Abstract
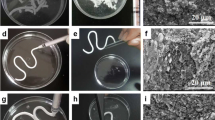
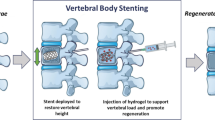
Polymethyl methacrylate (PMMA) bone cement is used in augmenting and stabilizing fractured vertebral bodies through percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP). However, applications of PMMA bone cement are limited by the high elasticity modulus of PMMA, its low biodegradability, and its limited ability to regenerate bone. To improve PMMA bioactivity and biodegradability and to modify its elasticity modulus, we mixed PMMA bone cement with oxidized hyaluronic acid and carboxymethyl chitosan in situ cross-linking hydrogel loaded with bone morphogenetic protein-2 (BMP-2) to achieve novel hybrid cement. These fabricated PMMA–hydrogel hybrid cements exhibited lower setting temperatures, a lower elasticity modulus, and better biodegradability and biocompatibility than that of pure PMMA cement, while retaining acceptable setting times, mechanical strength, and injectability. In addition, we detected release of BMP-2 from the PMMA–hydrogel hybrid cements, significantly enhancing in vitro osteogenesis of bone marrow mesenchymal stem cells by up-regulating the gene expression of Runx2, Col1, and OPN. Use of PMMA–hydrogel hybrid cements loaded with BMP-2 on rabbit femoral condyle bone-defect models revealed their biodegradability and enhanced bone formation. Our study demonstrated the favorable mechanical properties, biocompatibility, and biodegradability of fabricated PMMA–hydrogel hybrid cements loaded with BMP-2, as well as their ability to improve osteogenesis, making them a promising material for use in PKP and PVP.
Graphic abstract








Similar content being viewed by others
References
Lou S, Shi X, Zhang X et al (2019) Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. Osteoporos Int 30(12):2369–2380. https://doi.org/10.1007/s00198-019-05101-8
Chang X, Lv YF, Chen B et al (2015) Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop 39(3):491–500. https://doi.org/10.1007/s00264-014-2525-5
Sun X, Liu X, Wang J et al (2020) The effect of early limited activity after bipedicular percutaneous vertebroplasty to treat acute painful osteoporotic vertebral compression fractures. Pain Phys 23(1):E31-E40
Melton LJ (1997) Epidemiology of spinal osteoporosis. Spine 22(24 Suppl):2s–11s. https://doi.org/10.1097/00007632-199712151-00002
Felsenberg D, Silman AJ, Lunt M et al (2002) Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 17(4):716–724. https://doi.org/10.1359/jbmr.2002.17.4.716
Sun X, Wu Z, He D et al (2019) Bioactive injectable polymethylmethacrylate/silicate bioceramic hybrid cements for percutaneous vertebroplasty and kyphoplasty. J Mech Behav Biomed Mater 96:125–135. https://doi.org/10.1016/j.jmbbm.2019.04.044
Lu Q, Liu C, Wang D et al (2019) Biomechanical evaluation of calcium phosphate-based nanocomposite versus polymethylmethacrylate cement for percutaneous kyphoplasty. Spine J 19(11):1871–1884. https://doi.org/10.1016/j.spinee.2019.06.007
Cui X, Huang C, Zhang M, et al. (2017) Enhanced osteointegration of poly(methylmethacrylate) bone cements by incorporating strontium-containing borate bioactive glass. J R Soc Interf 14(131):20161057. https://doi.org/10.1098/rsif.2016.1057
Khandaker M, Vaughan MB, Morris TL et al (2014) Effect of additive particles on mechanical, thermal, and cell functioning properties of poly(methyl methacrylate) cement. Int J Nanomed 9:2699–2712. https://doi.org/10.2147/ijn.S61964
Zhang CL, Shen GQ, Zhu KP et al (2016) Biomechanical effects of morphological variations of the cortical wall at the bone-cement interface. J Orthop Surg Res 11(1):72. https://doi.org/10.1186/s13018-016-0405-y
Aghyarian S, Rodriguez LC, Chari J et al (2014) Characterization of a new composite PMMA-HA/Brushite bone cement for spinal augmentation. J Biomater Appl 29(5):688–698. https://doi.org/10.1177/0885328214544770
Goñi I, Rodríguez R, García-Arnáez I et al (2018) Preparation and characterization of injectable PMMA-strontium-substituted bioactive glass bone cement composites. J Biomed Mater Res B Appl Biomater 106(3):1245–1257. https://doi.org/10.1002/jbm.b.33935
Zhang J, Zhou H, Yang K et al (2013) RhBMP-2-loaded calcium silicate/calcium phosphate cement scaffold with hierarchically porous structure for enhanced bone tissue regeneration. Biomaterials 34(37):9381–9392. https://doi.org/10.1016/j.biomaterials.2013.08.059
