Abstract
Splenic ectopic pregnancy is extremely rare but carries a high risk of uncontrollable life-threatening bleeding. Our aim is to try to diagnose those cases earlier and to include splenic preservation as good alternative for selected cases. Extensive review of the literature has been performed. Thirty-one case reports were identified, of which 4 have been excluded because they were not written in English. A 36-year-old woman presented to the Emergency Department with haemorrhagic shock. Despite the levonorgestrel intrauterine system (LNG-IUS) being in situ for 4 months, urinary and serum tests were both positive for pregnancy, and an ultrasound scan revealed haemoperitoneum suggestive of a ruptured ectopic pregnancy. An emergency Pfannenstiel laparotomy was performed and a diagnosis of spontaneous tubal abortion was made and the abdomen was subsequently closed. Following a period of cardiovascular instability on the Intensive Care Unit postoperatively, an urgent CT scan was performed which revealed bleeding from the spleen. A midline laparotomy was performed by the general surgeon, which involved resection of the gestational sac and splenorrhaphy. Twenty-seven cases were reviewed, and 73% of them presented as an emergency and 21 cases (81%) had been managed with splenectomy. CT scan had been used in eight of the previous case reports of splenic ectopic pregnancy with 100% diagnostic accuracy rate. Non-tubal ectopic pregnancies are very rare. Splenorrhaphy is a safe alternative to splenectomy in cases of splenic ectopic pregnancy. CT abdomen and pelvis with intravenous contrast can be very helpful in relatively stable patients with a vaginal ultrasound demonstrating an empty uterus, no clear adnexal masses or free fluid.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ectopic pregnancy is defined as the implantation of a fertilised ovum outside the uterine cavity. The rate of ectopic pregnancy is 11 per 1000 pregnancies, with a maternal mortality of 0.2 per 1000 estimated ectopic pregnancies [1]. The usual site of ectopic implantation is within the fallopian tube, accounting for 95.5% of all ectopic gestations. Although rare, extra tubal pregnancies represent some of the most serious complications of pregnancy [2]. In these cases, the gestational sac can be implanted in the omentum, abdominal vital organs, or large vessels. It can be described as either primary [3], due to a failure of the fimbria to pick up the ovulated follicle, or secondary, when it is caused by early rupture or abortion of a tubal pregnancy or uterine perforation of an intrauterine pregnancy into the peritoneal cavity [4]. Abdominal ectopic pregnancy accounts for about 1.3% of all ectopic pregnancies. The spleen is one of the rarest sites for abdominal pregnancies with only 31 cases of primary splenic pregnancy having been reported worldwide, 27 of which have been documented in the English literature to date.
Ectopic pregnancy still accounts for 4 to 10% of pregnancy-related deaths, despite current advances in prenatal imaging and care [5]. The maternal death rate in cases of abdominal ectopic pregnancies is of 5.1 per 1,000 pregnancies [6]. Regarding the splenic site of ectopic implantation, the mortality rate is unknown, due to a publication bias and low reported case numbers in current literature.
We report a case of splenic ectopic pregnancy complicated by haemoperitoneum, which was diagnosed on CT scan after an initial negative laparotomy. Extensive review of the literature has been performed. Thirty-one case reports were identified, of which 4 have been excluded because they were not written in English.
Case Report
A 36-year-old-female presented to the Emergency Department following an episode of syncope, plus bilateral flank and right shoulder tip pain.
She had been feeling lethargic for the last 4 days at home. She has been avoiding attending the hospital due to the COVID-19 pandemic lockdown. On the day of presentation, she had developed pain in the abdomen, was unable to get out of the bed and, when tried, had a syncopal episode.
She was previously fit and well with no significant past medical history. She was G3P2 and had the LNG-IUS fitted in the community for contraception 4 months prior to admission. Her last menstrual period 2 months previously and she accepted this amenorrhoea as being due to the insertion of the IUS.
On clinical examination, she appeared pale and peripherally shut down, with a pulse rate of 120/min and blood pressure of 85/50 mmHg. Her abdomen was soft, non-distended but tender in bilateral flanks. A urinary pregnancy test was positive and serum beta-human chorionic gonadotropin (ß-hCG) levels were raised at 3139 miU/ml. A transvaginal ultrasound was carried out by the gynaecologist and showed the presence of the LNG-IUS low in the uterus with no intrauterine pregnancy and free fluid in the pelvis and abdomen.
