Abstract
We studied the introduction rate after a negative challenge to mixed tree nut biscuit. This is a retrospective review of patients who underwent and passed mixed tree nut biscuit challenges performed at Princess Margaret Hospital (PMH) between 2016 and 2018. Follow-up phone calls were made to families to ascertain if the tree nuts included in the tree nut biscuit were still included in the child’s diet 1 to 3 years following negative oral food challenge (OFC). A total of 162 children underwent mixed tree nut biscuit challenge between 2016 and 2018 at Princess Margaret Hospital, Perth, Western Australia. A total of 141 (87%) passed mixed tree nut biscuit challenge. Of the 133 children that were contacted (8 children could not be contacted), 104 children still included some or all of the challenge nuts in the child’s diet; with 24 children completely eliminating the challenge nuts (18%), 5 children eliminated some of the challenge nuts (3.5%). We found a high introduction rate (82%); however, some families may require more support to maintain the tree nuts in the child’s diet following a negative OFC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
To the Editor
Undiagnosed food allergy without known reaction to the avoided food could result in elimination of the suspected food from a child’s diet [1]. Performing OFC to individual tree nuts is time consuming and impractical. Following a negative OFC children need to regularly include that food in their diet with evidence showing this may help to maintain tolerance to that food [2].
Introduction
We studied the dietary introduction rate of tree nuts following a negative OFC. Most of the children avoided tree nuts because they were allergic to other foods or sensitized to tree nuts with no known clinical reaction. Some were avoiding tree nuts because another family member has a nut allergy.
Materials and Methods
The patients in this study are from a retrospective review of patients with a negative OFC to mixed tree nut biscuit performed at Princess Margaret Hospital (PMH), Western Australia between 2016 and 2018.
The tree nuts used in the OFC are almond, Brazil nut, macadamia, cashew, pistachio, walnut, pecan, hazel nut, pine nut, and coconut. Mixed tree nut biscuit OFC included at least 2 of the above nuts.
The cohort of patients had predominantly negative or low positive skin prick test (< 6-mm mean skin prick test weal diameter). Although most of the patients had a negative skin prick test (SPT), the challenge was done in hospital as families were anxious or reluctant to introduce the nuts at home.
The SPT was performed and read as per the published guidelines of the Australasian Society of Clinical Immunology and Allergy [3]. The SPT size on the day of the challenge was recorded.
The treating physician decides what nuts were included in the biscuit, and the patient’s family baked and provided the mixed tree nut biscuit according to the recipe provided by the PMH Immunology Department. The biscuit was then administered in a 5-step procedure starting with 1/16, 1/8, 1/4, 1/2, and the reminder of the biscuit given at 15-min intervals if challenge was performed in the outpatient department (OPD) or as a 7-step procedure starting with 1/64, 1/32, 1/16, 1/8, 1/4, 1/2, and reminder of the biscuit given at 20-min intervals if challenge was performed in the day procedure unit (DPU). The decision to either perform the challenge in the OPD or DPU was determined by the treating physician based on the clinical risk of allergic reaction. Eight grams of each challenge nut were included in the biscuit.
Signed consent for the challenge was obtained from the parents prior to the challenge.
Patients were recorded as a positive OFC if there were objective signs of an IgE-mediated reaction as follows: angioedema, generalized skin erythema, stridor, cough, wheeze, at least 3 or more noncontact urticaria persisting for 5 min or more, rhinoconjunctivitis, abdominal pain, vomiting, and hypotension [4]. All patients had follow-up phone contact 2–4 weeks following the OFC. The patients were termed tolerant if they had a negative OFC and were tolerating the nuts at their 2–4-week follow-up phone calls. Patients that passed the challenge were advised to continue eating the nuts included in the biscuit regularly (at least weekly).
Data was obtained from electronic patient records as well as patient charts and used in strictly anonymous form, according to the code of conduct for medical research approved by the hospital’s Medical Ethical Committee (Child and Adolescent Health Service Safety and Quality Committee).
