Abstract
Purpose
Non-operative treatment (NOT) for pediatric acute appendicitis complicated with intra-abdominal abscess (IAA) has been introduced in the last decade. The study aimed to report our experience with this approach and investigate potential predictors of success.
Methods
Medical records of patients affected by appendicitis complicated with IAA between January 2013 and December 2020 were reviewed. The interval before delayed appendectomy, rate of re-admission before delayed appendectomy and the rate of delayed appendectomy were the endpoints of NOT. The outcomes were compared between patients treated by NOT and patients who underwent urgent surgery for complicated appendicitis.
Results
In the study period, twenty-six patients (37%) underwent NOT, and 45 (63%) underwent urgent surgery for complicated appendicitis with IAA. A delayed appendectomy was performed in 24 children (92%). The median time before surgery was 32 days (IQR 20–58 days). Eight children (31%) were re-admitted before delayed appendectomy, and three cases presented a disease relapse. An appendicolith was detected in two of them.
Even though the overall hospital stay was longer for NOT (p = 0.0009), all these patients underwent laparoscopic appendectomy, and no conversions were reported (p = 0.0001; p = 0.0006). In addition, no difference in the rate of post-operative complications was found between the two groups (p = 0.62).
Conclusions
NOT presented a high rate of success. The presence of appendicolith at diagnosis might be considered a negative predictor of success. NOT might increase the success of mini-invasive surgery when compared to urgent surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complicated acute appendicitis might present with intra-abdominal abscess (IAA). This variant affects less than 10% of children with acute appendicitis [1]. The management of this entity is still controversial in the pediatric population. Indeed, a non-operative treatment (NOT) has been proposed in the last decade. A recent meta-analysis by Fugazzola proved that this approach resulted in better outcomes in terms of rate of complications when compared with urgent appendectomy [2]. On the other hand, NOT increases the length of hospital stay and the costs for healthcare systems [3].
Nevertheless, several issues about NOT are still debated. These issues included patient selection, the investigation of factors that predict the efficacy of this approach, the need for elective appendectomy and the timing for the intervention after the recovery from the acute infection.
For these reasons, the aim of this work is to describe our initial experience with NOT for appendicular abscess, focusing on the length of the interval before elective appendectomy and the histological findings. Secondary aims included investigating possible predicting factors and comparing the outcomes with urgent operative treatment (OT), including the overall length of hospital stay and the rate of complications.
Methods
Study design
This retrospective observational study was performed in a University Hospital, a tertiary care hospital for a regional and extra-regional population. The IRB was notified with no need for formal approval according to our Institution’s policy. For this reason, no report number was assigned. All the legal guardians gave their written consent to collect the data.
The paper was written following STROBE checklist.
Population and inclusion criteria
All children up to 18 years old treated for acute appendicitis at our hospital between January 2013 and September 2020 were included. The clinical records were reviewed to identify the patients affected by acute appendicitis complicated by IAA.
For the study purpose, patients affected by IAA were divided into two groups according to the treatment. Group 1 included all the patients affected by IAA and initially undergone NOT. Group 2 included all the patients affected by IAA and undergone urgent OT. The choice for urgent OT was based on patient’s clinical conditions, such as ill-appearance and disseminated abdominal tenderness, which were suspicious for appendicular peritonitis, regardless the size of the IAA. Moreover, the final decision was taken after a clinical assessment performed by the on-call Senior Surgeon.
The diagnosis of acute appendicitis complicated by IAA was suspected in case of appendicular mass at clinical evaluation. The diagnosis was confirmed by ultrasonography (US) in case of NOT or intraoperative findings in case of urgent OT.
NOT for IAA
Our current bundle for acute appendicitis complicated by IAA, which was reviewed in 2016, recommends NOT for well-appearing children without clinical signs of peritonitis, regardless the size of the IAA. US findings should confirm the diagnosis. Intravenous antibiotic therapy with ceftriaxone (100 mg/kg once a day) and metronidazole (22.5 mg/kg three times a day) are administrated for 7–10 days, followed by oral administration of amoxicillin-clavulanate (50 mg/kg in three times a day) for 5–7 days.
A delayed appendectomy is proposed for every patient after 4–6 weeks. One week before the date expected for the intervention, a clinical evaluation was performed to assess the full recovery and to exclude ongoing infectious process. The patients undergoing delayed appendectomy received intravenous antibiotic prophylaxis with cefazoline (75 mg/kg three times a day) and metronidazole (22.5 mg/kg three times a day) for 24 h. The children are usually discharged on the second post-operative day.
