Abstract
There is various evidence to suggest a relationship between female hormones and meningiomas; as clinicians, we often come to face challenging situations involving female patients diagnosed with meningiomas during the post-pubertal phases of their life. We aimed to review the specific circumstances (pregnancy, postpartum, hormonal contraception and hormone replacement therapy, gender-affirming hormonal treatment) clinicians might come to face during their daily clinical practice, given the absence of available guidelines. We therefore conducted a narrative review on articles found in PubMed and Embase databases using appropriate keywords. Ninety-six relevant articles were included. The available evidence on managing meningiomas in post-pubertal women often implies personal strategies, highlighting the lack of a unified approach. The knowledge of the biological links between female hormones and meningiomas is fundamental to correctly counsel patients in various life phases. Prospective randomized studies are required to improve available guidelines on how to best manage meningiomas in female post-pubertal patients.



Similar content being viewed by others
References
DeAngelis LM. Brain tumors. N Engl J Med. 2001;344(2):114–23. https://doi.org/10.1056/NEJM200101113440207.
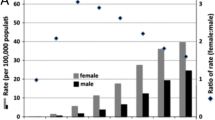
Longstreth WT Jr, Dennis LK, McGuire VM, Drangsholt MT, Koepsell TD. Epidemiology of intracranial meningioma. Cancer. 1993;72(3):639–48.
Mindermann T, Wilson CB. Age-related and gender-related occurrence of pituitary adenomas. Clin Endocrinol. 1994;41(3):359–64. https://doi.org/10.1111/j.1365-2265.1994.tb02557.x.
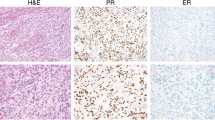
Blankenstein MA, Verheijen FM, Jacobs JM, Donker TH, van Duijnhoven MW, Thijssen JH. Occurrence, regulation, and significance of progesterone receptors in human meningioma. Steroids. 2000;65(10-11):795–800. https://doi.org/10.1016/s0039-128x(00)00193-8.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–20. https://doi.org/10.1007/s00401-016-1545-1.
Bos D, Poels MM, Adams HH, Akoudad S, Cremers LG, Zonneveld HI, et al. Prevalence, clinical management, and natural course of incidental findings on brain MR images: the population-based Rotterdam Scan Study. Radiology. 2016;281(2):507–15. https://doi.org/10.1148/radiol.2016160218.
Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J, et al. Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg. 2015;122(1):4–23. https://doi.org/10.3171/2014.7.JNS131644.
Lee CC, Trifiletti DM, Sahgal A, DeSalles A, Fariselli L, Hayashi M, et al. Stereotactic radiosurgery for benign (World Health Organization Grade I) cavernous sinus meningiomas-International Stereotactic Radiosurgery Society (ISRS) practice guideline: a systematic review. Neurosurgery. 2018;83(6):1128–42. https://doi.org/10.1093/neuros/nyy009.
Kaley T, Barani I, Chamberlain M, McDermott M, Panageas K, Raizer J, et al. Historical benchmarks for medical therapy trials in surgery- and radiation-refractory meningioma: a RANO review. Neuro-Oncology. 2014;16(6):829–40. https://doi.org/10.1093/neuonc/not330.
Klaeboe L, Lonn S, Scheie D, Auvinen A, Christensen HC, Feychting M, et al. Incidence of intracranial meningiomas in Denmark, Finland, Norway and Sweden, 1968-1997. Int J Cancer. 2005;117(6):996–1001. https://doi.org/10.1002/ijc.21255.
Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neuro-Oncol. 2010;99(3):307–14. https://doi.org/10.1007/s11060-010-0386-3.
Magdelenat H, Pertuiset BF, Poisson M, Martin PM, Philippon J, Pertuiset B, et al. Progestin and oestrogen receptors in meningiomas. Biochemical characterization, clinical and pathological correlations in 42 cases. Acta Neurochir. 1982;64(3-4):199–213. https://doi.org/10.1007/BF01406053.
