Abstract
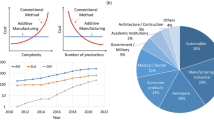
Over millions of years of evolution, nature has created organisms with overwhelming performances due to their unique materials and structures, providing us with valuable inspirations for the development of next-generation biomedical devices. As a promising new technology, 3D printing enables the fabrication of multiscale, multi-material, and multi-functional three-dimensional (3D) biomimetic materials and structures with high precision and great flexibility. The manufacturing challenges of biomedical devices with advanced biomimetic materials and structures for various applications were overcome with the flourishing development of 3D printing technologies. In this paper, the state-of-the-art additive manufacturing of biomimetic materials and structures in the field of biomedical engineering were overviewed. Various kinds of biomedical applications, including implants, lab-on-chip, medicine, microvascular network, and artificial organs and tissues, were respectively discussed. The technical challenges and limitations of biomimetic additive manufacturing in biomedical applications were further investigated, and the potential solutions and intriguing future technological developments of biomimetic 3D printing of biomedical devices were highlighted.












Similar content being viewed by others
References
Poukens J, Laeven P, Beerens M, Nijenhuis G, Sloten JV, Stoelinga P et al (2008) A classification of cranial implants based on the degree of difficulty in computer design and manufacture. Int J Med Rob Comput Assisted Surg 4(1):46–50. https://doi.org/10.1002/rcs.171
Yang Y, Song X, Li X, Chen Z, Zhou C, Zhou Q et al (2018) Recent progress in biomimetic additive manufacturing technology: from materials to functional structures. Adv Mater. https://doi.org/10.1002/adma.201706539
Leung Y-S, Kwok T-H, Li X, Yang Y, Wang CCL, Chen Y (2019) Challenges and status on design and computation for emerging additive manufacturing technologies. J Comput Inf Sci Eng doi 10(1115/1):4041913
Yang Y, Li X, Zheng X, Chen Z, Zhou Q, Chen Y (2018) 3D-printed biomimetic super-hydrophobic structure for microdroplet manipulation and oil/water separation. Adv Mater 30(9):1704912. https://doi.org/10.1002/adma.201704912
Li X, Yang Y, Liu L, Chen Y, Chu M, Sun H et al (2020) 3D-printed cactus-inspired spine structures for highly efficient water collection. Adv Mater Interfaces 7(3):1901752. https://doi.org/10.1002/admi.201901752
Li X, Yang Y, Xie B, Chu M, Sun H, Hao S et al (2019) 3D printing of flexible liquid sensor based on swelling behavior of hydrogel with carbon nanotubes. Adv Mater Technol 4(2):1800476. https://doi.org/10.1002/admt.201800476
Yang Y, Li X, Chu M, Sun H, Jin J, Yu K et al (2019) Electrically assisted 3D printing of nacre-inspired structures with self-sensing capability. Sci Adv 5(4):eaau9490. https://doi.org/10.1126/sciadv.aau9490
Ma PX (2008) Biomimetic materials for tissue engineering. Adv Drug Del Rev 60(2):184–198. https://doi.org/10.1016/j.addr.2007.08.041
Aizenberg J, Fratzl P (2009) Biological and biomimetic materials. Adv Mater 21(4):387–388. https://doi.org/10.1002/adma.200803699
Fisher OZ, Khademhosseini A, Langer R, Peppas NA (2010) Bioinspired materials for controlling stem cell fate. Acc Chem Res 43(3):419–428. https://doi.org/10.1021/ar900226q
Kushner AM, Guan Z (2011) Modular design in natural and biomimetic soft materials. Angew Chem Int Ed 50(39):9026–9057. https://doi.org/10.1002/anie.201006496
Holzapfel BM, Reichert JC, Schantz J-T, Gbureck U, Rackwitz L, Noeth U et al (2013) How smart do biomaterials need to be? A translational science and clinical point of view. Adv Drug Del Rev 65(4):581–603. https://doi.org/10.1016/j.addr.2012.07.009
Li X, Yuan Y, Liu L, Leung Y-S, Chen Y, Guo Y et al (2020) 3D printing of hydroxyapatite/tricalcium phosphate scaffold with hierarchical porous structure for bone regeneration. Bio-Des Manuf 3(1):15–29. https://doi.org/10.1007/s42242-019-00056-5
Huang G, Li F, Zhao X, Ma Y, Li Y, Lin M et al (2017) Functional and biomimetic materials for engineering of the three-dimensional cell microenvironment. Chem Rev 117(20):12764–12850. https://doi.org/10.1021/acs.chemrev.7b00094
Balakrishnan B, Banerjee R (2011) Biopolymer-based hydrogels for cartilage tissue engineering. Chem Rev 111(8):4453–4474. https://doi.org/10.1021/cr100123h
Sands RW, Mooney DJ (2007) Polymers to direct cell fate by controlling the microenvironment. Curr Opin Biotechnol 18(5):448–453. https://doi.org/10.1016/j.copbio.2007.10.004
Edalat F, Sheu I, Manoucheri S, Khademhosseini A (2012) Material strategies for creating artificial cell-instructive niches. Curr Opin Biotechnol 23(5):820–825. https://doi.org/10.1016/j.copbio.2012.05.007
Yi H-G, Lee H, Cho D-W (2017) 3D printing of organs-on-chips. Bioengineering (Basel) 4(1):10. https://doi.org/10.3390/bioengineering4010010
Hoffman AS (2012) Hydrogels for biomedical applications. Adv Drug Del Rev 64:18–23. https://doi.org/10.1016/j.addr.2012.09.010
