Abstract
Continuous pulse wave signals monitoring is the essential basis for clinical cardiovascular diagnosis and treatment. Recent researches show the majority of current electronic pulse sensors usually face challenges in electrical safety concern, poor durability and demanding precision in position alignment. Thus, a highly sensitive, inherently electrical safe, robust and alignment-free device is highly desired. Here, we present a wearable alignment-free microfiber-based sensor chip (AFMSC) for precise vital signs monitoring and cardiovascular health assessment. The AFMSC comprises an optical micro/nano fiber sensor (MNF) and a flexible soft liquid sac while the MNF sensor is used to perceive the physiological signals and the liquid sac is used to eliminate the misalignment. The real-time and accurate monitoring of the pulse signals was realized by tracking the optical power variation of transmitted light from MNF. Then, the cardiovascular vital signs extracted from radial artery pulse signals were used to evaluate cardiovascular health condition and the results were in accordance with human physiological characteristics. Moreover, the pulse signals from different arterial area, the respiration signals from chest and the radial pulse signals before and after exercise were detected and analyzed. The non-invasive, continuous and accurate monitoring of cardiovascular health based on the reported wearable and alignment-free device is promising in both fitness monitoring and medical diagnostics for cardiovascular disease prevention and diagnosis.
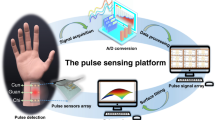
Graphical abstract







Similar content being viewed by others
References
Wei-Wei C, Run-Lin G, Li-Sheng L, Man-Lu Z, Wen W, Yong-Jun W, Zhao-Su W, Hui-Jun L, Dong-Feng G, Yue-Jin Y. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol JGC 2017;14:1.
Liu L. Cardiovascular diseases in China. Biochem Cell Biol 2007;85:157.
Allender S, Scarborough P, Peto V, Rayner M, Leal J, Luengo-Fernandez R, Gray A. European cardiovascular disease statistics. Eur Heart Netw 2008;3:11.
Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation 2016;133:1605.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982.
Yang T, Jiang X, Zhong Y, Zhao X, Lin S, Li J, Li X, Xu J, Li Z, Zhu H. A wearable and highly sensitive graphene strain sensor for precise home-based pulse wave monitoring. ACS Sens 2017;2:967.
Xu L, Meng MQ-H, Shi C, Wang K, Li N. Quantitative analyses of pulse images in Traditional Chinese Medicine. Med Acupunct. 2008;20:175.
Ram MR, Madhav KV, Krishna EH, Komalla NR, Reddy KA. A novel approach for motion artifact reduction in PPG signals based on AS-LMS adaptive filter. IEEE Trans Instrum Meas 2011;61:1445.
Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas 2007;28:R1.
Choi Y, Zhang Q, Ko S. Noninvasive cuffless blood pressure estimation using pulse transit time and Hilbert–Huang transform. Comput Electr Eng 2013;39:103.
Kim D-H, Lu N, Ma R, Kim Y-S, Kim R-H, Wang S, Wu J, Won SM, Tao H, Islam A. Epidermal electronics. Science 2011;333:838.
Windmiller JR, Bandodkar AJ, Valdés-Ramírez G, Parkhomovsky S, Martinez AG, Wang J. Electrochemical sensing based on printable temporary transfer tattoos. Chem Commun 2012;48:6794.
Zeng Z, Huang Z, Leng K, Han W, Niu H, Yu Y, Ling Q, Liu J, Wu Z, Zang J. Nonintrusive monitoring of mental fatigue status using epidermal electronic systems and machine-learning algorithms. ACS Sens 2020;5:1305.
Mannsfeld SC, Tee BC, Stoltenberg RM, Chen CVH, Barman S, Muir BV, Sokolov AN, Reese C, Bao Z. Highly sensitive flexible pressure sensors with microstructured rubber dielectric layers. Nat Mater 2010;9:859.
Jason NN, Ho MD, Cheng W. Resistive electronic skin. J Mater Chem C 2017;5:5845.
Wang X, Zhou J, Song J, Liu J, Xu N, Wang ZL. Piezoelectric field effect transistor and nanoforce sensor based on a single ZnO nanowire. Nano Lett 2006;6:2768.
Fan F-R, Lin L, Zhu G, Wu W, Zhang R, Wang ZL. Transparent triboelectric nanogenerators and self-powered pressure sensors based on micropatterned plastic films. Nano Lett 2012;12:3109.
Leitão C, Domingues MF, Novais S, Tavares C, Pinto J, Marques C, Antunes P (2018) Arterial pulses assessed with FBG based films: a smart skin approach. Biophotonics: Photonic Solutions for Better Health Care VI; 2018: International Society for Optics and Photonics
Pant S, Umesh S, Asokan S. A novel approach to acquire the arterial pulse by finger plethysmography using fiber Bragg grating sensor. IEEE Sens J 2020;20:5921.