Donnell MS, Meyer GA, Donegan WL. Estrogen-receptor protein in intracranial meningiomas. J Neurosurg. 1979;50(4):499–502. https://doi.org/10.3171/jns.1979.50.4.0499.
Lesch KP, Fahlbusch R. Analysis of estradiol and progesterone receptors in meningioma. Neurochirurgia (Stuttg). 1986;29(4):99–104. https://doi.org/10.1055/s-2008-1054147.
Lesch KP, Schott W, Engl HG, Gross S, Thierauf P. Gonadal steroid receptors in meningiomas. J Neurol. 1987;234(5):328–33. https://doi.org/10.1007/BF00314289.
Poisson M, Pertuiset BF, Hauw JJ, Philippon J, Buge A, Moguilewsky M, et al. Steroid hormone receptors in human meningiomas, gliomas and brain metastases. J Neuro-Oncol. 1983;1(3):179–89. https://doi.org/10.1007/BF00165601.
Olson JJ. Laboratory evidence for the hormonal dependency of meningiomas. Hum Reprod. 1994;9(Suppl 1):195–201. https://doi.org/10.1093/humrep/9.suppl_1.195.
Maiuri F, Mariniello G, Guadagno E, Barbato M, Corvino S, Del Basso De Caro M. WHO grade, proliferation index, and progesterone receptor expression are different according to the location of meningioma. Acta Neurochir. 2019;161(12):2553–61. https://doi.org/10.1007/s00701-019-04084-z.
Nishioka T, Kondo A, Aoyama I, Shimotake K, Takahashi J, Kusaka H. Primary interosseous meningioma associated with pregnancy--case report. Neurol Med Chir (Tokyo). 1989;29(7):619–23. https://doi.org/10.2176/nmc.29.619.
Chakravarthy V, Kaplan B, Gospodarev V, Myers H, De Los RK, Achiriloaie A. Houdini tumor: case report and literature review of pregnancy-associated meningioma. World Neurosurg. 2018;114:e1261–e5. https://doi.org/10.1016/j.wneu.2018.03.187.
Casabella AM, Urakov TM, Basil G, Morcos JJ. Management of Foramen magnum meningioma during pregnancy: literature review and case report. World Neurosurg. 2017;97:752 e15–8. https://doi.org/10.1016/j.wneu.2016.10.058.
King AB. Neurologic conditions occurring as complications of pregnancy. Arch NeurPsych. 1950;63(4):611–33. https://doi.org/10.1001/archneurpsyc.1950.02310220078008.
Weyland RD, MacCarthy CS, Wilson RB. The effect of pregnancy on intercranial meningiomas occurring about the optic chiasma. Surg Clin N Amer. 1951;31:122.
Priddy BH, Otto BA, Carrau RL, Prevedello DM. Management of skull base tumors in the obstetric population: a case series. World Neurosurg. 2018;113:e373–e82. https://doi.org/10.1016/j.wneu.2018.02.038.
Wigertz A, Lonn S, Hall P, Auvinen A, Christensen HC, Johansen C, et al. Reproductive factors and risk of meningioma and glioma. Cancer Epidemiol Biomark Prev. 2008;17(10):2663–70. https://doi.org/10.1158/1055-9965.EPI-08-0406.
Laviv Y, Bayoumi A, Mahadevan A, Young B, Boone M, Kasper EM. Meningiomas in pregnancy: timing of surgery and clinical outcomes as observed in 104 cases and establishment of a best management strategy. Acta Neurochir. 2018;160(8):1521–9. https://doi.org/10.1007/s00701-017-3146-8.
Harland TA, Freeman JL, Davern M, McCracken DJ, Celano EC, Lillehei K, et al. Progesterone-only contraception is associated with a shorter progression-free survival in premenopausal women with WHO Grade I meningioma. J Neuro-Oncol. 2018;136(2):327–33. https://doi.org/10.1007/s11060-017-2656-9.