Caliari SR, Burdick JA (2016) A practical guide to hydrogels for cell culture. Nat Methods 13(5):405–414. https://doi.org/10.1038/nmeth.3839
DeForest CA, Anseth KS (2012) Advances in bioactive hydrogels to probe and direct cell fate. In: Prausnitz JM (eds) Annual review of chemical and biomolecular engineering, vol 3, pp 421–444
Faulk DM, Johnson SA, Zhang L, Badylak SF (2014) Role of the extracellular matrix in whole organ engineering. J Cell Physiol 229(8):984–989. https://doi.org/10.1002/jcp.24532
Aamodt JM, Grainger DW (2016) Extracellular matrix-based biomaterial scaffolds and the host response. Biomaterials 86:68–82. https://doi.org/10.1016/j.biomaterials.2016.02.003
Hong S, Sycks D, Chan HF, Lin S, Lopez GP, Guilak F et al (2015) 3D printing of highly stretchable and tough hydrogels into complex, cellularized structures. Adv Mater 27(27):4035–4040. https://doi.org/10.1002/adma.201501099
Yi H-G, Kang KS, Hong JM, Jang J, Park MN, Jeong YH et al (2016) Effects of electromagnetic field frequencies on chondrocytes in 3D cell-printed composite constructs. J Biomed Mater Res A 104(7):1797–1804. https://doi.org/10.1002/jbm.a.35714
Lozano R, Stevens L, Thompson BC, Gilmore KJ, Gorkin R III, Stewart EM et al (2015) 3D printing of layered brain-like structures using peptide modified gellan gum substrates. Biomaterials 67:264–273. https://doi.org/10.1016/j.biomaterials.2015.07.022
Zander NE, Dong H, Steele J, Grant JT (2014) Metal cation cross-linked nanocellulose hydrogels as tissue engineering substrates. ACS Appl Mater Interfaces 6(21):18502–18510. https://doi.org/10.1021/am506007z
Zhu J, Kaufman LJ (2014) Collagen I self-assembly: revealing the developing structures that generate turbidity. Biophys J 106(8):1822–1831. https://doi.org/10.1016/j.bpj.2014.03.011
Miao Z, Lu Z, Wu H, Liu H, Li M, Lei D et al (2018) Collagen, agarose, alginate, and Matrigel hydrogels as cell substrates for culture of chondrocytes in vitro: a comparative study. J Cell Biochem 119(10):7924–7933. https://doi.org/10.1002/jcb.26411
Xiong R, Chai W, Huang Y (2019) Laser printing-enabled direct creation of cellular heterogeneity in lab-on-a-chip devices. Lab Chip 19(9):1644–1656. https://doi.org/10.1039/c9lc00117d
Martinsen A, Skjakbraek G, Smidsrod O (1989) Alginate as immobilization material. 1. Correlation between chemical and physical-properties of alginate gel beads. Biotechnol Bioeng 33(1):79–89. https://doi.org/10.1002/bit.260330111
Augst AD, Kong HJ, Mooney DJ (2006) Alginate hydrogels as biomaterials. Macromol Biosci 6(8):623–633. https://doi.org/10.1002/mabi.200600069
Freeman I, Kedem A, Cohen S (2008) The effect of sulfation of alginate hydrogels on the specific binding and controlled release of heparin-binding proteins. Biomaterials 29(22):3260–3268. https://doi.org/10.1016/j.biomaterials.2008.04.025
Madl CM, Mehta M, Duda GN, Heilshorn SC, Mooney DJ (2014) Presentation of BMP-2 mimicking peptides in 3D hydrogels directs cell fate commitment in osteoblasts and mesenchymal stem cells. Biomacromolecules 15(2):445–455. https://doi.org/10.1021/bm401726u
Boontheekul T, Kong HJ, Mooney DJ (2005) Controlling alginate gel degradation utilizing partial oxidation and bimodal molecular weight distribution. Biomaterials 26(15):2455–2465. https://doi.org/10.1016/j.biomaterials.2004.06.044
Rebelo R, Fernandes M, Fangueiro R (2017) Biopolymers in medical implants: a brief review. In: Fangueiro R (eds) 3rd international conference on natural fibers: advanced materials for a greener world. ICNF 2017, pp 236–243
Naumenko EA, Guryanov ID, Yendluri R, Lvov YM, Fakhrullin RF (2016) Clay nanotube-biopolymer composite scaffolds for tissue engineering. Nanoscale 8(13):7257–7271. https://doi.org/10.1039/c6nr00641h
Stoppel WL, Ghezzi CE, McNamara SL, Black LD III, Kaplan DL (2015) Clinical applications of naturally derived biopolymer-based scaffolds for regenerative medicine. Ann Biomed Eng 43(3):657–680. https://doi.org/10.1007/s10439-014-1206-2
Jiang Y, Wang Y, Wang H, Zhou L, Gao J, Zhang Y et al (2015) Facile immobilization of enzyme on three dimensionally ordered macroporous silica via a biomimetic coating. New J Chem 39(2):978–984. https://doi.org/10.1039/c4nj01947d
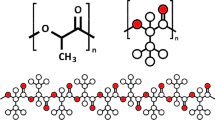
Singh D (2018) Investigations on biomimetic PLA scaffold fabricated by fused deposition modelling [D]
Lih E, Park KW, Chun SY, Kim H, Kwon TG, Joung YK et al (2016) Biomimetic porous PLGA scaffolds incorporating decellularized extracellular matrix for kidney tissue regeneration. ACS Appl Mater Interfaces 8(33):21145–21154. https://doi.org/10.1021/acsami.6b03771
Zhang K, Fu Q, Yoo J, Chen X, Chandra P, Mo X et al (2017) 3D bioprinting of urethra with PCL/PLCL blend and dual autologous cells in fibrin hydrogel: an in vitro evaluation of biomimetic mechanical property and cell growth environment. Acta Biomater 50:154–164. https://doi.org/10.1016/j.actbio.2016.12.008
Li X, Yang Y, Chen Y (2017) Bio-inspired micro-scale texture fabrication based on immersed surface accumulation process. In: World congress on micro and nano manufacturing conference, pp 33–36
