Abstract
The overall burden of cardiovascular disease (CVD) in Sub-Saharan Africa (sSA) tends to be underestimated. Model predictions, estimating CVDs are responsible for approximately 13% of all deaths and 38% of all non-communicable disease (NCD) deaths in sSA, are based on data mainly from urban areas and primarily hospital-based clinical data. Conservative estimates report NCD account for a total of 2.6 million deaths in sSA. Additionally, upstream determinants of poor health in general such as poverty and level of education extend beyond established and reliable data-capture systems. Majority of these present challenges require multi-sectoral and inter-disciplinary strategies to effectively address. However, the limitations notwithstanding, available estimates show that countries in sSA are facing a double burden of infectious and non-communicable diseases. The infectious disease burden in sSA has previously been high; however, populations in Africa are undergoing both an epidemiological and demographic transition with increased survival from childhood to adulthood. There has also been a rise in modifiable risk factors, such as dietary and sedentary lifestyle, accounting for an increasing prevalence of cardiovascular diseases and other non-communicable diseases. This shift and a rise in cardiovascular morbidity have placed substantial strain on healthcare systems in Sub-Saharan Africa that require to be prioritized right from policy to practice. The recent COVID-19 pandemic with a disproportionately higher incidence of morbidity and mortality among patients with pre-existing risk factors for cardiovascular disease has also highlighted challenges and potential areas of improvement in the delivery of cardiovascular healthcare in Sub-Saharan Africa.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Disease burden in Sub-Saharan Africa (sSA) was previously largely attributable to infectious diseases. However, with the epidemiological and demographic transition and an increase in the prevalence of non-communicable diseases (NCDs), sSA currently faces a double burden of both infectious and non-communicable diseases such as cardiovascular diseases [1]. The leading causes of hospital admission and in-hospital deaths among adults in sSA were both cardiovascular and infectious diseases [2]. In 2020, cardiovascular diseases remained the leading cause of global disease burden [3]. Previously, the estimated number of deaths in sSA that were attributable to cardiovascular diseases (CVDs) were one million, constituting 5.5% of all global CVD-related deaths and 11.3% of all deaths in Africa; however, recent data show increasing survival with attendant co-morbidities from CVDs [3, 4]. The global incidence of CVD-mortality is increasing [5], and overall NCDs are projected to account for more than 50% of deaths in sSA by 2030 [6]. Additionally, these CVD-related deaths form 38% of all NCD-related deaths in Africa [7].
Despite these attempts in quantifying the burden of CVDs in sSA, there are still challenges that need to be addressed, some of which have been previously reviewed by Yuyun et al. [5]. Firstly, data on CVDs in low-and-middle income countries (LMICs) beyond urban centres can be very sparse [8] and in majority of cases non-existent. Secondly, rapidly advancing technologies in the spectrum of cardiovascular medicine ranging from novel diagnostics to therapeutics remain inaccessible to majority of patients living in LMIC settings in sSA. Thirdly, public health policies and systems favouring preventive and promotive health are needed. Fourthly, existing curative healthcare systems require strengthening for efficient service delivery including adequate resource allocation for specialised human resource staffing and equipping. Finally, the on-going COVID-19 pandemic is an additional challenge on already strained healthcare systems in sSA and the long-term sequelae of COVID-19 infection on the cardiovascular system remain largely unknown.
Therefore, the aim of this paper is to provide an updated overview of the challenges encountered in the management of CVDs in sSA countries. It also highlights some of the important priorities for management of CVDs in sSA countries post the COVID-19 pandemic.