Variables and endpoints
The medical record review yielded all the general information about the clinical history of the included patients.
The following variables were reported to describe our experience with the NOT approach: time between recovery and delayed appendectomy, rate of re-admission to Emergency Department before delayed appendectomy, rate of delayed appendectomy and the histological findings of the surgical specimens. Hematoxylin and eosin-stained slides were analyzed by a Senior Pathologist blinded to clinical data. The presence of inflammation and the type of phlogistic infiltrate, acute or chronic, were ruled out.
The appendicolith was considered a potential predicting factor, and its presence was searched in the US or CT scan reports.
The following endpoints were compared between the two groups: overall length of hospital stay, the surgical technique for the appendectomy, length of surgery, rate of conversion to open surgery, and rate of post-operative complications (grade II or above, according to Clavien-Dindo classification) [4].
Statistics
The statistical analysis results were provided by IBM® SPSS Inc. Version 26.0.
Quantitative variables were reported as median value and inter-quartile range (IQR). Qualitative variables were reported as absolute and relative frequency.
Mann–Whitney U tests and Fisher’s exact tests were used to compare quantitative and qualitative variables, respectively.
p value ≤ 0.05 was considered statistically significant.
Results
Study population
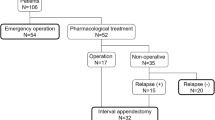
In the study period, 553 children affected by acute appendicitis were treated at our hospital. Of them, 71 cases (13%) were complicated acute appendicitis with IAA. Twenty-six patients (37%) underwent NOT (Group 1), while the other 45 (63%) underwent urgent OT (Group 2).
The choice of NOT increased in the last years, as shown in Fig. 1.
The characteristics of the two groups are reported in Table 1. No difference was found.
NOT outcomes
The median length of intravenous antibiotic therapy was 8 days (IQR 6–11 days). In 25 children (96%), intravenous therapy was followed by oral antibiotics at discharge. Percutaneous drainage of the IAA was required only in one case (3.8%).
A delayed appendectomy was not performed only in two children (7.7%). In both cases parents refused the intervention.
The median length of the interval before surgery was 32 days (IQR 20–58 days). Eight children (31%) were admitted to the emergency department for abdominal pain during this period. In three cases, an urgent appendectomy was performed due to the relapse of the infectious process. It is relevant to point out that in two of them, an appendicolith was detected at the initial US scan.
The median hospital stay after delayed appendectomy was two days (IQR 2–5.3 days). Post-operative complications graded more than II according to Clavien Dindo classification were reported in two cases (8.3%). Both cases presented a residual abdominal collection requiring a second surgical look performed through a laparoscopic approach after five days in the first case and 15 days in the other.
In our series, NOT was successful in managing appendicular abscesses in 23 children out of 26 (88%).
As to the surgical specimens, all of them presented with inflammatory infiltrate. In fifteen cases (63%), the infiltrate consisted of acute inflammatory cells. Nevertheless, the interval length before surgery did not impact the type of infiltrate (p = 0.49).
Comparison between group 1 and group 2
The comparison of the outcomes between the two Groups is reported in Table 2. The overall hospital stay was longer in Group 1 (p = 0.0009). However, all the patients belonging to the Group 1 underwent laparoscopic appendectomy and no conversions to open surgery were reported (p = 0.0001; p = 0.0006). Furthermore, the patients in the Group 1 presented a shorter duration of laparoscopic appendectomy (p = 0.01). Six adverse events (13%) graded more than Clavien Dindo II were reported in Group 2: three of them surgical site infections, one post-operative collection, one pleural effusion and one intestinal obstruction. Nevertheless, no difference in the rate of post-operative complications was found between the two Groups (p = 0.62).
Discussion
NOT for complicated acute appendicitis with IAA presented a high rate of success in children. An appendicolith was present in most of the cases that failed NOT. A delayed appendectomy was performed on most of the population. Histological examination found an acute inflammatory infiltrate in more than 60% after a median interval of 32 days. Despite the longer overall hospital stay, NOT made the laparoscopic approach safe and feasible in all the cases, without any conversion to open surgery. Finally, NOT presented a similar rate of post-operative complications compared to OT.
NOT was successful in more than 80% of the cases. This rate was consistent with the data found in other series, including randomized controlled trials [5, 6]. It is relevant to underline that all the patients belonging to our cohorts were diagnosed with IAA. Indeed, only in this case NOT did not increase the risk of adverse events [7].
