Abstract
Elite athletes will compete in extreme heat more frequently as global land and sea temperatures increase, alongside more intense, frequent and longer duration heatwaves. Best practices to protect athlete health and performance during competition include heat acclimation/acclimatisation [(HA); i.e., long-term pre-competition preparation] complemented by pre-planned and practised cooling and hydration strategies (i.e., short-term interventions immediately before or during competition). This review explores elite athletes’ current behaviours and practices when preparing for competition in the heat and assesses the level of knowledge that has been exhibited by athletes and their practitioners in this space. Recommendations for future research, discussions of current best practices, and methods to improve translation of research into practice are provided. Available research focuses on small samples of elite endurance athletes during a selection of World Championship/Olympic/Paralympic events (~6% of competing athletes). While generally an increase in the adoption of evidence-based HA is seen chronologically from 2015 onwards, universal adoption is not seen. HA adoption is lowest in those who live/train in cold/temperate environments with cost and access to facilities/equipment being the most commonly reported barriers. Further research is required across the sporting landscape to fully characterise elite athlete behaviours and practices in these spaces. International federations and national governing bodies should continue their efforts to educate athletes and focus on regularly updated and reinvigorated release of evidence-based guidelines (in multiple germane languages) for competing in the heat, to increase the adoption of HA and other heat related best practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the 2023 annual climate update the World Meteorological Organisation (WMO) estimated that global temperatures are likely (likelihood: 66%) to increase 1.5 °C above pre-industrial levels before 2027 [113]. Inevitably, this affects the sport landscape (an increasingly global industry estimated to be worth $700 billion by 2026 [111]). Indeed, Tokyo 2020 was the hottest Olympic [67] and Paralympic [64] games on record, and Paris (Olympic and Paralympic Games host, 2024), not typically considered a hot climate, could see temperatures regularly exceed 30 °C during the Games, or even reach 40 °C should a heat wave similar to that observed in 2022 occur [42]. Heatwaves are increasing in their frequency, intensity and duration [18], with maximum land [106] and sea [24] temperature records being regularly broken. The World Aquatics Championships (open water swimming events) in Fukuoka in July 2023 saw water temperatures of 25.8 °C to 28.2 °C in the Open Water Swim events. The World Athletics Championships in Budapest (August 2023) saw ambient temperatures and humidity exceed 35 °C and 90% respectively [wet bulb globe temperatures (WBGT) ranged from 21 to 29.5 °C (data provided via personal communication with World Athletics)], comparable to the Tokyo Olympic Games 2020. The forthcoming World Athletics Championships (Tokyo September 2025) and the Summer Olympic and Paralympic Games (Los Angeles July 2028) will be held in hot summer climates. For context, the hottest temperature recorded on earth (54.4 °C; July 2021) was reported in Death Valley, California, less than 200 miles (~322 km) from the Olympic and Paralympic site [23]. Elite athletes will inevitably be faced with extreme heat at future events given the increased frequency, length and severity of heatwaves seen and forecast. Concerningly, such extreme heat-related competition environments now occur at events, and within seasons, where such extreme weather conditions are historically rare, or have not been seen before (e.g., Race Walking World Championships Muscat March 2022, historical data predicted race temperatures of ~22 to ~26 °C but reached 31.3 °C [33]). For the purposes of this review elite athletes are those competing at Tier Four (Elite/International Level) and/or Tier Five (World Class) level of the Participant Classification Framework [61].
The increase in global temperatures, especially heatwaves, has substantial implications for public health, leading to significant increases in heat related fatalities (>60,000 deaths have been attributed to heat during the 2022 summer heat wave in Europe [9]) and overwhelmed health systems [58]. Similarly, hot environments have detrimental health and performance effects on individuals engaged in regular physical activity, from recreational to elite athletes [108]. In hot, compared to temperate, environments, significant exercise-mediated rises in core (Tc) and/or skin (Tsk) temperature (Tc: ~2–2.5 °C [25], Tsk: ~5 °C [69]) occur alongside concomitant plasma volume loss and dehydration, increasing physiological and perceptual strain [69, 72, 105]. These responses combine to negatively affect physical [36, 69] and cognitive [57, 101] performance in the heat. High Tc in this scenario is also associated with an increased risk of exertional heat illness (EHI) and the potentially fatal exertional heat stroke (EHS [71]). EHS will be diagnosed when an individual presents a Tc ≥ 40.5 °C and profound neuropsychological impairment (i.e., altered mental status [11, 20, 40, 41, 51]). Elite endurance training provides a health protective effect against EHS. For example, even temperate-based elite endurance training induces a partially heat acclimated phenotype [3, 7, 35, 102] whilst elite endurance athletes who are heat acclimated/acclimatised can tolerate a Tc ≥ 41 °C without succumbing to EHS (i.e., no alteration in mental status [80, 84, 97]). Across various competition levels, intermittent sport athletes (386 individuals across 34 studies) have been observed to reach a peak Tc of 38.5 °C to 39.5 °C (24 of 34 studies included in a recent systematic review) and ≥ 39.5 °C (6 out of 34 studies [38]). Across intermittent and endurance sport competition and levels, 11.9% of athletes (1450 athletes from 49 studies) presented with a Tc ≥ 40 °C, with only 2.8% of these experiencing any EHI/EHS symptoms [91]. That said, it must be acknowledged that EHS can occur in any athlete, even within temperate environments, and this medical emergency remains one of the three leading causes of sudden death in sport [21, 115].
Unprecedented and previously unseen action has been taken at recent World Athletics Championships (midnight race starts at the World Championships Doha 2019; 5000 m heats moved from morning to evening session at Budapest 2023), Olympic Games (Tokyo 2020: marathon and racewalks moved from Tokyo to Sapporo and women’s soccer final stadium and time changed) and the FIFA World Cup (Qatar 2022 was moved from summer to winter) in an attempt to avoid extreme heat. Of these actions not all were successful, for example WBGT reached 30.6 °C [80] at Sapporo, with similar conditions in Tokyo [99]. Thus, athletes can and should control their own preparation (i.e., implement heat mitigation strategies) as even sensible policy/logistical changes do not always elicit desired effects (i.e., the environment is not controllable). It is true that international federations in tandem with local organising committees must do their utmost to place athlete health at the forefront of decision-making regarding competition locations and timings alongside event logistics (e.g., appropriate medical tent set up, size and medical staff; emergency cooling equipment and expertise to perform cold water immersion; access to ice; enough wheelchairs and other athlete transports measures; evidence-informed heat-related policies, etc. [3, 11, 21, 49, 63]) in an a priori manner to optimise the environment for safe performance. That said, extreme weather conditions are becoming increasingly unpredictable and exceeding historical maximums [18, 24, 106]. Therefore, alongside an optimised performance environment (e.g., logistics, timings, and locations, etc.) supporting ‘thrive’ rather than ‘survive’ competition, within event day flexible policies are also required (e.g., timings and locations of events) which do not disadvantage athlete preparations (some of which may have been planned out for several years) or performance—an evidently challenging and multi-faceted space to get policy correct within. For example, only 6 women at the 2023 World Athletics Championships in Budapest ran under the Olympic Marathon standard of 2:26:50 in the extreme heat seen [race start (7 a.m.): 23 °C, 75% humidity WBGT: 22 °C, first finisher: 29 °C, 75% humidity, WBGT: 29 °C)], even though 34 women had personal best times better than the Olympic marathon standard. To reduce the impact of the heat, midnight races were organised at IAAF Doha 2019, but the conditions remained very difficult (max: 32.7 °C, 80.6% humidity, 30.6 °C WBGT [80]). Clearly, this space continues to evolve alongside the increased likelihood of competition in extreme heat [18, 24, 106]. The solutions rely on all stakeholders’ collaborating to deliver evidence-informed policy [3, 11, 21, 49, 63], education [4, 33] and event-planning [81] related to competitions whilst athletes adopt gold-standard preparation [3, 35, 72, 76, 78, 81, 100, 103] and are helped to overcome barriers they may experience (e.g., access to facilities and expertise [4, 33]). Implementation of evidence-based practice as policy can impact the risk of EHI/EHS [27, 49]. Where policies have been introduced that mandate heat acclimation/acclimatisation (HA) alongside physical activity in the heat guidelines (by government and/or athletic governing bodies) the risk of EHI can be reduced from 35 to 100% depending on environmental conditions [27, 49].
Evidence-based optimal preparation for competition in the heat focuses on long- and/or short-term preparation strategies. Long-term preparation involves implementing a long-term HA strategy consisting of 10–14 days of consecutive passive and/or active heat exposures (for which there are a plethora of guidelines available [3, 35, 72, 76, 78, 81, 100, 103]). From this point forward, HA will be used when referring to heat acclimation/acclimatisation in general, whereas heat acclimation [use of an artificial hot environment (e.g., heat chamber, sauna, hot baths, overdressing)] or heat acclimatisation [naturally hot environment (e.g., hot climate)] will be used when referring to a specific strategy. Short-term heat mitigation strategies should be complementary to (not instead of) long term HA; long term-HA strategies are by far the most health protective and performance enhancing compared to short-term interventions [35]. Short-term approaches can include implementing a pre-planned and practiced nutritional/hydration strategy [12] and pre and/or per-cooling techniques [2, 98, 100]. Therefore, it would appear prudent for those operating within the elite athlete space (e.g., researchers and practitioners) to be aware of how athletes are preparing to compete in hot environments and whether they are adopting evidence-based best practice when implementing any strategies aimed at alleviating the physiological and perceptual strain of competing in heat [4, 33]. Understanding elite athlete knowledge of evidence-based practice and determining any barriers/challenges that prevent the adoption of these practices are also necessary to remain athlete centred and coach-/practitioner-led [4, 33]. Such understanding can also inform governing body and federation driven educational initiatives and resources for their stakeholders. From this point forward, when referring to practitioners, this is inclusive of all members of an inter-disciplinary team that support an athlete (e.g., sports science/medicine staff, coaches, etc.).
