Abstract
This study uses nested Cox proportional hazard models to analyze data from five waves (2002, 2005, 2008, 2011, 2014) of the Chinese Longitudinal Healthy Longevity Survey. We found that secular social participation and religious participation both contributed to statistically lower death risk among older respondents. These associations still held after controlling for a wide range of covariates. In particular, secular social participation predicted a greater decrease in death risk and had interactive effects with gender and age-group. Female and young–old adults enjoyed more health benefits from participating in secular social activities than their male or old–old counterparts, respectively. This interactive effect was not observed regarding the impact of religious participation on death hazard.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Research background
Due to reduced fertility and mortality rates, life expectancy has risen steadily in many nations (Murphy 2011), with China’s older citizens having a life expectancy of 76 years in 2015 (Cai and Zhang 2017). In the worldwide profile of population aging, China is witnessing an accelerating pace of senescence. According to the 1% National Population Sample Survey conducted in 2015, total population had reached approximately 1,373,490,000, with the number of older citizens aged 60 and above in China accounting for 16.15%, an increase of 2.89% from 2010 national census data.
Given this increase in the number of older people, questions concerning how to ensure healthy aging have become a shared concern of experts, practitioners, policy-makers, and older people themselves. Addressing these issues is an arduous task that requires cross-sector cooperation and interdisciplinary insight. Both healthy aging and successful aging (Rowe and Kahn 1987, 1997, 2015) not only imply low probability of disease or disease-related disability, and high cognitive and physical functional capacity, but also indicate active engagement with life.
Factors affecting health have been explored thoroughly in the fields of medicine, biology, sociology and psychology. With longer life expectancy predictable globally, old-age health has increasingly become a focus of attention. At present, it is widely believed that health outcomes for older people are influenced by genetics, natural or social environments, and personal or family characteristics (Hernandez and Blazer 2006). Social participation is an important part of personal characteristics and stands out as a key determinant.
1.1 The meaning of social participation
When it comes to the concept of social participation per se, there is no widespread agreement on a definition of the term or what its underlying dimensions are (Levasseur et al. 2010). A number of studies have used alternative phrases that are similar in their implications, like social cohesion (Latham and Clarke 2018), social connectedness (Kim et al. 2015), social engagement (Mendes de Leon 2005), social integration (Lennartsson and Silverstein 2001), social involvement (Badley 2008), social interaction (Croezen et al. 2015), social networks (Hanson et al. 1997), social support (Lyyra and Heikkinen 2006), and social ties (Berkman and Syme 1979), to name several.
Even among those researchers who have used the same term “social participation”, there are different ideas with respect to what the term means. Some scholars have highlighted the individual’s membership in formal or informal organizations or groups (Del Bono et al. 2007; Ellaway and Macintyre 2007; Hsu 2007; Lindström 2005), others have focused more on actual interactive activities and events (Bath and Deeg 2005; Mars et al. 2008), while a few have emphasized resources-sharing and emotion-exchanging (Bukov et al. 2002; Lövdén et al. 2005; Thompson and Whearty 2004).
Given this lack of definitional clarity, we provide a clear definition of “social participation” in the data section.
1.2 Social participation and mortality
The impact of older people’s social participation on their death risk was first discussed decades ago (Berkman and Syme 1979; Seeman et al. 1987). The results of the earlier studies showed that older people who lacked social and community ties were more susceptible to death.
Since then, studies exploring the relationship between the social participation and mortality of older people have abounded and continue to accumulate (Badley 2008; Hanson et al. 1997; Kim et al. 2015; Lennartsson and Silverstein 2001; Lyyra and Heikkinen 2006; Mendes de Leon 2005). Researchers using data from Alameda County in California (Berkman and Syme 1979), Tecumseh County in the US (House et al. 1982), Sweden (Lennartsson and Silverstein 2001), Australia (Ding and Berry 2015) and a number of European countries (Croezen et al. 2015) all found that social participation was associated with reduced death risk.
In East Asian regions, studies from Japan (Ishikawa et al. 2016), South Korea (Kim et al. 2015) and Taiwan (Hsu 2007) have also demonstrated the association of social participation with health benefits. However, there have been few empirical investigations that present statistical findings on how social participation affects mortality among mainland China’s citizens. Wei and Wu (2015) drew upon four waves (2002, 2005, 2008 and 2011) of CLHLS (Chinese Longitudinal Healthy Longevity Survey) data and used principal component analysis to disentangle social participation into cultural entertainment and household activities. Then they applied a Cox proportional hazard model to suggest that cultural entertainment and household activities helped reduce death hazard among China’s older people. Wei and Wu’s longitudinal study is more effective than cross-sectional analysis at establishing solid causal inference, but they excluded religious participation information included in the CLHLS 2002 questionnaire.