Nonetheless, the success of NOT for appendicular abscess might be implemented by carefully selecting the patients. It might be speculated that the presence of an appendicolith might represent a contraindication for this approach, probably leading to the creation of a sanctuary for bacterial overgrowth and antibiotic resistance. Maita et al. [8] and Kessler et al. [9] found a higher failure rate and readmission rate after conservative management of uncomplicated acute appendicitis with a fecalith. An appendicolith was found at diagnosis in most patients who failed NOT in our series. This might be an innovative predictive factor that should be considered in the choice of the approach for the treatment of IAA. However, this interesting result was only preliminary because of our limited population. Only studies with larger samples focusing on the presence of the appendicolith might confirm the issue.
Moreover, it could be relevant to report that a recent study found that mucosal ulceration detected by US could predict the failure of conservative management for uncomplicated acute appendicitis [10]. Nevertheless, mucosal ulceration might be extremely frequent in acute appendicitis complicated by IAA, and this parameter might not be useful for this selected population.
Currently, delayed appendectomy should be recommended because of the high risk of recurrences and the lack of long-term follow-up. Indeed, a prospective study that followed-up children conservatively treated reported that 12% of the patients developed recurrent appendicitis within 12 months [11]. This rate was more than 30% in other series [12]. Histological findings also supported the recommendation for the delayed appendectomy. Several works reported the presence of inflammatory infiltrates in most cases, even if the appendix did not present any macroscopic lesion [13]. Nonetheless, the evolution of these findings is not known. Furthermore, even though the epidemiology might be different, it is relevant to outline that a trial in the adult population that compared follow-up versus delayed appendectomy was interrupted because of a high occurrence of neoplasms among the participants [14].
In our series, more than half of the patients presented acute inflammatory infiltration of the appendix after surgery. Nevertheless, this rate decreased after waiting for a longer interval before surgery [15]. Recently, Farr et al. found that acute inflammation was associated with longer operative time for delayed appendectomy, reducing the potential benefits of NOT. Most importantly, this work reported a reduced risk of acute inflammation after waiting 12 weeks before surgery. For these reasons, the Authors recommended a 12-week interval before delayed appendectomy [16].
These findings were in contrast with the shorter interval decided for our NOT bundle. The choice was made to avoid early readmission or parental anxiety. Even though no peculiar intraoperative findings were reported during delayed appendectomy in our population, the two post-operative adverse events in the Group 2 might have been explained by some residual inflammation after this shorter interval. For this reason, our policy has been changed according to the current evidence and the interval has been prolonged to twelve weeks.
This work highlighted that conservative management allowed the feasibility of mini-invasive surgery (MIS) in the whole cohort and reduced operative times. A recent meta-analysis reported a shorter hospital stay and a lower risk of adverse events, including surgical site infections, after MIS. Moreover, the laparoscopic approach fastened the time for oral intake and decreased the need for analgesics [17]. For this reason, this might be another advantage of NOT.
Even though Fugazzola et al. reported a lower complication rate after NOT [2], our series did not identify any difference. This aspect might be related to the setting of the study, conducted in a tertiary-care hospital where a senior surgeon was always present in the operative room. Nevertheless, the patients in the Group 2 were affected by more severe adverse events.
NOT presented an overall longer length of hospital stay in our series, which might increase the costs for family and health systems [3]. The overall hospital stay might be reduced by implementing enhanced recovery after surgery (ERAS) for delayed appendectomy [18]. Indeed, same-day discharge after surgery for uncomplicated acute appendicitis has been already proposed with success [19].
This study presents some limitations, mainly due to the retrospective design. First, the size of the study population was limited, and this might not allow a clear identification of predicting factors for the outcome of NOT. Second, in the first period of the study, the approach to IAA lacked standardization, and the choice of the approach relied on the senior surgeon’s experience and the availability of radiologists with experience in pediatric ultrasonography. This might have represented a main selection bias. Furthermore, the clinical presentation of the patients in the Group 2 might have been worse, leading the surgeon towards an urgent intervention. For this reason, this aspect might have also in part undermined the comparison of the outcomes between the groups. Third, our hospital is a teaching center, and this aspect might have justified the higher number rate of open surgery in Group 2. Another potential recall bias concerned the lack of radiological findings in the medical records. Finally, the histological examination lacked a standard score, which might have led to an interpretation bias.
To conclude, NOT for acute appendicitis complicated by IAA presented a high success rate. The presence of an appendicolith at diagnosis might be considered a negative predictive factor for the success of NOT. Nevertheless, this result required further studies for confirmation. NOT might ease the feasibility of MIS with the related benefits for patients. Delayed appendectomy should always be recommended after a 12-week interval to reduce the risk of acute residual inflammation.
