Abstract
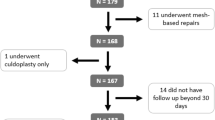
The objective was to present our experience with unilateral sacrospinous ligament hysteropexy performed through an anterior vaginal incision. This is a retrospective cohort study identifying women who underwent unilateral sacrospinous hysteropexy (CPT code 57282) performed through an anterior vaginal wall incision at the University of Rochester between January 2013 and October 2017. Exclusions included follow-up < 6 months, graft augmentation, bilateral sacrospinous ligament suspension, and a posterior approach. Data were compared using a t test, Wilcoxon rank sum test, Chi-square test, or Fisher’s exact test as appropriate; p < 0.05 was considered statistically significant. The cohort (n = 59) consists predominantly of Caucasian (93%), nonsmoking (54%), post-menopausal women (92%), and women with private insurance (59%). Median baseline values were age 63 years (range, 43–80 years), body mass index 26.8 kg/m2 (range, 18.9–43.1 kg/m2), and stage 3 prolapse (range, 2–3). The median operative time was 80 min (IQR 67, 94.5 min) and estimated blood loss 50 mL (IQR 25, 50 mL). Most women (81%) were discharged home on the day of surgery. Subjective recurrence, in any compartment, was 25.4% (n = 15). The recurrence rate was greatest at 44% during the first year (2013), reflecting a learning curve. In years after, recurrence rates averaged 17%. Recurrence was not associated with the surgeon, subject characteristics, obstetric history, or operative factors. Unilateral anterior sacrospinous hysteropexy is an efficient procedure with few complications. It provides a convenient approach for uterus-preservation pelvic organ prolapse repair with a recurrence comparable to anterior sacrospinous ligament vaginal vault suspension.
Similar content being viewed by others
Abbreviations
- (SSLH):
-
Sacrospinous ligament hysteropexy
- (UVP):
-
uterovaginal prolapse
- (US):
-
United States
- (BMI):
-
body mass index
- (EBL):
-
estimated blood loss
- (mins):
-
minutes
- (IQR):
-
intra-quartile range
- (MME):
-
morphine milligram equivalents
- (CI):
-
confidence interval
- (EMR):
-
electronic medical record
- (POPQ):
-
Pelvic Organ Prolapse Quantification
- (PACU):
-
post-anesthesia care unit
References
DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6 Pt 1):1717–24 discussion 24-8.
Madsen AM, Raker C, Sung VW. Trends in hysteropexy and apical support for uterovaginal prolapse in the United States from 2002 to 2012. Female Pelvic Med Reconstr Surg. 2017;23(6):365–71. https://doi.org/10.1097/spv.0000000000000426.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9. https://doi.org/10.1097/SPV.0b013e31827d8667.
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470.e1–6. https://doi.org/10.1016/j.ajog.2013.08.003.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803–13. https://doi.org/10.1007/s00192-013-2171-2.
Bradley S, Gutman RE, Richter LA. Hysteropexy: an option for the repair of pelvic organ prolapse. Curr Urol Rep. 2018;19(2):15. https://doi.org/10.1007/s11934-018-0765-4.
Ridgeway BM. Does prolapse equal hysterectomy? The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. 2015;213(6):802–9. https://doi.org/10.1016/j.ajog.2015.07.035.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–46.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Richardson DA, Scotti RJ, Ostergard DR. Surgical management of uterine prolapse in young women. J Reprod Med. 1989;34(6):388–92.
Dietz V, de Jong J, Huisman M, Schraffordt Koops S, Heintz P, van der Vaart H. The effectiveness of the sacrospinous hysteropexy for the primary treatment of uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1271–6. https://doi.org/10.1007/s00192-007-0336-6.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16. https://doi.org/10.1007/s00192-009-1014-7.
Dietz V, Schraffordt Koops SE, van der Vaart CH. Vaginal surgery for uterine descent; which options do we have? A review of the literature. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(3):349–56. https://doi.org/10.1007/s00192-008-0779-4.
Dietz V, Huisman M, de Jong JM, Heintz PM, van der Vaart CH. Functional outcome after sacrospinous hysteropexy for uterine descensus. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):747–52. https://doi.org/10.1007/s00192-007-0520-8.
Holley RL, Varner RE, Gleason BP, Apffel LA, Scott S. Sexual function after sacrospinous ligament fixation for vaginal vault prolapse. J Reprod Med. 1996;41(5):355–8.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):381–4 discussion 4-5.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ (Clinical research ed). 2015;351:h3717. https://doi.org/10.1136/bmj.h3717.
Schulten SFM, Detollenaere RJ, Stekelenburg J, IntHout J, Kluivers KB, van Eijndhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ (Clinical research ed). 2019;366:l5149. https://doi.org/10.1136/bmj.l5149.
