Abstract
Prediction of mortality in growing aged population will offer several benefits for health sector. Cystatin C, which has long been known as biomarker to more accurately evaluate glomerular filtration rate in elderly, has also been shown to predict mortality from several studies. Studies regarding its predictive ability were vastly varied, and there has not been systematic review to examine its ability in predicting long-term mortality in elderly population. This study aimed to evaluate cystatin C performance as predictor for all-cause and cardiovascular mortality among elderly population. A systematic review of prospective cohort studies was performed. Literature searching was done in major databases such as PubMed, Cochrane, Scopus, EBSCOhost, and ProQuest. Manual searching was also performed. Inclusion criteria were studies involving elderly age 65 or older, cystatin C serum levels available, all-cause mortality as outcome, and 5-year minimum of follow-up. Study selection was performed according to PRISMA algorithm. Newcastle–Ottawa scale for cohort study was used to assess primary studies’ quality and risk of bias. Study results were presented in descriptive tables and forest plot. Initial searching revealed 609 hits with 12 studies eligible for the review: five studies evaluated all-cause mortality, three studies evaluated cardiovascular mortality, and four studies evaluated both. Meta-analysis showed that high cystatin C levels are increasing risk of long-term all-cause mortality [(HR: 1.74 (95% CI: 1.48–2.04); p < 0.0001)] and cardiovascular mortality [HR: 2.01 (95% CI: 1.63–2.47); p < 0.0001)]. The prognostic ability of cystatin C was considerably moderate [AUC 0.70 (95% CI: 0.68–0.72); p = 0.02]. Cystatin C was able to predict long-term mortality in elderly population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystatin C (CysC), a 13-kDa molecules produced constantly by all nucleated cells, has been shown better to reflect renal function estimate. Cystatin C is less influenced by other extrarenal factors that may altered its serum concentration [1]. In addition, CysC has been shown to have several predictive value as well, especially in all-cause and cardiovascular mortality. Study found that it was able to predict rehospitalization in heart failure patients [2]. In general population with normal kidney function, higher CysC value was associated with higher mortality risk [3]. It was also associated with non-cardiovascular mortality after variable adjustment as well in one study [4].
In elderly population, primary studies were showing that CysC was better to predict mortality than creatinine [5,6,7,8]. Creatinine, which has been used long enough to estimate glomerular filtration rate (eGFR), is influenced by extrarenal factors in elderly. Creatinine production depends on muscle mass and nutritional status which were altered in older people, and also, it was deemed to insensitively reflect the degree of nephron loss [5, 9]. However, the studies that sought prognostic ability of cystatin C in elderly were varied in magnitude of prognostic value, moreover with significant variation, such as the subject studied, comorbidities, and degree of kidney function [10].
Predicting mortality may offer a lot of benefits regarding risk stratification and be used as prevention and may be targeted therapy in the future. Therefore, in the current study, we performed meta-analysis aimed to evaluate the ability of cystatin C to predict long-term all-cause mortality and cardiovascular mortality in elderly population.
Material and Methods
This is a systematic review of prospective observational studies conducted with the guidance of Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. Review protocol was submitted to PROSPERO, registration number CRD42020196010.
Articles Selection
Searching was performed on May 2020–7 July 2020 in five databases: PubMed, Cochrane, Scopus, EBSCOhost, and ProQuest. We also conducted hand-searching and snowballing strategy from the literature to search best available evidence. Peer group of selected topics of interest was also performed. Internet searching was performed using the following keywords from the PICO strategy: “elderly,” “cystatin c,” “mortality,” “cardiovascular mortality,” and “follow-up.” Boolean operators were used such as “AND” and “OR,” and truncation operators and MESH term were also used whenever possible. There was no language and year of publication restriction applied. All articles found were recorded in a database. Study selection performed following PRISMA algorithm. Screening duplicate was performed using Microsoft Excel. All searching hits were saved in “.RIS format” or “PubMed format,” and they were decoded, and we remove all unnecessary punctuation before screening duplicate was performed. Study selection was performed by two independent researchers.
