Abstract
Purpose
Cystic Fibrosis (CF) is a multisystem disease associated with symptoms such as dyspnoea, tachycardia and tachypnea that may be related to changes in autonomic function and sensitive to improvement following inspiratory muscle training (IMT). The aim of the present study was to investigate the effect of IMT on heart rate variability (HRV) and respiratory function in children.
Methods
Five CF and five matched controls (40% boys) performed a 4-weeks IMT programme, involving 30 breaths, twice a day. Weeks 1–2 of training were set at 40% of a participant’s maximal strength index (S.Index), with week’s 3–4 set at 50%. Participants wore an ActiHeart for three consecutive days at baseline and post-intervention and indices of HRV were derived. Standard measures of lung function were obtained along with health-related quality of life (HRQoL) using the CF-specific questionnaire (CFQ-R).
Results
IMT elicited clinically meaningful increases in respiratory muscle strength and respiratory symptom domain scores, but no improvements in respiratory volume, irrespective of group. Similarly, no significant improvements were found in HRQoL despite 62.5% of the population increased their HRQoL score. Post-intervention, CF participants showed a clinically meaningful decrease in the very low frequency (VLF) domain.
Conclusion
These results may indicate clinically meaningful changes in HRV and inspiratory muscle strength following a 4-week IMT intervention, although a more powerful study is required to draw further conclusions. Indeed, the trends for improved HRQoL support the need for such studies to ascertain the potential therapeutic role of IMT in those with CF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic Fibrosis (CF) is the most common, inherited, life-shortening condition among Caucasians, with an estimated population of 10,469 in the UK alone [9]. It is a multisystem disease affecting the respiratory, gastrointestinal, reproductive tract and sweat glands [22]. In addition to respiratory dysfunction, cardiac damage may also be present in those with CF, with primary symptoms including dyspnoea, tachycardia and tachypnoea [20]. Such symptoms may be attributed to β-2 agonist use, with hypoxemia potentially exacerbating cardiac autonomic dysfunction [20].
In those with CF, the autonomic nervous system may be influenced by the interaction between cardiac and pulmonary dysfunction [20]. Heart rate variability (HRV) provides an insight to the autonomic nervous system and can provide an early indication of damage to the cardiac system [58] and increased risk of cardiac mortality [57]. However, whether CF is associated with derangements in autonomic nervous system function is equivocal, with some reporting similar sympathovagal function during a six-minute walk test (6MWT) [20], whilst others found higher sympathetic [46] and/or lower parasympathetic tone in children with CF at rest and during recovery [20]. In adults with CF, further derangements in autonomic functions have yet to be demonstrated in children with CF, which may reflect age-related modulations and/or the progression of the disease itself [33]. Alternatively, or additionally, the apparent age-related differences may reflect differences in fitness [26] or the impact of medication [50]. Irrespective of the mechanisms for these differences, it is suggested that deleterious adaptations in HRV are associated with an increased risk of cardiovascular complications [39]. Therefore, improving HRV in those with CF is paramount to their physiological and psychological health.
Inspiratory muscle training (IMT), a breathing exercise that aims to strengthen the respiratory muscles by using a restricted airflow breathing technique to increase the load placed upon the intercostal muscles and diaphragm, has been shown to stimulate a hypertrophic response [18]. In adults with hypertension and diabetes, IMT has been shown to significantly enhance cardiac autonomic modulation in comparison to unloaded IMT [19, 30]. Furthermore, a respiratory muscle feedback and breathing retraining program in adults with CF elicited significant improvements in forced expiratory volume in 1 s (FEV1) and mean expiratory flow during forced vital capacity (FVC) compared to an age and severity matched control group [16]. In children with CF, IMT increases inspiratory muscle strength (IMS) [51, 52], vital capacity, total lung capacity and exercise tolerance [52], as well as respiratory muscle endurance [5]. In healthy individuals and those with heart failure, improvements in respiratory muscle function following a 12-weeks IMT are associated with an enhanced metaboreflex activation threshold, resulting in decreased cardiac sympathetic output at rest [14, 25, 61]. However, whether similar beneficial adaptations to automatic nervous system (ANS) control following IMT are observed in those with CF remains to be elucidated.
In addition to potential physiological adaptations, IMT has also been suggested to elicit positive benefits on quality of life (QoL) [15], anxiety and depression in CF adults [17]. Little data is available in children with CF, but a weak correlation between HRV and QoL has been observed in healthy children and adolescents, with suggestions that a stronger correlation would be evident in chronically ill children [54]. Interventions that simultaneously promote improvements in lung function and QoL are highly desirable, especially for those with CF who already face a substantial, time consuming, treatment schedule.
Therefore, the aim of this study was to ascertain the effects of IMT on cardiac autonomic control (HRV), lung function and QoL in children with CF compared to their healthy counterparts.