Several comprehensive evidence-based guidelines (and consensus statements) outline the clear benefits of heat mitigation strategies to alleviate the impact of heat on athlete health and performance (i.e., peak performance can only occur when health is optimised), albeit the majority of which are practitioner and athletic performance-focused (including but not limited to [35, 72, 76,77,78,79, 81, 100, 103]). However, only in the last decade has research investigated whether these guidelines are understood and/or implemented by elite athletes and/or their practitioners [6, 33, 74, 80, 85]. Therefore, it is the aim of this review to provide an overview of this research and outline the current state of elite athlete knowledge and adoption of evidence-based practice for competing in heat. In addition, this review will provide recommendations for best practice, future research, and what is required to improve the translation of research into practice among the elite athlete population.
This review will refer to several World Championship/Paralympic events with regularity and thus, these events will be referred to with abbreviations. The table below (Table 1) provides an overview of the key studies reviewed and the abbreviations used throughout this article.
Adoption of Heat Acclimation/Acclimatisation
HA is the optimal strategy to protect against the detrimental impact of heat on health and athletic performance [48, 78, 81]. The aim of implementing a HA strategy is to induce physiological adaptations (reduced resting and exercising heart rate, Tc and Tsk; increased sweat rate, decreased onset threshold for sweating, and increased blood and plasma volume [35, 73]) that attenuate heat strain during exercise. Therefore, determining the level of adoption of a dedicated HA strategy among elite athletes prior to competition in heat is paramount to identifying whether evidence-based practice is being implemented. Investigating any barriers/challenges that may inhibit elite athletes from adopting HA and providing recommendations for innovative and efficient strategies to elicit heat adaptations should also be prioritised.
Limited evidence of elite athlete use of HA prior to competition exists and, to date, has mainly focused on elite endurance athletes at World Championships [33, 74, 80, 85] with one study investigating HA adoption among paralympic athletes [6]. Table 2 provides an overview of the level of HA adoption at these championships where hot conditions were anticipated [temperatures across these competitions ranged from 19.5 to 32.7 °C (WBGT: 19.5 to 30.6 °C)]. In brief, the adoption of HA has increased since IAAF Beijing 2015 where 15% of surveyed athletes adopted a dedicated HA strategy [74] to 63% at IAAF Doha 2019 [80] (UCI Qatar 2016: 38% [85]; RWTC Muscat 2022: 57% [33]). Fifty-eight percent of paralympic athletes adopted a dedicated HA strategy, prior to the Tokyo Paralympics 2020; of those, only 45% had previously implemented a HA strategy at previous unspecified events [6]. This substantial increase in HA adoption from IAAF Beijing 2015 is likely due to increased education and awareness of evidence-based guidelines to protect athletes against the impairment of performance and risks posed to their health when competing in the heat.
Prior to IAAF Doha 2019, the IAAF [now World Athletics (WA)] released the ‘beat the heat’ pamphlet to all athletes, federations, and team doctors with similar initiatives implemented by the UCI, World Triathlon and the International Olympic Committee [(IOC) see Table 3 for full list]. Although, numbers of athletes/practitioners who read and/or specifically implemented the guidelines prior to these championships is unknown. Additionally, the majority of (if not all) educational material is published in English which, speculatively without specific data, may limit their impact within non-native English-speaking athletes, federations and/or those who have visual and intellectual disabilities. Significant media attention was paid to the extreme heat expected, alongside a plethora of research articles related to improving athletic performance in hot conditions in the build-up to IAAF Doha 2019 and the Tokyo 2020 Olympic and Paralympic Games (including but not limited to [13, 40, 46, 68]). Indeed, the British Journal of Sports Medicine published an open access series of editorials specifically focusing on the preparation of athletes for the Tokyo 2020 Olympic and Paralympic Games (see Table 3 for full list).
The translation of evidence from a scientific journal to athlete practice is somewhat limited [31] and may be an example of why adoption of HA is not universal. Indeed, passive dissemination strategies (i.e., provision of information in booklets) is often ineffective (especially if not in the readers native language and/or for those with visual and intellectual impairments), active participation during the provision of guidelines increases their implementation [90]. Alongside more accessible and palatable content a ‘hands-on’ active approach to educating elite sport practitioners and athletes needs to be made available to improve translation of research to practice [31, 90]. Combined, the increased attention and awareness of the impacts of competing in heat likely drove the increase in HA adoption from IAAF Beijing 2015 to IAAF Doha 2019. However, there was a small reduction (~6%) in HA adoption at the RWTC Muscat 2022 from IAAF Doha 2019 (3–4 years after the release of ‘beat the heat’). WA did not re-release the ‘beat the heat’ material from Doha 2019 prior to RWTC Muscat 2022, where 83% of athletes surveyed at RWTC Muscat 2022 were not aware of or had not read ‘beat the heat’ [33]. This, alongside less media attention and less extreme heat being anticipated, may have impacted the adoption of HA prior to RWTC Muscat 2022. Importantly, historical weather data suggested temperatures at these championships would be from 22.5 to 25.5 °C however, they reached up to 31.3 °C during the competition [33]. With the afore described increase in global temperatures and heatwaves, historical average weather data may be too low and athletes should be preparing for the record maximum temperatures in each location (even these are being regularly broken).
While it is encouraging to observe the increased adoption of HA in recent years, many athletes are still not adopting HA into practice. A self-reported survey of 55 elite athletes and 99 practitioners working with elite athletes identified a variety of significant barriers to adopting HA [4]. The cost (i.e., money required to live/train in a hot environment, or cost to access artificially hot environments) and access to facilities/equipment/expertise were the most commonly reported barriers to adopting HA [4], which were in agreement with HA adoption barriers reported at RWTC Muscat 2022 [33]. While funding may be seen as the most beneficial option to increase the adoption of HA, greater education (discussed in more detail below) of other possible low-cost and innovative strategies to achieve HA adaptations would likely increase the ability of athletes to achieve HA. For example, additional clothing [54, 94], and post-exercise/training sauna and hot water immersion [22, 37, 60], or simply having a treadmill/bike inside a camping tent/greenhouse with heaters (see Fig. 1—photos provided by author T. Stellingwerff), have proven effective in eliciting HA adaptations. Elite athletes may also struggle to implement a HA protocol within their training cycles [88]. In the build-up to major competitions athletes will generally complete a 4–6 week period of high volume/intensity training followed by a 1–2 week taper [88]. Adopting HA at the start of this intense block may lead to HA decay by the time of competition [28] and/or the quality of prescribed work being compromised [88]. HA during a taper or including heat exposures during the taper in a bid to re-induce adaptations that may have decayed [28] could (without careful consideration and prescription) disrupt the goals of the taper (i.e., reduced overall training load/stress) thus, adopting an evidence based ≥14 day HA protocol is challenging for the elite athlete and may be another barrier to its universal adoption [88]. The identified barriers to HA adoption [4, 33, 88] alongside the impact of the ‘beat the heat’ like material, highlights the importance of regular dissemination of the latest guidelines to athletes, national governing bodies, and practitioners to achieve universal adoption of HA prior to competing in heat.
Innovative low-cost strategy to induce HA adaptations (photos submitted by author T.Stellingwerff). Cycle ergometer and treadmill inside camping tents in a home garage with heaters (NB: athletes implementing these HA strategies should be supervised by qualified personnel at all times with tent temperature, thermal sensation and heart rate continually monitored. Ideally, body temperature measurement tools should also be used to avoid adverse health outcomes)
To date, there are minimal data on the specific HA strategies athletes use (e.g., acclimation vs. acclimatisation) and the specific HA protocols implemented (e.g., environmental temperatures, self-regulated vs. fixed intensity exercise). Heat acclimatisation (natural hot environment) appears to be most popular with elite endurance athletes, 59% (41% heat acclimation, IAAF Doha 2019 [80]) and 60% (32% heat acclimation, 8% combined HA, RWTC Muscat 2022 [33]). Heat acclimatisation was also most prevalent amongst paralympic athletes prior to the Paralympics Tokyo 2020 (51% vs. 16% acclimation [6]). Such data likely reflects a finding from Galan-Lopez et al. [33] where athletes who adopted a dedicated HA strategy were more likely to live/train in a hot climate, whereas those who live/train in cold/temperate climates have identified greater barriers to the adoption of HA compared to their counterparts from hot climates ([4, 33] specific data are provided and discussed in detail below). Greater specificity should be reported within the literature, as most studies do not report the breakdown of duration (i.e., number of days), exercise protocol (e.g., fixed vs. self-regulated work rate), or environmental characteristics (i.e., temperature, humidity) used. Only Galan-Lopez et al. [33] determined the specifics of HA protocols, with 62% of the athletes who adopted HA using self-regulated exercise intensities compared to 23% who used a fixed intensity. Ninety three percent of athletes who adopted heat acclimation used a fixed environmental temperature (mean ambient temperature: 31.5 °C) compared to an incremental temperature rise across the protocol (7% [33]). An observational study by Carr et al. [19] followed 6 Olympic racewalkers through their preparation for the Tokyo 2020 Olympic Games. These athletes completed an intermittent incremental heat acclimation protocol (1–2 treadmill sessions per week) over 3 months. This was followed by 18 days of heat acclimatisation during a team camp one month prior to the Tokyo 2020 Olympic Games [mean temperature range of training sessions: 23 °C, 71.4% relative humidity (RH) to 24.3 °C, 67.4% RH, mean maximal temperature: 27.3 °C, 89.4% RH (i.e., similar weather conditions to Tokyo), training intensity and duration varied across these sessions [19]]. Similarly, real-world HA practices in elite race-walking athletes have been described and include the use of combined outdoor and indoor HA training [97], and combined outdoor HA training and passive hot-water immersion [96]. While data of this nature are insightful, it is challenging to obtain this level of detail from elite athletes via a survey. In addition, Tc and/or other physiological data (e.g., heart rate, sweat rate) were not collected [19], and have not been collected elsewhere prior to world championship events [6, 33, 74, 80, 85] to objectively assess the physiological adaptations of the adopted HA strategies. Although, in-competition Tc/Tsk, performance and illness EHI/EHS presentation offer insight into the success of adopted self-reported HA strategies (e.g., Table 2 citations).