Eligibility Criteria
The eligibility criteria were prospective observational study which involved elderly minimum 65 years old of age on average with baseline cystatin C serum levels stated in main study, and all-cause mortality was one of the outcomes. The minimum follow-up length was 5 years (long term). Exclusion criteria were study of acute kidney injury subjects, evaluating urinary biomarkers, and short-term mortality (i.e., hospital mortality). We excluded reviews, letters, or posters publication.
Data Extraction
Data extraction were done using RevMan 5.3. software by Cochrane. The following data were extracted from each eligible study: author name, year of publication, subject number, age, type of population studied, outcomes, methods of cystatin C measurement, cystatin C levels classification, methods of glomerular filtration rate estimation (eGFR), creatinine serum levels classification, and variables that were used in Cox proportional hazard multivariate analysis. Data extracted is presented in descriptive tables.
Quality Assessment and Risk of Bias
Quality assessment and risk of bias were assessed using Newcastle–Ottawa scale (NOS) for cohort study. NOS for cohort study comprises of three domains: selection, comparability, and outcome with eight questions, and a maximum of nine stars could be given to each study. Study with 1–3 stars was qualified poor, 4–6 stars were moderate, and 7–9 stars were good. The assessment was performed by two independent reviewers. Third reviewer opinion was asked if there was any disagreement.
Meta-Analysis
The meta-analysis included only those studies that assessed the outcome all-cause mortality as primary outcome or cardiovascular mortality as secondary outcome, comparing the highest division (tertile, quartile, or quintile) of cystatin C with the first quartile (lowest division). The hazard ratio value and the 95% confidence interval adjusted by the multivariate regression analysis were used in the meta-analysis. Higgins I2 test was used to assess the heterogeneity between studies. We also performed the meta-analysis of AUROC value and relative risk of eGFR. The studies were considered heterogeneous when I2 > 60%. When there was homogeneity, the hazard ratio was calculated using the fixed effect model. When there was significant heterogeneity, the hazard ratio was calculated using the random effect model. If data were too heterogenous, we performed narrative review. We used statistical software ReviewManager version 5.3 to perform the statistical analysis and R software to perform meta-analysis of AUROC.
Results
Literature Search
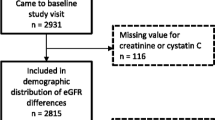
There were 609 hits of articles at initial. After screening and selection, there were 12 eligible studies analyzed. Flowchart of literature search was conducted by accordance of PRISMA 2009 and presented in Fig. 1.
Description of Eligible Study
The description of twelve eligible studies is presented in Table 1. Descriptive data about methods of measuring eGFR and creatinine are presented in Table 2.
Quality Assessment and Risk of Bias
The quality and risk of bias assessment of each individual study are presented in Table 3.
There were six studies with moderate quality and other six studies with good quality. Maximum of two stars were given for comparability scoring, as follow: one star was given if the study performed multivariate analysis to clinical variables, two stars were given if the study performed multivariate analysis to clinical variables AND marker of inflammation.
Analysis of Data
Meta-analysis was performed for cystatin C and all-cause mortality and cardiovascular mortality. For all-cause mortality studies, involving 9408 participants, we found that higher cystatin C levels predict long-term mortality (HR 1.74 (95% CI; 1.48–2.04); p < 0.00001) compared to lower cystatin C groups. The forest plot can be seen in Fig. 2. Risk of mortality was higher for cardiovascular mortality (HR 2.01 (95% CI; 1.63–2.47) p < 0.00001)) (see Fig. 3). However, both possessed significant heterogeneity, so random effect was used (I2 65% for all cause and 77% for cardiovascular mortality) in this analysis.