Materials and Methods
Five CF and five matched control participants aged 10.4 ± 1.2 years (40% boys) were recruited from a CF unit in South Wales, from a local school and through University staff emails, respectively. Participants were recruited on the basis of meeting the following criteria: (1) documented clinical features of CF as well as an abnormal sweat test (sweat sodium and chloride 60 mmol/L); (2) absence of any additional known illness/or disease in CF patients or absence of any known illness or disease in healthy controls; and (3) voluntary participation and consent to comply with the study protocol. Ethical approval was obtained from the Bromley National Health Service Research Ethics Committee (REC reference: 13/LO/1907) and written informed assent and consent were obtained from participants and their parents/guardian, respectively. Participants were required to attend two testing visits in total (baseline and post-intervention), which both took place within a week before the first or after the last IMT session.
Participants were supplied with their own personal POWERbreathe Plus device (POWERbreathe Plus LR Level 1, Gaiam Ltd. E & OE, UK) and undertook a familiarisation session to ensure that they were comfortable with the training and device. Participants were encouraged to practice breathing technique and ask any questions until they were comfortable with the regime, which involved 30 breaths twice a day, for 28 consecutive days. The device resistance was determined by the participants baseline strength index (S.Index). Specifically, the first two weeks of the training programme were performed at 40% of participant’s pre-IMT maximal S.Index, with the remaining two weeks at 50%.
Anthropometrics
Anthropometrical characteristics were measured according to standard procedures pre- and post-intervention. Specifically, body mass was measured to the nearest 0.01 kg (Seca 899 flat scale, Seca, UK), stature and sitting stature were measured to the nearest 0.01 m (Seca portable stadiometer, Seca, UK). Waist and hip circumference were measured to the nearest 0.01 m using a non-elastic anthropometric tape (Seca Ltd, Birmingham, UK) at the narrowest point between the bottom of the ribs and the iliac crest and around the widest point of the buttocks [59]. Maturity offset was calculated using the equations developed by Moore et al. [37] (Table 1).
Heart Rate Variability
Participants were required to wear an ActiHeart (Actiheart4, Camntech Ltd, Cambridge, UK) recording at 126 Hz for three consecutive days. The ActiHeart, which has high intra-and inter-instrument reliability and demonstrates good validity [6], comprises of two standard ECG electrodes adhered at V1 or V2 positions and approximately 10 cm away on the left side at V4 or V5. This specific placement ensures a better signal to noise ratio, free from movement artefacts and with higher ECG amplitudes [6]. At least two complete 24-h RR recordings were used to obtain HRV parameters which were subsequently averaged. The analogue signal from the ActiHeart was band-pass filtered (10–35 Hz) and processed by a real time QRS-detection algorithm. The RR data also underwent visual examination in order to verify the accuracy of the data prior to subsequent analysis. When the RR interval(s) was anomalous, the RR data points were removed from the data set. Indices of HRV were derived from the frequency domain [very low frequency (VLF, 0.017–0.04 Hz), low frequency (LF, 0.04–0.15 Hz), high frequency (HF, 0.15–0.4 Hz) power, LF:HF ratio] according to the guidelines of the Task Force [57] and presented as relative values. Prior to the frequency domain analysis procedures RR interval data were re-sampled using a sampling frequency of 2 Hz and then linearly de-trended and windowed in consecutive one-minute segments; the power spectral density of each segment was then calculated using the Welch periodogram method, using short-term Fourier transformation and a 50% overlap between adjacent segments.
Inspiratory Function Measurements
Inspiratory muscle function and capacity were measured using the POWERbreathe K5 (HaB International Ltd, UK). The K5 was programmed with the participant’s age, stature, mass and sex, and, following a familiarisation session, three maximal inspiratory efforts were performed. Inspiratory volume (L), flow rate (L/s) and S.Index (cmH2O) were recorded and the average calculated across all three tests (Table 1).
Cystic Fibrosis Questionnaire—Revised (CFQ-R)
All participants completed the age-appropriate version of the CFQ-R [35, 41], a disease-specific patient reported outcome designed to measure the physical, social and emotional impact of CF on a four point Likert, true–false or frequency scale. The CFQ-R child version consists of 35 items grouped into the following categories: (i) physical symptoms (6); (ii) emotional functioning (8); (iii) social functioning (7); (iv) body image (3); (v) eating disturbance (3); (vi) treatment burden (3); (vii) respiratory (4); and (viii) digestive symptoms (1). Those participants aged 6–11 years undertook an interviewer-administered version of the CFQ-R, whilst 12-year olds completed the self-report version. Control participants were excluded from treatment specific questions and their overall score was made relative to account for the reduced number of questions completed. Moreover, parent/guardians completed a 44-item CFQ-R questionnaire based on their perceptions of their child’s QoL. Raw scores from the CFQ-R Child and Parent/guardian questionnaires were standardised to a 0–100 scale, with a higher score indicative of a higher HRQoL. For the respiratory symptom domain, the minimal clinically important difference (MCID) was defined as a change of 4.0 points [42].