Li X, Shan W, Yang Y, Joralmon D, Zhu Y, Chen Y, Yuan Y, Xu H, Rong J, Dai R, Nian Q, Chai Y, Chen Y (2020) Limpet teeth inspired painless microneedles fabricated by magnetic field assisted 3D printing. Adv Funct Mater. https://doi.org/10.1002/adfm.202003725
Price PM, Mahmoud WE, Al-Ghamdi AA, Bronstein LM (2018) Magnetic drug delivery: where the field is going. Front Chem https://doi.org/10.3389/fchem.2018.00619
Ikada Y (2006) Challenges in tissue engineering. J R Soc Interface 3(10):589–601. https://doi.org/10.1098/rsif.2006.0124
Ng YC, Berry JM, Butler M (1996) Optimization of physical parameters for cell attachment and growth on macroporous microcarriers. Biotechnol Bioeng 50(6):627–635. https://doi.org/10.1002/(sici)1097-0290(19960620)50:6%3c627:Aid-bit3%3e3.0.Co;2-m
D. Anh-Vu, R. Smith, T. M. Acri, S. M. Geary, A. K. Salem, 3D printing technologies for 3D scaffold engineering, in: Y. Deng, J. Kuiper, Functional 3d Tissue Engineering Scaffolds: Materials, Technologies, and Applications, 2018, pp. 203-234
Wang X, Jiang M, Zhou ZW, Gou JH, Hui D (2017) 3D printing of polymer matrix composites: a review and prospective. Compos Part B-Eng 110:442–458. https://doi.org/10.1016/j.compositesb.2016.11.034
Zhao P, Gu H, Mi H, Rao C, Fu J, Turng L-S (2018) Fabrication of scaffolds in tissue engineering: a review. Front Mech Eng 13(1):107–119. https://doi.org/10.1007/s11465-018-0496-8
Deville S, Saiz E, Tomsia AP (2006) Freeze casting of hydroxyapatite scaffolds for bone tissue engineering. Biomaterials 27(32):5480–5489. https://doi.org/10.1016/j.biomaterials.2006.06.028
Desimone D, Li W, Roether JA, Schubert DW, Crovace MC, Rodrigues ACM et al (2013) Biosilicate (R)-gelatine bone scaffolds by the foam replica technique: development and characterization. Sci Technol Adv Mater 14(4):045008. https://doi.org/10.1088/1468-6996/14/4/045008
Cai Q, Yang JA, Bei JZ, Wang SG (2002) A novel porous cells scaffold made of polylactide-dextran blend by combining phase-separation and particle-leaching techniques. Biomaterials 23(23):4483–4492. https://doi.org/10.1016/s0142-9612(02)00168-0
Mi H-Y, Salick MR, Jing X, Jacques BR, Crone WC, Peng X-F et al (2013) Characterization of thermoplastic polyurethane/polylactic acid (TPU/PLA) tissue engineering scaffolds fabricated by microcellular injection molding. Mater Sci Eng C-Mater Biol Appl 33(8):4767–4776. https://doi.org/10.1016/j.msec.2013.07.037
Sin D, Miao X, Liu G, Wei F, Chadwick G, Yan C et al (2010) Polyurethane (PU) scaffolds prepared by solvent casting/particulate leaching (SCPL) combined with centrifugation. Mater Sci Eng C Mater Biol Appl 30(1):78–85. https://doi.org/10.1016/j.msec.2009.09.002
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng Part B-Rev 14(1):61–86. https://doi.org/10.1089/teb.2007.0150
Sopyan I, Mel M, Ramesh S, Khalid KA (2007) Porous hydroxyapatite for artificial bone applications. Sci Technol Adv Mater 8(1–2):116–123. https://doi.org/10.1016/j.stam.2006.11.017
Baji A, Wong SC, Srivatsan TS, Njus GO, Mathur G (2006) Processing methodologies for polycaprolactone–hydroxyapatite composites: a review. Mater Manuf Processes 21(2):211–218. https://doi.org/10.1081/amp-200068681
Hwang YK, Jeong U, Cho EC (2008) Production of uniform-sized polymer core–shell microcapsules by coaxial electrospraying. Langmuir 24(6):2446–2451. https://doi.org/10.1021/la703546f
Huang K, Hou J, Gu Z, Wu J (2019) Egg-white-/eggshell-based biomimetic hybrid hydrogels for bone regeneration. ACS Biomater Sci Eng 5(10):5384–5391. https://doi.org/10.1021/acsbiomaterials.9b00990
Feng C, Zhang W, Deng C, Li G, Chang J, Zhang Z et al (2017) 3D printing of lotus root-like biomimetic materials for cell delivery and tissue regeneration. Adv Sci 4(12):1700401. https://doi.org/10.1002/advs.201700401
Zhang M, Lin RC, Wang X, Xue JM, Deng CJ, Feng C et al (2020) 3D printing of Haversian bone-mimicking scaffolds for multicellular delivery in bone regeneration. Sci Adv 6(12):eaaz6725. https://doi.org/10.1126/sciadv.aaz6725
Kim W, Kim M, Kim GH (2018) 3D-printed biomimetic scaffold simulating microfibril muscle structure. Adv Funct Mater 28(26):1800405. https://doi.org/10.1002/adfm.201800405
Melchels FPW, Feijen J, Grijpma DW (2010) A review on stereolithography and its applications in biomedical engineering. Biomaterials 31(24):6121–6130. https://doi.org/10.1016/j.biomaterials.2010.04.050
Koffler J, Zhu W, Qu X, Platoshyn O, Dulin JN, Brock J et al (2019) Biomimetic 3D-printed scaffolds for spinal cord injury repair. Nat Med 25(2):263. https://doi.org/10.1038/s41591-018-0296-z
Li X, Baldacchin T, Song X, Chen Y (2016) Multi-scale additive manufacturing: an investigation on building objects with macro-, micro-and nano-scales features. In: The 11th international conference on micro manufacturing
Li X, Chen Y (2017) Micro-scale feature fabrication using immersed surface accumulation. J Manuf Proces 28:531–540. https://doi.org/10.1016/j.jmapro.2017.04.022
Li X, Chen Y (2018) Multi-scale 3D printing of bioinspired structures with functional surfaces. In: Proceedings of the international symposium on flexible automation. The Institute of Systems, Control and Information Engineers, pp 13–20