Gaps
Data on Burden of Cardiovascular Disease in Africa
The burden of cardiovascular diseases in Africa remains largely under-estimated primarily due to factors such as weaker systems of data collection that are mainly centred in and around urban centres, reduced funding for research as well as shortage of skilled expertise [9]. According to the World Health Organization (WHO), 77% of all reported NCD-related deaths occur in low- and middle-income countries (LMICs), and the burden being even higher accounting for 85% of deaths preventing adults over 30 years from reaching their full life-span [10]. In a 2014 study investigating the use of linked clinical and demographic surveillance data to measure the burden of disease among adults living in coastal Kenya, we showed that there are several factors at play including distance from the hospital and gender-based health-seeking behaviour [11]. Nevertheless, there was evidence of a combined burden of infectious and non-infectious diseases including cardiovascular illnesses in this rural cohort [11]. Yuyun et al. also highlighted the challenges of incomplete epidemiological data collection on CVDs in sSA [5]. Despite these challenges, some efforts have still been made at describing the burden and types of CVDs commonly seen in sSA. Mebrahtom et al. recently reported a high prevalence of rheumatic heart disease (RHD) affecting one in seven people in East Africa with over one million children affected [12]. Approximately 500,000 children born annually in Africa have a significant congenital heart disease (CHD) requiring specialist cardiac care which is limited and largely confined to urban areas [13]. Zikarg et al. reported a pooled-prevalence of approximately 30% for cardiac septal defects among children in East Africa [14]. Majority of CHD patients in Africa die early during infancy, while the minority that survive to adolescence and adulthood have a reduced quality of life due to significant morbidity and chronic illness [13]. The international congestive heart failure study (INTER-CHF) conducted across Africa, Asia, Middle East and South America reported a high mortality rate of heart failure in Africa (34%) that was double the global average [15]. Overall, the lack of proper disease surveillance programmes and weaker health systems compromise the ascertainment of the true burden and trends of CVDs in sSA. Additionally, discrepancies in prevalence reported in the literature arise from differences in capacity to detect cases due to lack of standardised diagnostic assessment procedures and tools or requisite expertise across different countries in sSA and also between rural and urban centres within the same country [12]. Current evidence shows a higher burden of CVDs in urban areas compared to rural areas in sSA [5, 16].
Technological Advances
Technological advances and the use of artificial intelligence algorithms continue to exponentially increase in delivery of healthcare. Ranging from the incorporation of digital health innovations to more advanced diagnostic and therapeutic technologies, there is growing evidence of improved delivery of CVD care as well as patient outcomes with the use of these technologies.
In 2020, Santo and Redfern reported that short message services (SMS) were the most studied type of digital health intervention, showing positive results in improved education, medication adherence and reduction of CVD risk [17]. Over the last two decades, sSA has seen increasing use of digital technologies in healthcare systems, including mHealth and tele-medicine [18]. However, while these are generally good in improving access, they come with new challenges such as data privacy, regulation, costs and sustainability among others [19]. According to the Global System for Mobile Communications (GSMA), there are 5.3 billion people (67%) connected to mobile services globally [20]. In sSA, mobile phone subscribers were 46% of the total population with Nigeria having the highest number of mobile phones [21,22,23]. However, there is sparse data showing effective linkage of mobile and digital technology with access, and/or delivery of healthcare for CVDs in sSA.
Existing technologies such as automated blood pressure measurements which form the basis for the diagnosis and management of hypertension have also been shown to simplify measurement processes and minimize misclassification errors that could have serious implications in the management of CVDs [24]. Other higher-end diagnostic and therapeutic technologies for CVDs remain largely out of reach for majority of the populations living in sSA due to several factors such as costs, access, availability and general lack of awareness.
Health Policies and Systems
Universal access to healthcare for CVDs which includes the full range of essential health services — ranging from health promotion to prevention, curative treatment, rehabilitation and palliative care — remain out of reach for majority of the populations living in sSA. In instances where there is the ideal coverage for CVDs, this comes at a prohibitively high cost, limiting universal access. According to the WHO, universal health coverage (UHC) implies that all people have access to the health services they need, and of sufficient quality, without suffering financial hardship [25]. UHC is embedded within the third United Nations Sustainable Development Goal (UN SDG-3) and requires effective healthcare financing policies and strategies; however, these remain a challenge in sSA [26]. Catastrophic health expenditures have been reported to impoverish over 100 million people annually worldwide, majority of whom are in sSA where more than 56% of countries are affected by direct out-of-pocket (OOP) payments for healthcare services [27]. In 2022, Eze et al. reviewed population-level and disease-specific factors associated with catastrophic health expenditure in sSA. Morbidities related to NCDs including CVDs, lack of access to specialist healthcare and absent health insurance are examples of contributing factors to high direct OOP payments affecting mainly the elderly, people of lower socioeconomic status, those with chronic illness and those living in rural areas [28].