Data availability
The data that support the findings of this study are available on reasonable request from the corresponding author.
References
Humes DJ, Simpson J (2006) Acute appendicitis. BMJ 333:530–534
Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L (2019) Early appendectomy vs. conservative management in complicated acute appendicitis in children: a meta-analysis. J Pediatr Surg 54:2234–2241
Watanabe R, Otsuji A, Nakamura Y et al (2020) Superior outcomes (but at higher costs) of non-operative management with interval appendectomy over immediate surgery in appendicitis with abscess: results from a large adult population cohort. Asian J Endosc Surg 13:186–194
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:2015–2113
Tanaka Y, Uchida H, Kawashima H et al (2016) More than one-third of successfully nonoperatively treated patients with complicated appendicitis experienced recurrent appendicitis: is interval appendectomy necessary? J Pediatr Surg 51:1957–1961
St Peter SD, Aguayo P, Fraser JD et al (2010) Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg 45:236–240
Duggan EM, Marshall AP, Weaver KL et al (2016) A systematic review and individual patient data meta-analysis of published randomized clinical trials comparing early versus interval appendectomy for children with perforated appendicitis. Pediatr Surg Int 32:649–655
Kessler U, Mosbahi S, Walker B et al (2017) Conservative treatment versus surgery for uncomplicated appendicitis in children: a systematic review and meta-analysis. Arch Dis Child 102:1118–1124
Maita S, Andersson B, Svensson JF, Wester T (2020) Nonoperative treatment for nonperfoated appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int 36:261–269
Levy S, Hiller N, Lev-Cohain N, Goldberg SN, Mizrahi I, Simanovsky N (2022) Ultrasonographic features can predict outcome of conservative management of acute appendicitis in children. Emerg Radiol 29:59–65. https://doi.org/10.1007/s10140-021-01984-5
Hall NJ, Eaton S, Stanton MP, CHINA Study Collaborators and the paediatric Surgery Trainees Research Network et al (2017) Active observation versus interval appendicectomy after successful non-operative treatment of an appendix mass in children (CHINA study): an open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 2:253–260
Tanaka Y, Uchido H, Kawashima H et al (2016) More than one-third of successfully nonoperatively treated patients with complicated appendicitis experienced recurrent appendicitis: is interval appendectomy necessary? J Pediatr Surg 51:1957–1961
Fouad D, Kauffman JD, Chandler NM (2020) Pathology findings following interval appendectomy: should it stay or go? J Pediatr Surg 55:737–741
Mällinen J, Rautio T, Grönroos J et al (2019) Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized controlled trial. JAMA Surg 154:200–207
Pederiva F, Bussani R, Shafiei V, Codrich D, Guida E, SchleeF J (2021) The histopathology of the appendix in children at interval appendectomy. Children (Basel) 8:811
Farr BJ, Carey DE, Mooney DP (2021) When to take it out? Optimal timing of interval appendectomy in 500 consecutive children. J Pediatr Surg 56:1822–1825
Neogi S, Banerjee A, Panda SS, Ratan SK, Narang R (2022) Laparoscopic versus open appendicectomy for complicated appendicitis in children: a systematic review and meta-analysis. J Pediatr Surg 57:394–405. https://doi.org/10.1016/j.jpedsurg.2021.07.005
Gao R, Yang H, Li Y et al (2019) Enhanced recovery after surgery in pediatric gastrointestinal surgery. J Int Med Res 47:4815–4826
Gee KM, Ngo S, Burkhalter L, Beres AL (2021) Same-day discharge vs. observation after laparoscopic pediatric appendectomy: a prospective cohort study. Transl Gastroenterol Hepatol 6:45. https://doi.org/10.21037/tgh-20-39
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement. The authors declare the study received no funding.
Author information
Authors and Affiliations
Contributions
Study conception and design: FG, PG and EG; data collection: FG and EG; analysis and interpretation FG, EG, CV and DD; draft manuscript preparation FG, DD, CV, FDC, CT, MZ and PG. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethics approval
This is a retrospective study. The IRB was notified with no need for formal approval according to our Institution’s policy. For this reason, no report number was assigned.
Informed consent
All the legal guardians gave their written consent to collect the data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghidini, F., Donà, D., Giacomini, E. et al. Benefit for non-operative treatment of pediatric appendicitis with intra-abdominal abscess. A single-center report. J Ped Endosc Surg 5, 73–78 (2023). https://doi.org/10.1007/s42804-023-00177-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-023-00177-w