Abstract
In vivo, vascular endothelial growth factor (VEGF) and vascular endothelial cadherin (VE-cadherin) co-regulate the dynamic organization of endothelial cells during vascular sprouting, balancing angiogenesis and vascular stability. In this study, a novel bioactive surface integrating human VE-cadherin-Fc and VEGF-Fc fusion proteins was innovatively developed for the modification of poly(ε-caprolactone) (PCL) small-caliber electrospun fibrous grafts (VE-cad/VEGF-PCL) to promote the regeneration of functional endothelium and improve the patency of artificial vascular grafts. These fusion proteins self-assembled on the PCL fibers through the hydrophobic binding of Fc domains, improving surface hydrophilicity while reducing the adhesion of fibrinogen. In vitro results showed that the VE-cadherin/VEGF surface upregulated the expression of endogenous VE-cadherin and synergistically activated the VE-cadherin/VEGFR2/FAK/AKT/ERK signal transduction, which facilitated the functioning of human umbilical vein endothelial cells (HUVECs). Moreover, the VE-cadherin/VEGF surface significantly enhanced cellularization and capillary formation, then subsequently accelerated the regeneration of functional endothelium and smooth muscle in the VE-cad/VEGF-PCL grafts in a rat abdominal aorta replacement model. Together, these results highlight the advantages of VE-cadherin/VEGF surface in enhancing rapid endothelialization of electrospun vascular grafts and provide new insights into the design of cross-activating biomaterials.
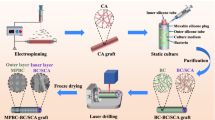
Graphical Abstract










Similar content being viewed by others
References
Collaborators GBDS. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021;20:795.
Asakura T, Tanaka T, Tanaka R. Advanced silk fibroin biomaterials and application to small-diameter silk vascular grafts. ACS Biomater Sci Eng 2019;5:5561.
Obiweluozor FO, Emechebe GA, Kim DW, Cho HJ, Park CH, Kim CS, Jeong IS. Considerations in the development of small-diameter vascular graft as an alternative for bypass and reconstructive surgeries: a review. Cardiovasc Eng Technol 2020;11:495.
Du F, Wang H, Zhao W, Li D, Kong D, Yang J, Zhang Y. Gradient nanofibrous chitosan/poly varepsilon-caprolactone scaffolds as extracellular microenvironments for vascular tissue engineering. Biomaterials 2012;33:762.
Lotfi M, Bagherzadeh R, Naderi-Meshkin H, Mahdipour E, Mafinezhad A, Sadeghnia HR, Esmaily H, Maleki M, Hasssanzadeh H, Ghayaour-Mobarhan M, Bidkhori HR, Bahrami AR. Hybrid chitosan-ss-glycerol phosphate-gelatin nano-/micro fibrous scaffolds with suitable mechanical and biological properties for tissue engineering. Biopolymers 2016;105:163.
Zhang Y, Liu Y, Jiang Z, Wang J, Zhao H. Poly(glyceryl sebacate)/silk fibroin small-diameter artificial blood vessels with good elasticity and compliance. Smart Mater Med 2021;2:74.
Kirillova A, Yeazel TR, Asheghali D, Petersen SR, Dort S, Gall K, Becker ML. Fabrication of biomedical scaffolds using biodegradable polymers. Chem Rev 2021;121:11238.
Wang D, Xu Y, Li Q, Turng LS. Artificial small-diameter blood vessels: materials, fabrication, surface modification, mechanical properties, and bioactive functionalities. J Mater Chem B 1801;2020:8.
Ardila DC, Liou JJ, Maestas D, Slepian MJ, Badowski M, Wagner WR, Harris D, Vande Geest JP. Surface modification of electrospun scaffolds for endothelialization of tissue-engineered vascular grafts using human cord blood-derived endothelial cells. J Clin Med 2019;8:185.
Apte RS, Chen DS, Ferrara N. VEGF in signaling and disease: beyond discovery and development. Cell 2019;176:1248.
Trojanowska M. Cellular and molecular aspects of vascular dysfunction in systemic sclerosis[J]. Nat Rev Rheumatol 2010;6:453.
Melincovici CS, Bosca AB, Susman S, Marginean M, Mihu C, Istrate M, Moldovan IM, Roman AL, Mihu CM. Vascular endothelial growth factor (VEGF)—key factor in normal and pathological angiogenesis. Rom J Morphol Embryol 2018;59:455.
