highlighted a strong placebo effect, indicating that participation in the study itself, rather than the supplements [42]. Van Haaps et al. [44] found that LOWFOOD diet or Endometriosis diet lead to reduced pain and improved quality of life for women with endometriosis after six months. Notably, those following the diet experienced less bloating and better quality of life in medical treatment and social support area [44].
The other treatment Cognitive Behavioral Therapy (CBT) may be beneficial for women with endometriosis due to the complex interplay between physical symptoms and mental health challenges associated with endometriosis. Donatti et al. [45] presented that CBT decreased depression from 64 to 12% in women, as well as stress prevalence decreased from 72 to 24%, and quality of live improved (p > 0.001) [45]. Wu et al. [46] assessed the impact of CBT and Tai Chi training on the quality of life of women who underwent surgery for endometriosis. Tai Chi training has shown effectiveness in reducing anxiety and stress, while the inclusion of CBT increased the positive effect on the quality of life and reduced depression [46]. In turn, Kold et al. [47] confirmed the effectiveness of mindfulness techniques, individual and group therapy. Women participating in the study significantly increased their quality of life and reduced pain associated with endometriosis.
Symptoms associated with endometriosis can also be effectively managed through psychological interventions and diet. A detailed description of the research can be found in Table 7.
Discussion
The aim of this review was to outline the most prevalent physiotherapeutic and non-medical approaches utilized in addressing symptoms linked with endometriosis and to assess their efficacy.
Endometriosis is often associated with chronic pelvic pain [51], frequently intensifies during menstruation [12]. Pain prompts individuals to adopt antalgic postures, and poor body posture, in turn, fosters myofascial disorders, such as muscle shortening, heightened tension, and consequently, weakness [12, 52]. Women may present Myofascial Trigger Points in the pelvic floor muscles as well as devious locations, complicating their identification. Trigger Points are a hypersensitive spot in the taut band and stimulation of this point cause referred pain [53]. These Points can disrupt both motor and autonomic function, disrupting the function of visceral organs [54]. Prolonged muscle tension causes muscle ischemia, worse trophic, stimulating pain receptors [55], which in turn leads to pelvic floor dysfunction [15]. Nevertheless, theories regarding trigger points are controversial [56]. Studies showed, that many women resign from physical activity due to pain [57]. Pain induces reduced activity, which precipitates trophic alterations in soft tissues, compromising their function, thereby weakening motor control in the lumbopelvic region, amplifying pain, and curtailing activity and social engagement [51]. The phenomenon of central sensitization is also often observed in women with endometriosis, which may be related to a lower response to treatment [58]. Nociceptive neurons in the dorsal horn of the spinal cord increase their excitability by repeated exposure to noxious stimuli, such as damage. Long-term irritation of nociceptive neurons causes a reduced pain threshold and an increased response to pain. Long-term pain also causes changes in the activity and structure of the brain, leading to changes in the processing of pain and sensory impulses. In addition, changes are also observed in the hypothalamic-pituitary-adrenal axis, which is also responsible for pain modulation [59].