Jang J, Yi H-G, Cho D-W (2016) 3D printed tissue models: present and future. ACS Biomater Sci Eng 2(10):1722–1731. https://doi.org/10.1021/acsbiomaterials.6b00129
Seok J, Warren HS, Cuenca AG, Mindrinos MN, Baker HV, Xu W et al (2013) Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci USA 110(9):3507–3512. https://doi.org/10.1073/pnas.1222878110
Huh D, Torisawa Y-S, Hamilton GA, Kim HJ, Ingber DE (2012) Microengineered physiological biomimicry: organs-on-Chips. Lab Chip 12(12):2156–2164. https://doi.org/10.1039/c2lc40089h
Ingber DE, Mow VC, Butler D, Niklason L, Huard J, Mao J et al (2006) Tissue engineering and developmental biology: going biomimetic. Tissue Eng 12(12):3265–3283. https://doi.org/10.1089/ten.2006.12.3265
Hussey GS, Dziki JL, Badylak SF (2018) Extracellular matrix-based materials for regenerative medicine. Nat Rev Mater 3(7):159–173. https://doi.org/10.1038/s41578-018-0023-x
Moroni L, Burdick JA, Highley C, Lee SJ, Morimoto Y, Takeuchi S et al (2018) Biofabrication strategies for 3D in vitro models and regenerative medicine. Nat Rev Mater 3(5):21–37. https://doi.org/10.1038/s41578-018-0006-y
Zhu W, Ma X, Gou M, Mei D, Zhang K, Chen S (2016) 3D printing of functional biomaterials for tissue engineering. Curr Opin Biotechnol 40:103–112. https://doi.org/10.1016/j.copbio.2016.03.014
Stone HA, Stroock AD, Ajdari A (2004) Engineering flows in small devices: microfluidics toward a lab-on-a-chip. Annu Rev Fluid Mech 36:381–411. https://doi.org/10.1146/annurev.fluid.36.050802.122124
Dittrich PS, Manz A (2006) Lab-on-a-chip: microfluidics in drug discovery. Nat Rev Drug Discovery 5(3):210–218. https://doi.org/10.1038/nrd1985
Sosa-Hernandez JE, Villalba-Rodriguez AM, Romero-Castillo KD, Aguilar-Aguila-Isaias MA, Garcia-Reyes IE, Hernandez-Antonio A et al (2018) Organs-on-a-chip module: a review from the development and applications perspective. Micromachines 9(10):536. https://doi.org/10.3390/mi9100536
Oliveira NM, Vilabril S, Oliveira MB, Reis RL, Mano JF (2019) Recent advances on open fluidic systems for biomedical applications: a review. Mater Sci Eng C Mater Biol Appl 97:851–863. https://doi.org/10.1016/j.msec.2018.12.040
Robinson TF, Cohengould L, Factor SM (1983) Skeletal framework of mammalian heart-muscle: arrangement of inter and pericellular connective-tissue structures. Lab Invest 49(4):482–498
Kim D-H, Lipke EA, Kim P, Cheong R, Thompson S, Delannoy M et al (2010) Nanoscale cues regulate the structure and function of macroscopic cardiac tissue constructs. Proc Natl Acad Sci USA 107(2):565–570. https://doi.org/10.1073/pnas.0906504107
Feng Z-Q, Chu X, Huang N-P, Wang T, Wang Y, Shi X et al (2009) The effect of nanofibrous galactosylated chitosan scaffolds on the formation of rat primary hepatocyte aggregates and the maintenance of liver function. Biomaterials 30(14):2753–2763. https://doi.org/10.1016/j.biomaterials.2009.01.053
De Jaeghere E, De Vlieghere E, Van Hoorick J, Van Vlierberghe S, Wagemans G, Pieters L et al (2018) Heterocellular 3D scaffolds as biomimetic to recapitulate the tumor microenvironment of peritoneal metastases in vitro and in vivo. Biomaterials 158:95–105. https://doi.org/10.1016/j.biomaterials.2017.12.017
Ma X, Qu X, Zhu W, Li Y-S, Yuan S, Zhang H et al (2016) Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proc Natl Acad Sci USA 113(8):2206–2211. https://doi.org/10.1073/pnas.1524510113
Park JY, Ryu H, Lee B, Ha D-H, Ahn M, Kim S et al (2019) Development of a functional airway-on-a-chip by 3D cell printing. Biofabrication 11(1):015002. https://doi.org/10.1088/1758-5090/aae545
Kim BS, Lee J-S, Gao G, Cho D-W (2017) Direct 3D cell-printing of human skin with functional transwell system. Biofabrication 9(2):025034. https://doi.org/10.1088/1758-5090/aa71c8
Bazaz SR, Rouhi O, Raoufi MA et al (2020) 3D printing of inertial microfluidic devices[J]. Sci Rep 10(1):1–14. https://doi.org/10.1038/s41598-020-62569-9
Katseli V, Economou A, Kokkinos C (2020) A novel all-3D-printed cell-on-a-chip device as a useful electroanalytical tool: application to the simultaneous voltammetric determination of caffeine and paracetamol. Talanta 208:120388. https://doi.org/10.1016/j.talanta.2019.120388
Magin CM, Alge DL, Anseth KS (2016) Bio-inspired 3D microenvironments: a new dimension in tissue engineering. Biomed Mater 11(2):022001. https://doi.org/10.1088/1748-6041/11/2/022001
Sharafeldin M, Jones A, Rusling JF (2018) 3D-printed biosensor arrays for medical diagnostics. Micromachines 9(8):394. https://doi.org/10.3390/mi9080394
Sapudom J, Pompe T (2018) Biomimetic tumor microenvironments based on collagen matrices. Biomater Sci 6(8):2009–2024. https://doi.org/10.1039/c8bm00303c
Gill EL, Li X, Birch MA, Huang YYS (2018) Multi-length scale bioprinting towards simulating microenvironmental cues. Bio-Des Manuf 1(2):77–88. https://doi.org/10.1007/s42242-018-0014-1
Gladman AS, Matsumoto EA, Nuzzo RG, Mahadevan L, Lewis JA (2016) Biomimetic 4D printing. Nat Mater 15(4):413. https://doi.org/10.1038/nmat4544