Senturk MB, Guraslan H, Cakmak Y, Ekin M. Bilateral sacrospinous fixation without hysterectomy: 18-month follow-up. J Turk German Gynecol Assoc. 2015;16(2):102–6. https://doi.org/10.5152/jtgga.2015.15220.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8. https://doi.org/10.1007/s00192-014-2564-x.
Shkarupa D, Kubin N, Shapovalova E, Zaytseva A. The resurrection of sacrospinous fixation: unilateral apical sling hysteropexy. Int Urogynecol J. 2020;31(2):351–7. https://doi.org/10.1007/s00192-019-03964-3.
Petruzzelli P, Chiado Fiorio Tin M, Cosma S, Parisi S, Garofalo A, Todros T. Combined sacrospinous hysteropexy and cystopexy using a single anterior incision. Int J Gynaecol Obstet. 2016;135(1):101–6. https://doi.org/10.1016/j.ijgo.2016.03.028.
Winkler HA, Tomeszko JE, Sand PK. Anterior sacrospinous vaginal vault suspension for prolapse. Obstet Gynecol. 2000;95(4):612–5.
Goldberg RP, Tomezsko JE, Winkler HA, Koduri S, Culligan PJ, Sand PK. Anterior or posterior sacrospinous vaginal vault suspension: long-term anatomic and functional evaluation. Obstet Gynecol. 2001;98(2):199–204.
Berger MB, Kolenic GE, Fenner DE, Morgan DM, DeLancey JOL. Structural, functional, and symptomatic differences between women with rectocele versus cystocele and normal support. Am J Obstet Gynecol. 2018;218(5):510.e1–8. https://doi.org/10.1016/j.ajog.2018.01.033.
Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006;195(6):1837–40. https://doi.org/10.1016/j.ajog.2006.06.065.
Chung CP, Miskimins R, Kuehl TJ, Yandell PM, Shull BL. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23(2):223–7. https://doi.org/10.1007/s00192-011-1556-3.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Team RC. R: a language environment for statistical computing. R Foundation for Statistical Computing 2015. https//www.r-project.org/.
Team R. RStudio: integrated development for R. RStudio, Inc., Boston, MA. 2015. http://rstudio.com/.
Barber MD, Neubauer NL, Klein-Olarte V. Can we screen for pelvic organ prolapse without a physical examination in epidemiologic studies? Am J Obstet Gynecol. 2006;195(4):942–8. https://doi.org/10.1016/j.ajog.2006.02.050.
Shkarupa D, Kubin N, Pisarev A, Zaytseva A, Shapovalova E. The hybrid technique of pelvic organ prolapse treatment: apical sling and subfascial colporrhaphy. Int Urogynecol J. 2017;28(9):1407–13. https://doi.org/10.1007/s00192-017-3286-7.
Holley RL, Varner RE, Gleason BP, Apffel LA, Scott S. Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. J Am Coll Surg. 1995;180(4):444–8.
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. Jama. 2014;311(10):1023–34. https://doi.org/10.1001/jama.2014.1719.
Shippert RD. A study of time-dependent operating room fees and how to save $100 000 by using time-saving products. Am J Cosmet Surg. 2005;22(1):25–34. https://doi.org/10.1177/074880680502200104.
Nguyen JK, Hall CD, Bhatia NN. Sacrospinous ligament suspension of the vagina using the Capio suturing device. Female Pelvic Med Reconstr Surg. 2000;6(4):204–9.
Acknowledgments
None.
Funding
No external funding.
Author information
Authors and Affiliations
Contributions
DJ Sanderson: protocol/project development, data collection/analysis, manuscript writing/editing.
J Matloubieh: data collection, manuscript writing/editing.
GM Buchsbaum: protocol/project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of Interest
DJ Sanderson: Consultant with InterPRO Urology. J Maloubieh and GM Buchsbaum have no conflicts of interest to disclose.
Ethical Approval
All research activities performed in this retrospective analysis were in accordance with ethical standards.
Informed Consent
This research was conducted under waived informed consent due, approved by the University of Rochester Research Subjects Review Board, Rochester, NY.
Conference Presentation
Initial results were presented at the Society of Gynecologic Surgeons (SGS) Annual Meeting, Tucson, Arizona, USA, March 31–April 3, 2019.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Brief Summary
Unilateral anterior sacrospinous ligament hysteropexy is a novel technique that is well tolerated with few complications and provides a convenient approach for a single-incision multi-compartment repair of uterovaginal prolapse.
Rights and permissions
About this article
Cite this article
Sanderson, D.J., Matloubieh, J. & Buchsbaum, G.M. Unilateral Anterior Sacrospinous Ligament Hysteropexy: a Single-Center Experience. SN Compr. Clin. Med. 2, 948–955 (2020). https://doi.org/10.1007/s42399-020-00327-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00327-8