Human Resources
According to the WHO estimates, Africa has 14% of the world population and bears nearly a quarter of the overall global disease burden but only accounts for less than 4% of the global workforce in healthcare [29]. Another challenge facing not just sSA but most low- and middle-income countries (LMICs) has been brain drain of professional healthcare workers seeking better career and employment prospects in high income countries (HICs) [30,31,32,33]. Of the estimated 23,000 qualified academic and health professionals who emigrate from Africa annually, specialists in CVD healthcare tend to be one of the highest affected [31]. Faced with a double burden of communicable and non-communicable diseases alongside a growing demand for chronic health care, there is need for developing integrated models of healthcare at all levels of health systems in sSA [34]. This will incorporate attraction, training and retaining of competent and skilled personnel as well as capacity building for routine epidemiology and demographic health surveillance systems and research platforms [34].
COVID-19 Pandemic
Infection with severe acute respiratory syndrome coronavirus type-2 (SARS-CoV-2) causing coronavirus disease of 2019 (COVID-19) led to a global pandemic that left the already weak healthcare systems in sSA more vulnerable. This only served to further emphasise the existing gaps in UHC and CVD services within sSA [26]. The epidemiological review by Yuyun et al. was conducted prior to the COVID-19 pandemic [5]. Elderly patients and those with chronic CVDs have been shown to be at a higher risk of morbidity and mortality from COVID-19 compared to the rest of the population from published literature [35]. Emerging data from cohorts of patients in the West who recovered from COVID-19 and survived have revealed increased risk to the cardiovascular system [36], including in those who were vaccinated [37]. There has been limited data on the impact of COVID-19 on CVDs in sSA with one published report showing discordant association of COVID-19 on overall mortality in sSA [38]. One plausible hypothesis for the relatively lower mortality of COVID-19 in sSA has been the possible mandatory and high use of the Bacille Calmette-Guérin (BCG) vaccination against tuberculosis and background anti-retroviral therapy for human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) infection [39]. In 2020, Escobar et al. explored the potential mechanisms underlying BCG vaccination and protection from viral infections of the respiratory tract such as COVID-19. While BCG protection against Mycobacterium tuberculosis is through a cellular immune response, they described an additional long-lasting innate immune response beyond those specific to mycobacteria including modification of macrophages that led to a broad immune protection, a phenomenon referred to as trained immunity [40]. In 2021, the African COVID-19 Critical Care Outcomes Study (ACCCOS) that specifically focused on critically ill and intensive care patients reported higher mortalities in African countries than that reported elsewhere [41]. Some of the factors attributed to this finding of higher COVID-19 related deaths among critically ill Africans included limited critical care resources, comorbidities such as HIV/AIDS and chronic liver, kidney diseases as well as diabetes [41]. The true burden and effect of COVID-19 on CVDs in sSA remains unknown.
Other important challenges which have been previously described by Yuyun et al. include factors such as differences in prevalence of CVDs in different ethnicities [42, 43] and skewed resource allocation. Governments, academic institutions, international health organisations, donors and other stakeholders in sSA ought to develop structured surveillance programmes, seek sustainable funding and invest in research in order to capture vital statistics and the true morbidity and mortality burden from CVDs in sSA [5].
Priorities
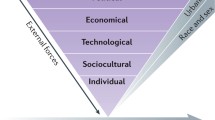
In order to address these gaps and effectively reduce the increasing burden of CVDs, there is an urgent need to establish priorities for policy formulation, resource allocation and capacity development for public healthcare, clinical service delivery and research in sSA. Additionally, a wholistic approach aimed at prevention of CVDs through risk-factor modification and overall wellbeing, rather than the fragmented focus on curative services for specific disease entities will be an important priority in reducing the burden of CVDs in sSA. These factors can be considered at different levels; individual, local health institutional regional administrative units, national government, pan-African and global scales.
At the global policy level, the WHO published a resolution recommending prioritization of the implementation, expansion and integration of digital health technologies to strengthen existing health systems [44]. Indeed, the previously untapped potential of digital health became even more apparent during the imposed restrictions on close social contact as a result of the COVID-19 pandemic. However, this served to highlight some policy and regulatory restrictions that hinder digital health expansion and the need for governments to urgently address these, since the benefits of digital health transcend COVID-19 and will impact CVDs as well [45].