Endometriosis exerts a profound impact on women’s lives, manifesting in reduced quality of life. Endometriosis-associated conditions, including sleep disturbances, fatigue, depression, anxiety, infertility, diminished productivity, and sexual dysfunction, impinge upon various aspects of life. Literature review and multivariate analysis of the impact of endometriosis on life performed by Missmer et al. [60] showed that endometriosis affects educational achievements, social, family and emotional life, and mental health [60]. To reduce the negative impact of the disease on the quality of life, it’s crucial to detect endometriosis early and initiate treatment promptly. Pharmacological therapies are commonly used for endometriosis symptoms, however may be associated with sleep disturbances, hot flashes, vaginitis, headaches, nausea and decreased bone density [61]. Pharmacotherapy typically results in a reduction of pelvic pain by approximately 2 points on a 10-cm visual analogue scale after 3 months [62]. However, despite the many side effects associated with pharmacological treatment, physiotherapy appears to offer an equally effective alternative for alleviating symptoms linked with endometriosis. Physiotherapeutic interventions employed in managing endometriosis symptoms encompass physical therapy, comprising exercises [25], aerobic training [26], yoga [22] and relaxation techniques, such as stretching, breathing [24] and progressive muscle relaxation [28]. Physical activity seems to be an effective, non-invasive method of alleviating the side effects of medications, delaying the decline in bone density, increasing the quality of life, and reducing pain. Physical therapy proves efficacious in reducing stress, anxiety, and normalizing cortisol levels [24]. Pain, dysmenorrhea and dyspareunia may be also treated by manual therapy [29,30,31, 37, 39]. Through myofascial connections, tensions can be transferred to other areas of the body, while inflammation and an increased number of inflammatory mediators in the pelvic organ area can contribute to myofascial disorders, intra-organ movement and vascular drainage [63]. Visceral therapy improved physical and mental function among 80% of women with endometriosis [29]. Transvaginal manual therapy relaxes muscles and restores normal pelvic tone, consequently reducing dyspareunia [30]. Adhesions commonly occurre with endometriosis and can be identified by physiotherapists; specialized techniques enable the detachment of adhesive crosslinks and alleviate pain during menstruation and intercourse [31]. Specialists may also use transperineal ultrasound to evaluate pelvic floor muscle functioning and localize muscles dysfunction [30]. Other complementary treatment for symptoms associated with endometriosis may be electrotherapy, exactly transcutaneous electrical nerve stimulation (TENS), which reduce pain. Studies suggest that TENS reduced chronic pelvic pain in VAS scale for approximately 2.55 points, whereas hormonal treatment alone reduced pain for approximately 0.27 points in VAS scale [34]. Positive outcomes have also been observed in studies on electrical neuromuscular stimulation (NMES); after 5 weeks of NMES treatment, pain decreased by approximately 1.4 points on a scale ranging from 0 to 10 [32]. Besides electrotherapy, epth are important [35]. Virtual reality may also prove to be a helpful technique in modern physiotherapy treatment aimed at better pain modulation [30]. Acupuncture is more and more often used as a therapy for gynecological disorders, despite the controversies. It demonstrates positive effects in women with endometriosis, reducing chronic pelvic pain by 66% and dyspareunia by 65%, with the effects persisting for at least 2 months post-acupuncture therapy [38]. Acupuncture exhibited a superior analgesic effect compared to Ibuprofen during menstruation in women with endometriosis [40]. Endometriosis, a proinflammatory condition, may be managed through dietary interventions, such as the Mediterranean diet, which has been linked to pain relief in patients [42]. Vitamin D supplementation and fish oil showed some benefits, though a strong placebo effect was noted [42]. The LOWFOOD diet also reduced pain and improved quality of life, particularly in reducing bloating and enhancing social support [44]. Cognitive Behavioral Therapy (CBT) has proven effective in reducing depression, stress, and improving the quality of life for women with endometriosis [45]. Additionally, Tai Chi and mindfulness techniques, both individual and group therapy, have shown significant benefits in managing anxiety, stress, and pain associated with endometriosis [46, 47].
Our review has its limitations. Firstly, many of the studies included had small sample sizes, and participant selection was not always heterogeneous, thus caution should be exercised in interpreting the results. Often, the research included women with severe endometriosis, which may not necessarily reflect outcomes in women with milder symptoms. Another constraint is the lack of validation of questionnaires for specific populations. Additionally, a considerable number of participants were lost during the study and follow-up. Not all studies were randomized, and some lacked proper controls. Short follow-up periods hindered the determination of long-term therapy effects. Furthermore, publications were restricted to those available in Polish and English. It’s important to note that specific criteria regarding the duration and type of research were not uniformly applied, which could influence the findings. Nonetheless, this allowed us to identify common non-medical methods for treating endometriosis and pinpoint areas requiring further investigation.
In conclusions, it is worth add physiotherapy methods in the reduce of symptoms of endometriosis. Physical activity, manual therapy, electrophysical agents, acupuncture, diet and cognitive behavioral therapy showed no negative side effects and reduced pain, what improved the quality of life and reduced the perceived stress.
Data availability
not applicable.
Code availability
not applicable.
References
Parazzini F, Esposito G, Tozzi L, Noli S, Bianchi S. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol. 2017;209:3–7. https://doi.org/10.1016/j.ejogrb.2016.04.021.
Zondervan KT, Becker CM, Koga K, Missmer SA, Taylor RN, Viganò P, Endometriosis. Nat Rev Dis Primers. 2018;4(1):9. https://doi.org/10.1038/s41572-018-0008-5.