Subgroup analysis was performed by dividing studies into healthy elderly and morbid elderly. The heterogeneity for all-cause mortality after subgroup analysis were reduced in both groups with similar hazard ratio value. Meanwhile, the heterogeneity for cardiovascular mortality after subgroup analysis was still high, the risk was even higher for morbid elderly (HR 2.29 (95% CI; 1.54–3.42). See Fig. 4.
The accuracy of prognostic ability of cystatin C to predict long-term all-cause mortality is presented in Fig. 5.
The prognostic accuracy of cystatin C to predict long-term all-cause mortality was moderate (AUC 0.70 (95% CI: 0.68–0.72; p = 0.02)).
Discussion
In this study, we found that higher cystatin C level was shown to increase the risk of long-term all-cause mortality in elderly compared to lower cystatin C level. The risk was even higher for cardiovascular mortality. We observed that this relationship was consistent among studies. Primary studies also showed that HR of mortality was increasing along with cystatin C quartiles [5, 8]. In one study, this relationship was not observed in creatinine percentile; only the highest has significant HR to mortality [5].
The heterogeneity observed in our analysis might be contributed by difference of population used in primary studies. In the case of all-cause mortality, heterogeneity was reduced after studies were grouped according to baseline disease. It was quite challenging to perform meta-analysis due to variation of cystatin C value among groups. The lowest cystatin quartile we observed was < 0.55 mg/L, while the highest was > 2.34 mg/L. In order to minimize heterogeneity, we decided to select cystatin C quartiles that were quite similar to be compared to lowest cystatin C value. Therefore, the range of highest cystatin C used in our analysis was > 1.06– > 1.26 mg/L, while the lowest was < 0.88 mg/L.
We found that in all-cause mortality, heterogeneity might be attributed by difference in follow-up time. Studies with longer follow-up time might have higher death rates compared to shorter ones. In the subgroup analysis, the HR of morbid elderly might seem lower than in healthy elderly. However, this must be cautiously interpreted because there were only two studies that addressed this. More studies were needed to more accurately seek this relationship. On the other side, morbid elderly was shown to have increased risk of cardiovascular death compared to the healthy ones as we used more studies.
In the analysis, we used adjusted hazard ratio, which means the results had been adjusted to the risk to several important clinical risk factors that might contribute to mortality. Although variation of risk factors could not be avoided, this implies that cystatin C might predict mortality independently from clinical factors. However, this must be sought further in a homogenous study and analysis. There were only four studies did adjusted analysis to inflammatory markers, such as CRP, IL-6, or TNF-α. Three studies incorporated them in clinical model [13, 16, 21], but one did separate analysis from the clinical model [5]. It was observed that inflammatory status attenuated hazard ratio which implies inflammation might have a role that can biologically explained in relation to mortality.
In all of the studies included, lower eGFR was associated with higher risk of mortality. However, the hazard ratios for mortality were higher for CysC compared to eGFR and Cr within the same percentiles. The presence of chronic kidney disease in subjects did increase the hazard ratios for mortality. As we know, chronic low-grade inflammation has long been known as the hallmark of chronic kidney disease. Several factors such as increased pro-inflammatory cytokine production, oxidative stress, acidosis, infection, disruption of adipose tissue metabolism, and gut dysbiosis are playing the role. Pro-inflammatory cytokines in circulation may activate microvascular in the kidney which later create reactive oxygen species (ROS) and more pro-inflammatory cytokines. This may lead to disrupt ion of adhesion molecule in cell surface, glycocalyx destruction, and altered endothelial which may activate the coagulation system [22].
There were some possible explanations regarding the more pronounced effect of CysC compared to eGFR and Cr serum, especially in elderly. First, Shrunken pore syndrome (SPS), defined by a eGFRcys/eGFRcr being < 0.6 or < 0.7 in the absence of extrarenal influences of serum CysC and Cr concentration, has been associated with increased in long-term mortality and morbidity, even in the absence of reduced GFR [23]. In this particular syndrome, renal clearance of 10–30 kDa molecules was selectively decreased compared to the clearance of smaller molecules like creatinine (0.113 kDa) or water (0.018 kDa) [24]. Therefore, inflammatory molecules might not be filtered out while causing damage in the body.