The current ratio of 0.8 health workers per 10,000 inhabitants in Africa falls way below the WHO recommended minimum threshold of 44.5 health workers per 10,000 population in 2030 [46]. The ratio of health workers for delivery of specialized healthcare for CVDs in sSA is even lower and needs to be addressed through policies and programs aimed at expansion of training opportunities as well as retention of these specialists in hospitals and health institutions within sSA. One way to address the shortages is through collaborations. These can be between universities, hospitals and research institutions within a county or even across different countries. The leading hubs for cardiovascular research collaboration in sSA are the Hatter Institute for Cardiovascular Research in Africa (HICRA) at the University of Cape Town and the Chris Baragwanath Hospital that is affiliated with the University of Witwatersrand all in South Africa [47]. Through a number of multi-country studies and collaborations, other sSA countries have benefitted from the resources, expertise and training in CVD research at these institutions [47]. There are other inter-university collaborations happening predominantly in the Anglophone-speaking compared to Francophone-speaking sSA countries that is partly attributed to dominance of institutions in South Africa and Nigeria; however, the Pan-African Society of Cardiology (PASCAR) continues to advocate for collaboration, networking and resource-mobilisation for CVD research and training in sSA [47,48,49]. These efforts could help increase the availability and access to specialist healthcare workers for CVDs in rural and other under-served areas in sSA. Other unique collaborations focusing on CVDs could arise in a similar way that the ACCCOS collaboration described above developed spontaneously in response to the COVID-19 pandemic [41]. The COVID-19 pandemic led to disruption in the delivery of regular healthcare services including CVD services across most parts of Africa. An explanatory study focusing on the effects of COVID-19 in South Africa reported impact of factors such as increased surveillance and behaviour change on the health system and society in general but not CVD specifically [50]. However, the reorganisation of public health services including incorporation of surveillance systems could be used prospectively for implementation of better monitoring and improved delivery of healthcare to CVD patients [51].
At the level of healthcare facilities, there is increasing research on geospatial mapping, including the recently reported mapping of 98,745 public health facilities [52]. In keeping with SDG-3 on healthcare, access to health services is important for achieving equity and UHC. To achieve this, defining the geographical availability of health services in relation to the communities they serve and increasing complexity of the referral chain is necessary [52]. While attempts have been made at mapping health facilities in sSA, majority of the reports in the literature have focused on primary healthcare facilities offering basic medical and surgical care rather than specialist services including CVD care [52, 53] with the geospatial mapping being done after the COVID-19 pandemic [54, 55]. Prior to the onset of the COVID-19 pandemic, Chikafu and Chimbari (2019), had described a rise in CVD admissions in sSA with rural residence and lower socio-economic status being negatively associated with utilization of healthcare facilities [56]. This could be attributed to both the lack of specialist healthcare facilities for CVD in rural areas as well as a high cost of accessing this care where it was available. Kapwata and Manda (2018) had reported similar findings in South Africa with lower densities of health facilities offering CVD care for populations living in rural settings leaving populations at risk of CVD-related morbidity and mortality due to factors such as late diagnosis and lack of proper management [57]. Notably, mapping and integration of geospatial datasets to evaluate constraints of physical distancing during the COVID-19 pandemic has been done in Kenya [58]. This can be replicated in the mapping of access to specialist CVD healthcare services. Additionally, infrastructural investment in health facilities to enable reliable data-capture for accurate quantification of the burden of CVD in sSA will be required. These systems will need to ideally leverage on the health technology potential in Africa as well as be scalable for maximal benefit [18].
At the individual level in sSA context, future priorities need to focus on CVD-educational initiatives aimed at increasing health-seeking behaviour [59] as well as maintaining regular follow-up contact with healthcare services when known to have pre-existing risk-factors for CVD [60]. With the potential for many functionalities, future digital health technologies should focus more on features likely to impact an individual’s behaviour and that will largely be aimed at preventing CVDs [61]. Existing examples of these include wearable devices which have been shown to impact lifestyle factors like physical activity as well as other outcomes such as blood pressure, management of blood sugars and lipid levels among others [17].