Alimi Y, Iwanaga J, Loukas M, Tubbs RS. The clinical anatomy of endometriosis: a review. Cureus. 2018;10(9):e3361. https://doi.org/10.7759/cureus.3361.
Caporossi L, Capanna S, Viganò P, Alteri A, Papaleo B. From environmental to possible Occupational exposure to risk factors: what role do they play in the etiology of endometriosis? Int J Environ Res Public Health. 2021;18(2). https://doi.org/10.3390/ijerph18020532.
Królak A, Kurowska P, Giermaziak W. Ekonomiczny i społeczny wymiar endometriozy. Farm Pol. 2018;74(6):337–. https://doi.org/10.32383/farmpol/118772. 44.
Falcone T, Flyckt R. Clinical management of endometriosis. Obstet Gynecol. 2018;131(3):557–. https://doi.org/10.1097/aog.0000000000002469. 71.
Parasar P, Ozcan P, Terry KL. Endometriosis: epidemiology, diagnosis and clinical management. Curr Obstet Gynecol Rep. 2017;6(1):34–41. https://doi.org/10.1007/s13669-017-0187-1.
Morotti M, Vincent K, Brawn J, Zondervan KT, Becker CM. Peripheral changes in endometriosis-associated pain. Hum Reprod Update. 2014;20:717–36. https://doi.org/10.1093/humupd/dmu021.
Orr NL, Wahl KJ, Lisonek M, et al. Central sensitization inventory in endometriosis. Pain. 2022;163:e234–45. https://doi.org/10.1097/j.pain.0000000000002351.
Morotti M, Vincent K, Becker CM. Mechanisms of pain in endometriosis. Eur J Obstet Gynecol Reprod Biol. 2017;209:8–13. https://doi.org/10.1016/j.ejogrb.2016.07.497.
Zheng P, Zhang W, Leng J, Lang J. Research on central sensitization of endometriosis-associated pain: a systematic review of the literature. J Pain Res. 2019;12:1447–56. https://doi.org/10.2147/JPR.S197667.
Awad E, Ahmed HAH, Yousef A, Abbas R. Efficacy of exercise on pelvic pain and posture associated with endometriosis: within subject design. J Phys Ther Sci. 2017;29(12):2112–5. https://doi.org/10.1589/jpts.29.2112.
Lorbergs AL, Allaire BT, Yang L, Kiel DP, Cupples LA, Jarraya M, et al. A longitudinal study of Trunk Muscle Properties and Severity of thoracic kyphosis in women and men: the Framingham Study. J Gerontol Biol Sci Med Sci. 2019;74(3):420–7. https://doi.org/10.1093/gerona/gly056.
Lara-Ramos A, Álvarez-Salvago F, Fernández-Lao C, Galiano-Castillo N, Ocón-Hernández O, Mazheika M, et al. Widespread Pain Hypersensitivity and Lumbopelvic impairments in women diagnosed with endometriosis. Pain Med. 2021;22(9):1970–81. https://doi.org/10.1093/pm/pnaa463.
Cameron B, Sabourin J, Sanaee MS, Koenig NA, Lee T, Geoffrion R. Pelvic floor hypertonicity in women with pelvic floor disorders: a case control and risk prediction study. Neurourol Urodyn. 2019;38(2):696–702. https://doi.org/10.1002/nau.23896.
Wójcik M, Szczepaniak R, Placek K. Physiotherapy Management in Endometriosis. Int J Environ Res Public Health. 2022;19. https://doi.org/10.3390/ijerph192316148.
Smolarz B, Szyłło K, Romanowicz H, Endometriosis. Epidemiology, classification, Pathogenesis, Treatment and Genetics (Review of Literature). Int J Mol Sci. 2021;22(19). https://doi.org/10.3390/ijms221910554.
Tennfjord MK, Gabrielsen R, Tellum T. Effect of physical activity and exercise on endometriosis-associated symptoms: a systematic review. BMC Womens Health. 2021;21(1):355. https://doi.org/10.1186/s12905-021-01500-4.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, Bmj. 2009;339:b2535; https://doi.org/10.1371/journal.pmed.1000097.
Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. https://doi.org/10.1136/bmj.i4919.