Bickerstaff ER, Small JM, Guest IA. The relapsing course of certain meningiomas in relation to pregnancy and menstruation. J Neurol Neurosurg Psychiatry. 1958;21(2):89–91. https://doi.org/10.1136/jnnp.21.2.89.
Schlehofer B, Blettner M, Wahrendorf J. Association between brain tumors and menopausal status. J Natl Cancer Inst. 1992;84(17):1346–9. https://doi.org/10.1093/jnci/84.17.1346.
Wahab M, Al-Azzawi F. Meningioma and hormonal influences. Climacteric. 2003;6(4):285–92.
Hortobagyi T, Bencze J, Murnyak B, Kouhsari MC, Bognar L, Marko-Varga G. Pathophysiology of Meningioma Growth in Pregnancy. Open Med (Wars). 2017;12:195–200. https://doi.org/10.1515/med-2017-0029.
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007;357(18):1821–8. https://doi.org/10.1056/NEJMoa070972.
Verheecke M, Halaska MJ, Lok CA, Ottevanger PB, Fruscio R, Dahl-Steffensen K, et al. Primary brain tumours, meningiomas and brain metastases in pregnancy: report on 27 cases and review of literature. Eur J Cancer. 2014;50(8):1462–71. https://doi.org/10.1016/j.ejca.2014.02.018.
Graillon T, Cuny T, Castinetti F, Courbiere B, Cousin M, Albarel F, et al. Surgical indications for pituitary tumors during pregnancy: a literature review. Pituitary. 2020;23(2):189–99. https://doi.org/10.1007/s11102-019-01004-3.
Dietrich J, Rao K, Pastorino S, Kesari S. Corticosteroids in brain cancer patients: benefits and pitfalls. Expert Rev Clin Pharmacol. 2011;4(2):233–42. https://doi.org/10.1586/ecp.11.1.
Schiff D, Lee EQ, Nayak L, Norden AD, Reardon DA, Wen PY. Medical management of brain tumors and the sequelae of treatment. Neuro-Oncology. 2015;17(4):488–504. https://doi.org/10.1093/neuonc/nou304.
Wapner RJ, Sorokin Y, Mele L, Johnson F, Dudley DJ, Spong CY, et al. Long-term outcomes after repeat doses of antenatal corticosteroids. N Engl J Med. 2007;357(12):1190–8. https://doi.org/10.1056/NEJMoa071453.
Morsi A, DeFranco D, Witchel SF. The hypothalamic-pituitary-adrenal axis and the fetus. Horm Res Paediatr. 2018;89(5):380–7. https://doi.org/10.1159/000488106.
Brosnan PG. The hypothalamic pituitary axis in the fetus and newborn. Semin Perinatol. 2001;25(6):371–84. https://doi.org/10.1053/sper.2001.29038.
Bain MD, Copas DK, Landon MJ, Stacey TE. In vivo permeability of the human placenta to inulin and mannitol. J Physiol. 1988;399:313–9. https://doi.org/10.1113/jphysiol.1988.sp017082.
Kazemi P, Villar G, Flexman AM. Anesthetic management of neurosurgical procedures during pregnancy: a case series. J Neurosurg Anesthesiol. 2014;26(3):234–40. https://doi.org/10.1097/ANA.0000000000000029.
Veroniki AA, Cogo E, Rios P, Straus SE, Finkelstein Y, Kealey R, et al. Comparative safety of anti-epileptic drugs during pregnancy: a systematic review and network meta-analysis of congenital malformations and prenatal outcomes. BMC Med. 2017;15(1):95. https://doi.org/10.1186/s12916-017-0845-1.
Christianne Lok MD, PhD. Surgery during pregnancy. In: Oncology TEVoG, editor. Textbook of Cancer in Pregnancy. 2017. p. 25 - 8.