Religious participation is a particular sub-type of social participation whose relationship with death risk among China’s old people has been documented by a couple of studies. Zhang (2008) used two waves (1998 and 2000) of CLHLS data and estimated the Cox proportional hazard model, pointing out that religious attendance was significantly associated with lower risk of mortality for the old–old women aged above 80 and for individuals in poor health in China. Another study (Zeng et al. 2011) estimated the Cox semi-parametric proportional hazard model on two waves (2002 and 2005) of CLHLS data, showing that for all respondents aged 65 and over, risk of death was 21% lower among religious participants than among nonparticipants. Another study (Zhu and Lu 2012) also applied Cox proportional hazard model analysis to four waves (1998, 2000, 2002 and 2005) of CLHLS, indicating that the correlation between religious attendance and mortality risk among China’s older old people became statistically insignificant after controlling for a respondent’s baseline health status.
As the information in this section suggests, the association of religious participation with death risk among China’s older adults requires further study, as the existing evidence is insufficient to draw definitive conclusions about this association. Moreover, comparisons of the impact of secular social participation on mortality with that of religious participation is understudied in the empirical research.
1.3 Mechanisms linking social participation to mortality
Why do older people participate in social activities? Both activity theory (Havighurst 1963) and continuity theory (Atchley 1989) believe that older adults, who were inextricably interconnected with others via social, economic, political and cultural life throughout their youth and middle age, will try to maintain this dynamic structure in old age by getting involved in social activities.
Then how can social participation reduce death risk? With respect to social participation in general, sociologist Émile Durkheim crystallized the concept of social integration and its significance in gluing together religious groups or guild members (Berkman et al. 2000). Proper social integration deters deviant behaviors like suicide, maintains social norms and strengthens social solidarity (Kawachi and Kennedy 1997). It is possible that older adults who participate in social activities are more likely to have tighter social networks and stronger social support. For older grandparents who take care of their grandchildren, a sense of satisfaction might result from the continuity of family lineage. Another factor connecting social participation to reduced death risk is that taking part in social activities can bring about behavioral and physiological changes. Social participation encourages a non-sedentary lifestyle involving physical activity and exercise, and this may help sharpen older people’s mind and maintain articulation, and it boosts cardiovascular, neuroendocrine and immune functions (Uchino 2006). As for older people who take part in religious activities, fighting or hurting each other is discouraged, life satisfaction is uplifted even when living conditions are poor, and health-seeking behaviors like seeing a doctor are promoted (Zeng et al. 2011).
To summarize, general social participation and religious activities impact health outcomes via psychological, physiological and behavioral pathways.
1.4 Interactive effects
The impact of social and religious participation on death hazard is not monolithic across populations of older people when socio-demographic characteristics are taken into account. Social participation might be regarded as an approach to empowering socio-economically disadvantaged women and the old–old people, both of which groups may enjoy more benefits from social participation (Zhang et al. 2015). However, with respect to religious participation in China, association with death risk among young–old men was significantly stronger than among old–old men, but no such significant young–old versus old–old differentials in women were found (Zeng et al. 2011). This inconclusive evidence requires further study in the context of China.
2 Contribution to literature and hypotheses
To date, there have been a few studies that have drawn upon longitudinal data from CLHLS to estimate Cox proportional hazard model to investigate how social participation (Wei and Wu 2015) and a particular type of social participation, i.e. religious participation (Zeng et al. 2011; Zhang 2008; Zhu and Lu 2012) affect death risk among China’s older adults. These studies have yielded mixed findings because the relationship between participation and death risk may disappear after controlling for baseline health status (Zhu and Lu 2012) or vary in strength across different subgroups (Zeng et al. 2011).
Therefore, it is important to present a broader picture by comprehensively examining the associations of both social and religious participation with mortality and the interactive effects that socio-demographic characteristics have on such associations.
Building on a literature review and critical reflections outlined here, we will test the following two hypotheses.
Hypothesis 1
Social participation reduces death risk among China’s older citizens.
Hypothesis 2
Gender and age-group differences affect the impact of social participation on death risk.