Gonçalves AV, Barros NF, Bahamondes L. The practice of Hatha yoga for the treatment of Pain Associated with endometriosis. J Altern Complement Med. 2017;23(1):45–52. https://doi.org/10.1089/acm.2015.0343.
Gonçalves AV, Makuch MY, Setubal MS, Barros NF, Bahamondes L. A qualitative study on the practice of yoga for women with Pain-Associated Endometriosis. J Altern Complement Med. 2016;22(12):977–82. https://doi.org/10.1089/acm.2016.0021.
Friggi Sebe Petrelluzzi K, Garcia MC, Petta CA, Ribeiro DA, de Oliveira Monteiro NR, Céspedes IC, et al. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. J Psychosom Obstet Gynaecol. 2012;33(4):191–8. https://doi.org/10.3109/0167482x.2012.729625.
Armour M, Sinclair J, Chalmers KJ, Smith CA. Self-management strategies amongst Australian women with endometriosis: a national online survey. BMC Complement Altern Med. 2019;19(1):17. https://doi.org/10.1186/s12906-019-2431-x.
Bergström I, Freyschuss B, Jacobsson H, Landgren BM. The effect of physical training on bone mineral density in women with endometriosis treated with GnRH analogs: a pilot study. Acta Obstet Gynecol Scand. 2005;84(4):380–3. https://doi.org/10.1111/j.0001-6349.2005.00558.x.
Merlot B, Dispersyn G, Husson Z, et al. Pain Reduction with an Immersive Digital Therapeutic Tool in Women Living with endometriosis-related Pelvic Pain: Randomized Controlled Trial. J Med Internet Res. 2022;24:e39531. https://doi.org/10.2196/39531.
Zhao L, Wu H, Zhou X, Wang Q, Zhu W, Chen J. Effects of progressive muscular relaxation training on anxiety, depression and quality of life of endometriosis patients under gonadotrophin-releasing hormone agonist therapy. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):211–5. https://doi.org/10.1016/j.ejogrb.2012.02.029.
Daraï C, Deboute O, Zacharopoulou C, Laas E, Canlorbe G, Belghiti J, et al. Impact of osteopathic manipulative therapy on quality of life of patients with deep infiltrating endometriosis with colorectal involvement: results of a pilot study. Eur J Obstet Gynecol. 2015;188:70–3. https://doi.org/10.1016/j.ejogrb.2015.03.001.
Del Forno S, Arena A, Alessandrini M, Pellizzone V, Lenzi J, Raimondo D, et al. Transperineal Ultrasound Visual Feedback assisted pelvic floor muscle physiotherapy in Women with Deep infiltrating endometriosis and Dyspareunia: a pilot study. J Sex Marital Ther. 2020;46(7):603–11. https://doi.org/10.1080/0092623X.2020.1765057.
Wurn BF, Wurn LJ, Patterson K, King CR, Scharf ES. Decreasing Dyspareunia and Dysmenorrhea in Women with endometriosis via a Manual Physical Therapy: results from two Independent studies. J Endometr. 2011;3(4):188–96. https://doi.org/10.5301/JE.2012.9088.
Bi X-l, Xie C-x. Effect of neuromuscular electrical stimulation for endometriosis-associated pain: a retrospective study. Medicine. 2018;97(26). https://doi.org/10.1097/MD.0000000000011266.
Hawkins RS, Hart AD. The use of thermal biofeedback in the treatment of pain associated with endometriosis: preliminary findings. Appl Psychophysiol Biofeedback. 2003;28(4):279–. https://doi.org/10.1023/a:1027378825194. 89.
Mira TAA, Yela DA, Podgaec S, Baracat EC, Benetti-Pinto CL. Hormonal treatment isolated versus hormonal treatment associated with electrotherapy for pelvic pain control in deep endometriosis: randomized clinical trial. Eur J Obstet Gynecol. 2020;255:134–41. https://doi.org/10.1016/j.ejogrb.2020.10.018.
Thabet AAE, Alshehri MA. Effect of Pulsed High-Intensity Laser Therapy on Pain, adhesions, and Quality of Life in Women having endometriosis: a Randomized Controlled Trial. Photomed Laser Surg. 2018;36(7):363–9. https://doi.org/10.1089/pho.2017.4419.