A diagnosis of a ruptured ectopic pregnancy was made and she was taken to theatre immediately for exploratory laparotomy with a Pfannenstiel incision. On exploration, 2 l of blood was evacuated from the abdomen and both fallopian tubes, ovaries and other pelvic organs were carefully examined. The fallopian tubes were intact with normal ovaries; however, the right fallopian tube was slightly hyperaemic as compared to the left. The inferior surfaces of the spleen and liver were visualised and they were found to be intact with no evidence of bleeding. After washout of the abdominal cavity with warm saline, no evidence of further bleeding was noted.
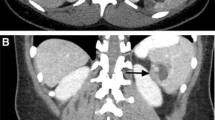
Due to the hyperaemia noted in the right fallopian tube, a diagnosis of spontaneous tubal abortion was made and the abdomen was closed with a pelvic drain in situ. Two units of packed red blood cells were transfused intraoperatively and she was transferred to the Critical Care Unit for close monitoring, where a further 2 units of blood were administered. A high output of fresh red blood was noted in the pelvic drain, and persistent hypotension prompted the commencement of peripheral vasopressors and urgent review by the gynaecologist. A CT scan of the abdomen and pelvis with intravenous contrast showed active bleeding with linear contrast extravasation (Fig. 1) from the small oval low density “defect” at the posterior side of the spleen with haemoperitoneum in the parasplenic space. The CT scan also showed an incidental finding of horseshoe/arcuate kidneys with the lower end of both kidneys fused together.
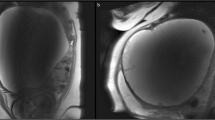
The case was discussed with the general surgeon on call and the patient returned to theatre urgently for a splenectomy due to a possible diagnosis of splenic ectopic pregnancy. The abdomen was explored with an upper midline incision and disclosed 1500 ml of intraperitoneal free blood with masses of clots in the left upper abdomen. The spleen was noted to be hypermobile and showed a 3 × 3-cm ruptured sac on its posteroinferior surface (Fig. 2) which was oozing arterial blood. As the lesion was located at the periphery of the spleen, wedge resection was performed using electrocautery. The surface of the spleen was further secured with TachosilTM (sealant matrix coated with fibrinogen and thrombin) and both surfaces of the wedge were approximated with 2-0 Maxon™ (monofilament polyglyconate synthetic absorbable sutures) atraumatic needle suture using horizontal mattress technique. Excellent haemostasis was achieved and the abdomen was closed after washout with insertion of a drain in the perisplenic region (Fig. 3).
A further 2 units of packed red blood cells, 2 units of fresh frozen plasma and 2 units of platelets were administered intraoperatively. Postoperatively, the patient was again transferred to the Critical Care Unit for monitoring, before being stepped down to the surgical ward 2 days later where the rest of her recovery was uneventful. ß-hCG levels fell to 656.7 mIu/ml 15 h after the initial presentation (Fig. 4). The pelvic drain was removed on day 3 and the patient was discharged on day 4 post-operation. She was followed up in the outpatients’ clinic afterwards and had an uneventful recovery at home.
Histopathology of the resected spleen showed numerous chorionic villi and decidua invading the splenic parenchyma. Pathology showed a fragment of haemorrhagic splenic tissue measuring 23 × 20 × 17 mm, with focal capsular disruption. Inside this capsular defect was a small amount of adherent blood clot and an irregular capsular projection. On sectioning, there was a corresponding well-delineated but non-encapsulated spherical nodule of cystic, soft, and haemorrhagic red-brown to focally tan grey soft tissue.
Microscopic examination of the haemorrhagic nodule showed splenic parenchyma with capsular disruption. Underlying the disruption were numerous chorionic villi and intermediate trophoblasts infiltrating the spleen (Fig. 3); thus, a confirmed diagnosis of primary splenic ectopic pregnancy was made.