Gao B, Yang Q, Zhao X, Jin G, Ma Y, Xu F (2016) 4D bioprinting for biomedical applications. Trends Biotechnol 34(9):746–756. https://doi.org/10.1016/j.tibtech.2016.03.004
Trenfield SJ, Awad A, Goyanes A, Gaisford S, Basit AW (2018) 3D printing pharmaceuticals: drug development to frontline care. Trends Pharmacol Sci 39(5):440–451. https://doi.org/10.1016/j.tips.2018.02.006
Awad A, Trenfield SJ, Gaisford S, Basit AW (2018) 3D printed medicines: a new branch of digital healthcare. Int J Pharm 548(1):586–596. https://doi.org/10.1016/j.ijpharm.2018.07.024
Collins FS, Varmus H (2015) A new initiative on precision medicine. New Engl J Med 372(9):793–795. https://doi.org/10.1056/NEJMp1500523
Bittner SM, Guo JL, Mikos AG (2018) Spatiotemporal control of growth factors in three-dimensional printed scaffolds. Bioprinting (Amsterdam, Netherlands) 12:e00032. https://doi.org/10.1016/j.bprint.2018.e00032
Gao G, Cui X (2016) Three-dimensional bioprinting in tissue engineering and regenerative medicine. Biotech Lett 38(2):203–211. https://doi.org/10.1007/s10529-015-1975-1
Ozbolat IT, Hospodiuk M (2016) Current advances and future perspectives in extrusion-based bioprinting. Biomaterials 76:321–343. https://doi.org/10.1016/j.biomaterials.2015.10.076
Ceylan H, Yasa IC, Yasa O, Tabak AF, Giltinan J, Sitti M (2019) 3D-printed biodegradable microswimmer for theranostic cargo delivery and release. ACS Nano 13(3):3353–3362. https://doi.org/10.1021/acsnano.8b09233
Zhu W, Li J, Leong YJ, Rozen I, Qu X, Dong R et al (2015) 3D-printed artificial microfish. Adv Mater 27(30):4411–4417. https://doi.org/10.1002/adma.201501372
Wang XP, Chen XZ, Alcantara CCJ, Sevim S, Hoop M, Terzopoulou A et al (2019) MOFBOTS: metal-organic-framework-based biomedical microrobots. Adv Mater. https://doi.org/10.1002/adma.201901592
Oblom H, Zhang JX, Pimparade M, Speer I, Preis M, Repka M et al (2019) 3D-printed isoniazid tablets for the treatment and prevention of tuberculosis personalized dosing and drug release. Aaps Pharmscitech 20(2):52. https://doi.org/10.1208/s12249-018-1233-7
Khaled SA, Alexander MR, Irvine DJ, Wildman RD, Wallace MJ, Sharpe S et al (2018) Extrusion 3D printing of paracetamol tablets from a single formulation with tunable release profiles through control of tablet geometry. AAPS PharmSciTech 19(8):3403–3413. https://doi.org/10.1208/s12249-018-1107-z
Wang YZ, Miao Y, Zhang JL, Wu JP, Kirk TB, Xu JK et al (2018) Three-dimensional printing of shape memory hydrogels with internal structure for drug delivery. Mater Sci Eng C-Mater Biol Appl 84:44–51. https://doi.org/10.1016/j.msec.2017.11.025
Clark EA, Alexander MR, Irvine DJ, Roberts CJ, Wallacec MJ, Sharpe S et al (2017) 3D printing of tablets using inkjet with UV photoinitiation. Int J Pharm 529(1–2):523–530. https://doi.org/10.1016/j.ijpharm.2017.06.085
Awad A, Fina F, Trenfield SJ, Patel P, Goyanes A, Gaisford S et al (2019) 3D printed pellets (miniprintlets): a novel, multi-drug, controlled release platform technology. Pharmaceutics 11(4):148. https://doi.org/10.3390/pharmaceutics11040148
Richbourg NR, Peppas NA, Sikavitsas VI (2019) Tuning the biomimetic behavior of scaffolds for regenerative medicine through surface modifications. J Tissue Eng Regener Med 13(8):1275–1293. https://doi.org/10.1002/term.2859
Bloomquist CJ, Mecham MB, Paradzinsky MD, Janusziewicz R, Warner SB, Luft JC et al (2018) Controlling release from 3D printed medical devices using CLIP and drug-loaded liquid resins. J Control Rel 278:9–23. https://doi.org/10.1016/j.jconrel.2018.03.026
Lee J, Lee S-H, Lee B-K, Park S-H, Cho Y-S, Park Y (2018) Fabrication of microchannels and evaluation of guided vascularization in biomimetic hydrogels. Tissue Eng Regener Med 15(4):403–413. https://doi.org/10.1007/s13770-018-0130-1
Hall H (2007) Modified fibrin hydrogel matrices: both, 3D-scaffolds and local and controlled release systems to stimulate angiogenesis. Curr Pharm Des 13(35):3597–3607. https://doi.org/10.2174/138161207782794158
Suzuki M, Sawa T, Takahashi T, Aoyagi S, IEEE (2015) Ultrafine three-dimensional (3D) laser lithographic fabrication of microneedle and its application to painless insertion and blood sampling inspired by mosquito. In: 2015 IEEE/RSJ international conference on intelligent robots and systems, pp 2748–2753
Liaw C-Y, Guvendiren M (2017) Current and emerging applications of 3D printing in medicine. Biofabrication 9(2):024102. https://doi.org/10.1088/1758-5090/aa7279
Goyanes A, Buanz ABM, Basit AW, Gaisford S (2014) Fused-filament 3D printing (3DP) for fabrication of tablets. Int J Pharm 476(1–2):88–92. https://doi.org/10.1016/j.ijpharm.2014.09.044
Skowyra J, Pietrzak K, Alhnan MA (2015) Fabrication of extended-release patient-tailored prednisolone tablets via fused deposition modelling (FDM) 3D printing. Eur J Pharm Sci 68:11–17. https://doi.org/10.1016/j.ejps.2014.11.009
Sandler N, Salmela I, Fallarero A, Rosling A, Khajeheian M, Kolakovic R et al (2014) Towards fabrication of 3D printed medical devices to prevent biofilm formation. Int J Pharm 459(1–2):62–64. https://doi.org/10.1016/j.ijpharm.2013.11.001