3 Method and measurements
3.1 Data
The data are from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a reliable nationally representative longitudinal dataset incorporating a large number of China’s older citizens (Zeng et al. 2001). Its baseline survey in 1998 selected half of the counties and cities of 22 Chinese provinces.
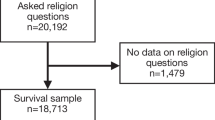
CLHLS did not contain young–old (65–79 years old) respondents until the 2002 wave and removed a question about religious participation from its questionnaire after the 2002 wave. In order to make comparisons between the young–old group and the old–old group, and ones between the non-religious and religious subsamples, we used five waves (2002, 2005, 2008, 2011, 2014) of CLHLS data to study the death risk of respondents newly included in the 2002 wave. We followed these respondents through all five waves or until they died; the number of valid analytic samples was 8069.
3.2 Variables
3.2.1 Mortality
Individual survival time was calculated by taking the time elapsed between the first interview date in 2002 and the exact death date.
Of the 9703 respondents aged 65 and over newly included in the 2002 wave, 2909 died and 1289 were lost to follow-up before the 2005 wave, while 5505 remained alive. Between 2005–2008, 2008–2011 and 2011–2014, various numbers of respondents died (1341 between 2005–2008, 722 between 2008–2011 and 515 between 2011–2014) or were lost (953, 363 and 96, respectively, between the waves) so that only 1515 respondents were still alive for the 2014 wave. The total number of respondents shrank from 9703 in 2002, 5505 in 2005, 3211 in 2008, 2126 in 2011 to finally 1515 in 2014. Respondents who were still alive at the 2014 wave were deemed censored samples. As for respondents lost between each wave, only those lost between the 2005 and 2014 waves were treated as censored samples whose survival day was calculated by calculating the time elapsed between their interview day in 2002 and the final interview day before they were lost. For example, the survival time of a sample lost between 2005 and 2008 was his or her interview day in 2002 subtracted from his or her interview day in 2005. It is noteworthy that this approach, although also adopted by one previous study (Zhu and Lu 2012), is an inaccurate estimate of survival time. Those lost between 2002 and 2005 wave were removed from analysis because we had no way of knowing if they were alive or dead.
3.2.2 Social participation
Respondents were asked at their 2002 wave interview how often they read books, watched TV or listened to the radio, did housework or took care of grandchildren, played cards or mah-jong, took part in social activities, and engaged in religious activities. These six questions were selected as the operationalization of social participation. Wei and Wu (2015) included questions about reading books, watching TV and listening to the radio in their study and we agreed with this approach. We believe these activities represent less active forms of social participation during which older people are taking in and processing social news and information. After factor analysis, two common factors were generated with religious activity alone accounting for the second common factor. However, factor loadings for the other five subjects were undesirable so that it was not appropriate to use factor analysis. Both literature review and factor analysis suggested that religious participation was quite unique. As a result, we divided social participation into “secular social participation” and “religious participation”, both binary variables with complete nonparticipants being coded 0. For all 8069 interviewees, 1438 respondents reported no secular social participation while 6623 had no religious participation.
3.2.3 Covariates
Socio-demographic variables (age-group, gender, ethnicity, place of residence, educational attainment), family background and social ties (marital status, financial condition, living arrangements, filial support, medical availability), lifestyle (exercise, smoking, alcohol consumption), baseline health status (ADL, last-2-year illness record, life satisfaction, self-reported health) are recoded to binary control variables. Therefore, the young–old (50.66%), female (56.72%), Han (94.10%), rural residence (63.75%), illiterate (61.63%), not-in-marriage (61.24%), living alone (12.69%), bad financial condition (70.78%), no filial support (26.51%), medical unavailability (10.50%), no exercise (68.98%), lifelong smoking (20.72%), lifelong drinking (21.94%), poor ADL (22.89%), became a patient in last 2 years (15.01%), low life satisfaction (43.88%), poor self-reported health (52.94%) were reference groups and coded 0.
It should be pointed out that living alone means the respondent lives with no one other than his or her spouse, neither with his or her other relatives nor in a care institution. An older person is believed to have good ADL only if he or she is capable of bathing, dressing, toileting, exercising continence, transferring and self-feeding. Low life satisfaction indicates that the respondent thinks his or her life condition is “very bad” or “bad”, while poor self-reported health indicates that the respondent believes his or her health status is “very bad”, “bad” or “just so-so”.