Results
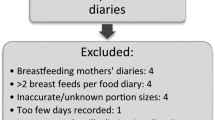
A total of 162 children underwent mixed tree nut biscuit OFC between 2016 and 2018 at PMH. A total of 141 passed mixed tree nut biscuit challenge (87%). The majority of OFCs were conducted in the OPD (70.4%). All 141 patient charts were examined with follow-up phone calls made to families to ascertain if the nuts were still included in the child’s diet 1–3 years following the OFC. Eight families could not be contacted. The majority were male (55%). Median age at challenge was 8 years and 5 months (range 1 year and 7 months to 17 years and 7 months). Twenty-seven children were administered six nut challenge, 40 underwent 5 nut challenge, 38 had 4 nut challenge, 23 had 3 nut challenge, and 13 patients had 2 nut challenge.
Of the 133 families that were contacted, 104 families still included some or all of the challenge nuts in the child’s diet. Twenty-four patients completely eliminated the challenge nuts (18%) and 5 patients eliminated some of the challenge nuts (3.5%).
Discussion
Possible factors influencing the introduction of the challenge nuts in the diet are shown in Table 1. Other patient characteristics with successful, partial, and unsuccessful challenge nut dietary introduction are shown in Table 1. There are no statistically relevant differences between the three groups.
The reasons for the 24 families who completely eliminated the challenge nuts from the child’s diet, in spite of a negative OFC, are depicted in Fig. 1.
Review of Fig. 1 shows 3 children being scared to continue eating the challenge nuts; 4 children being diagnosed with another nut allergy that was not included in the OFC so the family choose to avoid all nuts; 1 child being busy with final year of high school; and another child having general poor health.
More boys (90%) than girls (83%) had partially or successfully introduced the nuts. Of those that continued to eat the nuts, all but 2 families reported there was no reactions to any of the nuts. One family reported that the child developed hives secondary to hazel nut exposure. This child had OFC performed which included almond, hazel nut, Brazil nut, macadamia, and pine nut with the following SPTs: Almond, Brazil nut, and macadamia are all negative SPT. Hazel nut SPT was 4 × 4 mm. Pine nut SPT was 3 × 3 mm.
The other family describes exacerbation of the child’s asthma to all nuts. However, there was no clinical correlation between exposure to nuts and exacerbation of asthma with the elimination of nuts having no impact on the asthma symptoms. This patient was challenged to almond, Brazil nut, walnut (negative SPT), hazel nut (2 × 2 mm SPT), and macadamia nut (1 × 1mm SPT).
Of the 5 children whose families partially introduced the tree nuts, we note the following:
The first child is the same child that excluded hazel nut because she had hives to hazel nut. She retained almond, Brazil, macadamia, and pine nuts in her diet.
Two children ate almond only for no defined reason. One child had challenge to almond, Brazil nut, walnut, and macadamia, while the other child had challenge to almond, macadamia, Brazil, hazel, and pine nuts.
One child retained 2 of the 4 nuts included in their biscuit challenge (hazel and macadamia nuts) with the remaining nuts (brazil and cashew nuts) excluded as this child is reported to be a “fussy eater” by parents.
The last child retained 3 of the 5 nuts included in their biscuit challenge (almond, hazel, and macadamia nuts) with the remaining nuts (brazil and walnut) excluded based on taste.
Average number of tree nuts in challenges was four. Macadamia was the most frequently included tree nut in the OFC. Table 2 is a representation of the tree nuts included in the biscuit and tree nuts eliminated or maintained in the diet following OFC. Just as macadamia, almond, and Brazil nuts were most likely to be maintained in the diet, they also had high rates of elimination from diet which may be a reflection of the frequency these nuts were included in the OFC.
SPT ranged from negative to 7 × 5 mm prior to the test. SPT was done for all nuts included in the biscuit. Figure 2 is a representation of the SPT performed prior to the challenge.
Previous reaction to tree nuts included in the biscuit range from none (sensitized only with no previous exposure) to objective symptoms as well as nonobjective symptoms.
Of all the 139 who had negative OFC, 6 describe symptoms to the challenge nuts prior to the challenge. Characteristics of this group are reflected in Table 3.