Weisman JA, Nicholson JC, Tappa K, Jammalamadaka U, Wilson CG, Mills DK (2015) Antibiotic and chemotherapeutic enhanced three-dimensional printer filaments and constructs for biomedical applications. Int J Nanomed 10:357–370. https://doi.org/10.2147/ijn.S74811
Moulton SE, Wallace GG (2014) 3-dimensional (3D) fabricated polymer based drug delivery systems. J Controll Release 193:27–34. https://doi.org/10.1016/j.jconrel.2014.07.005
Postiglione G, Alberini M, Leigh S, Levi M, Turri S (2017) Effect of 3D-printed microvascular network design on the self-healing behavior of cross-linked polymers. ACS Appl Mater Interfaces 9(16):14371–14378. https://doi.org/10.1021/acsami.7b01830
Karam GN (2005) Biomechanical model of the xylem vessels in vascular plants. Ann Bot 95(7):1179–1186. https://doi.org/10.1093/aob/mci130
Knight C (1981) Pressure component construction… design and materials application. Taylor and Francis, London
Bader MG, Smith W, Isham AB, Rolston J (1990) Delaware composites design encyclopedia. vol. 3: processing and fabrication technology. Technomic Publishing Company, Lancaster, PA (1990)
Shevchenko YN, Merzlyakov VA, Galishin AZ, Novikov SV, Los AO, Yukhimets PS (1993) Determination of the limiting stress-strain state of helically corrugated pipes. Strength Mater 25(7):507–511. https://doi.org/10.1007/bf00775128
Hoballah JJ (2000) Vascular reconstructions: anatomy, exposures and techniques. Springer, Berlin
Lei D, Yang Y, Liu Z, Yang B, Gong W, Chen S et al (2019) 3D printing of biomimetic vasculature for tissue regeneration. Mater Horizons 6(6):1197–1206. https://doi.org/10.1039/c9mh00174c
Dean LM, Krull BP, Li KR, Fedonina YI, White SR, Sottos NR (2018) Enhanced mixing of microvascular self-healing reagents using segmented gas-liquid flow. ACS Appl Mater Interfaces 10(38):32659–32667. https://doi.org/10.1021/acsami.8b09966
Kim S-R, Getachew BA, Kim J-H (2017) Toward microvascular network-embedded self-healing membranes. J Membr Sci 531:94–102. https://doi.org/10.1016/j.memsci.2017.02.038
Yu F, Choudhury D (2019) Microfluidic bioprinting for organ-on-a-chip models. Drug Discov Today 24(6):1248–1257. https://doi.org/10.1016/j.drudis.2019.03.025
Fedorovich NE, Alblas J, de Wijn JR, Hennink WE, Verbout AJ, Dhert WJA (2007) Hydrogels as extracellular matrices for skeletal tissue engineering: state-of-the-art and novel application in organ printing. Tissue Eng 13(8):1905–1925. https://doi.org/10.1089/ten.2006.0175
Norotte C, Marga FS, Niklason LE, Forgacs G (2009) Scaffold-free vascular tissue engineering using bioprinting. Biomaterials 30(30):5910–5917. https://doi.org/10.1016/j.biomaterials.2009.06.034
Kinstlinger IS, Miller JS (2016) 3D-printed fluidic networks as vasculature for engineered tissue. Lab Chip 16(11):2025–2043. https://doi.org/10.1039/c6lc00193a
Murphy SV, Atala A (2014) 3D bioprinting of tissues and organs. Nat Biotechnol 32(8):773–785. https://doi.org/10.1038/nbt.2958
Knowlton S, Onal S, Yu CH, Zhao JJ, Tasoglu S (2015) Bioprinting for cancer research. Trends Biotechnol 33(9):504–513. https://doi.org/10.1016/j.tibtech.2015.06.007
Ho CMB, Sum Huan N, Li KHH, Yoon Y-J (2015) 3D printed microfluidics for biological applications. Lab Chip 15(18):3627–3637. https://doi.org/10.1039/c5lc00685f
Wu W, DeConinck A, Lewis JA (2011) Omnidirectional printing of 3D microvascular networks. Adv Mater 23(24):H178–H183. https://doi.org/10.1002/adma.201004625
Bhattacharjee T, Zehnder SM, Rowe KG, Jain S, Nixon RM, Sawyer WG et al (2015) Writing in the granular gel medium. Sci Adv 1(8):e1500655. https://doi.org/10.1126/sciadv.1500655
Bertassoni LE, Cecconi M, Manoharan V, Nikkhah M, Hjortnaes J, Cristino AL et al (2014) Hydrogel bioprinted microchannel networks for vascularization of tissue engineering constructs. Lab Chip 14(13):2202–2211. https://doi.org/10.1039/c4lc00030g
Gao G, Kim H, Kim BS, Kong JS, Lee JY, Park BW et al (2019) Tissue-engineering of vascular grafts containing endothelium and smooth-muscle using triple-coaxial cell printing. Appl Phys Rev 6(4):041402. https://doi.org/10.1063/1.5099306
Grigoryan B, Paulsen SJ, Corbett DC, Sazer DW, Fortin CL, Zaita AJ et al (2019) BIOMEDICINE Multivascular networks and functional intravascular topologies within biocompatible hydrogels. Science 364(6439):458. https://doi.org/10.1126/science.aav9750
Kim SH, Yeon YK, Lee JM, Chao JR, Lee YJ, Seo YB et al (2018) Precisely printable and biocompatible silk fibroin bioink for digital light processing 3D printing. Nat Commun. https://doi.org/10.1038/s41467-018-03759-y
Datta P, Ayan B, Ozbolat IT (2017) Bioprinting for vascular and vascularized tissue biofabrication. Acta Biomater 51:1–20. https://doi.org/10.1016/j.actbio.2017.01.035
Li X, Mao H, Pan Y, Chen Y (2019) Mask video projection-based stereolithography with continuous resin flow. J Manuf Sci Eng Trans ASME 141(8):081007. https://doi.org/10.1115/1.4043765
Chen Y, Mao H, Li X (2016) Mask video projection based stereolithography with continuous resin flow. U.S. Patent 10,308,007[P]. 2019-6-4