Current evidence of the adoption of HA mainly exists amongst elite endurance athletes prior to World Championships, Olympic and Paralympic competitions. However, these are not the only sporting events held in hot environments or the only elite athletes who benefit from adopting HA. Considerable research efforts are required to gauge the adoption of HA across the sports landscape and determine whether athletes are preparing(ed) to compete in the heat. Including and not limited to youth and master’s athletes whose thermoregulatory systems may be compromised compared to the elite adult athletes [65, 104]. International federations [e.g., World Athletics, International Olympic Committee (IOC), International Paralympic Committee (IPC)] and national governing bodies remain central advocates and educators to ensure that HA is universally adopted amongst elite athletes. Specific research into Paralympic athletes is also essential, given those with spinal cord injuries are at greater risk of EHS [34], and yet there is only one study to date investigating the adoption of heat preparation strategies prior to competition in this population [6].
Adoption of Heat Acclimation/Acclimatisation and the Impact on Performance and Medical Events
It is unlikely that an elite athlete will adopt any training method into their practice without understanding if it will improve their ability to perform in competition. At IAAF Doha 2019, athletes who had adopted HA finished better than those who did not (mean finishing position: 18th HA vs. 28th non-HA, P = 0.009) although, the relative performance in terms of percentage difference from an athlete’s own personal best (PB) time was not different (112.6% of PB time for HA vs. 113.3% non-HA [80]). Of those who undertook HA, only 19% did not finish (DNF) vs. 30% who did not HA, although this was not statistically significant [80]. In addition, the adoption of HA influenced physiological responses, with those undertaking HA having a lower race start Tc (− 0.2 °C, not statistically significant but potentially physiologically meaningful [105]) and lower in-race peak Tc (− 0.4 °C, statistically significant [80]). The potential to lower peak Tc by 0.4 °C over a race in hot conditions may mean the difference between competing for the win or experiencing EHI/EHS, especially given the regularity with which athletes (elite and recreational) reach and exceed a Tc of 40 °C, even in cool environments (see Table 4). Prior to RWTC Muscat 2022 the four surveyed athletes that achieved a medal had all adopted a dedicated HA strategy prior to the championships, and of the 15 surveyed athletes who finished within the top 10 in their race, 80% had adopted a specific HA strategy for the event [33].
Of the Australian racewalking athletes from Carr et al. [19], two improved their PB, two finished in the top 10 and the maximum performance decrement of the six athletes was 8.9% of their PB, which is within the expected range of performance decrement when performing in the heat (6%–16% or 0.3% to 0.4% for every 1 °C WBGT outside of 7.5–15 °C [22, 55]). This suggests the adopted HA strategies successfully induced physiological adaptations, although, confirmatory objective physiological (e.g., heart/sweat rate and plasma volume changes) data are not available. There are a multitude of studies that have observed a positive impact of HA on exercise performance in the laboratory (summarised in this meta-analysis [105]) and current evidence of in-competition performance, albeit limited by the small number of studies, suggests that this translates to elite level competition [19, 33, 80].
Performance is likely the key desired outcome for athletes, but for race organisers and international federations the health/safety of the athletes is of primary importance. Experiencing symptoms and clinical diagnosis of EHI is prevalent among elite athletes (outlined in Table 5 [6, 33, 74, 80, 85]) perhaps reflective, in part, of the lack of HA adoption observed. Studies have reported the number of previous incidents of EHI/EHS among their sample but have not associated this with previous adoption of HA [1.6% of surveyed athletes at Beijing 2015 [74], three cases of EHI (specifically, heat exhaustion) were recorded at UCI Qatar 2016 [85] and 21% of Paralympic athletes surveyed experienced symptoms of EHI [6]]. At IAAF Doha 2019, 32% of surveyed athletes who did not adopt HA experienced a heat related medical event compared to only 19% of those who did HA prior to the event although, not statistically significant (P ≥ 0.179 [80]). Female athletes experienced a higher prevalence of an in-race medical event compared to males (32% vs. 17%, respectively, P < 0.001) during the marathon, however, the environmental conditions during the respective marathons were considerably different (female race WBGT: 29.6 °C, male race WBGT: 23.5 °C) and likely explains this finding [80]. No differences between males and females were observed during the racewalk races (male and female races were run simultaneously, P = 0.597 [80]). Lower incidence of medical events in those that adopted HA is again indicative that the adopted HA strategies successfully induced physiological adaptations that reduced, but did not eradicate, medical events during competition in heat. It must also be noted that during real-world competition there are many factors that may have impacted the outcomes in these athletes (e.g., appropriate pacing strategy, cooling/hydration plan, non-heat related illness, etc.). More detailed data are required to determine with certainty if physiological adaptations have been induced and resulted in improved health and performance. Figure 2 provides an overview of current practice by elite athletes and the impacts on performance and medical events.
Adoption of HA in Elite Athletes: An overview of the literature that has assessed the adoption of HA in elite athletes, what influences the adoption of HA and the barriers to adopting HA that athletes experience. The content within this figure is derived from data within the following publications: Périard et al. [74], Racinais et al. [85], Racinais et al. [80], Galan-Lopez et al. [33], Alkemade et al. [6]. HA heat acclimation/acclimatisation, DNF did not finish, Tc core temperature
Effect of Climate and Biological Sex-Based Differences on the Adoption of Heat Acclimation/Acclimatisation
The climate an athlete lives and trains in may impact the adoption of HA to prepare for hot competitions however, data are scarce. Studies have assessed home continent and HA adoption; however, this is not indicative of any specific climate/conditions an athlete trained in [6, 74]. Alkemade et al. [6] observed that Paralympic athletes from Oceania were more likely to have adopted HA at prior events, but no differences were observed prior to the Paralympics Tokyo 2020. However, Galan-Lopez et al. [33] observed that, paradoxically, only 44% of athletes from a cold/temperate environment (self-reported) adopted an intentional HA strategy, compared to 82% from a hot climate. Importantly, this finding is linked to the barriers to HA identified by athletes and practitioners. The most common barrier to HA adoption among those residing in cold/temperate climates is accessibility of hot environments (52% vs. 37% from a hot climate [4] and 49% vs. 27% from hot [33] of surveyed athletes) and cost of implementing HA (up to 45% vs. 35% from hot [4, 33]). It should be noted that specific costs of implementing HA have not been identified, so it is not fully clear whether these high costs are real or perceived. These findings suggest that those residing in cold/temperate climates need greater support in adopting HA strategies. Where funding is not available, education is essential to increasing the adoption of HA (i.e., awareness of low cost and effective alternative HA strategies [22, 37, 54, 60, 94]).
The impact of biological sex differences on the adoption of HA has received more attention than climate within this context. Females [20%, males: 11.6% (P = 0.045)] were more likely to have trained in the heat at IAAF Beijing 2015 [74], and at UCI Qatar 2016 [85], there was a significant effect of biological sex on the adoption of HA. Specifically, more males (30%) than females (8%) did not implement any form of heat training [P < 0.05, UCI Qatar 2016 [85]]. In contrast, HA adoption was higher among males (63%, female: 46%) at RWTC Muscat 2022, although not statistically significant [33]. Alkemade et al. [6] observed that male Paralympic athletes were more likely to have adopted a HA strategy prior to past events but prior to the Paralympics Tokyo 2020 no differences between sexes were identified. Adoption of HA was not significantly different between sexes [56% and 68% (male vs. female not specified)] at IAAF Doha 2019 [80].
Findings are somewhat inconclusive in determining a specific impact of biological sex on the self-selected adoption of HA prior to major championships, due to limited available data/sample size. Significantly more research is required to determine any impact of sex on the adoption of HA prior to competition. Additionally, debate exists surrounding the timescale of male vs. female adaptation to the heat [47, 110]. Some evidence suggests that short (i.e., 5 day) HA protocols are likely insufficient for females to obtain physiological adaptations that are beneficial for health/performance [39, 50, 62, 109, 116] however, the limited data in females make specific conclusions difficult [47]. Thus, the continued comparison of elite male and female athlete real-world heat-based practices are warranted. Similarly, more data are required across the sport landscape to determine with greater certainty if and/or how living/training in a cold/temperate environment impacts an athlete’s ability to adopt HA. From the current data, international federations and governing bodies should make a concerted effort to support those from a cold/temperate environment to be able to adopt HA into their practice, whether this is through education or funding.
Knowledge of Heat Related Best Practice
Knowledge of athletes and practitioners can be assessed in multiple ways. Including but not limited to self-reported survey questions and/or interviews that directly evaluate knowledge, and observe current practice (i.e., training/competition preparation) to determine whether evidence-based guidelines are followed. For example, to achieve full HA adaptations ≥14 consecutive days of heat exposure for at least 60 min where Tc ≥ 38.5 °C, combined with high skin temperature and profuse sweating, are required [35, 73, 78]. Shorter HA protocols (minimum 5 days of heat exposure) can elicit some physiological adaptations and performance benefits [35, 44, 112]. Athletes that implement a dedicated HA strategy for ≥5 days are indicative of some/appropriate knowledge of HA best practice (and of course have the time, environment and/or facilities to do this).