3.3 Method
We used the Cox proportional hazard model to conduct survival analysis. Specification of the model without interactive variables is as follows:
Survival time referred to survival day, which began on the exact date the respondent was interviewed in 2002 and ended on the exact date when the respondent died. Respondents who died were regarded as failure samples and coded 1, while those still alive at the 2014 wave interview or those lost at or after the 2008 wave were deemed to be censored samples and coded 0.
4 Results
4.1 Survival analysis
Of the total of 8069 respondents, 5147 individuals failed at some point between the 2002 wave and the 2004 wave, while 2922 adults were censored. On average, samples quit on the 2026th day, with the first out on the first day and the last out on the 4463rd day. The median number was on the 1494th day, so the distribution was positively skewed.
The formula for the Kaplan–Meier survival function is as follows:
where K indicates the final end of several periods of time, nx is the number of surviving people at the end of period x, and dx is the number of dead people at the end of period x. The Kaplan–Meier survival function is used to estimate the survival probability.
Figure 1 showed how individuals quit between 2002 and 2014. At the end of this period, there were 1515 individuals who were still alive, so the survival rate was about 18.78%.
4.2 Social participation and death risk
To examine the principal associations of secular social participation and religious participation with death risk, nested Cox proportional models were used with covariates added in, and ultimately with interactive variables included.
Table 1 shows the direction, strength and significance of the impacts of two kinds of social participation on mortality hazard.
Model 1 which only included core independent variables showed that secular social participation and taking part in religious activities significantly reduced death risk by 74% and 16%, respectively. Model 2 in which socio-demographic variables were added, indicated that mortality hazard for older adults aged 80 and over was 314% higher than for their young–old counterparts, while gender did not exert a significant effect.
Model 3 contained all the covariates and we can see that the old–old group was still 209% more susceptible to mortality, while the male subgroup had 25% higher death risk than the female. As for family background and social ties, respondents who remained in a marriage tended to have a death hazard 32% lower, while respondents who lived with relatives other than a spouse or stayed in an institution showed mortality risk that was 12% higher. Regarding lifestyle, predictably doing exercise on a regular basis for a period of years brought health benefits for the older adults: a decrease in death risk of 7%. However, lifelong smoking and alcohol consumption did not have a salient impact. When it came to baseline health status, the result showed that older people with better ADL in 2002 had a significant 40% lower death hazard, while those who rated their health more positively also enjoyed lower mortality risk by 23%. Models 1–3 showed that after covariates were incorporated, the impact of secular social participation and religious participation on death risk, although they declined on strength, remained significant and the direction did not change. Therefore, Hypothesis 1 can be accepted.
Model 4 was constructed to test interactive effects; we found that women enjoyed more health benefits than men from participating in secular social activities. The death risk for men who reported secular social participation was 16% higher than that of women who participated in secular social activities. However, for the effect of religious activities, there was no difference between men and women. A look at different age groups revealed another disparity. Model 4 showed that young–old respondents gained more health advantages from participating in secular social activities than did their old–old counterparts, with the latter reporting a 44% higher mortality hazard. Engaging in religious activities, however, did not cause statistical death risk gap between the young–old and the old–old. Therefore, Hypothesis 2 can be partially accepted.
5 Conclusion and discussion
Like previous studies (Berkman and Syme 1979; Croezen et al. 2015; Ding and Berry 2015; House et al. 1982; Hsu 2007; Lennartsson and Silverstein 2001; Lu et al. 2017), our findings suggest that social participation is associated with lower levels of death risk for older citizens of mainland China. Secular social participation and religious participation predicted declines in mortality hazard by 56% and 16%, respectively. Religious participation, as previous studies (Zeng et al. 2011; Zhang 2008; Zhu and Lu 2012) have indicated, does exert a certain influence on death hazard, although the impact is lower in strength compared with the influence secular social participation can bring.
The impact of secular social activities on death risk varied when gender or age-group was taken into consideration. Our examination of interactive effects showed that female respondents or young–old respondents tended to gain statistically more health benefits from participating in secular social activities than did male or old–old respondents, respectively. These findings were similar to the results from previous studies (Latham and Clarke 2018; Zhang et al. 2015). Participation in religious activities, however, did not cause gaps in mortality risk between subgroups.