The presence of asthma, eczema, allergic rhinitis, and other food allergies was determined in out-patient clinic consultation before the OFC. This information is detailed in Table 4.
Most of the patients that passed the challenge had multiple food allergies. There were 256 cases of documented single or multiple food allergies. Of these 64 are allergic to peanuts, 58 allergic to other tree nuts not included in the OFC, 47 allergic to egg, 18 allergic to cow’s milk, and 69 allergic to other foods (wheat, other legumes, sesame, sea food, and kiwi fruit).
Previous study by Van Der Valk et al. looked at introduction of cashew nut following a negative OFC at 6 months with a successful introduction rate of 43.3% [5]. Our study found a combined total of successful and partial introduction rate of 82% for all challenge nuts.
There are some limitations to our study. It is a retrospective study which relied on the documentation of the treating physician. We also note the majority of patients had negative or low positive SPT which is not representative of patients with true tree nut allergy. The families prepared the tree nut biscuit as per our guidelines though this is not standardized with all tested tree nuts.
Our study reveals that there is a high success rate of passing the mixed tree nut OFC with the majority of families continuing to eat the nuts. Recurrence of tree nut allergy following OFC has not been reported to date.
It will be interesting to follow up children that failed the introduction of the challenge nuts to note if immunologic tolerance is maintained.
To further improve rates of introduction of the tree nuts following negative OFC, we should encourage families to maintain the nuts in the child’s diet. Contact between families and the Immunology Department should be streamlined to allow contemporaneous contact at the time of a possible reaction to the challenge nuts.
Conclusion
Our data show that open mixed tree nut OFC is useful in excluding multiple tree nut allergies in children with low suspicion of clinical allergy. Some families will require more support to maintain the challenge nuts in the child’s diet following a negative OFC.
References
Diagnosing and managing food allergy in children Holloway, Edward; Fox, Adam, Fitzsimons, Roisin. Practitioner; London Vol. 255, Iss. 1741.
Fleischer DM, Conover-Walker MK, Christie L, Burks AW, Wood RA. The natural progression of peanut allergy: resolution and the possibility of recurrence. J Allergy Clin Immunol St Louis. 2003;112(1):183–9. https://doi.org/10.1067/mai.2003.1517.
Australasian Society of Clinical Immunology and Allergy. Skin Prick Testing Working Party. Skin Prick testing for the diagnosis of allergic disease. Updated 2020. Available at https://www.allergy.org.au/ASCIA_HP_SPT_Guide_2020
Thalayasingam M, Noble V, Franzmann A, O’Sullivan M. Outcome of mixed nut biscuit challenge in low risk patients who are on tree nut exclusion diet. Paediatr Allergy Immunol. 2015. https://doi.org/10.1111/pai.12437.
van der Valk JPM, van Wijk RG, Dubois AEJ, de Groot H, de Jong NW. Failure of introduction of cashew nut after a negative oral food challenge test in children. Paediatr Allergy Immunol. 2016. https://doi.org/10.1111/PAI.12591.
Author information
Authors and Affiliations
Contributions
Authors 1, 2, and 3 contributed to the conception and design of the work and acquisition, analysis, and interpretation of data and also contributed to drafting the work and revising it critically for important intellectual content as well as final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Data was obtained from electronic patient records as well as patient charts and used in strictly anonymous form, according to the code of conduct for medical research approved by the hospital’s Medical Ethical Committee (Child and Adolescent Health Service Safety and Quality Committee).
Informed Consent
Signed consent for the challenge was obtained from the parents prior to the challenge. In accordance with the hospital’s guidelines for use of patient’s records, data was obtained from electronic patient records as well as patient charts and used in strictly anonymous form. Verbal consent was obtained from the parent prior to commencing the phone interview.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Appendix
Appendix
Recipe for mixed tree nut biscuit.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Itotoh, B., Roche, I. & Power, C. Following Mixed Tree Nut Biscuit Challenge, Are the Nuts Still Included in the Diet?. SN Compr. Clin. Med. 2, 2208–2213 (2020). https://doi.org/10.1007/s42399-020-00484-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00484-w