Second, if we dig into molecular mechanism, inflammasome might have a role that explained the relationship between cystatin C, elderly, and mortality. NLR family pyrin domain containing 3 (NLRP3) in the inflammasome has been known to play a major role in kidney disease such as glomerulonephritis, crystals nephropathy, diabetic nephropathy, hypertensive nephropathy, and nephritis lupus. It can be activated by several danger-associated molecular pattern (DAMPs) such as ATP, uric acid, oxidatively modified DNA, cholesterols, aggregates of protein, and ROS. DAMPs were also present in elderly which may exert such reaction (inflammaging). If NLRP3 is activated, it will commence NF-κB pathway and produce IL-1β and IL-18 as a pro-inflammatory cytokines [22, 25, 26].
Moreover, NLRP3 suggested to have a role on atherosclerotic lesion. Activation of NLRP3 will enhance lipid deposition and macrophage migration, thus promoting faster foam cell formation. NLRP3 also exerts its effect on fibroblast in cardiac cells which further enhance ischemic damage. IL-1β and IL-18 were also high in atherosclerotic lesion [27].
Research explained that cystatin C has a role of regulating host immune systems. One of the mechanisms is via monocyte and macrophages, which abundantly found in atherosclerosis plaque [28]. While it has been known that cystatin C inhibits cathepsin which in results decreasing atherosclerosis formation [29], latest research showed that cystatin C had non-cathepsin pathway. The non-cathepsin pathway will alter homeostasis through antagonizing TGF-β docking to its receptor and directly cause inflammation through fibril deposition in vascular wall [28]. This explains the relationship between high cystatin C and cardiovascular events in elderly, especially with chronic kidney disease.
The accuracy of prognostic ability of cystatin C to predict mortality was acceptable. Cumulative AUC we performed in our analysis show AUROC of 0.70 (95% CI; 0.68–0.75). It was higher compared to creatinine or eGFR. The adjusted AUC told us to use prognostic ability of cystatin C with wise consideration to other clinical factors. Our analysis also strengthen the use of CKD-EPI equation in elderly as it is more precise in such subject.
Predicting long-term mortality in elderly population offers benefits such as to help in stratifying risk of cardiovascular outcome later. Risk stratification might help clinician to decide primary or secondary prevention. Cystatin C might play as more accurate measures to estimate kidney function while predicting long-term mortality as well. Nevertheless, the prognostic features must be tailored each and cannot be generalized. Future studies should take in specific population and clinical variables to seek further stronger relationship. In daily practice, cystatin C may not be readily available to access in several areas, and the cost is still quite high compared to creatinine. We hope that in the near future, the cost might be reduced so it could be accessed easily.
To our knowledge, this is the first meta-analysis that seeks long-term mortality risk of cystatin C levels in elderly population. The studies included were good and in moderate quality. This systematic review also combines large studies from several race and geographic location so it can be widely used. However, there are some limitations we realized in this study. First, study heterogeneity was still high due to population and difference in cardiovascular pathology (ranging from ischemic heart disease, congestive heart failure, to peripheral arterial disease). The percentage division of cystatin C levels also varied; therefore, a cutoff value cannot be obtained from this study. Future studies should saw the value considered high risk to mortality in elderly. Third, not all primary study stated to exclude hyper-/hypothyroidism which may influence cystatin C levels in blood.
Conclusion
Higher cystatin C level was associated with higher risk of long-term mortality in elderly. Higher cystatin C associated with increased risk of all-cause mortality and cardiovascular mortality is compared to low cystatin C level.
Data Availability
The authors declare that the data supporting the findings of this study are available within the article (and its supplementary information files).
Code Availability
N/A.