Data Analysis
Between group characteristics and anthropometrics were compared at baseline using an independent t-test. A repeated measures ANOVA was used to analyze lung function and HRV in response to the IMT intervention and their interaction with disease status. The MCIDS were calculated using distribution-based methods. Specifically, changes in HRV and lung function from baseline to follow-up were calculated as 0.5 multiplied by SD of baseline. Scores are shown as the proportion of individuals whose scores exhibited a clinically meaningful increase or decrease, in lung function or HRV of ≥ 0.05 SD. Effect size was calculated using the mean change in scores divided by the SD of baseline scores [11]. For interpreting effect sizes, Cohen (1988) has proposed the following benchmarks: 0.2 (small), 0.50 (moderate) and 0.80 (large). A moderate effect size is considered a clinically important effect [23]. Pearson’s correlation coefficients were used to assess the relationship between CFQ-R domains, HRV and lung function, with Cronbach’s Alpha used to measure internal consistency within the questionnaires [12]. Internal consistency was good for CF children (α = 0.83–0.98), CF parents (α = 0.92–0.95), control children (α = 0.72–0.79) and adequate for control parents (α = 0.55–0.59). For the CFQ-R, change scores were compared to established MCID scores in the paediatric CF population [36, 42]. All data was analysed using a statistical software package (IBM SPSS, Version 25.0) and is presented as Mean ± SD. Statistical significance was accepted as P < 0.05.
Results
Lung Function
There was no significant difference in lung function between those with and without CF at baseline. IMT elicited increases in lung function, irrespective of group. Specifically, in those with CF, S.Index and flow rate significantly increased by 18.3% and 18.1%, respectively, whilst in the healthy children, S.Index and flow increased by 31% and 57%, respectively (Table 2). In contrast, there was not a significant intervention effect on volume in either group. All CF participants exhibited a large clinically meaningful increase in S.Index (d = 8.0) and flow rate (d = 9.9), but only 25% showed a clinically meaningful increase in volume which was associated with a small effect size (d = 0.3). When the absolute magnitude of change was considered, the healthy children demonstrated greater increases in flow rate (1.0 ± 0.9 vs. 0.6 ± 0.3 L/s; P < 0.05) and S.Index (14.8 ±11.3 vs. 10.5 ± 5.6 cmH2O; P < 0.05) than those with CF.
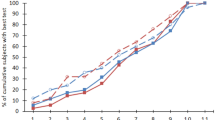
Heart Rate Variability
At baseline, frequency domain measures were not significantly different between those with CF and their healthy peers. A repeated measures ANOVA with a Greenhouse–Geisser correction determined that frequency domain indices did not differ significantly between time-points. Specifically, while IMT in those with CF was associated with an increase in VLF (1.7%), HF (1.8%) and LF:HF (0.2), and a reduction in LF (− 1.6%) post-intervention, these were not statistically significant. However, changes in VLF exhibited a moderate clinically meaningful decrease (d = 0.6), while other HRV parameters exhibited small to trivial clinical effect in CF (Table 3). In contrast, in the healthy group, reductions in VLF (− 2.7%) and LF:HF (− 0.29) and an increase in LF (0.7%) and HF (2.1%) were observed post-IMT but were not statistically significant.
CFQ-R
There was no significant difference in HRQoL over time, irrespective of disease status. However, 62.5% of the population increased their HRQoL post-intervention. At baseline, the CFQ-R respiratory domain demonstrated a weak negative correlation with S.Index (r = − 0.29) and flow rate (r = − 0.23) and a weak positive correlation with volume (r = 0.24). After the intervention, the respiratory domain of the CFQ-R showed a strong negative correlation with S.Index (r = − 0.85; P = 0.008) and flow rate (r = − 0.84; P = 0.009). The respiratory symptom domain change score indicated that CF participants perceived clinically meaningful improvements.
Similar to their children, parent/guardian’s perceptions of their child’s HRQoL did not differ between time-points. The CF group showed no significant difference in perceived HRQoL between child and parents at baseline (child 88.9% ± 7.5%; parent 90.9% ± 7.7%) or post-intervention (child 89.3% ± 8.8%; parent 90.7% ± 8.4%).
Discussion
The main finding of this pilot study was that IMT elicited clinically meaningful improvements in S.Index and flow rate, indicative of improvements in IMS, irrespective of health status. Whilst the mechanistic basis of these changes in lung function remains to be elucidated, there were some indications of changes in parasympathetic modulation, although these were not significant and a clinically meaningful decrease in sympathetic modulation. In line with the changes in lung function, IMT elicited a perceived improvement in the respiratory symptom domain in CF participants. Overall, the current study provides preliminary indications that the benefits of IMT should be considered to extend to cardiovascular, as well as respiratory, function, and highlights that further work is warranted to ascertain the potential therapeutic benefits of IMT for children with CF.