Chen Y, Li X (2018) Surface projection tool for multi-axis additive manufacturing. U.S. Patent Application 15/868,891[P]. 2018-7-12
Chiu YC, Shen YF, Lee AKX, Lin SH, Wu YC, Chen YW (2019) 3D printing of amino resin-based photosensitive materials on multi-parameter optimization design for vascular engineering applications. Polymers 11(9):1394. https://doi.org/10.3390/polym11091394
Zhang Z, Wang B, Hui D, Qiu J, Wang S (2017) 3D bioprinting of soft materials-based regenerative vascular structures and tissues. Compos Part B Eng 123:279–291. https://doi.org/10.1016/j.compositesb.2017.05.011
Hospodiuk M, Dey M, Sosnoski D, Ozbolat IT (2017) The bioink: a comprehensive review on bioprintable materials. Biotechnol Adv 35(2):217–239. https://doi.org/10.1016/j.biotechadv.2016.12.006
Gungor-Ozkerim PS, Inci I, Zhang YS, Khademhosseini A, Dokmeci MR (2018) Bioinks for 3D bioprinting: an overview. Biomater Sci 6(5):915–946. https://doi.org/10.1039/c7bm00765e
Burdick JA, Prestwich GD (2011) Hyaluronic acid hydrogels for biomedical applications. Adv Mater 23(12):H41–H56. https://doi.org/10.1002/adma.201003963
Choudhury D, Tun HW, Wang T, Naing MW (2018) Organ-derived decellularized extracellular matrix: a game changer for bioink manufacturing? Trends Biotechnol 36(8):787–805. https://doi.org/10.1016/j.tibtech.2018.03.003
Yoo S-S (2015) 3D-printed biological organs: medical potential and patenting opportunity. Expert Opin Ther Pat 25(5):507–511. https://doi.org/10.1517/13543776.2015.1019466
Colla G, Porto LM (2014) Development of artificial blood vessels through tissue engineering. In: BMC proceedings. 8. BioMed Central, P45
Kapalczynska M, Kolenda T, Przybyla W, Zajaczkowska M, Teresiak A, Filas V et al (2018) 2D and 3D cell cultures: a comparison of different types of cancer cell cultures. Arch Med Sci 14(4):910–919. https://doi.org/10.5114/aoms.2016.63743
Park JY, Jang J, Kang H-W (2018) 3D Bioprinting and its application to organ-on-a-chip. Microelectron Eng 200:1–11. https://doi.org/10.1016/j.mee.2018.08.004
Mironov V, Kasyanov V, Drake C, Markwald RR (2008) Organ printing: promises and challenges. Regener Med 3(1):93–103. https://doi.org/10.2217/17460751.3.1.93
Schubert C, van Langeveld MC, Donoso LA (2014) Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol 98(2):159–161. https://doi.org/10.1136/bjophthalmol-2013-304446
Zhao H, Chen Y, Shao L, Xie M, Nie J, Qiu J et al (2018) Airflow-assisted 3D bioprinting of human heterogeneous microspheroidal organoids with microfluidic nozzle. Small 14(39):1802630. https://doi.org/10.1002/smll.201802630
Zhu L, Li Y, Zhang Q, Wang H, Zhu M (2010) Fabrication of monodisperse, large-sized, functional biopolymeric microspheres using a low-cost and facile microfluidic device. Biomed Microdev 12(1):169–177. https://doi.org/10.1007/s10544-009-9373-x
Cai B, Guo F, Zhao L, He R, Chen B, He Z et al (2014) Disk-like hydrogel bead-based immunofluorescence staining toward identification and observation of circulating tumor cells. Microfluid Nanofluid 16(1–2):29–37. https://doi.org/10.1007/s10404-013-1198-5
Kim BS, Gao G, Kim JY, Cho D-W (2019) 3D cell printing of perfusable vascularized human skin equivalent composed of epidermis, dermis, and hypodermis for better structural recapitulation of native skin. Adv Healthc Mater 8(7):1801019. https://doi.org/10.1002/adhm.201801019
Binder KW, Zhao W, Aboushwareb T, Dice D, Atala A, Yoo JJ (2010) In situ bioprinting of the skin for burns. J Am Coll Surg 211(3):S76. https://doi.org/10.1016/j.jamcollsurg.2010.06.198
Lee V, Singh G, Trasatti JP, Bjornsson C, Xu X, Thanh Nga T et al (2014) Design and fabrication of human skin by three-dimensional bioprinting. Tissue Eng Part C-Methods 20(6):473–484. https://doi.org/10.1089/ten.tec.2013.0335
Skardal A, Mack D, Kapetanovic E, Atala A, Jackson JD, Yoo J et al (2012) Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl Med 1(11):792–802. https://doi.org/10.5966/sctm.2012-0088
Cubo N, Garcia M, del Canizo JF, Velasco D, Jorcano JL (2017) 3D bioprinting of functional human skin: production and in vivo analysis. Biofabrication 9(1):015006. https://doi.org/10.1088/1758-5090/9/1/015006
Miriyev A, Stack K, Lipson H (2017) Soft material for soft actuators. Nat Commun 8(1):1–8. https://doi.org/10.1038/s41467-017-00685-3
Isaacson A, Swioklo S, Connon CJ (2018) 3D bioprinting of a corneal stroma equivalent. Exp Eye Res 173:188–193. https://doi.org/10.1016/j.exer.2018.05.010
Adams F, Qiu T, Mark A, Fritz B, Kramer L, Schlager D et al (2017) Soft 3D-printed phantom of the human kidney with collecting system. Ann Biomed Eng 45(4):963–972. https://doi.org/10.1007/s10439-016-1757-5
Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T (2019) 3D printing of personalized thick and perfusable cardiac patches and hearts. Adv Sci 6(11):1900344. https://doi.org/10.1002/advs.201900344
Edri R, Gal I, Noor N, Harel T, Fleischer S, Adadi N et al (2019) Personalized hydrogels for engineering diverse fully autologous tissue implants. Adv Mater 31(1):1803895. https://doi.org/10.1002/adma.201803895