Rubi-Klein K, Kucera-Sliutz E, Nissel H, Bijak M, Stockenhuber D, Fink M, et al. Is acupuncture in addition to conventional medicine effective as pain treatment for endometriosis? A randomised controlled cross-over trial. Eur J Obstet Gynecol. 2010;153(1):90–. https://doi.org/10.1016/j.ejogrb.2010.06.023. 3.
Muñoz-Gómez E, Alcaraz-Martínez AM, Mollà-Casanova S, et al. Effectiveness of a Manual Therapy Protocol in Women with Pelvic Pain due to endometriosis: a Randomized Clinical Trial. J Clin Med. 2023;12. https://doi.org/10.3390/jcm12093310.
de Sousa TR, de Souza BC, Zomkowisk K, da Rosa PC, Sperandio FF. The effect of acupuncture on pain, dyspareunia, and quality of life in Brazilian women with endometriosis: a randomized clinical trial. Complement Ther Med. 2016;25:114–21. https://doi.org/10.1016/j.ctcp.2016.09.006.
Sillem M, Juhasz-Böss I, Klausmeier I, Mechsner S, Siedentopf F, Solomayer E. Osteopathy for endometriosis and Chronic Pelvic Pain– a pilot study. Geburtshilfe Frauenheilkd. 2016;76:960–3. https://doi.org/10.1055/s-0042-111010.
Tian L, Cheng Z, Cheng X, Nie T. Acupuncture for dysmenorrhea of adenomyosis: a randomized controlled trial. World J Acupunct Moxibustion. 2022;32:199–203. https://doi.org/10.1016/j.wjam.2021.11.004.
Del Forno S, Cocchi L, Arena A, et al. Effects of Pelvic Floor muscle physiotherapy on urinary, Bowel, and sexual functions in women with deep infiltrating endometriosis: a Randomized Controlled Trial. Medicina. 2024;60:67. https://doi.org/10.3390/medicina60010067.
Nodler JL, DiVasta AD, Vitonis AF, et al. Supplementation with vitamin D or ω-3 fatty acids in adolescent girls and young women with endometriosis (SAGE): a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr. 2020;112:229–36. https://doi.org/10.1093/ajcn/nqaa096.
Cirillo M, Argento FR, Becatti M, Fiorillo C, Coccia ME, Fatini C. Mediterranean Diet and oxidative stress: a relationship with Pain Perception in Endometriosis. Int J Mol Sci. 2023;24:14601. https://doi.org/10.3390/ijms241914601.
van Haaps AP, Wijbers JV, Schreurs AMF, et al. The effect of dietary interventions on pain and quality of life in women diagnosed with endometriosis: a prospective study with control group. Hum Reprod. 2023;38:2433–46. https://doi.org/10.1093/humrep/dead214.
Donatti L, Podgaec S, Baracat EC. Efficacy of cognitive behavioral therapy in treating women with endometriosis and chronic pelvic pain: a randomized trial. J Health Psychol. 2024;2:13591053241240198. https://doi.org/10.1177/13591053241240198.
Wu S, Wang X, Liu H, Zheng W. Efficacy of cognitive behavioral therapy after the surgical treatment of women with endometriosis: a preliminary case-control study. Med (Baltim). 2022;101:e32433. https://doi.org/10.1097/MD.0000000000032433.
Kold M, Hansen T, Vedsted-Hansen H, Forman A. Mindfulness-based psychological intervention for coping with pain in endometriosis. Nordic Psychol. 2012;64:2–16. https://doi.org/10.1080/19012276.2012.693727.
Piggin J. What is physical activity? A holistic definition for teachers, Researchers and Policy makers. Front Sports Act Living. 2020;2:72. https://doi.org/10.3389/fspor.2020.00072.
Geri T, Viceconti A, Minacci M, Testa M, Rossettini G. Manual therapy: exploiting the role of human touch. Musculoskelet Sci Pract. 2019;44:102044. https://doi.org/10.1016/j.msksp.2019.07.008.
Becker CM, Bokor A, Heikinheimo O, Horne A, Jansen F, Kiesel L, King K, Kvaskoff M, Nap A, Petersen K, Saridogan E, Tomassetti C, van Hanegem N, Vulliemoz N, Vermeulen N. ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum Reprod Open. 2022, 26;2022(2):hoac009; https://doi.org/10.1093/hropen/hoac009.