The significant improvements in S.Index following the 4-weeks IMT intervention are congruent with previous research in adults [1, 15, 17, 52] and children with CF [1]. Indeed, Asher et al. [1] found significant improvements in IMS and endurance following a 4-weeks training programme of 15 min twice per day, in children and adults with CF. However, in contrast to the present study, Asher et al. [1] used a substantially higher training intensity of 80% maximal inspiratory pressure (MIP). Similarly, Sawyer and Clanton [52] reported improvements in IMS following a protocol involving 60% MIP, 30 min a day for 10 weeks and de Jong et al. [15] noted improvements in inspiratory muscle endurance following training at 20%–40% MIP for 20 min, five days a week for 6-weeks. Although the optimal training intensity, duration and frequency clearly remains to be elucidated, research suggests that the specific combination used may influence the specific respiratory parameters effected. Specifically, it appears that low intensity training elicits improvements in inspiratory muscle endurance whilst high-intensity training influences IMS [45]. Interestingly, in accord with whole body strength training regimens, it has been suggested that during the first four weeks IMT predominantly induces neural adaptations [7, 44], with any improvements thereafter considered to be largely related to morphological adaptations [21]. Therefore, given the 18% clinically meaningful improvement in S.Index observed in the current study, it could be postulated that 40% MIP is the minimum intensity required to elicit significant benefits in IMS. However, it appears that a longer duration and/or greater resistance may be required to elicit changes in lung volume. Indeed, Enright et al. [18] found significant improvements in lung volume at 80% MIP resistance, but not 20% MIP, this study extends this finding to suggest that greater than 40% MIP is required. The current findings highlight the importance of tailoring the resistance to the desired outcome, whilst being cognisant that lower resistances are likely to be associated with better long-term adherence and perceptions of feasibility and enjoyment [32].
Inspiratory muscle training engendered clinically meaningful improvements in flow rate in those with CF (18.1%) but not in their healthy counterparts. This may be attributable to the slightly, albeit not significantly, lower values at baseline in those with CF, given that baseline “fitness” is broadly associated with the magnitude of response to training interventions [49]. However, this finding may also reflect a better adherence to the IMT protocol in those with CF. Whilst measurement of adherence was beyond the scope of the present study, those with CF have been reported to enjoy and perceive the benefits of IMT for their health associated with CF [32]. An improved flow rate has been associated with greater capacity for gas exchange due to more time available for alveolar emptying [10], while reduced respiratory comfort has been attributed to decreases in inspiratory flow rate [31]. Therefore, it could be hypothesised that improving inspiratory flow rate may enhance the efficiency of the respiratory system and feelings of discomfort. Indeed, in chronic obstructive pulmonary disease (COPD), IMT has been shown to enable deeper breaths and higher inspiratory flows, reducing inspiratory effort and dyspnoea scores [13]. However, whether this is similarly applicable in those with CF requires further investigation.
This is the first study to investigate the influence of IMT on HRV in CF despite the inextricable associations and interrelations between cardiovascular and respiratory systems [38, 62]. At rest, the CF group had a higher LF:HF, suggested to be indicative of a higher sympathetic activity [2] and in accord with previous studies [20, 33]. Although the exact mechanisms underpinning this CF-related adaptation remain inconclusive at this time, such findings could be attributed to alterations in respiratory patterns [40], differences in participant age and its interaction with disease progression [33], higher work of breathing [29] or, indeed, differences in the levels of catecholamines, between those with and without CF [63]. Whilst the decrease in LF and LF:HF in the CF group following IMT was not significant, the clinically meaningful decrease in VLF could result in a reduction in the sympathetic tone relative to parasympathetic tone [56]. Previous research has suggested that inspiratory muscle fatigue increases the metaboreflex, which increases peripheral sympathetic activity; improving respiratory muscle function by IMT may therefore increase fatigue resistance and lessen sympathetic outflow [19]. However, this remains speculative given the lack of power associated with this pilot study. Nonetheless, the current results are similar to previous IMT studies in healthy adults that reported 8-weeks IMT, 20 min a day at 30% MIP increased S.Index and HF and decreased LF [19], with others reporting the same protocol was associated with an increased lung volume and QoL [34]. However, the studies of Ferreira et al. [19] and Mello et al. [34] were of a longer duration and in older populations with cardiothoracic complications, which may explain the significant improvements in cardiac function. Previous research has shown that respiratory patterns alter autonomic cardiovascular modulation, especially with respect to HF [57], which could explain the increase in parasympathetic modulation observed in the current study. Further studies should seek to determine the acute HRV response during, and following, IMT.