Li S, Chien S, Brånemark PI (1999) Heat shock-induced necrosis and apoptosis in osteoblasts. J Orthop Res 17(6):891–899. https://doi.org/10.1002/jor.1100170614
Sa Y, Yang F, de Wijn JR et al (2016) Physicochemical properties and mineralization assessment of porous polymethylmethacrylate cement loaded with hydroxyapatite in simulated body fluid. Mater Sci Eng C Mater Biol Appl 61:190–198. https://doi.org/10.1016/j.msec.2015.12.040
Meng B, Qian M, Xia SX et al (2013) Biomechanical characteristics of cement/gelatin mixture for prevention of cement leakage in vertebral augmentation. Eur Spine J 22(10):2249–2255. https://doi.org/10.1007/s00586-013-2886-2
Lin HH, Chang MC, Wang ST et al (2018) The fates of pedicle screws and functional outcomes in a geriatric population following polymethylmethacrylate augmentation fixation for the osteoporotic thoracolumbar and lumbar burst fractures with mean ninety five month follow-up. Int Orthop 42(6):1313–1320. https://doi.org/10.1007/s00264-018-3812-3
Thambi T, Li Y, Lee DS (2017) Injectable hydrogels for sustained release of therapeutic agents. J Contr Release 267:57–66. https://doi.org/10.1016/j.jconrel.2017.08.006
Gorantla S, Waghule T, Rapalli VK et al (2019) Advanced hydrogels based drug delivery systems for ophthalmic delivery. Recent Pat Drug Deliv Formul 13(4):291–300. https://doi.org/10.2174/1872211314666200108094851
Li L, Wang N, Jin X et al (2014) Biodegradable and injectable in situ cross-linking chitosan-hyaluronic acid based hydrogels for postoperative adhesion prevention. Biomaterials 35(12):3903–3917. https://doi.org/10.1016/j.biomaterials.2014.01.050
Chen Z, Zhang Z, Ma X et al (2019) Newly designed human-like collagen to maximize sensitive release of BMP-2 for remarkable repairing of bone defects. Biomolecules 9(9):450. https://doi.org/10.3390/biom9090450
Ryoo HM, Lee MH, Kim YJ (2006) Critical molecular switches involved in BMP-2-induced osteogenic differentiation of mesenchymal cells. Gene 366(1):51–57. https://doi.org/10.1016/j.gene.2005.10.011
Yang J, Zhang K, Zhang S, et al (2015) Preparation of calcium phosphate cement and polymethyl methacrylate for biological composite bone cements. Med Sci Monit 21:1162–1172. https://doi.org/10.12659/msm.893845
Liu Z, Pu F, Huang S et al (2013) Long-circulating Gd2O3:Yb3+, Er3+ up-conversion nanoprobes as high-performance contrast agents for multi-modality imaging. Biomaterials 34(6):1712–1721. https://doi.org/10.1016/j.biomaterials.2012.11.009
Sun X, Ma Z, Zhao X et al (2021) Three-dimensional bioprinting of multicell-laden scaffolds containing bone morphogenic protein-4 for promoting M2 macrophage polarization and accelerating bone defect repair in diabetes mellitus. Bioact Mater 6(3):757–769. https://doi.org/10.1016/j.bioactmat.2020.08.030
Zhang X, Kang T, Liang P et al (2018) Biological activity of an injectable biphasic calcium phosphate/pmma bone cement for induced osteogensis in rabbit model. Macromol Biosci 18(3):1700331. https://doi.org/10.1002/mabi.201700331
Zhu T, Ren H, Li A et al (2017) Novel bioactive glass based injectable bone cement with improved osteoinductivity and its in vivo evaluation. Sci Rep 7(1):3622. https://doi.org/10.1038/s41598-017-03207-9
Galovich LA, Perez-Higueras A, Altonaga JR et al (2011) Biomechanical, histological and histomorphometric analyses of calcium phosphate cement compared to PMMA for vertebral augmentation in a validated animal model. Eur Spine J 20 (Suppl 3):376–382. https://doi.org/10.1007/s00586-011-1905-4
Boger A, Bohner M, Heini P et al (2008) Properties of an injectable low modulus PMMA bone cement for osteoporotic bone. J Biomed Mater Res B Appl Biomater 86(2):474–482. https://doi.org/10.1002/jbm.b.31044
Helgason B, Perilli E, Schileo E et al (2008) Mathematical relationships between bone density and mechanical properties: a literature review. Clin Biomech 23(2):135–146. https://doi.org/10.1016/j.clinbiomech.2007.08.024
Chen L, Tang Y, Zhao K et al (2019) Fabrication of the antibiotic-releasing gelatin/PMMA bone cement. Colloids Surf B Biointerf 183:110448. https://doi.org/10.1016/j.colsurfb.2019.110448
Zhao H, Ni CF, Huang J et al (2014) Effects of bone cement on intervertebral disc degeneration. Exp Ther Med 7(4):963–969. https://doi.org/10.3892/etm.2014.1531
Kim SH, Kang HS, Choi JA et al (2004) Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 45(4):440–445. https://doi.org/10.1080/02841850410005615