Discussion
A young female of reproductive age presenting to the Emergency Department with secondary amenorrhea, abdominal pain and shock is predominantly considered to be a ruptured ectopic pregnancy. This picture is becoming less frequent in Western countries in recent times, due to the early gynaecological consultation with serial serum hCG levels and advances in sonographic technology. However, ectopic pregnancy contributes to 80% of maternal deaths that occur in the first trimester, and these deaths occur predominantly in abdominal pregnancies. The risk factors, signs and symptoms of a ruptured abdominal pregnancy are no different to a ruptured tubal ectopic and this poses diagnostic challenges in a haemodynamically unstable patient. Deaths with significant haemorrhages reach up to 3% in abdominal gestations [1]. Hence, a high index of suspicion is essential to recognise the implantation site of ectopic pregnancy. Early diagnosis and effective treatment are critical to avoid significant maternal mortality.
Numerous factors are known to increase the risk of an ectopic pregnancy, including endometriosis, previous pelvic surgery, reproductive assistance, a history of pelvic inflammatory disease and previous ectopic pregnancy [7]. In our case, the patient had the LNG-IUS in situ but it was situated low in the cavity. The LNG-IUS is a hormonal IUD which provides highly effective, long-term, safe and reversible contraception. The cumulative pregnancy rate for LNG-IUS is quoted as 0.1% at 1 year and 0.5% at 5 years [8]. Unlike copper intrauterine devices, which do not affect the menstrual cycle pattern, amenorrhoea and irregular bleeding patterns are expected side effects of LNG-IUS. In our literature review, we identified that 8% of the early abdominal ectopic pregnancies occurred with an intrauterine device (IUD) in place [6] and approximately 15% of the historical splenic implantation had an IUD.
Surgery is usually the way to manage ectopic pregnancy in women presenting with signs of an acute abdomen and hypovolemic shock. It may be provided either through laparotomy or by laparoscopic approach. Laparoscopy has become the recommended route in most cases. Laparotomy is usually reserved for patients who are haemodynamically unstable. Midline laparotomy is considered to be a preferred surgical approach in a patient with haemoperitoneum of unknown source as it provides quick access to the whole abdomen. However, midline laparotomies carry up to 20% long-term risk of incisional hernia [9]. Subsequently, due to the low chance of having an extra pelvic ectopic pregnancy and its multiple advantages regarding pain, cosmetics and herniation risk, transverse lower abdominal incision as Pfannenstiel is favoured.
The spleen cannot accommodate placental attachment or a growing embryo; therefore, splenic pregnancy tends to present earlier than the other abdominal ectopic pregnancies, mostly presenting with acute abdomen and haemoperitoneum occurring at 6–8 weeks’ gestation. It is a challenging diagnosis due its low incidence but it can be considered in patients who have a positive pregnancy test without confirmation of intrauterine or pelvic pregnancy because of its pronounced likelihood of rupture and mortality. Nevertheless, no mortality has been reported yet in such a dangerous condition, and this may be related to misdiagnosis as a spontaneous splenic rupture and publication bias in not reporting fatal outcomes in patients who reach a medical centre.
Ultrasound has been widely used in patients with suspected abdominal ectopic pregnancy. A few cases of splenic pregnancy have been diagnosed by ultrasound alone but all of those were stable patients and the majority of them presented before the rupture of the ectopic pregnancy (Table 1). Computed tomography scan is the most reliable investigation to diagnose such rare cases and should be considered in all stable patients where ultrasound failed to demonstrate the tubal pregnancy with absent intrauterine pregnancy. CT scan had been used in eight of the previous case reports of splenic ectopic pregnancy with 100% diagnostic accuracy rate.
Partial splenectomy requires technical skill as well as precise judgement for patient selection. A partial splenectomy, or splenorrhaphy, requires at least one-third of viable splenic tissue. Essential steps are atraumatic mobilization of spleen, temporary splenic artery occlusion avoiding injury to pancreatic parenchyma, the use of haemostatic agents such as absorbable fibrin sealant patch (TachosilTM) and the use of absorbable meshes. This approach enables spleen-preserving surgery, making it a feasible and reproducible procedure and an alternative to classical splenectomy.
Splenic preservation in patients with blunt splenic injury by operative or non-operative treatment is established in current surgical practice leading to lower early infection rates in adults and, therefore, could be encouraged to treat ruptured splenic pregnancies [35]. In the very scarce elective situations or in haemodynamically stable patients, radiologically guided splenic artery embolization (SAE) could be attempted, either proximal or selective [34], depending on the location of the embryo. Of the 27 cases of splenic ectopic pregnancy reviewed in the literature (Table 1), 73% presented as an emergency and 21 cases (81%) had been managed with splenectomy. Three cases had been treated conservatively following diagnosis with a combination of intramuscular methotrexate injections with embolization or intra-gestational sac injection being performed in the other 2 cases [26, 34]. Two cases were managed with splenorrhaphy [24, 30].