Inspiratory muscle training may improve oxygen supply by augmenting tidal volume, leading to a reduction in chemoreflex activity and, consequently, decreased sympathetic nerve discharge [4, 48]. According to previous research in healthy adults, inspiratory loads lower than 60% of MIP do not engender diaphragm fatigue as the metaboreflex of the inspiratory muscles is not activated and therefore sympathetic tone is not increased [8]. Reduced lung function is related to sympathetic overactivity in those with bronchiectasis and COPD, suggesting an increased cardiorespiratory risk [43]. Therefore, if IMT has the potential to improve HRV, it may improve lung function in those with CF, or vice versa.
In accord with some [5], but not all [18], previous studies, IMT had no significant impact on QoL. However, it is important to acknowledge that Enright et al. [18] researched adults who may have had more severe impairments in lung function, and thus QoL, and improvements may therefore be more likely to be evident following IMT given the lower baseline. In children, the CFQ may also lack the sensitivity to reveal small treatment effects in stable patients, but no alternative scoring system for short-term changes in symptoms and clinical findings is currently available [5]. Alternatively, this discrepancy may be related to the length of the intervention, indicating that longer interventions are needed to induce significant improvements in QoL in children [28, 53]. Despite this, the change in the respiratory domain scores, while not statistically significant, was clinically meaningful post IMT. Furthermore, the respiratory domain, S.index and flow were significantly correlated following IMT. A recent systematic review reported that lung function was consistently associated with respiratory symptoms within the CFQ-R and should be considered an important outcome measure in CF [24]. However, there is limited research regarding the relationship between QoL and IMT, with HRQoL remaining an underutilised tool that should be more widely incorporated into future IMT research.
Whilst there are numerous strengths, it is important to consider certain limitations in the interpretation of this study. We acknowledge the controversy that surrounds interpretation of HF, LF and LF:HF [27], however, HRV is a non-invasive tool that provides prognostic insight into global cardiovascular health [47, 57, 60]. The small sample size limits our statistical power and a larger study is required to ratify our findings. Given the challenges of obtaining large sample sizes of participants with CF [36], the application of MCID suggests whilst our results are statistically significant, they were also clinically meaningful, highlighting the potential impact of IMT within the CF population [3]. The short duration of our intervention may also be perceived as a limitation, although it also increases the ecological validity of the findings as it more closely replicates how IMT may be used as an adjunct therapeutic strategy. Indeed, individual responses to exercise training are highly variable and distinguishing patients with- and without-significant, and clinically relevant training responses is a key factor in the identification of effective interventions, ensuring a patient-centred approach. Furthermore, the consideration of intervention fidelity, adherence and the factors that underpin these, which were not assessed in the present study, must be considered in future studies wishing to investigate the potential therapeutic role of IMT in those with CF.
In conclusion, 4-weeks of IMT led to clinically significant increases in IMS and in the respiratory symptom domain, while potentially having important influences on the autonomic nervous system in those with CF. Overall, preliminary indications suggest that IMT could be considered to benefit respiratory and cardiovascular function in children with CF.
Data Availability
Due to the small sample size and potentially identifiable markers, the data will not be made available.
Code Availability
Not applicable.
References
Asher MI, Pardy RL, Coates AL, Thomas E, Macklem PT. The effects of inspiratory muscle training in patients with cystic fibrosis. Am Rev Resp Dis. 1982;126(5):855–9. https://doi.org/10.1164/arrd.1982.126.5.855.
Bartur G, Vatine JJ, Raphaely-Beer N, Peleg S, Katz-Leurer M. Heart rate autonomic regulation system at rest and during paced breathing among patients with CRPS as compared to age-matched healthy controls. Pain Med. 2014;15(9):1569–74. https://doi.org/10.1111/pme.12449.
Beaton DE, Boers M, Wells GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheumatol. 2002;14(2):109–14. https://doi.org/10.1097/00002281-200203000-00006.
Bernardi L, Porta C, Gabutti A, Spicuzza L, Sleight P. Modulatory effects of respiration. Auton Neurosci. 2001;90(1–2):47–56. https://doi.org/10.1016/S1566-0702(01)00267-3.
Bieli C, Summermatter S, Boutellier U, Moeller A. Respiratory muscle training improves respiratory muscle endurance but not exercise tolerance in children with cystic fibrosis. Pediatr Pulm. 2017;52(3):331–6. https://doi.org/10.1002/ppul.23647.
Brage S, Brage N, Franks PW, Ekelund U, Wareham NJ. Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur J Clin Nutr. 2005;59(4):561–70. https://doi.org/10.1038/sj.ejcn.1602118.
Brown SJ, Child RB, Day SH, Donnelly AE, Row N, JChildDonnelly SRBAE. Exercise-induced skeletal muscle damage and adaptation following repeated bouts of eccentric muscle contractions Exercise-induced skeletal m uscle damage and adaptation following repeated bouts of eccentric m uscle contractions. J Sports Sci. 1997;15(2):215–22. https://doi.org/10.1080/026404197367498.
Callegaro CC, Ribeiro JP, Tan CO, Taylor JA. Attenuated inspiratory muscle metaboreflex in endurance-trained individuals. Resp Physiol Neurobi. 2011;177(1):24–9. https://doi.org/10.1016/j.resp.2011.03.001.
