Abstract
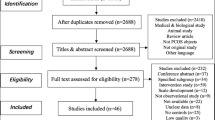
While polycystic ovarian syndrome (PCOS) is one of the most common hormonal endocrine disorders among women of reproductive age, the psychosocial impact of PCOS has not been evaluated across different quality of life (QoL) indicators. We rigorously analyzed available evidence pertaining to the psychosocial burden of PCOS in women of reproductive age and compared validated QoL scores of women with and without PCOS before and after treatment. We searched and considered publications from PubMed, PsychINFO, Embase, and Cochrane Library that evaluated the association between diagnosed PCOS and QoL by standardized and validated questionnaires at baseline and after treatment. Reviewers assessed the risk of bias using established Cochrane and Newcastle–Ottawa Scale guidelines. A total of 33 studies were included in the review: 14 randomized controlled trials and 19 observational studies. The 36-Item Short Form Survey and World Health Organization Quality of Life – BREF questionnaire both revealed that the diagnosis and life experience of PCOS had a disability score that was similar to or surpassed that of heart disease, diabetes mellitus, or breast cancer. QoL scores, associated with mental health issues, infertility, sexual dysfunction, obesity, menstrual disorder, and hirsutism, were lower at the baseline than after treatment in the majority of instruments measuring these variables in women with PCOS. PCOS is associated with significant psychosocial stress and reduced QoL across baseline measures and in comparison, to other diseases. Evidence suggests that treatment with therapy, medications, and lifestyle management decreased psychosocial burdens and alleviated QoL experienced by women with PCOS.

Similar content being viewed by others
Data Availability
The data that support the findings of this study were derived from the following resources available in the public domain: PubMed, Embase, PsycINFO, and Cochrane Library databases.
Code Availability
N/A.
References
Azziz R. PCOS: a diagnostic challenge. Reprod Biomed Online. 2004;8(6):644–8. https://doi.org/10.1016/s1472-6483(10)61644-6.
Riestenberg C, Jagasia A, Markovic D, Buyalos RP, Azziz R. Health care-related economic burden of polycystic ovary syndrome in the United States: pregnancy-related and long-term health consequences. J Clin Endocrinol Metab. 2022;107(2):575–85. https://doi.org/10.1210/clinem/dgab613.
Centers for Disease Control and Prevention. PCOS (polycystic ovary syndrome) and diabetes. https://www.cdc.gov/diabetes/basics/pcos.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Flibrary%2Fspotlights%2Fpcos.html. Published March 24, 2020. Accessed June 19, 2022.
Legro RS, Arslanian SA, Ehrmann DA et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline [published correction appears in J Clin Endocrinol Metab. 2021;106(6):e2462]. J Clin Endocrinol Metab. 2013;98(12):4565–4592. https://doi.org/10.1210/jc.2013-2350
Tabassum F, Jyoti C, Sinha HH, Dhar K, Akhtar MS. Impact of polycystic ovary syndrome on quality of life of women in correlation to age, basal metabolic index, education and marriage. PLoS One. 2021;16(3):e0247486. https://doi.org/10.1371/journal.pone.0247486
Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018;62(2):318–25. https://doi.org/10.1007/s12020-018-1692-3.
Angin P, Yoldemir T, Atasayan K. Quality of life among infertile PCOS patients. Arch Gynecol Obstet. 2019;300(2):461–7. https://doi.org/10.1007/s00404-019-05202-z.
Ou HT, Chen PC, Wu MH, Lin CY. Metformin improved health-related quality of life in ethnic Chinese women with polycystic ovary syndrome [published correction appears in Health Qual Life Outcomes. 2018;16(1):217]. Health Qual Life Outcomes. 2016;14(1):119. https://doi.org/10.1186/s12955-016-0520-9
Addington-Hall J, Kalra L. Who should measure quality of life? BMJ. 2001;322(7299):1417–20. https://doi.org/10.1136/bmj.322.7299.1417.
Sulaiman MA, Al-Farsi YM, Al-Khaduri MM, Waly MI, Saleh J, Al-Adawi S. Psychological burden among women with polycystic ovarian syndrome in Oman: a case-control study. Int J Womens Health. 2017;9:897–904. https://doi.org/10.2147/IJWH.S145383
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928
Wells G, Shea B, O’Connell D et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed June 20, 2022.
Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: a randomized controlled clinical trial. J Psychosom Obstet Gynaecol. 2019;40(4):283–93. https://doi.org/10.1080/0167482X.2018.1502265.