Currently, there is limited comparability between research studies given the surveys that have been implemented to assess athlete knowledge lack standardisation, thus, the key findings are conveyed descriptively here. Alabdulwahed et al. [4] determined elite athletes and practitioners’ knowledge and use of heat adaptation practices via an online self-reported survey. Athletes had less heat related best practice knowledge than practitioners, and although both populations exhibited greater knowledge of appropriate nutritional strategies for training/competing in the heat, greater education is still required [4]. Perceived performance decrement in hot conditions was ~30% (median) among both athletes and practitioners, considerably higher than the reported 6% to 16% and 0.3% to 0.4% per degree of WBGT from the optimal 7.5 °C to 15 °C in the literature [22, 55]; with a range of ~ 5% to 50% in perceived performance decrement highlighting a highly varied level of knowledge. The median number of days athletes/practitioners believed were needed to achieve full HA was ~ 15 days, which suggests appropriate knowledge of HA adaptations; however, the large range of responses (from 3 to 30 days) does not support this [4, 33]. When rating the effectiveness of HA to offset heat induced performance decrements, athletes most commonly (38%) selected that HA was ‘moderately effective’ compared to 49% of practitioners who perceived it as ‘extremely/most effective’ [4]. Interestingly, both athletes and practitioners perceived cooling strategies, pre (58% and 60%, respectively) and mid-cooling (66% and 74%, respectively), to have good efficacy in reducing heat induced performance decrements. This is reflected in current practice where 50%–80% of athletes have pre-planned cooling strategies across competitions (discussed in depth below [74, 83, 85]). Athletes and practitioners had limited knowledge of safe Tc during exercise with biologically implausible Tc’s (range of 25 °C to 45 °C) being reported as a ‘safe’ Tc to attain during exercise [4]. Measuring Tc during training/competition was considered to be important (53% to 74% of surveyed athletes reported it as important) yet, 75% to 91% of those surveyed reported not having measured Tc previously [4], similarly 77% of those at the RWTC Muscat 2022 had never measured Tc [33]. These data highlight that knowledge of evidence-based practice does not always translate to the adoption of best practice [4]. Finally, only 35% of athletes at RWTC Muscat 2022 were aware of what WBGT is [33], suggesting athletes may be unaware of the magnitude by which ambient conditions may impact their health and performance.
Not all research assessing elite athlete preparation for competition in heat has directly assessed athlete or practitioner knowledge. However, the low adoption of HA in these studies may infer that a significant proportion of athletes may not be aware of the importance/benefits of adopting HA and/or how to induce beneficial HA adaptations prior to competition in the heat, or face significant barriers that prevent its adoption [6, 33, 74, 80, 85]. Given the events studied are World Championship and Paralympic events and are generally considered the pinnacle of an athlete’s career, it would be expected that athletes would prioritise preparation for these events to achieve the highest place finish possible. Furthermore, national federations likely provide greater financial support to athletes competing at these events and it can be assumed that these competitions represent maximal adoption of HA in comparison to events of lesser standing. Those who did adopt a dedicated HA strategy prior to events did so for between 5 and 30 days, indicative of athletes implementing short to long-term HA [6, 33, 74, 80, 85]. At RWTC Muscat 2022, 57% undertook self-reported HA for > 10 days, suggesting an attempt to elicit fuller HA adaptations [33]; however, this is speculative.
Effect of Climate and Biological Sex-Based Differences on Knowledge of Heat Related Best Practice
The climate that an athlete lives/trains in has limited impact on knowledge of heat related practice. Alabdulwahed et al. [4] observed minimal differences in knowledge between athletes residing in hot compared with cold/temperate climates. Seventy eight percent of surveyed athletes/practitioners from a cold/temperate climate (hot: 57%) identified pre-cooling as the most effective strategy for reducing performance decrements induced by hot conditions, suggesting limited knowledge among athletes/practitioners from both climates. Biological sex differences in knowledge were not assessed within this study [4]. Galan-Lopez et al. [33] saw no impact of climate on knowledge but there were differences between sexes. A comparison between men and women showed that 83% of females vs. 55% of males did not know what WBGT was, 42% of females vs. 14% of males were more likely to report not knowing the maximum environmental conditions expected at the RWTC Muscat 2022, and only 8% females vs. 31% males reported having measured Tc in training/competition previously.
Based on current evidence, knowledge of heat related practice appears to be limited among elite athletes. International federations and national governing bodies must remain central advocates for the implementation of concerted efforts to improve knowledge among their athletes, practitioners and stakeholders. More informed/educated athletes are likely to adopt evidence-based practice that will benefit themselves (i.e., improved performance in the heat) and race organisers (i.e., fewer medical events). It is unclear whether the educational material provided by the IAAF prior to IAAF Doha 2019 drove the increase in the adoption of HA (amid substantial media and scientific attention given to the conditions); however, regular release of such material with updated recommendations (and in multiple languages) should be encouraged. In the short-term, based on the limited available data, female athletes may require increased educational focus given they have exhibited less knowledge in this area than male athletes.
Adoption of Hydration and Cooling Strategies
Hydration [5, 32, 72] and cooling strategies alone [14, 16] are effective in alleviating heat strain and improving athletic performance in hot conditions, but evidence suggests they should be complementary to the adoption of HA [100]. Hydration investigations during competition have focused on pre-planned fluid intake (namely water) and supplementation with carbohydrates and electrolytes. The prevalence of a pre-planned fluid intake strategy is generally high among elite athletes (≥80%), as is electrolyte and carbohydrate supplementation [74, 83, 85]. Adoption of a pre-planned fluid intake is considerably higher than that of HA and likely a reflection of athlete and practitioner knowledge, and reduced barriers to adoption of short-term heat mitigation strategies compared with HA. Alabdulwahed et al. [4] found that athletes and practitioners had superior knowledge of nutrition and hydration strategies compared to HA, and their self-reported practice was aligned with consensus recommendations for training and competing in the heat [78]. The use of a pre-planned fluid intake strategy and the volume of fluid varies depending on the event, due to a combination of competition rules (i.e., fluids not permitted), event duration, event temperatures, and ease of fluid intake during events (i.e., pace/speed of athlete during a race and frequency of aid stations [59]). Up to ~38% of track athletes (13.6% sprints, 37.8 middle distance, 23.4% long distance runners and 0% decathlon/heptathlon) at IAAF Beijing 2015 did not plan to consume any fluids during their competition [inclusive of warm-up/cool down [74]]. Time trialists (~45 min event) during UCI Qatar 2016 (65%–70%) planned to drink less than 0.5 L compared to the road race [~3 (female) to 6 (male) hour race) athletes who planned to drink over 2 L [90% [85]]. The event an athlete competed in impacted planned fluid composition with up to 54% of time trialists and ~70% of road race athletes at UCI Qatar 2016 planning to supplement their fluid with carbohydrates or electrolytes [85]. The attention given to heat prior to IAAF Doha 2019 and release of ‘beat the heat’ educational material likely reflects the high prevalence (93%) of athletes having a pre-planned hydration strategy with high use of electrolyte (83%) and carbohydrate (81%) supplementation [83]. Competition event (likely due to duration and race day weather conditions) still impacted fluid consumption, 82% of 50 km racewalk athletes reported planned consumption of over 2 L compared to 41% of 20 km racewalkers and marathon runners [83]. Only 30% of Paralympic athletes planned to consume fluids with electrolytes and 16% with carbohydrates. The rate of electrolyte/carbohydrate supplementation is likely due to the sample covering all Paralympic athletes and not only endurance-based events [6]. Hypohydration (reduced body water), equivalent to a body mass loss of 2%–3%, decreases plasma volume and increases cardiovascular strain when exercising in the heat, which may be detrimental to performance [45, 66]. Elite athletes have been observed to experience severe hypohydration in competition and can still produce world class performances [10]. While this apparent tolerance is not well understood, it does seem that some ‘habituation’ to hypohydration may be possible [30] and elite athletes (due to their high absolute work rates and prolonged training) would likely regularly experience hypohydration in training and competition. Nonetheless, hypohydration is reported to exacerbate heat [89] and cardiovascular [1] strain and impair performance, even when athletes are blinded to their hydration status [32]. Fluid ingestion is also an effective measure to attenuate Tc rise during endurance performance [5]. The adoption of pre-planned hydration strategies and generally appropriate consumption levels by elite athletes suggests that they implement evidence-based guidelines when competing in the heat.
Cooling strategies have been widely adopted by elite athletes with an increase being observed in more recent competitions. From 52% of surveyed athletes at IAAF Beijing 2015 [74] to as much as 96% of time trialists at UCI Qatar 2016 (road race athletes: 74% [85], 80% IAAF Doha 2019 [83], 77% Paralympics Tokyo 2020 [6]). Cooling methods have varied greatly across studies with a high prevalence of ice vest use [83]. Mid-cooling (i.e., cooling during an event) has not been widely investigated, only at IAAF Doha 2019 and the Paralympics Tokyo 2020. Ninety-three percent (IAAF Doha 2019) and 88% (Paralympics Tokyo 2020) of surveyed athletes intended to implement a mid-cooling strategy [6, 83]. Ninety-nine percent of those who had a planned pre-cooling strategy at IAAF Doha 2019 also had a planned mid-cooling strategy, and the predominant strategies were cold water dousing (65%) and cold water ingestion (52% [83]). This increased use of cooling strategies is representative of athletes perceived effectiveness of the strategy, having most commonly ranked pre- and mid-cooling as the most effective strategies to reduce the detrimental impact of heat stress on performance [4]. The prevalence of pre-planned cooling strategies among elite athletes is representative of the ease with which they can be applied in practice and suggests knowledge of evidence-based guidelines.