Charman S, Connon R, Cosgriff R, Lee A, Carr S. UK cystic fibrosis registry annual data report 2017. Cystic Fibrosis Trust. 2018; 1–80. https://cysticfibrosis.org.uk/registryreports.
Connors AF, McCaffree DR, Gray BA. Effect of inspiratory flow rate on gas exchange during mechanical ventilation. Am Rev Respir Dis. 1981;124(5):537–43. https://doi.org/10.1164/arrd.1981.124.5.537.
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7(5):541–6. https://doi.org/10.1016/j.spinee.2007.01.008.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. https://doi.org/10.1007/BF02310555.
Dacha S, Langer D, Ciavaglia C, Webb K, Preston M, O’Donnell DE. Effect of inspiratory muscle training (IMT) on static and dynamic respiratory muscle function in patients with COPD. Physiotherapists. 2017;50(suppl 61):OA2923. https://doi.org/10.1183/1393003.congress-2017.OA2923.
Dall’Ago P, Chiappa GRS, Guths H, Stein R, Ribeiro JP. Inspiratory muscle training in patients with heart failure and inspiratory muscle weakness. J Am Coll Cardiol. 2006;47(4):757–63. https://doi.org/10.1016/j.jacc.2005.09.052.
de Jong W, Van Aalderen WMC, Kraan J, Ter Ko GH, Van Der Schans CP. Inspiratory muscle training in patients with cystic fibrosis. Respir Med. 2001;95:31–6. https://doi.org/10.1053/rmed.2000.0966.
Delk KK, Gevirtz R, Hicks DA, Carden F, Rucker R. The effects of biofeedback assisted breathing retraining on lung functions in patients with cystic fibrosis. Chest. 1994;105(1):23–8.
Enright S, Chatham K, Ionescu AA, Unnithan VB, Shale DJ. Inspiratory muscle training improves lung function and exercise capacity in adults with cystic fibrosis. Chest. 2004;126(2):405–11. https://doi.org/10.1378/chest.126.2.405.
Enright SJ, Unnithan VB, Heward C, Withnall L, Davies DH. Effect of high-intensity inspiratory muscle training on lung volumes, diaphragm thickness, and exercise capacity in subjects who are healthy. Phys Ther. 2006;86(3):345–54. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16506871.
Ferreira JB, Plentz RDM, Stein C, Casali KR, Arena R, Lago PD. Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J Cardiol. 2013;166(1):61–7. https://doi.org/10.1016/j.ijcard.2011.09.069.
Florêncio R, Fregonezi G, Brilhante S, Borghi-Silva A, Dias F, Resqueti V. Heart Rate Variability at rest and after the 6-minute walk test (6MWT) in children with cystic fibrosis. Braz J Phys Ther. 2013;17(5). https://doi.org/10.1590/S1413-35552012005000109.
Folland J, Williams AG. The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med. 2007;37:145–68.
Goetzinger KR. Cystic fibrosis. Obstetric Imaging. 2018;579–581.e1. https://doi.org/10.1016/B978-0-323-44548-1.00141-8.
Guyatt GH, Walter S, Norman G. Measuring change over time: assessing the usefulness of evaluative instruments. J Chron Dis. 1987;40(2):171–8. https://doi.org/10.1016/0021-9681(87)90069-5.
Habib ARR, Manji J, Wilcox PG, Javer AR, Buxton JA, Quon BS. A systematic review of factors associated with health-related quality of life in adolescents and adults with cystic fibrosis. Ann Am Thorac Soc. 2015;12(3):420–8. https://doi.org/10.1513/AnnalsATS.201408-393OC.
HajGhanbari B, Yamabayashi C, Buna TR, Coelho JD, Freedman KD, Morton TA, Reid WD. Effects of respiratory muscle training on performance in athletes. J Strength Cond Res. 2013;27(6):1643–63. https://doi.org/10.1519/JSC.0b013e318269f73f.
Hautala AJ, Karjalainen J, Kiviniemi AM, Kinnunen H, Mäkikallio TH, Huikuri HV, Tulppo MP. Physical activity and heart rate variability measured simultaneously during waking hours. Am J Physiol-Heart C. 2010;298(3):H874–H880880. https://doi.org/10.1152/ajpheart.00856.2009.
Hayano J, Yuda E. Pitfalls of assessment of autonomic function by heart rate variability. J Physiol Anthropol. 2019;38(1):3. https://doi.org/10.1186/s40101-019-0193-2.
Hebestreit H, Kieser S, Junge S, Ballmann M, Hebestreit A, Schindler C, Kriemler S. Long-term effects of a partially supervised conditioning programme in cystic fibrosis. Eur Respir J. 2010;35(3):578–83. https://doi.org/10.1183/09031936.00062409.