Ancel PY, Goffinet F, Group E-W, Kuhn P, Langer B, Matis J, et al. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015;169(3):230–8. https://doi.org/10.1001/jamapediatrics.2014.3351.
Manuck TA, Rice MM, Bailit JL, Grobman WA, Reddy UM, Wapner RJ, et al. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol. 2016;215(1):103 e1–e14. https://doi.org/10.1016/j.ajog.2016.01.004.
Su TM, Lan CM, Yang LC, Lee TC, Wang KW, Hung KS. Brain tumor presenting with fatal herniation following delivery under epidural anesthesia. Anesthesiology. 2002;96(2):508–9. https://doi.org/10.1097/00000542-200202000-00041.
Rodrigues AJ, Waldrop AR, Suharwardy S, Druzin ML, Iv M, Ansari JR, et al. Management of brain tumors presenting in pregnancy: a case series and systematic review. Am J Obstet Gynecol MFM. 2021;3(1):100256. https://doi.org/10.1016/j.ajogmf.2020.100256.
Yust-Katz S, de Groot JF, Liu D, Wu J, Yuan Y, Anderson MD, et al. Pregnancy and glial brain tumors. Neuro-Oncology. 2014;16(9):1289–94. https://doi.org/10.1093/neuonc/nou019.
Mallari RJ, Thakur JD, Griffiths C, Krauss H, Eisenberg A, Barkhoudarian G, et al. Tuberculum sellae meningiomas in pregnancy: 3 cases treated in the second trimester and literature review. World Neurosurg. 2020;143:268–75. https://doi.org/10.1016/j.wneu.2020.07.198.
International Commission on Radiological P. Pregnancy and medical radiation. Ann ICRP. 2000;30(1):iii-viii, 1-43. https://doi.org/10.1016/s0146-6453(00)00037-3.
Philip Poortmans M, PhD, Orit Kaidar-Person, MD, Helene Masset, PhD, MSc, Elzbieta Lampka, MD. Radiotherapy during Pregnancy. In: Oncology TEVoG, editor. Textbook of Cancer in Pregnancy. INCIP; International Network of Cancer, Infertility and Pregnancy; 2017. p. 17 - 24.
Committee on Obstetric P. Committee Opinion No. 723: Guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 2017;130(4):e210-e2e6. doi:https://doi.org/10.1097/AOG.0000000000002355.
Mervak BM, Altun E, McGinty KA, Hyslop WB, Semelka RC, Burke LM. MRI in pregnancy: indications and practical considerations. J Magn Reson Imaging. 2019;49(3):621–31. https://doi.org/10.1002/jmri.26317.
Anic GM, Madden MH, Nabors LB, Olson JJ, LaRocca RV, Thompson ZJ, et al. Reproductive factors and risk of primary brain tumors in women. J Neuro-Oncol. 2014;118(2):297–304. https://doi.org/10.1007/s11060-014-1427-0.
Johnson N, Sermer M, Lausman A, Maxwell C. Obstetric outcomes of women with intracranial neoplasms. Int J Gynaecol Obstet. 2009;105(1):56–9. https://doi.org/10.1016/j.ijgo.2008.11.037.
Owens MA, Craig BM, Egan KM, Reed DR. Birth desires and intentions of women diagnosed with a meningioma. J Neurosurg. 2015;122(5):1151–6. https://doi.org/10.3171/2014.11.JNS14522.
Custer B, Longstreth WT Jr, Phillips LE, Koepsell TD, Van Belle G. Hormonal exposures and the risk of intracranial meningioma in women: a population-based case-control study. BMC Cancer. 2006;6:152. https://doi.org/10.1186/1471-2407-6-152.
Daniels K, Abma JC. Current contraceptive status among women aged 15-49: United States, 2017-2019. NCHS Data Brief. 2020(388):1–8.