Hydration and cooling strategies are highly prevalent in elite athletes competing in the heat and there has been an increased prevalence since IAAF Beijing 2015 (see Fig. 3 for what is currently implemented by athletes in practice). The level with which hydration and cooling strategies have been adopted by athletes is significantly higher than HA, likely due to superior knowledge of, and logistical ease of employing these strategies compared to implementing and undertaking a HA regimen across several days/weeks. It would be of interest to determine the specifics of cooling strategies adopted by athletes, to date, only details of whether a cooling strategy will be used and which strategy (e.g., ice-vest, cold water ingestion) an athlete might adopt have been evaluated. Understanding differences in sport specific use of cooling strategies [2] and the duration, timing and aggressiveness of cooling interventions would help to determine whether evidence-based recommendations are being adopted [e.g., not inducing shivering, cool Tc and warm periphery (muscle temperature) as outlined by Taylor et al. [100]].
Nutrition, Hydration, and Cooling: An overview of the acute race day strategies implemented by elite athletes, what influences the strategy used and recommendations for athletes and practitioners. The content within this figure is derived from data within the following publications: Périard et al. [74], Racinais et al. [85], Racinais et al. [80], Galan-Lopez et al. [33], Alkemade et al. [6]
Effect of Climate and Biological Sex-Based Differences on Hydration and Cooling Strategy Adoption
The impact of the climate an athlete lives/trains has not been investigated for hydration and cooling strategies to date. However, Racinais et al. [83] noted that of the eight African based runners who completed their questionnaire two declared they planned no fluid intake [also observed in African runners previously [10]) and, perhaps consequently, these two athletes finished in the bottom 50% of finishers. African runners also had significantly higher body mass losses (− 3.9% vs. − 2.0%) compared to other athletes (P = 0.001 [83]). Sex-based differences have been observed within the hydration and cooling data [74, 83]. Females were less likely to supplement their fluid consumption with electrolyte or carbohydrates at IAAF Beijing 2015 [74]. Females’ planned use of electrolytes (72%; men: 91%; P = 0.029) and carbohydrate (67%; men: 93%; P = 0.003) was significantly lower than their male counterparts at IAAF Doha 2019 [83]. Forty two percent (females) and 52% (males) planned a pre-cooling strategy at IAAF Beijing 2015 [74] however, at UCI Qatar 2016 96% of females planned to adopt a pre-cooling strategy prior to the road race compared to 57% of males (use among team/individual time trialists was not different between sexes [85]). The use of a pre- or mid-cooling strategy at IAAF Doha 2019 was not different between sexes other than higher (31%) adoption of pre-cooling via ice-slurry in females (males: 13% [83]). The sample of data in this space are limited, and further investigation is warranted to provide a greater understanding of hydration strategies between sexes.
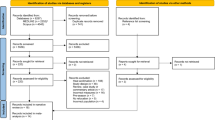
Recommendations for Best Practice, Future Research and the Translation of Research into Practice
The recommendations were initially outlined by authors CE and LT and whenever possible align with existing consensus, meta-analysis, reviews and best-practices (as extensively cited above). Refinement and consensus between authors was reached via three rounds of author revisions (all authors). Further in-depth validation was sought from authors SR and TS. These recommendations are realised through a combination of best practice guidelines and author experience (including but not limited to: elite sport practitioners, elite sport researchers/scientists, elite sport clinicians and medical doctors, and members of international federations/governing bodies) within elite sport. Figure 4 provides an overview of these recommendations.
Recommendations: An overview of best practice recommendations, what research should focus on in the future and how to improve the adoption of these recommendations. These recommendations are realised through a combination of best practice guidelines and author experience within elite sport. Tc core temperature, Tsk skin temperature, HA heat acclimation/acclimatisation, IF international federation, NGB national governing body
Best Practice
-
1.
HA is optimal to improve performance and protect health when competing in the heat. To achieve HA at least 10–14 consecutive days of active heat exposure (using a natural or artificial environment), where Tc is ≥38.5 °C, Tsk is ~35 °C with an increase in skin blood flow and profuse sweating is induced for at least 60 min, should be adopted in environmental conditions that are similar to or exceed the expected conditions (i.e., historical peak temperature/humidity) of the competition location [3, 35, 72, 76, 78, 81, 100, 103]. Elite athlete training schedules may not allow for this type of regimen thus, they should look to complement specific HA training with the following two recommendations.
-
2.
Where exercise in a hot environment is not achievable, post-exercise sauna (≥ 80 °C) or hot water immersion (≥40 °C) for 20–40 min [22, 37, 60] or wearing additional clothing during training [54, 94] should be adopted to induce HA adaptations (NB: tolerance to these HA strategies should be built up gradually over time ideally, supervised by qualified personnel and monitored using body temperature measurement tools to avoid adverse health outcomes). An additional benefit of this approach is ‘quality’ preservation of the ‘active’ sport-specific part of the training session.
-
3.
Pre-cooling strategies should be complementary to HA (but not replace) and focus on the physical and perceptual reduction of Tc and deep body tissue temperatures while maintaining a warm activated periphery (i.e., muscle temperature) to facilitate initial competition performance capacity [100]. If the periphery is cooled too much pre-competition (i.e., to the point of shivering), a disruption in peripheral to central feedback processes can occur at race onset which, until a relative equilibrium is reached, compromises pacing (athletes and coaches should plan for this within their adopted pacing strategies). CWI for 10–15 min at 10–15 °C is the most efficacious pre-cooling strategy to reduce body tissue temperature yet is often incompatible with practice [100]. Alternative albeit less effective (in terms of body tissue temperature reduction) methods include ice-vests/towels and ice slurry/cold water ingestion which have good practice-compatibility [14, 16]. Mid-competition cooling, ideally adopted in a complimentary manner to both HA and pre-cooling, should focus on reducing the rate of rise in Tc and favourably altering body tissue and Tsk perceptions [100]. Ice cold water ingestion at regular intervals during competition, ice hats/towels and menthol spray are mid-competition cooling strategies observed to provide an ergogenic effect [14, 16, 95]. Importantly, an individualised approach to cooling should be adopted and thoroughly practised in training to ensure tolerance, avoid negative consequences (e.g., gastrointestinal issues, altered pacing, shivering) and ensure optimal implementation prior to and during competition [100].
-
4.
Hydration strategies should be complementary to HA and pre-/mid-cooling approaches. Athletes should be euhydrated prior to competition and hydration strategies should begin in the days leading up to competition [45]. Competition day strategies should begin several hours before the start of competition to allow for fluid absorption and urination to return to normal. In-competition strategies should plan for fluid intake to, if possible, avoid significant dehydration (body mass losses of >2%) accruing during competition, but it must be acknowledged that in some settings this may not be possible [45, 66]. Fluids may consist of electrolyte and/or carbohydrate solutions, although carbohydrate intake in particular, needs to be well planned to ensure carbohydrate intake is appropriate (i.e., not too little or too much). All strategies should be individualised and specific to the competition with thorough planning and repeated practise during training to avoid negative performance effects (e.g., gastrointestinal disturbances, hyponatraemia) during competition [45].
Research
-
1.
Take a holistic approach to assessing heat-based best practice within elite athletes linking the levels of adoption of HA, use of cooling and hydration strategies to self-reported knowledge and their execution to objectively measurable outcomes (e.g., the impact on performance and medical events). Investigation with large samples of competition fields is imperative (i.e., only 6% of athletes competing at the competitions in this review were surveyed, Table 1) and the research must be expanded from the current endurance athletes across other types of sports, sport modes and athletes’ performance levels.
-
2.
Research should focus on capturing the athlete voice and identifying: (1) those unable to undertake HA and determine the barriers faced in adopting HA and how these can be overcome; (2) where athletes obtain their knowledge (e.g., practitioners, medical teams) of heat-based practice; and (3) individual differences and perceptions of the necessity for adopting dedicated HA training (e.g., individuals from a hot climate may perceive they are already/always HA and do not need to adopt HA).
-
3.
Practitioners (e.g., medical team, coaches) have an instrumental role in knowledge translation and adoption of heat mitigation strategies thus, assessing their knowledge and where they obtain their knowledge provide insight to the results seen in athletes.
Translation of Research into Practice
-
1.
International federations and national governing bodies must remain central advocates and educators of evidence-based practice with regular (not only prior to major championships) dissemination of updated and evidence-based educational materials, to all stakeholders including the athletes. Efforts should be made to deliver content in multiple languages and be accessible for athletes who may be visually impaired or have intellectual disabilities. Deploying strategies for active education (i.e., more than simply disseminating material) of evidence-based practice is likely required to observe an increase in the adoption of evidence-based practice among athletes [31, 90].
-
2.
Specific focus should be given to athletes from cold/temperate climates with innovative strategies to HA, given that these athletes are seen to be considerably less likely to adopt HA due to actual and/or perceived barriers faced accessing facilities and hot environments to live/train [4, 33].
-
3.
Education surrounding evidence-based hydration and cooling guidelines should be implemented to ensure athletes implement best practice and are ideally prepared for their event. Particularly for female athlete populations who have demonstrated sub-optimal practices compared to males which may be, in part, due to a lack of knowledge [33, 83].