This study has some limitations. Respondents who were reported lost at or after the 2008 wave were included as censored samples, because at least they survived from the initial 2002 wave through at least one more wave. In this case, their survival time could be calculated by comparing the interview date in 2002 and the date they were interviewed at previous wave. This approach can cause bias when inferring survival time. As for the core independent variables, on the basis of our literature review and factor analysis, we divided social participation into (a) secular social participation which included items, the use of which is questioned by some researchers, like reading books, watching TV and listening to the radio and (b) religious participation. In the context of China, older people who participate in religious activities may not have the same amount of religious commitment as Western church-goers have. In other words, religious activities might be secularized and integrated in quotidian routine social practice for Chinese older citizens, who are simply looking for good luck. Although religious participation predicted less health benefits than secular social participation, the line between these two kinds of activities may be blurry. Therefore, despite the fact that this division is supported by factor analysis and the literature review, its practical implications should be interpreted with caution. Also, the operationalization of covariates still has room for refinement. Finally, all of the values for variables processed are from the 2002 wave, which means information from the later four waves was not used at all. As a result, the influence of variables that can change over time like marital status (maybe the respondent suffered from bereavement) or changes in health status may skew the results.
Future study should take into consideration more life events information of older citizens and use refined statistical methods to present more robust results.
References
Atchley, R. C. (1989). A continuity theory of normal aging. The Gerontologist, 29(2), 183–190.
Badley, E. M. (2008). Enhancing the conceptual clarity of the activity and participation components of the International Classification of Functioning, Disability, and Health. Social Science and Medicine, 66(11), 2335–2345.
Bath, P. A., & Deeg, D. (2005). Social engagement and health outcomes among older people: Introduction to a special section. European Journal of Ageing, 2(1), 24–30.
Berkman, L. F., Glass, T., Brissette, I., & Seeman, T. E. (2000). From social integration to health: Durkheim in the new millennium. Social Science and Medicine, 51(6), 843–857.
Berkman, L. F., & Syme, S. L. (1979). Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology, 109(2), 186–204.
Bukov, A., Maas, I., & Lampert, T. (2002). Social participation in very old age: Cross-sectional and longitudinal findings from BASE. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57(6), P510–P517.
Cai, F., & Zhang, G. (2017). The determinants of life expectancy—A case of four largest cities in China. ASBBS Proceedings, 24(1), 121.
Croezen, S., Avendano, M., Burdorf, A., & Van Lenthe, F. (2015). Social participation and depression in old age: A fixed-effects analysis in 10 European countries. American Journal of Epidemiology, 182(2), 168–176.
Del Bono, E., Sala, E., Hancock, R., Gunnell, C., & Parisi, L. (2007). Gender, older people and social exclusion: A gendered review and secondary analysis of the data (No. 2007-13). ISER Working Paper Series.
Ding, N., & Berry, H. L. (2015). One-year reciprocal relationship between community participation and mental wellbeing in Australia: A panel analysis. Social Science & Medicine, 128(C), 246–254.
Ellaway, A., & Macintyre, S. (2007). Is social participation associated with cardiovascular disease risk factors? Social Science and Medicine, 64(7), 1384–1391.
Hanson, B. S., Ostergren, P., & Elmstahl, S. (1997). Reliability and validity assessments of measures of social network, social support and control: Results from the Malmo Shoulder and Neck Study. Scandinavian Journal of Public Health, 25(4), 249–257.
Havighurst, R. J. (1963). Successful Aging. Process of Aging: Social and Psychological Perspectives, 1, 299–320.
Hernandez, L. M., & Blazer, D. G. (2006). The impact of social and cultural environment on health. In Genes behavior, and the social environment: Moving beyond the nature/nurture debate (pp. 25–43). Washington, DC: The National Academies Press.
House, S., Robbins, C., & Metzner, H. L. (1982). The association of social relationships and activities with mortality: Prospective evidence from the Tecumseh community health study. American Journal of Epidemiology, 116(1), 123–140.
Hsu, H. (2007). Does social participation by the elderly reduce mortality and cognitive impairment. Aging & Mental Health, 11(6), 699–707.
Ishikawa, Y., Kondo, N., Kondo, K., Saito, T., Hayashi, H., & Kawachi, I. (2016). Social participation and mortality: Does social position in civic groups matter? BMC Public Health, 16(1), 394.
Kawachi, I., & Kennedy, B. P. (1997). Socioeconomic determinants of health: Health and social cohesion: Why care about income inequality? BMJ, 314(7086), 1037.