Heindl S, Lehnert M, Criee CP, Hasenfuss G, Andreas S. Marked sympathetic activation in patients with chronic respiratory failure. Am J Respir Crit Care Med. 2001;164(4):597–601. https://doi.org/10.1164/ajrccm.164.4.2007085.
Kaminski DM, Schaan BD, da Silva AMV, Soares PP, Lago PD. Inspiratory muscle training in patients with diabetic autonomic neuropathy: a randomized clinical trial. Clin Auton Res. 2015;25(4):263–6. https://doi.org/10.1007/s10286-015-0291-0.
Manning HL, Schwartzstein RM. Pathophysiology of dyspnea. N Eng J Med. 1995;333(23):1547–53. https://doi.org/10.1056/NEJM199512073332307.
McCreery JL, Mackintosh KA, Cox NS, McNarry MA. Assessing the perceptions of inspiratory muscle training in children with cystic fibrosis and their multidisciplinary team: mixed-methods study. JMIR Pediatr Parent. 2018;1(2):e11189. https://doi.org/10.2196/11189.
McNarry MA, Mackintosh KA. Reproducibility of heart rate variability indices in children with cystic fibrosis. PLoS ONE. 2016;11(3):e0151464. https://doi.org/10.1371/journal.pone.0151464.
Mello PR, Guerra GM, Borile S, Rondon MU, Alves MJ, Negrão CE, Consolim-Colombo FM. Inspiratory muscle training reduces sympathetic nervous activity and improves inspiratory muscle weakness and quality of life in patients with chronic heart failure. J Cardiopul Rehabil Prev. 2012;32(5):255–61. https://doi.org/10.1097/HCR.0b013e31825828da.
Modi AC, Quittner AL. Validation of a disease-specific measure of health-related quality of life for children with cystic fibrosis. J Pediatr Psychol. 2003;28(8):535–45.
Modi AC, Lim CS, Driscoll KA, Piazza-Waggoner C, Quittner AL, Wooldridge J. Changes in pediatric health-related quality of life in cystic fibrosis after IV antibiotic treatment for pulmonary exacerbations. J Clin Psychol Med Settings. 2010;17(1):49–55. https://doi.org/10.1007/s10880-009-9179-2.
Moore SA, McKay HA, Macdonald H, Nettlefold L, Baxter-Jones ADG, Cameron N, Brasher PMA. Enhancing a somatic maturity prediction model. Med Sci Sports Exerc. 2015;47(8):1755–64. https://doi.org/10.1249/MSS.0000000000000588.
Pinsky MR. Cardiovascular issues in respiratory care. Chest. 2005;128(5):592S–7S. https://doi.org/10.1378/CHEST.128.5_SUPPL_2.592S.
Pivatelli F, dos Santos M, Fernandes G, Gatti M, de Abreu L, Valenti VE, de Godoy MF. Sensitivity, specificity and predictive values of linear and nonlinear indices of heart rate variability in stable angina patients. Int Arch Med. 2012;5(1):31. https://doi.org/10.1186/1755-7682-5-31.
Pöyhönen M, Syväoja S, Hartikainen J, Ruokonen E, Taka J. The effect of carbon dioxide, respiratory rate and tidal volume on human heart variability. Acta Anaesthesiol Scand. 2004;48(1):93–101.
Quittner AL, Sweeny S, Watrous M, Munzenberger P, Bearss K, Nitza AG, Henry B. Translation and linguistic validation of a disease-specific quality of life measure for cystic fibrosis. J Pediatri Psychol. 2000;25(6):403–14. https://doi.org/10.1093/jpepsy/25.6.403.
Quittner AL, Modi AC, Wainwright C, Otto K, Kirihara J, Montgomery AB. Determination of the minimal clinically important difference scores for the Cystic Fibrosis Questionnaire-Revised respiratory symptom scale in two populations of patients with cystic fibrosis and chronic Pseudomonas aeruginosa airway infection. Chest. 2009;135(6):1610–8. https://doi.org/10.1378/chest.08-1190.
Rached S, Amaral T, De Angelis K, Sartori M, Athanazio R, Sampaio LM, Dal Corso S. Abnormal heart rate variability in patients with bronchiectasis 5.2. Monitoring Airway Dis. 2015;46(suppl 59):PA1042. https://doi.org/10.1183/13993003.congress-2015.PA1042.
Ramsay JA, Blimkie CJ, Smith K, Garner S, MacDougall JD, Sale DG. Strength training effects in prepubescent boys. Med Sci Sports Exerc. 1990;22(5):605–14. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/2233199.
Reid WD, Samrai B. Respiratory muscle training for patients with chronic obstructive pulmonary disease. Phys Ther. 1995;75(11):996–1005.