Conclusions
Long term HA (i.e., ≥10 days) is by far the most health protective and performance enhancing strategy to mitigate the impacts of heat compared to short/medium term HA. Cooling and hydration strategies should complement and not be used instead of HA and strategies should be individualised and well-practised. The adoption of HA among elite athletes prior to competition in the heat appears to be increasing, however, is not universal. Provision of easily digestible educational materials with alternative low cost, innovative and implementable HA strategies appear to be paramount to increasing the adoption of HA. Materials of this nature are needed most by those from cold/temperate climates who have been shown to be the least likely to adopt a HA strategy and face the most significant barriers to its implementation. There is wide use of cooling and hydration strategies by elite athletes competing in heat, likely due to the ease of implementation compared to HA. Educational materials should also include evidence-based guidelines that ensure athletes are optimally prepared for competition. Importantly, a one size fits all approach should be avoided. Materials must cater for sport and sex specific differences ensuring Paralympic athlete specific challenges (i.e., altered thermoregulation) are accounted for. Finally, research is required on large competition samples across the sporting landscape to determine how elite athletes outside of World Championship/Olympic/Paralympic endurance events prepare to compete in the heat.
Data Availability
N/A.
References
Adams WM, Ferraro EM, Huggins RA, Casa DJ. Influence of body mass loss on changes in heart rate during exercise in the heat: a systematic review. J Strength Cond Res. 2014;28(8):2380–9.
Adams WM, Hosokawa Y, Casa DJ. Body-cooling paradigm in sport: maximizing safety and performance during competition. J Sport Rehabil. 2016;25(4):382–94.
Adams WM, Hosokawa Y, Casa DJ, Périard JD, Racinais S, Wingo JE, Yeargin SW, Scarneo-Miller SE, Kerr ZY, Belval LN, Alosa D, Csillan D, Labella C, Walker L. Roundtable on preseason heat safety in secondary school athletics: heat acclimatization. J Athl Train. 2021;56(4):352–61.
Alabdulwahed S, Galan-Lopez N, Hill T, James LJ, Chrismas BCR, Racinais S, Stellingwerff T, Leal DV, Hausen M, Chamari K, Fullagar HHK, Esh C, Taylor L. Heat adaptation and nutrition practices: athlete and practitioner knowledge and use. Int J Sports Physiol Perform. 2022;17(7):1011–24.
Alhadad SB, Tan PMS, Lee JKW. Efficacy of heat mitigation strategies on core temperature and endurance exercise: a meta-analysis. Front Physiol. 2019;10:71.
Alkemade P, Daanen HAM, Janssen TWJ, Broad E, Goosey-Tolfrey VL, Ibusuki T, Kneepkens H, Périard JD, Eijsvogels TMH. Heat preparedness and exertional heat illness in Paralympic athletes: a Tokyo 2020 survey. Temperature (Austin). 2023;10(2):264–75.
Armstrong LE, Maresh CM. The induction and decay of heat acclimatisation in trained athletes. Sports Med. 1991;12(5):302–12.
Aughey RJ, Goodman CA, Mckenna MJ. Greater chance of high core temperatures with modified pacing strategy during team sport in the heat. J Sci Med Sport. 2014;17:113–8.
Ballester J, Quijal-Zamorano M, Mendez Turrubiates RF, Pegenaute F, Herrmann FR, Robine JM, Basagana X, Tonne C, Anto JM, Achebak H. Heat-related mortality in Europe during the summer of 2022. Nat Med. 2023;29(7):1857–66.
Beis LY, Wright-Whyte M, Fudge B, Noakes T, Pitsiladis YP. Drinking behaviors of elite male runners during marathon competition. Clin J Sport Med. 2012;22(3):254–61.
Belval LN, Casa DJ, Adams WM, Chiampas GT, Holschen JC, Hosokawa Y, Jardine J, Kane SF, Labotz M, Lemieux RS. Consensus statement-prehospital care of exertional heat stroke. Prehosp Emerg. 2018;22(3):392–7.
Belval LN, Hosokawa Y, Casa DJ, Adams WM, Armstrong LE, Baker LB, Burke L, Cheuvront S, Chiampas G, Gonzalez-Alonso J, Huggins RA, Kavouras SA, Lee EC, Mcdermott BP, Miller K, Schlader Z, Sims S, Stearns RL, Troyanos C, Wingo J. Practical hydration solutions for sports. Nutrients. 2019;11(7):1550.
Bermon S, Adami PE. Meteorological risks in Doha 2019 Athletics World Championships: health considerations from organizers. Front Sports Act Living. 2019;1:58.
Bongers CC, Hopman MT, Eijsvogels TM. Cooling interventions for athletes: an overview of effectiveness, physiological mechanisms, and practical considerations. Temperature (Austin). 2017;4(1):60–78.
Bongers CC, Thijssen DH, Veltmeijer MT, Hopman MT, Eijsvogels TM. Precooling and percooling (cooling during exercise) both improve performance in the heat: a meta-analytical review. Br J Sports Med. 2015;49(6):377–84.
Bongers C, Ten Haaf DSM, Ravanelli N, Eijsvogels TMH, Hopman MTE. Core temperature and sweating in men and women during a 15-km race in cool conditions. Int J Sports Physiol Perform. 2020;15:1–6.
Byrne C, Lee JK, Chew SA, Lim CL, Tan EY. Continuous thermoregulatory responses to mass-participation distance running in heat. Med Sci Sports Exerc. 2006;38:803–10.
Capon A, Jay O, Ebi K, Lo S. Heat and health: a forthcoming Lancet Series. Lancet. 2019;394(1098):551–2.
Carr AJ, Vallance BS, Rothwell J, Rea AE, Burke LM, Guy JH. Competing in hot conditions at the Tokyo Olympic Games: preparation strategies used by Australian Race Walkers. Front Physiol. 2022;13:836858.
Casa DJ, Demartini JK, Bergeron MF, Csillan D, Eichner ER, Lopez RM, Ferrara MS, Miller KC, O’connor F, Sawka MN. National Athletic Trainers’ Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000.
Casa DJ, Hosokawa Y, Belval LN, Adams WM, Stearns RL. Preventing death from exertional heat stroke—the long road from evidence to policy. Kinesiol Rev. 2017;6(1):99–109.
Casadio JR, Kilding AE, Cotter JD, Laursen PB. From lab to real world: heat acclimation considerations for elite athletes. Sports Med. 2017;47(8):1467–76.
Chen S, Komatsu S. Plant proteomic research 4.0: frontiers in stress resilience. Int J Mol Sci. 2021;22(24):13362.
Cheng L, Abraham J, Trenberth KE, Fasullo J, Boyer T, Locarnini R, Zhang B, Yu F, Wan L, Chen X, Song X, Liu Y, Mann ME, Reseghetti F, Simoncelli S, Gouretski V, Chen G, Mishonov A, Reagan J, Zhu J. Upper ocean temperatures hit record high in 2020. Adv Atmos Sci. 2021;38:523–30.
Cheuvront SN, Kenefick RW, Montain SJ, Sawka MN. Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol. 2010;1985(109):1989–95.
Christensen CL, Ruhling RO. Thermoregulatory responses during a marathon. A case study of a woman runner. Br J Sports Med. 1980;14:131–2.
Cooper ER, Grundstein AJ, Miles JD, Ferrara MS, Curry P, Casa DJ, Hosokawa Y. Heat policy revision for Georgia high school football practices based on data-driven research. J Athl Train. 2020;55(7):673–81.
Daanen HAM, Racinais S, Périard JD. Heat acclimation decay and re-induction: a systematic review and meta-analysis. Sports Med. 2018;48(2):409–30.
Duffield R, Coutts AJ, Quinn J. Core temperature responses and match running performance during intermittent-sprint exercise competition in warm conditions. J Strength Cond Res. 2009;23:1238–44.
Fleming J, James LJ. Repeated familiarisation with hypohydration attenuates the performance decrement caused by hypohydration during treadmill running. Appl Physiol Nutr Metab. 2014;39(2):124–9.
Fullagar HHK, Mccall A, Impellizzeri FM, Favero T, Coutts AJ. The translation of sport science research to the field: a current opinion and overview on the perceptions of practitioners, researchers and coaches. Sports Med. 2019;49(12):1817–24.
Funnell MP, Mears SA, Bergin-Taylor K, James LJ. Blinded and unblinded hypohydration similarly impair cycling time trial performance in the heat in trained cyclists. J Appl Physiol. 2019;1985(126):870–9.
Galan-Lopez N, Esh C, Vaz Leal D, Gandini S, Lucas R, Garrandes F, Bermon S, Adami P, Kajeniene A, Hosokawa Y, Chrismas B, Stevens C, Taylor L. Heat preparation and knowledge at the world athletics race walking team Championships Muscat 2022. Int J Sports Physiol Perform. 2023;18(8):813–24.
Gee CM, Lacroix MA, Stellingwerff T, Gavel EH, Logan-Sprenger HM, West CR. Physiological considerations to support podium performance in para-athletes. Front Rehabil Sci. 2021;2:732342.
Gibson OR, James CA, Mee JA, Willmott AGB, Turner G, Hayes M, Maxwell NS. Heat alleviation strategies for athletic performance: a review and practitioner guidelines. Temperature (Austin). 2020;7:3–36.
Girard O, Brocherie F, Bishop DJ. Sprint performance under heat stress: a review. Scand J Med Sci Sports. 2015;25(Suppl 1):79–89.
Heathcote SL, Hassmen P, Zhou S, Stevens CJ. Passive heating: reviewing practical heat acclimation strategies for endurance athletes. Front Physiol. 2018;9:1851.