Michaud DS, Gallo V, Schlehofer B, Tjonneland A, Olsen A, Overvad K, et al. Reproductive factors and exogenous hormone use in relation to risk of glioma and meningioma in a large European cohort study. Cancer Epidemiol Biomark Prev. 2010;19(10):2562–9. https://doi.org/10.1158/1055-9965.EPI-10-0447.
Jhawar BS, Fuchs CS, Colditz GA, Stampfer MJ. Sex steroid hormone exposures and risk for meningioma. J Neurosurg. 2003;99(5):848–53. https://doi.org/10.3171/jns.2003.99.5.0848.
Benson VS, Pirie K, Green J, Bull D, Casabonne D, Reeves GK, et al. Hormone replacement therapy and incidence of central nervous system tumours in the Million Women Study. Int J Cancer. 2010;127(7):1692–8. https://doi.org/10.1002/ijc.25184.
Cea-Soriano L, Wallander MA, Garcia Rodriguez LA. Epidemiology of meningioma in the United Kingdom. Neuroepidemiology. 2012;39(1):27–34. https://doi.org/10.1159/000338081.
Lee E, Grutsch J, Persky V, Glick R, Mendes J, Davis F. Association of meningioma with reproductive factors. Int J Cancer. 2006;119(5):1152–7. https://doi.org/10.1002/ijc.21950.
Korhonen K, Raitanen J, Isola J, Haapasalo H, Salminen T, Auvinen A. Exogenous sex hormone use and risk of meningioma: a population-based case-control study in Finland. Cancer Causes Control. 2010;21(12):2149–56. https://doi.org/10.1007/s10552-010-9634-2.
Alderman CP. Probable drug-related meningioma detected during the course of medication review services. Consult Pharm. 2016;31(9):500–4. https://doi.org/10.4140/TCP.n.2016.500.
Champagne PO, Passeri T, Froelich S. Combined hormonal influence of cyproterone acetate and nomegestrol acetate on meningioma: a case report. Acta Neurochir. 2019;161(3):589–92. https://doi.org/10.1007/s00701-018-03782-4.
Gil M, Oliva B, Timoner J, Macia MA, Bryant V, de Abajo FJ. Risk of meningioma among users of high doses of cyproterone acetate as compared with the general population: evidence from a population-based cohort study. Br J Clin Pharmacol. 2011;72(6):965–8. https://doi.org/10.1111/j.1365-2125.2011.04031.x.
O'Shea T, Crowley RK, Farrell M, MacNally S, Govender P, Feeney J, et al. Growth of a progesterone receptor-positive meningioma in a female patient with congenital adrenal hyperplasia. Endocrinol Diabetes Metab Case Rep. 2016;2016. https://doi.org/10.1530/EDM-16-0054.
Peyre M, Gaillard S, de Marcellus C, Giry M, Bielle F, Villa C, et al. Progestin-associated shift of meningioma mutational landscape. Ann Oncol. 2018;29(3):681–6. https://doi.org/10.1093/annonc/mdx763.
Bernat AL, Oyama K, Hamdi S, Mandonnet E, Vexiau D, Pocard M, et al. Growth stabilization and regression of meningiomas after discontinuation of cyproterone acetate: a case series of 12 patients. Acta Neurochir. 2015;157(10):1741–6. https://doi.org/10.1007/s00701-015-2532-3.
Botella C, Coll G, Lemaire JJ, Irthum B. Intra cranial meningiomas and long term use of cyproterone acetate with a conventional dose in women. A report of two cases of tumor decrease after treatment withdrawal. Neurochirurgie. 2015;61(5):339–42. https://doi.org/10.1016/j.neuchi.2015.05.002.
Cebula H, Pham TQ, Boyer P, Froelich S. Regression of meningiomas after discontinuation of cyproterone acetate in a transsexual patient. Acta Neurochir. 2010;152(11):1955–6. https://doi.org/10.1007/s00701-010-0787-2.
Kalamarides M, Peyre M. Dramatic shrinkage with reduced vascularization of large meningiomas after cessation of progestin treatment. World Neurosurg. 2017;101:814 e7–e10. https://doi.org/10.1016/j.wneu.2017.03.013.