AlHussain F, AlRuthia Y, Al-Mandeel H, et al. Metformin improves the depression symptoms of women with polycystic ovary syndrome in a lifestyle modification program. Patient Prefer Adherence. 2020;14:737–746. https://doi.org/10.2147/PPA.S244273
Alkoudsi KT, Al-Qudah R, Basheti IA. Assessing the effectiveness of a pharmaceutical care service on the quality of life of women with polycystic ovarian syndrome living in war and non-war countries. J Eval Clin Pract. 2020;26(5):1467–77. https://doi.org/10.1111/jep.13310.
Altinok ML, Ravn P, Andersen M, Glintborg D. Effect of 12-month treatment with metformin and/or oral contraceptives on health-related quality of life in polycystic ovary syndrome. Gynecol Endocrinol. 2018;34(10):859–63. https://doi.org/10.1080/09513590.2018.1460343.
Artani M, Iftikhar MF, Khan S. Effects of metformin on symptoms of polycystic ovarian syndrome among women of reproductive age. Cureus. 2018;10(8):e3203. https://doi.org/10.7759/cureus.3203
Clayton WJ, Lipton M, Elford J, Rustin M, Sherr L. A randomized controlled trial of laser treatment among hirsute women with polycystic ovary syndrome. Br J Dermatol. 2005;152(5):986–92. https://doi.org/10.1111/j.1365-2133.2005.06426.x.
Hahn S, Benson S, Elsenbruch S, et al. Metformin treatment of polycystic ovary syndrome improves health-related quality-of-life, emotional distress and sexuality. Hum Reprod. 2006;21(7):1925–34. https://doi.org/10.1093/humrep/del069.
Hukire S, Devi TP. Effectiveness of lifestyle modification in late adolescent females with normal BMI polycystic ovarian syndrome. Indian J Forensic Med Toxicol. 2020;14(2):185–9. https://doi.org/10.37506/ijfmt.v14i2.2785.
Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of holistic yoga program on anxiety symptoms in adolescent girls with polycystic ovarian syndrome: a randomized control trial. Int J Yoga. 2012;5(2):112–7. https://doi.org/10.4103/0973-6131.98223.
Ramos FK, Lara LA, Kogure GS, et al. Quality of life in women with polycystic ovary syndrome after a program of resistance exercise training. Rev Bras Ginecol Obstet. 2016;38(7):340–7. https://doi.org/10.1055/s-0036-1585457.
Ramya R, Jose S, Mamatha K, KM S. Quality of life in women with polycystic ovarian syndrome: requisite of clinical pharmacist intervention. Asian J Pharm Clin Res. 2019;12(11):100–105. https://doi.org/10.22159/ajpcr.2019.v12i11.34426.
Ribeiro VB, Lopes IP, Dos Reis RM, et al. Continuous versus intermittent aerobic exercise in the improvement of quality of life for women with polycystic ovary syndrome: a randomized controlled trial. J Health Psychol. 2021;26(9):1307–17. https://doi.org/10.1177/1359105319869806.
Thomson RL, Buckley JD, Lim SS, et al. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertil Steril. 2010;94(5):1812–6. https://doi.org/10.1016/j.fertnstert.2009.11.001.
Aliasghari F, Mirghafourvand M, Charandabi SM, Lak TB. The predictors of quality of life in women with polycystic ovarian syndrome. Int J Nurs Pract. 2017;23(3):e12526. https://doi.org/10.1111/ijn.12526.
Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S. Predictive factors of health-related quality of life in patients with polycystic ovary syndrome: a structural equation modeling approach. Fertil Steril. 2013;100(5):1389–96. https://doi.org/10.1016/j.fertnstert.2013.06.043.
Behboodi Moghadam Z, Fereidooni B, Saffari M, Montazeri A. Polycystic ovary syndrome and its impact on Iranian women’s quality of life: a population-based study. BMC Womens Health. 2018;18(1):164. https://doi.org/10.1186/s12905-018-0658-1
Benetti-Pinto CL, Ferreira SR, Antunes A Jr, Yela DA. The influence of body weight on sexual function and quality of life in women with polycystic ovary syndrome. Arch Gynecol Obstet. 2015;291(2):451–5. https://doi.org/10.1007/s00404-014-3423-1.
Benson S, Hahn S, Tan S, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: results of an internet-based survey in Germany. Hum Reprod. 2009;24(6):1446–51. https://doi.org/10.1093/humrep/dep031.
Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian J Psychol Med. 2018;40(3):239–46. https://doi.org/10.4103/IJPSYM.IJPSYM_561_17.
Ching HL, Burke V, Stuckey BG. Quality of life and psychological morbidity in women with polycystic ovary syndrome: body mass index, age and the provision of patient information are significant modifiers. Clin Endocrinol (Oxf). 2007;66(3):373–9. https://doi.org/10.1111/j.1365-2265.2007.02742.x.