This study has some limitations. The higher prevalence of CVDs reported in urban areas could be due to availability of surveillance and access to diagnostic systems that are unavailable in rural areas. Other factors that could lead to seemingly lower prevalence of disease in rural areas include lack of awareness due to comparatively lower literacy levels as well as lack of access to specialist care for early diagnosis and timely treatment of CVDs. Other limitations that could not be explored due to lack of description in the literature on CVDs included health seeking behaviours and religious beliefs in communities living in sSA countries.
In summary, the interplay of all these factors eventually has a bearing on CVD-related burden and will need strategic planning, prioritization and implementation of policies and practices to reduce CVDs and improve clinical outcomes in sSA.
Data Availability
All the articles and websites quoted in the review are publicly available and accessible.
Code Availability
Not applicable.
Abbreviations
- ACCCOS :
-
African COVID-19 Critical Care Outcomes Study
- AIDS :
-
Acquired immunodeficiency syndrome
- BCG :
-
Bacille Calmette-Guérin
- CHD :
-
Congenital heart disease
- COVID-19 :
-
Coronavirus disease of 2019
- CVDs :
-
Cardiovascular diseases
- GSMA :
-
Global system for mobile communications
- HICs :
-
High-income countries
- HICRA :
-
Hatter Institute for Cardiovascular Research in Africa
- HIV :
-
Human immunodeficiency virus
- INTER-CHF :
-
International congestive heart failure study
- LMICs :
-
Low-and-middle-income countries
- NCDs :
-
Non-communicable diseases
- OOP :
-
Out-of-pocket
- PASCAR :
-
Pan-African Society of Cardiology
- RHD :
-
Rheumatic heart disease
- SARS-CoV-2 :
-
Severe acute respiratory syndrome coronavirus type-2
- SDG :
-
Sustainable development goals
- SMS :
-
Short message services
- sSA :
-
Sub-Saharan Africa
- UHC :
-
Universal health coverage
- UN :
-
United Nations
- WHO :
-
World Health Organization
References
Stower H. A disease transition in Sub-Saharan Africa. Nat Med. 2019;25(11):1647.
Etyang AO, Scott JA. Medical causes of admissions to hospital among adults in Africa: a systematic review. Glob Health Action. 2013;6:1–14.
Roth GA, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Mensah GA, et al. Mortality from cardiovascular diseases in Sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26(2 Suppl 1):S6-10.
Yuyun MF, et al. Cardiovascular Diseases in Sub-Saharan Africa compared to high-income countries: an epidemiological perspective. Glob Heart. 2020;15(1):15.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11): e442.
Keates AK, et al. Cardiovascular disease in Africa: epidemiological profile and challenges. Nat Rev Cardiol. 2017;14(5):273–93.
Kwan GF, et al. Endemic cardiovascular diseases of the poorest billion. Circulation. 2016;133(24):2561–75.
Mocumbi AO. Lack of focus on cardiovascular disease in Sub-Saharan Africa. Cardiovasc Diagn Ther. 2012;2(1):74–7.
Organization WH. Noncommunicable diseases. 2021. Available from: https://www.who.int/news-room/factsheets/detail/noncommunicable-diseases#:~:text=Key%20facts,%2D%20and%20middle%2Dincome%20countries. Accessed 14 Aug 2023
Etyang AO, et al. Burden of disease in adults admitted to hospital in a rural region of coastal Kenya: an analysis of data from linked clinical and demographic surveillance systems. Lancet Glob Health. 2014;2(4):e216–24.
Mebrahtom G, et al. Rheumatic heart disease in East Africa: a systematic review and meta-analysis. Int J Rheumatol. 2023;2023:8834443.
Jivanji SGM, et al. Congenital heart disease in East Africa. Front Pediatr. 2019;7:250.
Zikarg YT, Yirdaw CT, Aragie TG. Prevalence of congenital septal defects among congenital heart defect patients in East Africa: a systematic review and meta-analysis. PLoS One. 2021;16(4): e0250006.
Ajayi AA, Sofowora GG, Ladipo GO. Explaining heart failure hyper-mortality in Sub Saharan Africa: global genomic and environmental contribution review. J Natl Med Assoc. 2020;112(2):141–57.