Weill ANP, Yoldjian I, Fontanel S, Froelich S, Coste J. Exposition prolongée à de fortes doses d’acétate de cyprotérone et risque de méningiome chez la femme : une recherche-action de santé publique en France. Rev Epidemiol Sante Publique. 2020;68(March 2020):S3–4. https://doi.org/10.1016/j.respe.2020.01.004.
Passeri T, Champagne PO, Bernat AL, Hanakita S, Salle H, Mandonnet E, et al. Spontaneous regression of meningiomas after interruption of nomegestrol acetate: a series of three patients. Acta Neurochir. 2019;161(4):761–5. https://doi.org/10.1007/s00701-019-03848-x.
Mahajan DK, London SN. Mifepristone (RU486): a review. Fertil Steril. 1997;68(6):967–76. https://doi.org/10.1016/s0015-0282(97)00189-1.
Grunberg SM, Weiss MH, Spitz IM, Ahmadi J, Sadun A, Russell CA, et al. Treatment of unresectable meningiomas with the antiprogesterone agent mifepristone. J Neurosurg. 1991;74(6):861–6. https://doi.org/10.3171/jns.1991.74.6.0861.
Piper JG, Follett KA, Fantin A. Sphenoid wing meningioma progression after placement of a subcutaneous progesterone agonist contraceptive implant. Neurosurgery. 1994;34(4):723–5; discussion 5. https://doi.org/10.1227/00006123-199404000-00022.
Zairi F, Aboukais R, LER E, Marinho P, Maurage CA, Lejeune JP. Close follow-up after discontinuation of cyproterone acetate: a possible option to defer surgery in patients with voluminous intracranial meningioma. J Neurosurg Sci. 2017;61(1):98–101. https://doi.org/10.23736/S0390-5616.16.03243-4.
Ossewaarde ME, Bots ML, Verbeek AL, Peeters PH, van der Graaf Y, Grobbee DE, et al. Age at menopause, cause-specific mortality and total life expectancy. Epidemiology. 2005;16(4):556–62. https://doi.org/10.1097/01.ede.0000165392.35273.d4.
Hing E, Brett KM. Changes in U.S. prescribing patterns of menopausal hormone therapy, 2001-2003. Obstet Gynecol. 2006;108(1):33–40. https://doi.org/10.1097/01.AOG.0000220502.77153.5a.
Qi ZY, Shao C, Huang YL, Hui GZ, Zhou YX, Wang Z. Reproductive and exogenous hormone factors in relation to risk of meningioma in women: a meta-analysis. PLoS One. 2013;8(12):e83261. https://doi.org/10.1371/journal.pone.0083261.
Huang K, Whelan EA, Ruder AM, Ward EM, Deddens JA, Davis-King KE, et al. Reproductive factors and risk of glioma in women. Cancer Epidemiol Biomark Prev. 2004;13(10):1583–8.
Hatch EE, Linet MS, Zhang J, Fine HA, Shapiro WR, Selker RG, et al. Reproductive and hormonal factors and risk of brain tumors in adult females. Int J Cancer. 2005;114(5):797–805. https://doi.org/10.1002/ijc.20776.
Benson VS, Pirie K, Green J, Casabonne D, Beral V. Million Women Study C. Lifestyle factors and primary glioma and meningioma tumours in the Million Women Study cohort. Br J Cancer. 2008;99(1):185–90. https://doi.org/10.1038/sj.bjc.6604445.
Claus EB, Black PM, Bondy ML, Calvocoressi L, Schildkraut JM, Wiemels JL, et al. Exogenous hormone use and meningioma risk: what do we tell our patients? Cancer. 2007;110(3):471–6. https://doi.org/10.1002/cncr.22783.