Resqueti V, Florêncio R, Brilhante S, Lima I, Lavezzo F, Fregonezi G. Heart rate variability response to submaximal exercise in children with cystic fibrosis. Euro Resp J. 2012;40:P1547. https://doi.org/10.31525/ct1-nct04293926 .
del Paso GA, Langewitz W, Mulder LJM, van Roon A, Duschek S. The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: a review with emphasis on a reanalysis of previous studies. Psychophysiology. 2013;50(5):477–87. https://doi.org/10.1111/psyp.12027.
Rodrigues F, Araujo AA, Mostarda CT, Ferreira J, de Barros Silva MC, Nascimento AM, Rodrigues B. Autonomic changes in young smokers: acute effects of inspiratory exercise. Clin Auton Res. 2013;23(4):201–7. https://doi.org/10.1007/s10286-013-0202-1.
Rossman MJ, Nader S, Berry D, Orsini F, Klansky A, Haverkamp HC. Effects of altered airway function on exercise ventilation in asthmatic adults. Med Sci Sports Exerc. 2014;46(6):1104–13. https://doi.org/10.1249/MSS.0000000000000206.
Sammito S, Bocklemann I. Factors influencing heart rate variability. ICF J. 2016;6:18–22. https://doi.org/10.17987/icfj.v6i0.242.
Santana-Sosa E, Gonzalez-Saiz L, Groeneveld IF, Villa-Asensi JR, de Aguero MI, Fleck SJ, Lucia A. Benefits of combining inspiratory muscle with “whole muscle” training in children with cystic fibrosis: a randomised controlled trial. Br J Sports Med. 2014;48(20):1513–7. https://doi.org/10.1136/bjsports-2012-091892.
Sawyer EH, Clanton TL. Improved pulmonary function and exercise tolerance with inspiratory muscle conditioning in children with cystic fibrosis. Chest. 1993;104(5):1490–7.
Schneiderman-Walker J, Pollock SL, Corey M, Wilkes DD, Canny GJ, Pedder L, Reisman JJ. A randomized controlled trial of a 3-year home exercise program in cystic fibrosis. J Pediatri. 2000;136(3):304–10. https://doi.org/10.1067/mpd.2000.103408.
Seifert G, Calaminus G, Wiener A, Cysarz D. Heart rate variability reflects the natural history of physiological development in healthy children and is not associated with quality of life. PLoS ONE. 2014;9(3):e91036. https://doi.org/10.1371/journal.pone.0091036.
Shei RJ, Dekerlegand RL, Mackintosh KA, Lowman JD, McNarry MA. Inspiration for the future: the role of inspiratory muscle training in cystic fibrosis. Sports Med - Open. 2019;5(1):36. https://doi.org/10.1186/s40798-019-0210-3.
Silva IS, Fregonezi GA, Dias FAL, Ribeiro CT, Guerra RO, Ferreira GM. Inspiratory muscle training for asthma. Cochrane Database Sys Rev. 2013. https://doi.org/10.1002/14651858.CD003792.pub2.
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93(5):1043–65.
Vanderlei LCM, Pastre CM, Hoshi RA, Carvalho TD, Godoy MF. Basic notions of heart rate variability and its clinical applicability. Rev Bras Cirurgia Cardiovas. 2009;24(2):205–17. https://doi.org/10.1590/s0102-76382009000200018.
World Health Organisation. Waist circumference and waist-Hip ratio: Report of a WHO expert consultation. World Health Organisation. 2008;1–47.
Wilson LC, Peebles KC, Hoye NA, Manning P, Sheat C, Williams MJA, Baldi JC. Resting heart rate variability and exercise capacity in Type 1 diabetes. Physiolo Rep. 2017. https://doi.org/10.14814/PHY2.13248.
Witt JD, Guenette JA, Rupert JL, McKenzie DC, Sheel AW. Inspiratory muscle training attenuates the human respiratory muscle metaboreflex. J Physiol. 2007;584(3):1019–28. https://doi.org/10.1113/jphysiol.2007.140855.
Yasuma F, Jun-ichiro H. Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm. Chest. 2004;125(2):683–90.
Zouhal H, Jacob C, Delamarche P, Gratas-Delamarche A. Catecholamines and the effects of exercise. Training Gender Sports Med. 2008;38(5):401–23. https://doi.org/10.2165/00007256-200838050-00004.
Acknowledgements
Special thanks to Laura Morris and Nicholas Wade for running the intervention.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MAM and KAM conceived and designed the study. JLM collected, analysed and interpreted the data along with MAM and KAM. All authors contributed to manuscript preparation, read and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any conflict of interest to disclose.
Consent to Participate
Written informed assent and consent was obtained from participants and their parent/guardian, respectively.
Consent to Publication
Publication has been approved by all authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCreery, J.L., Mackintosh, K.A. & McNarry, M.A. Effects of Inspiratory Muscle Training on Heart Rate Variability in Children with Cystic Fibrosis: A Pilot Study. J. of SCI. IN SPORT AND EXERCISE 3, 66–74 (2021). https://doi.org/10.1007/s42978-020-00079-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42978-020-00079-w