Feng Z, Chen L, Hu X et al (2018) Vertebral augmentation can induce early signs of degeneration in the adjacent intervertebral disc: evidence from a rabbit model. Spine 43(20):E1195–E1203. https://doi.org/10.1097/brs.0000000000002666
Lee WS, Sung KH, Jeong HT et al (2006) Risk factors of developing new symptomatic vertebral compression fractures after percutaneous vertebroplasty in osteoporotic patients. Eur Spine J 15(12):1777–1783. https://doi.org/10.1007/s00586-006-0151-7
Wang C, Zhang X, Liu J et al (2019) Percutaneous kyphoplasty: risk factors for recollapse of cemented vertebrae. World Neurosurg 130:e307–e315. https://doi.org/10.1016/j.wneu.2019.06.071
Nazarian A, von Stechow D, Zurakowski D et al (2008) Bone volume fraction explains the variation in strength and stiffness of cancellous bone affected by metastatic cancer and osteoporosis. Calcif Tissue Int 83(6):368–379. https://doi.org/10.1007/s00223-008-9174-x
Chiu R, Smith KE, Ma GK et al (2010) Polymethylmethacrylate particles impair osteoprogenitor viability and expression of osteogenic transcription factors Runx2, osterix, and Dlx5. J Orthop Res 28(5):571–577. https://doi.org/10.1002/jor.21035
Zhu J, Yang S, Cai K et al (2020) Bioactive poly (methyl methacrylate) bone cement for the treatment of osteoporotic vertebral compression fractures. Theranostics 10(14):6544–6560. https://doi.org/10.7150/thno.44428
Dutta SR, Passi D, Singh P et al (2015) Ceramic and non-ceramic hydroxyapatite as a bone graft material: a brief review. Ir J Med Sci 184(1):101–106. https://doi.org/10.1007/s11845-014-1199-8
Wang B, Guo Y, Chen X et al (2018) Nanoparticle-modified chitosan-agarose-gelatin scaffold for sustained release of SDF-1 and BMP-2. Int J Nanomed 13:7395–7408. https://doi.org/10.2147/ijn.S180859
Chen D, Zhao M, Mundy GR (2004) Bone morphogenetic proteins. Growth Factors 22(4):233–241. https://doi.org/10.1080/08977190412331279890
Jung T, Lee JH, Park S et al (2017) Effect of BMP-2 delivery mode on osteogenic differentiation of stem cells. Stem Cells Int 2017:7859184. https://doi.org/10.1155/2017/7859184
Acknowledgements
This work was supported by the National Key R&D Program of China (No. 2018YFA0703000), the National Natural Science Foundation of China (Nos. 82071564, 82072412, and 81772326), the Fundamental Research Program Funding of Ninth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (No. JYZZ070), and Project of Shanghai Science and Technology Commission (No. 19XD1434200/18431903700).
Author information
Authors and Affiliations
Contributions
JWW, HYL, WJJ, KPS, and YKG were involved in conceptualization; XS, XZ, and WJJ helped in data curation; XS, XZ, and XJ contributed to formal analysis; JWW, WJJ, and XS were involved in funding acquisition; JWW, HYL, and WJJ helped in investigation; XS, XZ, XJ, JM, XZL, and HY contributed to methodology; JWW, HYL, and WJJ were involved in project administration; JWW, HYL, and WJJ helped in supervision; JWW, HYL, and WJJ contributed to validation; XS, XZ, XJ, JM, XZL, and HY were involved in writing—original draft; JWW, HYL, WJJ, KPS, YKG, XS, XZ, and XJ helped in writing—review & editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
All animal procedures and the use of animals in our study were approved by Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine Animal Care and Use Committee and complied with the guidelines of the National Institutes of Health Guide for Care and Use of Laboratory Animals (GB14925-2010).
Availability of data and material
The datasets used or analyzed during the current study are available from the corresponding authors on reasonable request.
Additional information
Jinwu Wang, Haiyan Li, and Wenjie Jin have contributed equally to this work and are joint corresponding authors.
Supplementary Information
Below is the link to the electronic supplementary material.
42242_2021_172_MOESM1_ESM.jpg
Supplemental Fig. S1. Live-Dead staining and quantitative analysis. a Dead cells are depicted in red and living cells in green; b percentage of live cells. (n=3 per group; * p<0.05) (JPG 6858 kb)
Rights and permissions
About this article
Cite this article
Sun, X., Zhang, X., Jiao, X. et al. Injectable bioactive polymethyl methacrylate–hydrogel hybrid bone cement loaded with BMP-2 to improve osteogenesis for percutaneous vertebroplasty and kyphoplasty. Bio-des. Manuf. 5, 318–332 (2022). https://doi.org/10.1007/s42242-021-00172-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-021-00172-1