Although splenectomy appeared to be the most favourable treatment option for the reported cases of splenic ectopic pregnancies, especially in those who presented with intraperitoneal haemorrhage, our successful experience demonstrates that splenic preservation should be considered when possible.
In conclusion, non-tubal ectopic pregnancies are very rare, abdominal implantations even more so. However, in cases of elevated ß-hCG, an empty uterus and normal pelvic findings, a high index of suspicion will have to be exercised for evaluation of the spleen as a potential site of implantation. Diagnosis of such exceptional cases can be augmented with the addition of a CT scan if the patient’s condition allows. Surgical exploration through a laparotomy may be the best choice in a patient with a massive haemoperitoneum who is haemodynamically unstable. However, this case highlights the need for prompt resuscitation, avoiding unnecessary delay in diagnosis and a multidisciplinary team working in such complex situations. Splenic preservation should be considered if technically feasible. Such patients will need careful counselling advice with regard to future pregnancies and contraceptive choices.
References
Overview | Ectopic pregnancy and miscarriage: diagnosis and initial management | Guidance | NICE [Internet]. NICE; [cited 2020 Apr 19]. Available from: https://www.nice.org.uk/guidance/ng126
Stucki D, Buss J. The ectopic pregnancy, a diagnostic and therapeutic challenge. J Med Life. 2008;1(1):40–8.
Studdiford WE. Primary peritoneal pregnancy. Am J Obstet Gynecol. 1942;44(3):487–91.
Xu Y, Xiao S, Liu W. Splenic hilum pregnancy with a live fetus: a case report and review of literature. Int J Clin Exp Med. 2018;11(4):4330–4332:3.
Marion LL, Meeks GR. Ectopic pregnancy: history, incidence, epidemiology, and risk factors. Clin Obstet Gynecol. 2012;55(2):376–86.
Poole AT, Poole A, Haas D, Magann EF. Early abdominal ectopic pregnancies: a systematic review of the literature. Gynecol Obstet Investig. 2012;74(4):249–60.
Yagil Y, Beck-Razi N, Amit A, Kerner H, Gaitini D. Splenic pregnancy: the role of abdominal imaging. J Ultrasound Med. 2007;26(11):1629–32.
The ESHRE Capri Workshop Group. Intrauterine devices and intrauterine systems. Hum Reprod Update. 2008;14(3):197–208.
Burger JWA, van’t Riet M, Jeekel J. Abdominal incisions: techniques and postoperative complications. Scand J Surg. 2002;91(4):315–21.
Mankodi RC, Sankari K, Bhatt SM. Primary splenic pregnancy. BJOG Int J Obstet Gynaecol. 1977;84(8):634–5.
Reddy KSP, Modgill VK. Intraperitoneal bleeding due to primary splenic pregnancy. BJS Br J Surg. 1983;70(9):564–4.
Huber DE, Martin SD, Orlay G. A case report of splenic pregnancy. Aust N Z J Surg. 1984;54(1):81–2.
Caruso V, Hall WHJ. Primary abdominal pregnancy in the spleen: a case report. Pathology (Phila). 1984;16(1):93–4.
Tantachamroon T, Songkrobhan S, Tuppasut NK. Primary splenic pregnancy. J Med Assoc Thail Chotmaihet Thangphaet. 1986;69(9):495–9.
Yackel DB, Panton ONM, Martin DJ, Lee D. Splenic pregnancy—case report. Obstet Gynecol. 1988;71(3):471–2.
Larkin JK, Garcia DM, Paulson EL, Powers DW. Primary splenic pregnancy with intraperitoneal bleeding and shock: a case report. Iowa Med J Iowa Med Soc. 1988;78(11):529–30.
Kahn JA, Skjeldestad FE, Düring VV, Sunde A, Molne K, Jørgensen OG. A spleen pregnancy. Acta Obstet Gynecol Scand. 1989;68(1):83–4.