Kim, H., Hong, S., & Kim, M. (2015). Living arrangement, social connectedness, and life satisfaction among Korean older adults with physical disabilities: The results from the National Survey on Persons with Disabilities. Journal of Developmental and Physical Disabilities, 27(3), 307–321.
Latham, K., & Clarke, P. J. (2018). Neighborhood disorder, perceived social cohesion, and social participation among older Americans: Findings from the National Health & Aging Trends Study. Journal of Aging and Health, 30(1), 3–26.
Lennartsson, C., & Silverstein, M. (2001). Does engagement with life enhance survival of elderly people in Sweden? The role of social and leisure activities. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 56(6), S335–S342.
Levasseur, M., Richard, L., Gauvin, L., & Raymond, E. (2010). Inventory and analysis of definitions of social participation found in the aging literature: Proposed taxonomy of social activities. Social Science and Medicine, 71(12), 2141–2149.
Lindström, M. (2005). Ethnic differences in social participation and social capital in Malmö, Sweden: A population-based study. Social Science and Medicine, 60(7), 1527–1546.
Lövdén, M., Ghisletta, P., & Lindenberger, U. (2005). Social participation attenuates decline in perceptual speed in old and very old age. Psychology and Aging, 20(3), 423.
Lu, J. H., Li, Y., & Zheng, B. (2017). The relationship between self-reported health and social participation of Chinese elderly: Evidence from CLHLS Survey. Population Research, 41(1), 15–26.
Lyyra, T. M., & Heikkinen, R. L. (2006). Perceived social support and mortality in older people. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 61(3), S147–S152.
Mars, G. M., Kempen, G. I., Mesters, I., Proot, I. M., & van Eijk, J. T. M. (2008). Characteristics of social participation as defined by older adults with a chronic physical illness. Disability and Rehabilitation, 30(17), 1298–1308.
Mendes de Leon, C. F. (2005). Social engagement and successful aging. European Journal of Ageing, 2(1), 64–66.
Murphy, M. (2011). Long-term effects of the demographic transition on family and kinship networks in Britain. Population and Development Review, 37(s1), 55–80.
Rowe, J. W., & Kahn, R. L. (1987). Human ageing: Usual and successful. Science, 237(4811), 143–149.
Rowe, J. W., & Kahn, R. L. (1997). Successful aging. Gerontologist, 37(4), 433–440.
Rowe, J. W., & Kahn, R. L. (2015). Successful aging 2.0: Conceptual expansions for the 21st century. Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 70(4), 593–596.
Seeman, T. E., Kaplan, G. A., Knudsen, L., Cohen, R. D., & Guralnik, M. (1987). Social network ties and mortality among the elderly in the Alameda County Study. American Journal of Epidemiology, 126(4), 714–723.
Thompson, E. H., Jr., & Whearty, P. M. (2004). Older men’s social participation: The importance of masculinity ideology. The Journal of Men’s Studies, 13(1), 5–24.
Uchino, B. N. (2006). Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377–387.
Wei, X. P., & Wu, R. J. (2015). The influence of the elderly’s social participation on their death hazard rate in China. South China Population, 30(2), 57–69.
Zeng, Y., Gu, D., & George, L. K. (2011). Association of religious participation with mortality among Chinese old adults. Research on Aging, 33(1), 51–83.
Zeng, Y., Vaupel, J. W., Xiao, Z., Zhang, C., & Liu, Y. (2001). The healthy longevity survey and the active life expectancy of the oldest old in China. Population: An English Selection, 13(1), 95–116.
Zhang, W. (2008). Religious participation and mortality risk among the oldest old in China. Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 63(5), 293–297.
Zhang, W., Feng, Q., Liu, L., & Zhen, Z. (2015). Social engagement and health: Findings from the 2013 Survey of the Shanghai Elderly Life and Opinion. International Journal of Aging and Human Development, 80(4), 332–356.
Zhu, H., & Lu, J. H. (2012). Impact of religious attendance on mortality risk of China’s oldest old. Population Research, 36(1), 83–92.
Funding
This study is funded by the China Natural Science Foundation (Grant 71490732)—Healthy Aging: basic scientific research on elderly population health and effective interventions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wu, J., Li, J. The impact of social participation on older people’s death risk: an analysis from CLHLS. China popul. dev. stud. 2, 173–185 (2018). https://doi.org/10.1007/s42379-018-0008-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42379-018-0008-x