Duong CN, Vestweber D. Mechanisms ensuring endothelial junction integrity beyond VE-cadherin. Front Physiol 2020;11:519.
Grimsley-Myers CM, Isaacson RH, Cadwell CM, Campos J, Hernandes MS, Myers KR, Seo T, Giang W, Griendling KK, Kowalczyk AP. VE-cadherin endocytosis controls vascular integrity and patterning during development. J Cell Biol 2020;219:e201909081.
Campinho P, Vilfan A, Vermot J. Blood flow forces in shaping the vascular system: a focus on endothelial cell behavior. Front Physiol 2020;11:552.
Xu K, Shuai Q, Li X, Zhang Y, Gao C, Cao L, Hu F, Akaike T, Wang JX, Gu Z, Yang J. Human VE-cadherin fusion protein as an artificial extracellular matrix enhancing the proliferation and differentiation functions of endothelial cell. Biomacromol 2016;17:756.
Xie J, Li X, Zhang Y, Tang T, Chen G, Mao H, Gu Z, Yang J. VE-cadherin-based matrix promoting the self-reconstruction of pro-vascularization microenvironments and endothelial differentiation of human mesenchymal stem cells. J Mater Chem B 2021;9:3357.
Esser S, Lampugnani MG, Corada M, Dejana E, Risau W. Vascular endothelial growth factor induces VE-cadherin tyrosine phosphorylation in endothelial cells. J Cell Sci 1998;111(Pt 13):1853.
Gavard J, Gutkind JS. VEGF controls endothelial-cell permeability by promoting the beta-arrestin-dependent endocytosis of VE-cadherin. Nat Cell Biol 2006;8:1223.
Sowmya B, Hemavathi AB, Panda PK. Poly (epsilon-caprolactone)-based electrospun nano-featured substrate for tissue engineering applications: a review. Prog Biomater 2021;10:91.
Xu K, Zhu C, Xie J, Li X, Zhang Y, Yao F, Gu Z, Yang J. Enhanced vascularization of PCL porous scaffolds through VEGF-Fc modification. J Mater Chem B 2018;6:4474.
Yu M, Du F, Ise H, Zhao W, Zhang Y, Yu Y, Yao F, Yang J, Akaike T. Preparation and characterization of a VEGF-Fc fusion protein matrix for enhancing HUVEC growth. Biotechnol Lett 2012;34:1765.
Wang K, Zhang Q, Zhao L, Pan Y, Wang T, Zhi D, Ma S, Zhang P, Zhao T, Zhang S, Li W, Zhu M, Zhu Y, Zhang J, Qiao M, Kong D. Functional Modification of electrospun poly(epsilon-caprolactone) vascular grafts with the fusion protein VEGF-HGFI enhanced vascular regeneration. ACS Appl Mater Interfaces 2017;9:11415.
Gao C, Zhang Y, Xie J, Wang X, Yang J. VE-cadherin functionalized injectable PAMAM/HA hydrogel promotes endothelial differentiation of hMSCs and vascularization. Appl Mater Today 2020;20:100690.
Zhi D, Cheng Q, Midgley AC, Zhang Q, Wei T, Li Y, Wang T, Ma T, Rafique M, Xia S, Cao Y, Li Y, Li J, Che Y, Zhu M, Wang K, Kong D. Mechanically reinforced biotubes for arterial replacement and arteriovenous grafting inspired by architectural engineering. Sci Adv 2022;8:eabl3888.
Houck KA, Ferrara N, Winer J, Cachianes G, Li B, Leung DW. The vascular endothelial growth factor family: identification of a fourth molecular species and characterization of alternative splicing of RNA. Mol Endocrinol 1806;1991:5.
Nakatsu MN, Sainson RC, Perez-del-Pulgar S, Aoto JN, Aitkenhead M, Taylor KL, Carpenter PM, Hughes CC. VEGF(121) and VEGF(165) regulate blood vessel diameter through vascular endothelial growth factor receptor 2 in an in vitro angiogenesis model. Lab Invest 1873;2003:83.
Kaushik K, Das A. Endothelial progenitor cell therapy for chronic wound tissue regeneration. Cytotherapy 2019;21:1137.
Bai Y, Bai L, Zhou J, Chen H, Zhang L. Sequential delivery of VEGF, FGF-2 and PDGF from the polymeric system enhance HUVECs angiogenesis in vitro and CAM angiogenesis. Cell Immunol 2018;323:19.