Cormio G, Santamato S, Vimercati A, Selvaggi L. Primary splenic pregnancy. A case report. J Reprod Med. 2003;48(6):479–81.
Kalof AN, Fuller B, Harmon M. Splenic pregnancy: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:3.
Kitade M, Takeuchi H, Kikuchi I, Shimanuki H, Kumakiri J, Kinoshita K. A case of simultaneous tubal-splenic pregnancy after assisted reproductive technology. Fertil Steril. 2005;83(4):1042.e19–21.
Aguh CJ, Salihu HM, Buckley A, Imegwu O, Ryave S, Yang RS, et al. Acute abdomen with bones in the spleen. Arch Gynecol Obstet. 2007;276(4):375–8.
Biolchini F, Giunta A, Bigi L, Bertellini C, Pedrazzoli C. Emergency laparoscopic splenectomy for haemoperitoneum because of ruptured primary splenic pregnancy: a case report and review of literature. ANZ J Surg. 2010;80(1–2):55–7.
Julania S, Tai R. Heterotopic simultaneous splenic and intrauterine pregnancy after spontaneous conception and review of literature. J Obstet Gynaecol Res. 2013;39(1):367–70.
Siddiqui MNA, Islam MT, Siddiqua F, Sultana S, Siddique AB. Abdominal pregnancy implanted in the spleen: a case report. Anwer Khan Mod Med Coll J. 2011;2(2):36–8.
Zhang Y, Kang D, Zhang B, Yang L, Fan Z. Ectopic pregnancy causing splenic rupture. Am J Emerg Med. 2016;34(6):1184.e1–2.
Python JL, Wakefield BW, Kondo KL, Bang TJ, Stamm ER, Hurt KJ. Ultrasound-guided percutaneous management of splenic ectopic pregnancy. J Minim Invasive Gynecol. 2016;23(6):997–1002.
Greenbaum A, Miskimins R, Coffman B, Paul J. Management of splenic ectopic pregnancy presenting with massive haemoperitoneum. BMJ Case Rep. 2016;8:2016.
Klang E, Keddel N, Inbar Y, Rimon U, Amitai M. Splenic pregnancy: a new minimally invasive approach to treatment. Cardiovasc Intervent Radiol. 2016;39(9):1339–42.
Patil NR, Birare SD, Dale AR, Mahule SK. Splenic Gestation: a rare case report. Int J Reprod Contracept Obstet Gynecol. 2017;6(6):2670.
Thomas A, Srivastava N, Tintoiya I, Kumar S. Splenic pregnancy: a case report. J Obstet Gynaecol India. 2017;67(4):291–4.
Wu B-Q, Zhu F, Jiang Y, Sun D-L. Case of spontaneous splenic rupture caused by ectopic pregnancy in the spleen. J Obstet Gynaecol Res. 2017;43(11):1778–80.
Rathore R, Shilpi S, Chopra R, Nargotra N. Primary splenic pregnancy- a rare but imperative cause of hemoperitoneum - case report and review of literature. Turk Patoloji Derg. 2017;35(3):242–6.
Wu L, Jiang X, Ni J. Successful diagnosis and treatment of early splenic ectopic pregnancy. Medicine (Baltimore) [Internet]. 2018 Apr 27 [cited 2020 Apr 16];97(17). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5944564/
Goudeli C, Patramani S, Mytaras V, Psycharaki S, Karamani A, Makrigiannakis A. Non-operative management of splenic pregnancy with selective embolism and methotrexate. Eur J Obstet Gynecol Reprod Biol. 2019;234:e209.
Gauer J-M, Gerber-Paulet S, Seiler C, Schweizer WP. Twenty years of splenic preservation in trauma: lower early infection rate than in splenectomy. World J Surg. 2008;32(12):2730–5.
Author information
Authors and Affiliations
Contributions
A. Antequera: Manuscript writing. Z. Babar: Data collection or management. C. Balachandar: Manuscript editing and reviewing. K. Johal: Data analysis. M. Sapujiendeski: Images review. N. Qandil: Images review.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antequera, A., Babar, Z., Balachandar, C. et al. Managing Ruptured Splenic Ectopic Pregnancy Without Splenectomy: Case Report and Literature Review. Reprod. Sci. 28, 2323–2330 (2021). https://doi.org/10.1007/s43032-021-00476-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00476-8