References
Tenstad O, Roald AB, Grubb A, Aukland K. Renal handling of radiolabelled human cystatin C in the rat. Scand J Clin Lab Invest. 1996;56(5):409–14.
Chen S, Tang Y, Zhou X. Cystatin C for predicting all-cause mortality and rehospitalization in patients with heart failure : a meta-analysis. Biosci Rep. 2019;39(2):20181761.
Einwoegerer CF, Domingueti CP. Original article association between increased levels of cystatin C and the development of cardiovascular events or mortality : a systematic review and Meta-Analysis. Arg Bras Cadiol. 2018;111(6):796–807.
Fried LF, Katz R, Sarnak MJ, Shlipak MG, Chaves PHM, Jenny NS, et al. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005;16(12):3728–35.
Shlipak MG, Fyr CLW, Chertow GM, Harris TB, Kritchevsky SB, Tylavsky FA, et al. Cystatin C and mortality risk in the elderly: the Health, Aging, and Body Composition study. J Am Soc Nephrol. 2006;17(1):254–61.
Bevc S, Hojs N, Knehtl M, Ekart R, Hojs R. Cystatin C as a predictor of mortality in elderly patients with chronic kidney disease. Aging Male [Internet]. 2018;0(0):1–6. https://doi.org/10.1080/13685538.2018.1479386.
Id JZW, Moon YP, Husain SA, Elkind MSV, Sacco L, Wolf M, et al. Creatinine versus cystatin C for renal function-based mortality prediction in an elderly cohort : the Northern Manhattan Study. PLoS One. 2020;15(1):1–26.
Shlipak MG, Sarnak MJ, Katz R, Fired LF, Seliger SL, Newman AB, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. NEJM. 2005;352(20):2049–60.
Herget-Rosenthal S, Marggraf G, Hüsing J, Göring F, Pietruck F, Janssen O, et al. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004;66(3):1115–22.
Shlipak MG, Mattes MD, Peralta CA. Update on cystatin C: incorporation into clinical practice. Am J Kidney Dis. 2013;62(3):595–603.
Shinkai S, Chaves PHM, Fujiwara Y, Watanabe S, Shibata H, Yoshida H, et al. B2 -microglobulin for risk stratification of total mortality in the elderly population. Arch Intern Med. 2008;168(2):200–6.
Alehagen U, Dahlström U, Lindahl TL. Cystatin C and NT-proBNP, a powerful combination of biomarkers for predicting cardiovascular mortality in elderly patients with heart failure: results from a 10-year study in primary care. Eur J Heart Fail. 2009;11(4):354–60.
Emberson JR, Haynes R, Dasgupta T, Mafham M, Landray MJ, Baigent C, et al. Cystatin C and risk of vascular and nonvascular mortality: a prospective cohort study of older men. J Intern Med. 2010;268(2):145–54.
Hoke M, Pernicka E, Niessner A, Goliasch G, Amighi J, Koppensteiner R, Minar E, Mlekusch W, Rumpold H, Wagner O, Schillinger M. Renal function and long-term mortality in patients with asymptomatic carotid atherosclerosis. Thromb Haemost. 2012;107(1):150–7.
Skoglund PH, Arpegård J, Östergren J, Svensson P. Amino-terminal pro-B-type natriuretic peptide and high-sensitivity C-reactive protein but not cystatin C predict cardiovascular events in male patients with peripheral artery disease independently of ambulatory pulse pressure. Am J Hypertens. 2014;27(3):363–71.
Hoogeveen EK, Geleijnse JM, Giltay EJ, Soedamah-Muthu SS, De Goede J, Oude Griep LM, et al. Kidney function and specific mortality in 60–80 years old post-myocardial infarction patients: a 10-year follow-up study. PLoS One. 2017;12(2):1–17.
Fu Z, Yang X, Shen M, Xue H, Qian G, Cao F, et al. Prognostic ability of cystatin C and homocysteine plasma levels for long-term outcomes in very old acute myocardial infarction patients. Clin Interv Aging. 2018;13:1201–9.