Henderson MJ, Grandou C, Chrismas BCR, Coutts AJ, Impellizzeri FM, Taylor L. Core body temperatures in intermittent sports: a systematic review. Sports Med. 2023;53(11):2147–70.
Hertig BA, Belding HS, Kraning KK, Batterton DL, Smith CR, Sargent F 2nd. Artificial acclimatization of women to heat. J Appl Physiol. 1963;18(2):383–6.
Hosokawa Y, Casa DJ, Racinais S. Translating evidence-based practice to clinical practice in Tokyo 2020: how to diagnose and manage exertional heat stroke. Br J Sports Med. 2020;54(15):883–4.
Hosokawa Y, Racinais S, Akama T, Zideman D, Budgett R, Casa DJ, Bermon S, Grundstein AJ, Pitsiladis YP, Schobersberger W. Prehospital management of exertional heat stroke at sports competitions: international Olympic Committee adverse weather impact expert working group for the Olympic Games Tokyo 2020. Br J Sports Med. 2021;55(24):1405–10.
Ibebuchi CC, Abu I-O. Characterization of temperature regimes in Western Europe, as regards the summer 2022 Western European heat wave. Clim Dyn. 2023;61:3707–20.
Ihsan M, Périard JD, Racinais S. How to integrate recovery during heat acclimation. 2021;55:185–6.
James CA, Richardson AJ, Watt PW, Willmott AG, Gibson OR, Maxwell NS. Short-term heat acclimation improves the determinants of endurance performance and 5-km running performance in the heat. Appl Physiol Nutr Metab. 2017;42(3):285–94.
James LJ, Funnell MP, James RM, Mears SA. Does hypohydration really impair endurance performance? Methodological considerations for interpreting hydration research. Sports Med. 2019;49(Suppl 2):103–14.
Kakamu T, Wada K, Smith DR, Endo S, Fukushima T. Preventing heat illness in the anticipated hot climate of the Tokyo 2020 Summer Olympic Games. Environ Health Prev Med. 2017;22(1):68.
Kelly MK, Bowe SJ, Jardine WT, Condo D, Guy JH, Snow RJ, Carr AJ. Heat adaptation for females: a systematic review and meta-analysis of physiological adaptations and exercise performance in the heat. Sports Med. 2023;53(7):1395–421.
Kerr Z, Register-Mihalik J, Pryor R. The effect of the National Athletic Trainers’ Association Inter-Association Task Force (NATA-IATF) preseason heat acclimatization guidelines on high school football preseason exertional heat illness rates. J Athl Train. 2018;53:S72.
Kerr ZY, Register-Mihalik JK, Pryor RR, Pierpoint LA, Scarneo SE, Adams WM, Kucera KL, Casa DJ, Marshall SW. The association between mandated preseason heat acclimatization guidelines and exertional heat illness during preseason high school American football practices. Environ Health Perspect. 2019;127(4):47003.
Kirby NV, Lucas SJE, Lucas RAI. Nine-, but not four-days heat acclimation improves self-paced endurance performance in females. Front Physiol. 2019;10:539.
Laitano O, Leon LR, Roberts WO, Sawka MN. Controversies in exertional heat stroke diagnosis, prevention, and treatment. J Appl Physiol. 2019;1985(127):1338–48.
Laursen PB, Suriano R, Quod MJ, Lee H, Abbiss CR, Nosaka K, Martin DT, Bishop D. Core temperature and hydration status during an Ironman triathlon. Br J Sports Med. 2006;40:320–5.
Lee JK, Nio AQ, Lim CL, Teo EY, Byrne C. Thermoregulation, pacing and fluid balance during mass participation distance running in a warm and humid environment. Eur J Appl Physiol. 2010;109:887–98.
Lundby C, Svendsen IS, Urianstad T, Hansen J, Ronnestad BR. Training wearing thermal clothing and training in hot ambient conditions are equally effective methods of heat acclimation. J Sci Med Sport. 2021;24(8):763–7.
Mantzios K, Ioannou LG, Panagiotaki Z, Ziaka S, Périard JD, Racinais S, Nybo L, Flouris AD. Effects of weather parameters on endurance running performance: discipline-specific analysis of 1258 races. Med Sci Sports Exerc. 2022;54(1):153–61.
Maron MB, Wagner JA, Horvath SM. Thermoregulatory responses during competitive marathon running. J Appl Physiol Respir Environ Exerc Physiol. 1977;42:909–14.
Martin K, Mcleod E, Périard J, Rattray B, Keegan R, Pyne DB. The impact of environmental stress on cognitive performance: a systematic review. Hum Factors. 2019;61(8):1205–46.
Mason H, King CJ, Peden EA, Franklin CR. Systematic review of the impact of heatwaves on health service demand in Australia. BMC Health Serv Res. 2022;22(1):960.
Mccubbin AJ, Allanson BA, Caldwell Odgers JN, Cort MM, Costa RJS, Cox GR, Crawshay ST, Desbrow B, Freney EG, Gaskell SK, Hughes D, Irwin C, Jay O, Lalor BJ, Ross MLR, Shaw G, Périard JD, Burke LM. Sports dietitians Australia position statement: nutrition for exercise in hot environments. Int J Sport Nutr Exerc Metab. 2020;30(1):83–98.
Mcintyre RD, Zurawlew MJ, Oliver SJ, Cox AT, Mee JA, Walsh NP. A comparison of heat acclimation by post-exercise hot water immersion and exercise in the heat. J Sci Med Sport. 2021;24(8):729–34.
Mckay AKA, Stellingwerff T, Smith ES, Martin DT, Mujika I, Goosey-Tolfrey VL, Sheppard J, Burke LM. Defining training and performance caliber: a participant classification framework. Int J Sports Physiol Perform. 2022;17(2):317–31.
Mee JA, Gibson OR, Doust J, Maxwell NS. A comparison of males and females’ temporal patterning to short- and long-term heat acclimation. Scand J Med Sci Sports. 2015;25(Suppl 1):250–8.
Miller KC, Casa DJ, Adams WM, Hosokawa Y, Cates J, Emrich C, Fitzpatrick T, Hopper M, Jardine JF, Labotz M, Lopez RM, O’connor F, Smith MS. Roundtable on preseason heat safety in secondary school athletics: prehospital care of patients with exertional heat stroke. J Athl Train. 2021;56(4):372–82.
Millet GP, Hosokawa Y, Sandbakk O, Girard O. Editorial: Tokyo 2020 Olympic and paralympic games: specificities, novelties and lessons learned. Front Sports Act Living. 2022;4:1026769.
Millyard A, Layden JD, Pyne DB, Edwards AM, Bloxham SR. Impairments to thermoregulation in the elderly during heat exposure events. Gerontol Geriatr Med. 2020;6:2333721420932432.
Murray B. Hydration and physical performance. J Am Coll Nutr. 2007;26(Suppl 5):542S–548S.
Nakamura M, Naito T, Saito T, Takahashi A, Muraishi K, Hakamada N, Otomo M, Iizuka S, Nakamura D, Takahashi H. Case report: countermeasures against heat and coronavirus for Japanese athletes at the Tokyo 2020 olympics and paralympic games. Front Sports Act Living. 2022;4: 878022.
Notley SR, Racinais S, Kenny GP. Do sex differences in thermoregulation pose a concern for female athletes preparing for the Tokyo Olympics? Br J Sports Med. 2021;55(6):298–9.
Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol. 2014;4(2):657–89.
Ozgunen KT, Kurdak SS, Maughan RJ, Zeren C, Korkmaz S, Yazici Z, Ersoz G, Shirreffs SM, Binnet MS, Dvorak J. Effect of hot environmental conditions on physical activity patterns and temperature response of football players. Scand J Med Sci Sports. 2010;20(Suppl 3):140–7.
Périard JD, Degroot D, Jay O. Exertional heat stroke in sport and the military: epidemiology and mitigation. Exp Physiol. 2022;107(10):1111–21.
Périard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. 2021;101(4):1873–979.
Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25(Suppl 1):20–38.
Périard JD, Racinais S, Timpka T, Dahlström Ö, Spreco A, Jacobsson J, Bargoria V, Halje K, Alonso J-M. Strategies and factors associated with preparing for competing in the heat: a cohort study at the 2015 IAAF World Athletics Championships. Br J Sports Med. 2017;51:264–70.
Periard JD, Wilson MG, Tebeck ST, Gilmore JB, Stanley J, Girard O. Influence of the thermal environment on work rate and physiological strain during a UCI World tour multistage cycling race. Med Sci Sports Exerc. 2023;55:32–45.
Pryor JL, Johnson EC, Roberts WO, Pryor RR. Application of evidence-based recommendations for heat acclimation: Individual and team sport perspectives. Temperature (Austin). 2019;6(1):37–49.
Pugh LG, Corbett JL, Johnson RH. Rectal temperatures, weight losses, and sweat rates in marathon running. J Appl Physiol. 1967;23:347–52.
Racinais S, Alonso JM, Coutts AJ, Flouris AD, Girard O, Gonzalez-Alonso J, Hausswirth C, Jay O, Lee JK, Mitchell N, Nassis GP, Nybo L, Pluim BM, Roelands B, Sawka MN, Wingo J, Périard JD. Consensus recommendations on training and competing in the heat. Br J Sports Med. 2015;49(18):1164–73.
Racinais S, Casa D, Brocherie F, Ihsan M. Translating science into practice: the perspective of the Doha 2019 IAAF world championships in the heat. Front Sports Act Living. 2019;1:39.