Jia D, Chao J, Li S, Zhang H, Yan Y, Liu T, Sun Y. A fiber Bragg grating sensor for radial artery pulse waveform measurement. IEEE Trans Biomed Eng 2017;65:839.
Samartkit P, Pullteap S, Seat HC. Validation of fiber optic-based fabry-perot interferometer for simultaneous heart rate and pulse pressure measurements. IEEE Sens J 2020;21(6195):6201.
Ushakov NA, Markvart AA, Liokumovich LB. Pulse wave velocity measurement with multiplexed fiber optic Fabry–Pérot interferometric sensors. IEEE Sens J 2020;20:11302.
Guo J, Zhou B, Zong R, Pan L, Li X, Yu X, Yang C, Kong L, Dai Q. Stretchable and highly sensitive optical strain sensors for human-activity monitoring and healthcare. ACS Appl Mater Interfaces 2019;11:33589.
Guo J, Niu M, Yang C. Highly flexible and stretchable optical strain sensing for human motion detection. Optica 2017;4:1285.
Tan S, Li Y, Liu T, Yan Z, Liu D, Sun Q. A large measurement range bending sensor based on microfiber probe. IEEE Photonics Technol Lett 1964;2019:31.
Fan X, Huang Y, Ding X, Luo N, Li C, Zhao N, Chen SC. Alignment-free liquid-capsule pressure sensor for cardiovascular monitoring. Adv Func Mater 2018;28:1805045.
Yan H, Wang Y, Fufeng L, Gong A, Yun F, Hong Y, Jin X, Cheng Y, Lei H, Zhaoxia X. Relationship of optimal pulse-taking pressure among cun, guan, chi pulse of 264 healthy undergraduates. China J Trad Chin Med Pharm 2006.
Wang J, Liu K, Sun Q, Ni X, Ai F, Wang S, Yan Z, Liu D. Diaphragm-based optical fiber sensor for pulse wave monitoring and cardiovascular diseases diagnosis. J Biophotonics 2019;12:e201900084.
Song Z, Li W, Bao Y, Wang W, Liu Z, Han F, Han D, Niu L. Bioinspired microstructured pressure sensor based on a janus graphene film for monitoring vital signs and cardiovascular assessment. Adv Electron Mater 2018;4:1800252.
Fu Y, Zhao S, Wang L, Zhu R. A Wearable sensor using structured silver-particle reinforced PDMS for radial arterial pulse wave monitoring. Adv Healthc Mater 2019;8:1900633.
Meng K, Chen J, Li X, Wu Y, Fan W, Zhou Z, He Q, Wang X, Fan X, Zhang Y. Flexible weaving constructed self-powered pressure sensor enabling continuous diagnosis of cardiovascular disease and measurement of cuffless blood pressure. Adv Func Mater 2019;29:1806388.
Liu Y, Meng F, Zhou Y, Mugo SM, Zhang Q. Graphene oxide films prepared using gelatin nanofibers as wearable sensors for monitoring cardiovascular health. Adv Mater Technol 2019;4:1900540.
Sun Y, Dong Y, Gao R, Chu Y, Zhang M, Qian X, Wang X. Wearable pulse wave monitoring system based on MEMS sensors. Micromachines 2018;9:90.
Ghosh SK, Mandal D. Sustainable energy generation from piezoelectric biomaterial for noninvasive physiological signal monitoring. ACS Sustain Chem Eng 2017;5:8836.
Shao D, Liu C, Tsow F. Noncontact physiological measurement using a camera: a technical review and future directions. ACS Sens 2020;6:321–34.
Sekine T, Gaitis A, Sato J, Miyazawa K, Muraki K, Shiwaku R, Takeda Y, Matsui H, Kumaki D, Domingues-Dos-Santos F. Low operating voltage and highly pressure-sensitive printed sensor for healthcare monitoring with analogic amplifier circuit. ACS Appl Electron Mater 2019;1:246.
Yamashina A, Tomiyama H, Arai T, Hirose K-I, Koji Y, Hirayama Y, Yamamoto Y, Hori S. Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res 2003;26:615.
Acknowledgements
This work was supported by the National Science Fund of China for Excellent Young Scholars (No. 61922033), the Science Found for Creative Research Groups of the Natural Science Foundation of Hubei (No. 2018CFA004), and the Innovation Fund of WNLO.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, L., Liu, Y., Song, C. et al. Wearable Alignment-Free Microfiber-Based Sensor Chip for Precise Vital Signs Monitoring and Cardiovascular Assessment. Adv. Fiber Mater. 4, 475–486 (2022). https://doi.org/10.1007/s42765-021-00121-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42765-021-00121-8