Moran A, et al. The epidemiology of cardiovascular diseases in Sub-Saharan Africa: the Global Burden of Diseases, Injuries and Risk Factors 2010 study. Prog Cardiovasc Dis. 2013;56(3):234–9.
Santo K, Redfern J. Digital health innovations to improve cardiovascular disease care. Curr Atheroscler Rep. 2020;22(12):71.
Njoroge M, et al. Assessing the feasibility of eHealth and mHealth: a systematic review and analysis of initiatives implemented in Kenya. BMC Res Notes. 2017;10(1):90.
Neumark T, Prince RJ. Digital health in East Africa: innovation, experimentation and the market. Glob Policy. 2021;12:65–74. https://doi.org/10.1111/1758-5899.12990.
Africa GSS. The mobile economy Sub-Saharan Africa 2022 report. 2022. Available from: https://www.gsma.com/mobileeconomy/wp-content/uploads/2022/10/The-Mobile-Economy-Sub-Saharan-Africa2022.pdf. Accessed 14 Aug 2023.
Dike FO, et al. Implementation and impact of mobile health (mHealth) in the management of diabetes mellitus in Africa: a systematic review protocol. BMJ Open. 2021;11(12): e047556.
Manyazewal T, et al. The potential use of digital health technologies in the African context: a systematic review of evidence from Ethiopia. NPJ Digit Med. 2021;4(1):125.
Anstey Watkins JOT, et al. Mobile phone use among patients and health workers to enhance primary healthcare: a qualitative study in rural South Africa. Soc Sci Med. 2018;198: 139–47.
Padwal R, et al. Optimizing observer performance of clinic blood pressure measurement: a position statement from the Lancet Commission on Hypertension Group. J Hypertens. 2019;37(9):1737–45.
Darrudi A, Ketabchi Khoonsari MH, Tajvar M. Challenges to achieving universal health coverage throughout the world: a systematic review. J Prev Med Public Health. 2022;55(2):125–33. https://doi.org/10.3961/jpmph.21.542.
Ifeagwu SC, et al. Health financing for universal health coverage in Sub-Saharan Africa: a systematic review. Glob Health Res Policy. 2021;6(1):8.
Bank TW. Delivering quality health services: a global imperative for universal health coverage. 2022. Available from: https://documents.worldbank.org/en/publication/documentsreports/documentdetail/482771530290792652/delivering-quality-health-services-a-globalimperative-for-universalhealth-coverage. Accessed 14 Aug 2023.
Eze P, et al. Factors associated with catastrophic health expenditure in Sub-Saharan Africa: a systematic review. PLoS One. 2022;17(10): e0276266.
Organization WH. Working for health and growth: investing in the health workforce - high-level commission on health employment and economic growth. Available from:https://www.who.int/publications/i/item/9789241511308. Accessed 14 Aug 2023.
Zimbudzi E. Stemming the impact of health professional brain drain from Africa: a systemic review of policy options. J Public Health Afr. 2013;4(1): e4.
Pang T, Lansang MA, Haines A. Brain drain and health professionals. BMJ. 2002;324(7336):499–500.
Kirigia JM, et al. The cost of health professionals’ brain drain in Kenya. BMC Health Serv Res. 2006;6:89.
Misau YA, Al-Sadat N, Gerei AB. Brain-drain and health care delivery in developing countries. J Public Health Afr. 2010;1(1): e6.
Mayosi BM, et al. The burden of non-communicable diseases in South Africa. Lancet. 2009;374(9693):934–47.
Chung MK, et al. COVID-19 and cardiovascular disease: from bench to bedside. Circ Res. 2021;128(8):1214–36.
Xie Y, et al. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–90.
Pillay J, et al. Incidence, risk factors, natural history, and hypothesised mechanisms of myocarditis and pericarditis following COVID-19 vaccination: living evidence syntheses and review. BMJ. 2022;378: e069445.
Chakafana G, et al. Interplay of COVID-19 and cardiovascular diseases in Africa: an observational snapshot. Clin Res Cardiol. 2020;109(12):1460–8.
Wickramasinghe D, Wickramasinghe N, Kamburugamuwa SA, Arambepola C, Samarasekera DN. Correlation between immunity from BCG and the morbidity and mortality of COVID-19. Trop Dis Travel Med Vaccines. 2020;6:17. https://doi.org/10.1186/s40794-020-00117-z.