Koepsel JT, Loveland SG, Schwartz MP, Zorn S, Belair DG, Le NN, Murphy WL. A chemically-defined screening platform reveals behavioral similarities between primary human mesenchymal stem cells and endothelial cells. Integr Biol (Camb) 2012;4:1508.
Rajendran S, Shen X, Glawe J, Kolluru GK, Kevil CG. Nitric oxide and hydrogen sulfide regulation of ischemic vascular growth and remodeling. Compr Physiol 2019;9:1213.
Yang L, Zhang Y, Ma Y, Du J, Gu L, Zheng L, Zhang X. Effect of melatonin on EGF- and VEGF-induced monolayer permeability of HUVECs. Am J Physiol Heart Circ Physiol 2019;316:H1178.
Franklin-Murray AL, Mallya S, Jankeel A, Sureshchandra S, Messaoudi I, Lodoen MB. Toxoplasma gondii dysregulates barrier function and mechanotransduction signaling in human endothelial cells. mSphere 2020;5:e00550-19.
Choi HJ, Zhang H, Park H, Choi KS, Lee HW, Agrawal V, Kim YM, Kwon YG. Yes-associated protein regulates endothelial cell contact-mediated expression of angiopoietin-2. Nat Commun 2015;6:6943.
Lampugnani MG, Dejana E, Giampietro C. Vascular endothelial (VE)-cadherin, endothelial adherens junctions, and vascular disease. Cold Spring Harb Perspect Biol 2018;10:a029322.
Duong CN, Bruckner R, Schmitt M, Nottebaum AF, Braun LJ, Meyer Zu BM, Ipe U, Vom BH, Scholer HR, Trapani G, Trappmann B, Ebrahimkutty MP, Huveneers S, de Rooij J, Ishiyama N, Ikura M, Vestweber D. Force-induced changes of alpha-catenin conformation stabilize vascular junctions independently of vinculin. J Cell Sci 2021;134:jcs259012.
Pulous FE, Grimsley-Myers CM, Kansal S, Kowalczyk AP, Petrich BG. Talin-dependent integrin activation regulates VE-cadherin localization and endothelial cell barrier function. Circ Res 2019;124:891.
Zhang Y, Liu J, Zou T, Qi Y, Yi B, Dissanayaka WL, Zhang C. DPSCs treated by TGF-beta1 regulate angiogenic sprouting of three-dimensionally co-cultured HUVECs and DPSCs through VEGF-Ang-Tie2 signaling. Stem Cell Res Ther 2021;12:281.
Calera MR, Venkatakrishnan A, Kazlauskas A. VE-cadherin increases the half-life of VEGF receptor 2. Exp Cell Res 2004;300:248.
Grazia Lampugnani M, Zanetti A, Corada M, Takahashi T, Balconi G, Breviario F, Orsenigo F, Cattelino A, Kemler R, Daniel TO, Dejana E. Contact inhibition of VEGF-induced proliferation requires vascular endothelial cadherin, beta-catenin, and the phosphatase DEP-1/CD148. J Cell Biol 2003;161:793.
Azuma K, Nagaoka M, Cho CS, Akaike T. An artificial extracellular matrix created by hepatocyte growth factor fused to IgG-Fc. Biomaterials 2010;31:802.
Xu J, Li S, Hu F, Zhu C, Zhang Y, Zhao W, Akaike T, Yang J. Artificial biomimicking matrix modifications of nanofibrous scaffolds by hE-cadherin-Fc fusion protein to promote human mesenchymal stem cells adhesion and proliferation. J Nanosci Nanotechnol 2014;14:4007.
Zhang Y, Mao H, Gao C, Li S, Shuai Q, Xu J, Xu K, Cao L, Lang R, Gu Z, Akaike T, Yang J. Enhanced biological functions of human mesenchymal stem-cell aggregates incorporating E-cadherin-modified PLGA microparticles. Adv Healthc Mater 1949;2016:5.
Folkman J. Fundamental concepts of the angiogenic process. Curr Mol Med 2003;3:643.
Mohan C, Sreerekha PR, Divyarani VV, Nair S, Chennazhi K, Menon D. Influence of titania nanotopography on human vascular cell functionality and its proliferation in vitro. J Mater Chem 2012;22:1326.
Zhuang Y, Zhang C, Cheng M, Huang J, Liu Q, Yuan G, Lin K, Yu H. Challenges and strategies for in situ endothelialization and long-term lumen patency of vascular grafts. Bioact Mater 2021;6:1791.