Racinais S, Havenith G, Aylwin P, Ihsan M, Taylor L, Adami PE, Adamuz MC, Alhammoud M, Alonso JM, Bouscaren N, Buitrago S, Cardinale M, Van Dyk N, Esh CJ, Gomez-Ezeiza J, Garrandes F, Holtzhausen L, Labidi M, Lange G, Lloyd A, Moussay S, Mtibaa K, Townsend N, Wilson MG, Bermon S. Association between thermal responses, medical events, performance, heat acclimation and health status in male and female elite athletes during the 2019 Doha World Athletics Championships. Br J Sports Med. 2022;56(8):439–45.
Racinais S, Hosokawa Y, Akama T, Bermon S, Bigard X, Casa DJ, Grundstein A, Jay O, Massey A, Migliorini S, Mountjoy M, Nikolic N, Pitsiladis YP, Schobersberger W, Steinacker JM, Yamasawa F, Zideman DA, Engebretsen L, Budgett R. IOC consensus statement on recommendations and regulations for sport events in the heat. Br J Sports Med. 2023;57(1):8–25.
Racinais S, Ihsan M. Why should I test my athletes in the heat several months before Tokyo 2020? Br J Sports Med. 2020;54:700–1.
Racinais S, Ihsan M, Taylor L, Cardinale M, Adami PE, Alonso JM, Bouscaren N, Buitrago S, Esh CJ, Gomez-Ezeiza J, Garrandes F, Havenith G, Labidi M, Lange G, Lloyd A, Moussay S, Mtibaa K, Townsend N, Wilson MG, Bermon S. Hydration and cooling in elite athletes: relationship with performance, body mass loss and body temperatures during the Doha 2019 IAAF World Athletics Championships. Br J Sports Med. 2021;55(23):1335–41.
Racinais S, Moussay S, Nichols D, Travers G, Belfekih T, Schumacher YO, Périard JD. Core temperature up to 41.5 °C during the UCI road cycling World Championships in the heat. Br J Sports Med. 2019;53(7):426–9.
Racinais S, Nichols D, Travers G, Moussay S, Belfekih T, Farooq A, Schumacher YO, Périard JD. Health status, heat preparation strategies and medical events among elite cyclists who competed in the heat at the 2016 UCI Road World Cycling Championships in Qatar. Br J Sports Med. 2020;54(16):1003–7.
Racinais S, Périard JD. Benefits of heat re-acclimation in the lead-up to the Tokyo Olympics. Br J Sports Med. 2020;54:945–6.
Sandford GN, Stellingwerff T, Koehle MS. Ozone pollution: a ‘hidden’ environmental layer for athletes preparing for the Tokyo 2020 Olympics & Paralympics. Br J Sports Med. 2021;55:189–90.
Saunders PU, Garvican-Lewis LA, Chapman RF, Périard JD. Special environments: altitude and heat. Int J Sport Nutr Exerc Metab. 2019;29(2):210–9.
Sawka MN, Cheuvront SN, Kenefick RW. Hypohydration and human performance: impact of environment and physiological mechanisms. Sports Med. 2015;45(Suppl 1):S51-60.
Schipper K, Bakker M, De Wit M, Ket JC, Abma TA. Strategies for disseminating recommendations or guidelines to patients: a systematic review. Implement Sci. 2016;11(1):82.
Singh G, Bennett K, Taylor L, Stevens C. Core body temperature responses during competitive sporting events: a narrative review. Biol Sport. 2023;40(4):1003–17.
Singh NR, Denissen EC, Mckune AJ, Peters EM. Intestinal temperature, heart rate, and hydration status in multiday trail runners. Clin J Sport Med 2012;22:311–8.
Stephenson BT, Hoekstra SP, Tolfrey K, Goosey-Tolfrey VL. High thermoregulatory strain during competitive paratriathlon racing in the heat. Int J Sports Physiol Perform. 2020;15:231–7.
Stevens CJ, Heathcote SL, Plews DJ, Laursen PB, Taylor L. Effect of two-weeks endurance training wearing additional clothing in a temperate outdoor environment on performance and physiology in the heat. Temperature (Austin). 2018;5(3):267–75.
Stevens CJ, Mauger AR, Hassmèn P, Taylor L. Endurance performance is influenced by perceptions of pain and temperature: theory, applications and safety considerations. Sports Med. 2018;48(3):525–37.
Stevens CJ, Ross ML, Carr AJ, Vallance B, Best R, Urwin C, Périard JD, Burke L. Postexercise hot-water immersion does not further enhance heat adaptation or performance in endurance athletes training in a hot environment. Int J Sports Physiol Perform. 2020;16(4):480–8.
Stevens CJ, Ross ML, Périard JD, Vallance BS, Burke LM. Core temperature responses to elite racewalking competition. Int J Sports Physiol Perform. 2020;15(6):892–5.
Stevens CJ, Taylor L, Dascombe BJ. Cooling during exercise: an overlooked strategy for enhancing endurance performance in the heat. Sports Med. 2017;47(5):829–41
Sugawara M, Manabe Y, Yamasawa F, Hosokawa Y. Athlete medical services at the marathon and race walking events during Tokyo 2020 olympics. Front Sports Act Living. 2022;4:872475.
Taylor L, Carter S, Stellingwerff T. Cooling at Tokyo 2020: the why and how for endurance and team sport athletes. Br J Sports Med. 2020;54(21):1243–5.
Taylor L, Watkins SL, Marshall H, Dascombe BJ, Foster J. The impact of different environmental conditions on cognitive function: a focused review. Front Physiol. 2015;6:372.
Taylor NA. Eccrine sweat glands. Adaptations to physical training and heat acclimation. Sports Med. 1986;3(6):387–97.
Taylor NA. Human heat adaptation. Compr Physiol. 2011;4(1):325–65.
Topham TH, Smallcombe JW, Clark B, Brown HA, Telford RD, Jay O, Périard JD. Influence of sex and biological maturation on the sudomotor response to exercise-heat stress: are girls disadvantaged? Am J Physiol Regul Integr Comp Physiol. 2022;323(2):R161–8.
Tyler CJ, Reeve T, Hodges GJ, Cheung SS. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med. 2016;46(11):1699–724.
Van Daalen KR, Romanello M, Rocklov J, Semenza JC, Tonne C, Markandya A, Dasandi N, Jankin S, Achebak H, Ballester J, Bechara H, Callaghan MW, Chambers J, Dasgupta S, Drummond P, Farooq Z, Gasparyan O, Gonzalez-Reviriego N, Hamilton I, Hanninen R, Kazmierczak A, Kendrovski V, Kennard H, Kiesewetter G, Lloyd SJ, Lotto Batista M, Martinez-Urtaza J, Mila C, Minx JC, Nieuwenhuijsen M, Palamarchuk J, Quijal-Zamorano M, Robinson EJZ, Scamman D, Schmoll O, Sewe MO, Sjodin H, Sofiev M, Solaraju-Murali B, Springmann M, Trinanes J, Anto JM, Nilsson M, Lowe R. The 2022 Europe report of the Lancet Countdown on health and climate change: towards a climate resilient future. Lancet Public Health. 2022;7(11):e942–65.
Veltmeijer MT, Eijsvogels TM, Thijssen DH, Hopman MT. Incidence and predictors of exertional hyperthermia after a 15-km road race in cool environmental conditions. J Sci Med Sport 2015;18:333–7.
Wald A, Demorest S. Race to beat the heat: climate change impacts physical activity. J Nurse Pract. 2022;18(4):388–94.
Weinman KP, Slabochova Z, Bernauer EM, Morimoto T, Sargent F 2nd. Reactions of men and women to repeated exposure to humid heat. J Appl Physiol. 1967;22(3):533–8.
Wickham KA, Wallace PJ, Cheung SS. Sex differences in the physiological adaptations to heat acclimation: a state-of-the-art review. Eur J Appl Physiol. 2021;121(2):353–67.
Wilby RL, Orr M, Depledge D, Giulianotti R, Havenith G, Kenyon JA, Matthews TKR, Mears SA, Mullan DJ, Taylor L. The impacts of sport emissions on climate: measurement, mitigation, and making a difference. Ann N Y Acad Sci. 2023;1519(1):20–33.
Willmott AGB, Hayes M, Waldock KAM, Relf RL, Watkins ER, James CA, Gibson OR, Smeeton NJ, Richardson AJ, Watt PW, Maxwell NS. Short-term heat acclimation prior to a multi-day desert ultra-marathon improves physiological and psychological responses without compromising immune status. J Sports Sci. 2017;35(22):2249–56.
WMO. WMO Global Annual to Decadal Climate Update (Target years: 2023–2027). 2023. https://library.wmo.int/index.php?lvl=notice_display&id=22272#.ZGS-wnZBxD. Accessed 17 May 2023.
Wyndham CH, Strydom NB. The danger of an inadequate water intake during marathon running. S Afr Med J. 1969;43:893–6.
Yankelson L, Sadeh B, Gershovitz L, Werthein J, Heller K, Halpern P, Halkin A, Adler A, Steinvil A, Viskin S. Life-threatening events during endurance sports: is heat stroke more prevalent than arrhythmic death? J Am Coll Cardiol. 2014;64(5):463–9.
Yanovich R, Ketko I, Charkoudian N. Sex differences in human thermoregulation: relevance for 2020 and beyond. Physiology (Bethesda). 2020;35(3):177–84.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Chris Esh, Lee Taylor and Sarah Carter conceived and designed the work. All other authors make substantial contributions during the drafting, editing and revising of the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
N/A.
Consent to participate
N/A.
Consent to Publish
N/A.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Esh, C.J., Carter, S., Galan-Lopez, N. et al. A Review of Elite Athlete Evidence-Based Knowledge and Preparation for Competing in the Heat. J. of SCI. IN SPORT AND EXERCISE (2024). https://doi.org/10.1007/s42978-024-00283-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42978-024-00283-y