Escobar LE, Molina-Cruz A, Barillas-Mury C. BCG vaccine protection from severe coronavirus disease 2019 (COVID-19). Proc Natl Acad Sci U S A. 2020;117(30):17720–6.
African C-CCOSI. Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study. Lancet. 2021;397(10288): 1885–94.
Alqahtani F, et al. Effect of race on the incidence of aortic stenosis and outcomes of aortic valve replacement in the United States. Mayo Clin Proc. 2018;93(5):607–17.
DiGiorgi PL, et al. Mitral valve disease presentation and surgical outcome in African-American patients compared with white patients. Ann Thorac Surg. 2008;85(1):89–93.
Labrique A, Agarwal S, Tamrat T et al. WHO Digital health guidelines: a milestone for global health. npj Digit. 2020. https://doi.org/10.1038/s41746-020-00330-2.
Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382(23): e82.
Organization WH. The decade for health workforce strengthening in the SEA region 2015–2024: mid-term review of progress. 2020. Available from: https://apps.who.int/iris/handle/10665/333611. Accessed 14 Aug 2023.
Ettarh RR. Institution-level collaboration in cardiovascular research in Sub-Saharan Africa. Cardiovasc Diagn Ther. 2015;5(4):311–5.
Mocumbi AO. Focus on non-communicable diseases: an important agenda for the African continent. Cardiovasc Diagn Ther. 2013;3(4):193–5.
Thienemann F, et al. The Pan African Society of Cardiology and its commitment to clinical research training. Eur Heart J. 2022;43(28):2652–4.
Mbunge E. Effects of COVID-19 in South African health system and society: an explanatory study. Diabetes Metab Syndr. 2020;14(6):1809–14.
Chippaux JP. Impact of COVID-19 on public health in Sub-Saharan Africa. Bull Acad Natl Med. 2023;207(2):150–64.
Maina J, et al. A spatial database of health facilities managed by the public health sector in Sub Saharan Africa. Sci Data. 2019;6(1):134.
Juran S, et al. Geospatial mapping of access to timely essential surgery in Sub-Saharan Africa. BMJ Glob Health. 2018;3(4): e000875.
South A, et al. A reproducible picture of open access health facility data in Africa and R tools to support improvement. Wellcome Open Res. 2020;5:157.
Moturi AK, et al. Geographic accessibility to public and private health facilities in Kenya in 2021: an updated geocoded inventory and spatial analysis. Front Public Health. 2022;10:1002975.
Chikafu H, Chimbari MJ. Cardiovascular disease healthcare utilization in sub-saharan africa: a scoping review. Int J Environ Res Public Health. 2019;16(3):419. https://doi.org/10.3390/ijerph16030419.
Kapwata T, Manda S. Geographic assessment of access to health care in patients with cardiovascular disease in South Africa. BMC Health Serv Res. 2018;18(1):197.
Chamberlain HR, Macharia PM, Tatem AJ. Mapping urban physical distancing constraints, Sub-Saharan Africa: a case study from Kenya. Bull World Health Organ. 2022;100(9):562–9.
Hertz JT, Sakita FM, Kweka GL, Loring Z, Thielman NM, Temu G, Bartlett JA. Healthcare-seeking behaviour, barriers to care and predictors of symptom improvement among patients with cardiovascular disease in northern Tanzania. Int Health. 2019;14(4):373–80. https://doi.org/10.1093/inthealth/ihz095.
Etyang AO, et al. Blood pressure and arterial stiffness in Kenyan adolescents with the Sickle cell trait. Am J Epidemiol. 2018;187(2):199–205.
Neubeck L, et al. The mobile revolution–using smartphone apps to prevent cardiovascular disease. Nat Rev Cardiol. 2015;12(6):350–60.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
Both authors were involved in the initial conceptualisation. NGO wrote the initial draft and AOE reviewed and provided critical input. Both authors have read and approved the final manuscript submitted.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Obonyo, N.G., Etyang, A.O. Cardiovascular Health Priorities in Sub-Saharan Africa. SN Compr. Clin. Med. 5, 262 (2023). https://doi.org/10.1007/s42399-023-01605-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01605-x