Drosdzol A, Skrzypulec V, Mazur B, Pawlińska-Chmara R. Quality of life and marital sexual satisfaction in women with polycystic ovary syndrome. Folia Histochem Cytobiol. 2007;45(Suppl 1):S93–7. https://doi.org/10.5603/4495.
Elsenbruch S, Hahn S, Kowalsky D, et al. Quality of life, psychosocial well-being, and sexual satisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88(12):5801–7. https://doi.org/10.1210/jc.2003-030562.
Greenwood EA, Pasch LA, Cedars MI, Legro RS, Huddleston HG, Eunice Kennedy Shriver National Institute of Child Health and Human Development Reproductive Medicine Network. Association among depression, symptom experience, and quality of life in polycystic ovary syndrome. Am J Obstet Gynecol. 2018;219(3):279.e1-279.e7. https://doi.org/10.1016/j.ajog.2018.06.017.
Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 2015;10(4):e0123608. https://doi.org/10.1371/journal.pone.0123608
Kumarapeli V, SeneviratneRde A, Wijeyaratne C. Health-related quality of life and psychological distress in polycystic ovary syndrome: a hidden facet in South Asian women. BJOG. 2011;118(3):319–28. https://doi.org/10.1111/j.1471-0528.2010.02799.x.
Månsson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landén M. Women with polycystic ovary syndrome are often depressed or anxious–a case control study. Psychoneuroendocrinology. 2008;33(8):1132–8. https://doi.org/10.1016/j.psyneuen.2008.06.003.
Schmid J, Kirchengast S, Vytiska-Binstorfer E, Huber J. Infertility caused by PCOS–health-related quality of life among Austrian and Moslem immigrant women in Austria. Hum Reprod. 2004;19(10):2251–7. https://doi.org/10.1093/humrep/deh432.
Tan S, Hahn S, Benson S, et al. Psychological implications of infertility in women with polycystic ovary syndrome. Hum Reprod. 2008;23(9):2064–71. https://doi.org/10.1093/humrep/den227.
Tekin A, Demiryürek E, Çakmak E, Temizkan O, Özer ÖA, Karamustafalıoğlu O. A cross-sectional investigation of quality of life in patients with polycystic ovary syndrome. Sisli Etfal Hastan Tip Bul. 2018;52(2):109–113. https://doi.org/10.14744/SEMB.2018.38247
Trent ME, Rich M, Austin SB, Gordon CM. Quality of life in adolescent girls with polycystic ovary syndrome. Arch Pediatr Adolesc Med. 2002;156(6):556–60. https://doi.org/10.1001/archpedi.156.6.556.
Alonso J, Ferrer M, Gandek B, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQoLA) Project. Qual Life Res. 2004;13(2):283–98. https://doi.org/10.1023/b:qure.0000018472.46236.05.
Lee SH, Min YS, Park HY, Jung TD. Health-related quality of life in breast cancer patients with lymphedema who survived more than one year after surgery. J Breast Cancer. 2012;15(4):449–53. https://doi.org/10.4048/jbc.2012.15.4.449.
Rose M, Köhler K, Köhler F, Sawitzky B, Fliege H, Klapp BF. Determinants of the quality of life of patients with congenital heart disease. Qual Life Res. 2005;14(1):35–43. https://doi.org/10.1007/s11136-004-0611-7.
Pandey S, Kumar P, Singh CM, Ranjan A, Bhar D, Agrawal N. Quality of life using WHOQOL-BREF of patients with type 2 diabetes mellitus attending a primary health centre of Patna, India. Indian J Prevent Soc Med. 2020;51:151–7.
Koboto DD, Deribe B, Gebretsadik A, et al. Quality of life among breast cancer patients attending Hawassa University Comprehensive Specialized Hospital Cancer Treatment Center. Breast Cancer (Dove Med Press). 2020;12:87–95. Published 2020 Jun 30. https://doi.org/10.2147/BCTT.S252030
Artini PG, Di Berardino OM, Simi G, Papini F, Ruggiero M, Monteleone P, Cela V. Best methods for identification and treatment of PCOS. Minerva Ginecol. 2010;62(1):33.
Moran LJ, Brinkworth G, Noakes M, Norman RJ. Effects of lifestyle modification in polycystic ovarian syndrome. Reprod Biomed Online. 2006;12(5):569–78. https://doi.org/10.1016/s1472-6483(10)61182-0.