Biglia N, Gadducci A, Ponzone R, Roagna R, Sismondi P. Hormone replacement therapy in cancer survivors. Maturitas. 2004;48(4):333–46. https://doi.org/10.1016/j.maturitas.2003.09.031.
Ettinger B, Barrett-Connor E, Hoq LA, Vader JP, Dubois RW. When is it appropriate to prescribe postmenopausal hormone therapy? Menopause. 2006;13(3):404–10. https://doi.org/10.1097/01.gme.0000188735.61994.5b.
Deli T, Orosz M, Jakab A. Hormone replacement therapy in cancer survivors - review of the literature. Pathol Oncol Res. 2020;26(1):63–78. https://doi.org/10.1007/s12253-018-00569-x.
Goldrat O, Kroman N, Peccatori FA, Cordoba O, Pistilli B, Lidegaard O, et al. Pregnancy following breast cancer using assisted reproduction and its effect on long-term outcome. Eur J Cancer. 2015;51(12):1490–6. https://doi.org/10.1016/j.ejca.2015.05.007.
Bergoglio MT, Gomez-Balaguer M, Almonacid Folch E, Hurtado Murillo F, Hernandez-Mijares A. Symptomatic meningioma induced by cross-sex hormone treatment in a male-to-female transsexual. Endocrinol Nutr. 2013;60(5):264–7. https://doi.org/10.1016/j.endonu.2012.07.004.
Gazzeri R, Galarza M, Gazzeri G. Growth of a meningioma in a transsexual patient after estrogen-progestin therapy. N Engl J Med. 2007;357(23):2411–2. https://doi.org/10.1056/NEJMc071938.
Deipolyi AR, Han SJ, Parsa AT. Development of a symptomatic intracranial meningioma in a male-to-female transsexual after initiation of hormone therapy. J Clin Neurosci. 2010;17(10):1324–6. https://doi.org/10.1016/j.jocn.2010.01.036.
Mancini I, Rotilio A, Coati I, Seracchioli R, Martelli V, Meriggiola MC. Presentation of a meningioma in a transwoman after nine years of cyproterone acetate and estradiol intake: case report and literature review. Gynecol Endocrinol. 2018;34(6):456–9. https://doi.org/10.1080/09513590.2017.1395839.
Ter Wengel PV, Martin E, Gooren L, Den Heijer M, Peerdeman SM. Meningiomas in three male-to-female transgender subjects using oestrogens/progestogens and review of the literature. Andrologia. 2016;48(10):1130–7. https://doi.org/10.1111/and.12550.
Carroll RS, Zhang J, Black PM. Expression of estrogen receptors alpha and beta in human meningiomas. J Neuro-Oncol. 1999;42(2):109–16. https://doi.org/10.1023/a:1006158514866.
Author information
Authors and Affiliations
Contributions
Serena Girardelli: conceptualization, methodology, investigation, resources, analysis and interpretation of data, and writing—original draft. Luigi Albano: conceptualization, methodology, investigation, resources, analysis and interpretation of data, and writing—original draft. Giorgia Mangili: conceptualization, supervision, and writing—reviewing and editing. Luca Valsecchi: visualization and writing—reviewing and editing. Emanuela Rabaiotti: visualization and writing—reviewing and editing. Paolo Cavoretto: visualization and writing—reviewing and editing. Pietro Mortini: writing—reviewing and editing. Massimo Candiani: writing—reviewing and editing.
Corresponding author
Ethics declarations
Ethical Standards
No procedures on humans and/or animals were performed during in this study. For this type of study, our institution’s review board has confirmed that formal consent is not required.
Consent for Publication
All authors have provided consent for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Serena Girardelli and Luigi Albano are joint first authorship.
Rights and permissions
About this article
Cite this article
Girardelli, S., Albano, L., Mangili, G. et al. Meningiomas in Gynecology and Reproduction: an Updated Overview for Clinical Practice. Reprod. Sci. 29, 2452–2464 (2022). https://doi.org/10.1007/s43032-021-00606-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00606-2