Mińko A, Turoń-Skrzypińska A, Rył A, Bargiel P, Hilicka Z, Michalczyk K, et al. Endometriosis-A multifaceted problem of a modern woman. Int J Environ Res Public Health. 2021;18(15). https://doi.org/10.3390/ijerph18158177.
Mechsner S. Endometriosis, an Ongoing Pain-Step-by-step treatment. J Clin Med. 2022;11(2). https://doi.org/10.3390/jcm11020467.
Fernández-de-Las-Peñas C, Dommerholt J. International Consensus on Diagnostic Criteria and clinical considerations of myofascial trigger points: a Delphi Study. Pain Med. 2018;19(1):142–50. https://doi.org/10.1093/pm/pnx207.
Aredo JV, Heyrana KJ, Karp BI, Shah JP, Stratton P. Relating Chronic Pelvic Pain and Endometriosis to signs of Sensitization and Myofascial Pain and Dysfunction. Semin Reprod Med. 2017;35(01):088–97. https://doi.org/10.1055/s-0036-1597123.
Dos Bispo AP, Ploger C, Loureiro AF, Sato H, Kolpeman A, Girão MJ, et al. Assessment of pelvic floor muscles in women with deep endometriosis. Arch Gynecol Obstet. 2016;294(3):519–. https://doi.org/10.1007/s00404-016-4025-x. 23.
Quintner JL, Bove GM, Cohen ML. A critical evaluation of the trigger point phenomenon. Rheumatology (Oxford). 2015;54(3):392–9. https://doi.org/10.1093/rheumatology/keu471.
Warzecha D, Szymusik I, Wielgos M, Pietrzak B. The impact of endometriosis on the quality of life and the incidence of Depression-A Cohort Study. Int J Environ Res Public Health. 2020;17(10). https://doi.org/10.3390/ijerph17103641.
Orr NL, Huang AJ, Liu YD, Noga H, Bedaiwy MA, Williams C, Allaire C, Yong PJ. Association of Central Sensitization Inventory scores with Pain outcomes after endometriosis surgery. JAMA Netw Open. 2023;6(2):e230780. https://doi.org/10.1001/jamanetworkopen.2023.0780.
McNamara HC, Frawley HC, Donoghue JF, Readman E, Healey M, Ellett L, Reddington C, Hicks LJ, Harlow K, Rogers PAW, Cheng C. Peripheral, Central, and Cross Sensitization in Endometriosis-Associated Pain and Comorbid Pain syndromes. Front Reprod Health. 2021;3:729642. https://doi.org/10.3389/frph.2021.729642.
Agarwal SK, Chapron C, Giudice LC, Laufer MR, Leyland N, Missmer SA, Singh SS, Taylor HS. Clinical diagnosis of endometriosis: a call to action. Am J Obstet Gynecol. 2019;220(4):354.e1-354.e12.
Brown J, Farquhar C. An overview of treatments for endometriosis. JAMA. 2015;313(3):296–7. https://doi.org/10.1001/jama.2014.17119.
Samy A, Taher A, Sileem SA, Abdelhakim AM, Fathi M, Haggag H, Ashour K, Ahmed SA, Shareef MA, AlAmodi AA, Keshta NHA, Shatat HBAE, Salah DM, Ali AS, El Kattan EAM, Elsherbini M. Medical therapy options for endometriosis related pain, which is better? A systematic review and network meta-analysis of randomized controlled trials. J Gynecol Obstet Hum Reprod. 2021;50(1):101798. https://doi.org/10.1016/j.jogoh.2020.101798.
Wojcik M, Plagens-Rotman K, Merks P, Mizgier M, Kedzia W, Jarzabek-Bielecka G. Visceral therapy in disorders of the female reproductive organs. Ginekol Pol. 2022;93(6):511–8. https://doi.org/10.5603/GP.a2022.0021.
Acknowledgements
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
None.
Ethics Approval
not applicable.
Consent to Participate
not applicable.
Consent for Publication
not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mazur-Bialy, A., Tim, S., Pępek, A. et al. Holistic Approaches in Endometriosis - as an Effective Method of Supporting Traditional Treatment: A Systematic Search and Narrative Review. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01660-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01660-2