Norman RJ, Davies MJ, Lord J, Moran LJ. The role of lifestyle modification in polycystic ovary syndrome. Trends Endocrinol Metab. 2002;13(6):251–7. https://doi.org/10.1016/s1043-2760(02)00612-4.
Vrbíková J, Cibula D. Combined oral contraceptives in the treatment of polycystic ovary syndrome. Hum Reprod Update. 2005;11(3):277–91. https://doi.org/10.1093/humupd/dmi005.
Shah D, Patil M, National PCOS Working Group. Consensus statement on the use of oral contraceptive pills in polycystic ovarian syndrome women in India. J Hum Reprod Sci. 2018;11(2):96–118. https://doi.org/10.4103/jhrs.JHRS_72_18.
Seli E, Duleba AJ. Should patients with polycystic ovarian syndrome be treated with metformin? Hum Reprod. 2002;17(9):2230–6. https://doi.org/10.1093/humrep/17.9.2230.
Cheang KI, Huszar JM, Best AM, Sharma S, Essah PA, Nestler JE. Long-term effect of metformin on metabolic parameters in the polycystic ovary syndrome. Diab Vasc Dis Res. 2009;6(2):110–9. https://doi.org/10.1177/1479164109336050.
Kilic S, Yilmaz N, Zulfikaroglu E, Erdogan G, Aydin M, Batioglu S. Inflammatory-metabolic parameters in obese and nonobese normoandrogenemic polycystic ovary syndrome during metformin and oral contraceptive treatment. Gynecol Endocrinol. 2011;27(9):622–9. https://doi.org/10.3109/09513590.2010.530706.
Blume-Peytavi U, Hahn S. Medical treatment of hirsutism. Dermatol Ther. 2008;21(5):329–39. https://doi.org/10.1111/j.1529-8019.2008.00215.x.
Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4. https://doi.org/10.1136/bmj.305.6846.160.
Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–8. https://doi.org/10.1016/s0895-4356(98)00109-7.
Kumarapeli V, de A Seneviratne R, Wijeyaratne CN. Validation of WHOQOL-BREF to measure quality of life among women with polycystic ovary syndrome. J Coll Commun Phys Sri Lanka. 2006;11(2):1–9. https://doi.org/10.4038/jccpsl.v11i2.8252.
Kurtin PS, Landgraf JM, Abetz L. Patient-based health status measurements in pediatric dialysis: expanding the assessment of outcome. Am J Kidney Dis. 1994;24(2):376–82. https://doi.org/10.1016/s0272-6386(12)80205-8.
Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis. 1994;18(Suppl 1):S79–83. https://doi.org/10.1093/clinids/18.supplement_1.s79.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the General Anxiety Disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713. https://doi.org/10.3389/fpsyg.2019.01713
Bocéréan C, Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry. 2014;14:354. https://doi.org/10.1186/s12888-014-0354-0
Meston CM. Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003;29(1):39–46. https://doi.org/10.1080/713847100.
Schmitt DP, Allik J. Simultaneous administration of the Rosenberg Self-Esteem Scale in 53 nations: exploring the universal and culture-specific features of global self-esteem. J Pers Soc Psychol. 2005;89(4):623–42. https://doi.org/10.1037/0022-3514.89.4.623.
Mark KP, Herbenick D, Fortenberry JD, Sanders S, Reece M. A psychometric comparison of three scales and a single-item measure to assess sexual satisfaction. J Sex Res. 2014;51(2):159–69. https://doi.org/10.1080/00224499.2013.816261.
Sheehan DV, Lecrubier Y, Sheehan KH, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–57.
Cosco TD, Prina M, Stubbs B, Wu YT. Reliability and validity of the center for epidemiologic studies depression scale in a population-based cohort of middle-aged U.S. Adults. J Nurs Meas. 2017;25(3):476–85. https://doi.org/10.1891/1061-3749.25.3.476.
Williams S, Sheffield D, Knibb RC. The polycystic ovary syndrome quality of life scale (PCOSQOL): development and preliminary validation. Health Psychol Open. 2018;5(2):2055102918788195. https://doi.org/10.1177/2055102918788195
Author information
Authors and Affiliations
Contributions
AR, IS, and BS conceived of the presented idea and supervised the findings of this work. EN searched the databases for review articles for the research questions. AR, IS, and BS interpreted the data and wrote the manuscript with help from JS and LS. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
N/A.
Consent to Participate
N/A.
Consent for Publication
N/A.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rempert, A.N., Sarria, I., Standeven, L.R. et al. A Systematic Review of the Psychosocial Impact of Polycystic Ovarian Syndrome Before and After Treatment. Reprod. Sci. 30, 3153–3178 (2023). https://doi.org/10.1007/s43032-023-01285-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01285-x