Werner K, Christensson A, Legrand H, Pihlsgård M, Sterner G, Elmståhl S, et al. Cystatin C and creatinine-based eGFR levels and their correlation to long-term morbidity and mortality in older adults. 2019; 1461–9
Mooney JF, Croal BL, Cassidy S, Lee VW, Chow CK, Cuthbertson BH, et al. Relative value of cystatin C and creatinine-based estimates of glomerular filtration rate in predicting long-term mortality after cardiac surgery: a cohort study. BMJ Open. 2019;9(9):1–9.
Deo R, Fyr LW, Fried LF, Newman AB, Chertow GM, Cummings SR, et al. Kidney dysfunction and fatal cardiovascular disease — an association independent of atherosclerotic events : results from the Health , Aging , and Body Composition ( Health ABC ) study. 2008
Shlipak MG, Katz R, Sarnak MJ, Fried LF, Newman AB. Cystatin C and prognosis for cardiovascular and kidney outcomes in elderly persons without chronic kidney disease. Ann Intern Med. 2006;145(4):237–46.
Mihai S, Codrici E, Popescu ID, Enciu A, Albulescu L, Necula LG, et al. Review article inflammation-related mechanisms in chronic kidney disease prediction , progression , and outcome. 2018;2018.
Åkesson A, Lindström V, Nyman U, Jonsson M, Abrahamson M, Christensson A, et al. Shrunken pore syndrome and mortality: a cohort study of patients with measured GFR and known comorbidities. Scand J Clin Lab Invest [Internet]. 2020;80(5):412–22. https://doi.org/10.1080/00365513.2020.1759139.
Grubb A. Shrunken pore syndrome - a common kidney disorder with high mortality Diagnosis, prevalence, pathophysiology and treatment options. Clin Biochem [Internet]. 2020;83(June):12–20. https://doi.org/10.1016/j.clinbiochem.2020.06.002.
Komada T, Muruve DA. The role of inflammasomes in kidney disease. Nat Rev Nephrol [Internet]. 2019;15(August). https://doi.org/10.1038/s41581-019-0158-z
Chi K, Geng X, Liu C, Cai G, Hong Q. Review article research progress on the role of inflammasomes in kidney disease. Mediators of Inflammation. 2020;1–9. https://doi.org/10.1155/2020/8032797
Chen Z, Martin M, Li Z, Shyy JY-J. Endothelial dysfunction: the role of SREBP-induced NLRP3 inflammasome in atherosclerosis. Curr Opin Lipidol. 2011;4(164):339–49.
Zi M, Xu Y. Involvement of cystatin C in immunity and apoptosis. Immunol Lett. 2018;196:80–90.
Salgado JV, Souza FL, Salgado BJ. How to understand the association between cystatin C levels and cardiovascular disease: imbalance, counterbalance, or consequence? J Cardiol [Internet]. 2013;62(6):331–5. https://doi.org/10.1016/j.jjcc.2013.05.015.
Author information
Authors and Affiliations
Contributions
The author CT has made substantial contributions to the conception, design of the work, acquisition, analysis, and data interpretation and also drafted the work and revision. Author LAB has made contribution in the conception and interpretation of data. Author MBM has made contribution in analysis and interpretation of data. Author AR has made substantial contribution in work design, analysis and data interpretation, and revision of the data. Author KR has made contribution in analysis and revision. All of the authors have approved the submitted revision and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, is appropriately investigated and resolved, and the resolution is documented in the literature.
Corresponding author
Ethics declarations
Ethics Approval
N/A
Consent to Participate
N/A
Consent for Publication
N/A
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanto, C., Bawazier, L.A., Marbun, M.B.H. et al. Cystatin C as Predictor of Long-Term Mortality in Elderly: a Systematic Review and Meta-Analysis. SN Compr. Clin. Med. 4, 171 (2022). https://doi.org/10.1007/s42399-022-01233-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01233-x