Brash JL. Exploiting the current paradigm of blood-material interactions for the rational design of blood-compatible materials. J Biomater Sci Polym Ed 2000;11:1135.
Zhao L, Ma S, Pan Y, Zhang Q, Wang K, Song D, Wang X, Feng G, Liu R, Xu H, Zhang J, Qiao M, Kong D. Functional modification of fibrous PCL scaffolds with fusion protein VEGF-HGFI enhanced cellularization and vascularization. Adv Healthc Mater 2016;5:2376.
Gao X, Kouklis P, Xu N, Minshall RD, Sandoval R, Vogel SM, Malik AB. Reversibility of increased microvessel permeability in response to VE-cadherin disassembly. Am J Physiol Lung Cell Mol Physiol 2000;279:L1218.
Pennel T, Bezuidenhout D, Koehne J, Davies NH, Zilla P. Transmural capillary ingrowth is essential for confluent vascular graft healing. Acta Biomater 2018;65:237.
Gupta P, Mandal BB. Tissue-ngineered vascular grafts: emerging trends and technologies. Adv Funct Mater 2021;31:2100027.
Peng X, Wang X, Cheng C, Zhou X, Gu Z, Li L, Liu J, Yu X. Bioinspired, artificial, small-diameter vascular grafts with selective and rapid endothelialization based on an amniotic membrane-derived hydrogel. ACS Biomater Sci Eng 2020;6:1603.
Lyu N, Du Z, Qiu H, Gao P, Yao Q, Xiong K, Tu Q, Li X, Chen B, Wang M, Pan G, Huang N, Yang Z. Mimicking the nitric oxide-releasing and glycocalyx functions of endothelium on vascular stent surfaces. Adv Sci (Weinh) 2020;7:2002330.
Acknowledgements
The authors gratefully acknowledge financial support from the National Key R&D Program of China (2020YFA0710802), the National Natural Science Foundation of China (Grant No. 32071364, 82172106), the NCC Fund (NCC2020PY18), Tianjin “Project + Team” Key Training Foundation (XC202035), and China Postdoctoral Science Foundation (2022M711707).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
42765_2022_213_MOESM3_ESM.tif
Supplementary file3 Scratch-wound healing images of HUVECs cultured on the TC-PS, VE-cad-Fc, VEGF-Fc, and VE-cad/VEGF-Fc surfaces for 8 and 24 hours (TIF 20606 KB)
42765_2022_213_MOESM4_ESM.tif
Supplementary file4 Characterization of the VE-cadherin/VEGF interface on the PCL electrospun fibrous grafts. a Morphology of the electrospun fibrous grafts detected by SEM, b XPS spectra of electrospun fibrous grafts before and after functionalization, c Stability of hVE-cad-Fc and hVEGF-Fc proteins immobilized on the VE-cad/VEGF-PCL grafts were evaluated by ELISA (TIF 14604 KB)
42765_2022_213_MOESM5_ESM.tif
Supplementary file5 Evaluation of the cellularization and capillary formation of the VE-cadherin/VEGF functionalized PCL electrospun fibrous grafts after subcutaneous implantation. A Representative H&E staining of the explanted PCL, VE-cad-PCL, VEGF-PCL, and VE-cad/VEGF-PCL grafts, B Quantitative analysis of cellularization of explanted grafts, C The capillaries in the cellularization area were detected by immunofluorescent staining with vWF (green) antibody (arrow indicated), D Quantitative analysis of blood number in the explanted grafts, E Quantitative analysis of blood vessel density in the explanted grafts. Statistical significance was calculated by One-way ANOVA followed by Tukey’s test. The data were reported as mean ± SEM, n = 3. **Significant difference, P < 0.01; *Significant difference, P < 0.05; ns indicated no statistical differences (TIF 19782 KB)
42765_2022_213_MOESM6_ESM.tif
Supplementary file6 Color Doppler ultrasound evaluation of the PCL, VE-cad-PCL, VEGF-PCL, and VE-cad/VEGF-PCL electrospun fibrous grafts at the 4th week after implantation (TIF 946 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Xu, K., Zhi, D. et al. Improving Vascular Regeneration Performance of Electrospun Poly(ε-Caprolactone) Vascular Grafts via Synergistic Functionalization with VE-Cadherin/VEGF. Adv. Fiber Mater. 4, 1685–1702 (2022). https://doi.org/10.1007/s42765-022-00213-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42765-022-00213-z