Yang Y, Chen ZY, Song X, Zhang ZF, Zhang J, Shung KK et al (2017) Biomimetic anisotropic reinforcement architectures by electrically assisted nanocomposite 3D printing. Adv Mater 29(11):1605750. https://doi.org/10.1002/adma.201605750
Chen YW, Zhang JM, Liu X, Wang S, Tao J, Huang YL et al (2020) Noninvasive in vivo 3D bioprinting. Sci Adv 6(23):eaba7406. https://doi.org/10.1126/sciadv.aba7406
Seol Y-J, Kang H-W, Lee SJ, Atala A, Yoo JJ (2014) Bioprinting technology and its applications. Eur J Cardiothorac Surg 46(3):342–348. https://doi.org/10.1093/ejcts/ezu148
Zell K, Sperl JI, Vogel MW, Niessner R, Haisch C (2007) Acoustical properties of selected tissue phantom materials for ultrasound imaging. Phys Med Biol 52(20):N475–N484. https://doi.org/10.1088/0031-9155/52/20/n02
Elias H, Bengelsdorf H (1952) The structure of the liver of vertebrates. Cells Tissues Organs 14(4):297–337
Abdel-Misih SRZ, Bloomston M (2010) Liver anatomy. Surg Clin N Am 90(4):643. https://doi.org/10.1016/j.suc.2010.04.017
Yun W, Zhi Yuan L, Wenger AC, Tam KC, Xiaowu T (2018) 3D bioprinting of liver-mimetic construct with alginate/cellulose nanocrystal hybrid bioink. Bioprinting 9:1–6. https://doi.org/10.1016/j.bprint.2017.12.001
Xu F, Kang T, Deng J, Liu J, Chen X, Wang Y et al (2016) Functional nanoparticles activate a decellularized liver scaffold for blood detoxification. Small 12(15):2067–2076. https://doi.org/10.1002/smll.201503320
Villar G, Graham AD, Bayley H (2013) A tissue-like printed material. Science 340(6128):48–52. https://doi.org/10.1126/science.1229495
Gurkan UA, El Assal R, Yildiz SE, Sung Y, Trachtenberg AJ, Kuo WP et al (2014) Engineering anisotropic biomimetic fibrocartilage microenvironment by bioprinting mesenchymal stem cells in nanoliter gel droplets. Mol Pharm 11(7):2151–2159. https://doi.org/10.1021/mp400573g
Moon S, Hasan SK, Song YS, Xu F, Keles HO, Manzur F et al (2010) Layer by layer three-dimensional tissue epitaxy by cell-laden hydrogel droplets. Tissue Eng Part C-Methods 16(1):157–166. https://doi.org/10.1089/ten.tec.2009.0179
Guillotin B, Guillemot F (2011) Cell patterning technologies for organotypic tissue fabrication. Trends Biotechnol 29(4):183–190. https://doi.org/10.1016/j.tibtech.2010.12.008
Ferris CJ, Gilmore KG, Wallace GG, Panhuis MIH (2013) Biofabrication: an overview of the approaches used for printing of living cells. Appl Microbiol Biotechnol 97(10):4243–4258. https://doi.org/10.1007/s00253-013-4853-6
Skardal A, Atala A (2015) Biomaterials for Integration with 3-D bioprinting. Ann Biomed Eng 43(3):730–746. https://doi.org/10.1007/s10439-014-1207-1
Arslan-Yildiz A, El Assal R, Chen P, Guven S, Inci F, Demirci U (2016) Towards artificial tissue models: past, present, and future of 3D bioprinting. Biofabrication 8(1):014103. https://doi.org/10.1088/1758-5090/8/1/014103
Hribar KC, Soman P, Warner J, Chung P, Chen S (2014) Light-assisted direct-write of 3D functional biomaterials. Lab Chip 14(2):268–275. https://doi.org/10.1039/c3lc50634g
Gruene M, Deiwick A, Koch L, Schlie S, Unger C, Hofmann N et al (2011) Laser printing of stem cells for biofabrication of scaffold-free autologous grafts. Tissue Eng Part C-Methods 17(1):79–87. https://doi.org/10.1089/ten.tec.2010.0359
Koch L, Kuhn S, Sorg H, Gruene M, Schlie S, Gaebel R et al (2010) Laser printing of skin cells and human stem cells. Tissue Eng Part C-Methods 16(5):847–854. https://doi.org/10.1089/ten.tec.2009.0397
Malda J, Visser J, Melchels FP, Juengst T, Hennink WE, Dhert WJA et al (2013) 25th anniversary article: engineering hydrogels for biofabrication. Adv Mater 25(36):5011–5028. https://doi.org/10.1002/adma.201302042
Ozbolat IT, Yu Y (2013) Bioprinting toward organ fabrication: challenges and future trends. IEEE Trans Biomed Eng 60(3):691–699. https://doi.org/10.1109/tbme.2013.2243912
Shim J-H, Lee J-S, Kim JY, Cho D-W (2012) Bioprinting of a mechanically enhanced three-dimensional dual cell-laden construct for osteochondral tissue engineering using a multi-head tissue/organ building system. J Micromech Microeng 22(8):085014. https://doi.org/10.1088/0960-1317/22/8/085014
Ringeisen BR, Kim H, Barron JA, Krizman DB, Chrisey DB, Jackman S et al (2004) Laser printing of pluripotent embryonal carcinoma cells. Tissue Eng 10(3–4):483–491. https://doi.org/10.1089/107632704323061843
Derakhshanfar S, Mbeleck R, Xu K, Zhang X, Zhong W, Xing M (2018) 3D bioprinting for biomedical devices and tissue engineering: a review of recent trends and advances. Bioactive Mater 3(2):144–156. https://doi.org/10.1016/j.bioactmat.2017.11.008
Chen Z, Wu Y, Yang Y, Li J, Xie B, Li X et al (2018) Multilayered carbon nanotube yarn based optoacoustic transducer with high energy conversion efficiency for ultrasound application. Nano Energy 46:314–321. https://doi.org/10.1016/j.nanoen.2018.02.006
Zhang J, Yang Y, Zhu B, Li X, Jin J, Chen Z et al (2018) Multifocal point beam forming by a single ultrasonic transducer with 3D printed holograms. Appl Phys Lett 113(24):243502. https://doi.org/10.1063/1.5058079
Xiangjia L, Benshuai X, Jie J, Yang C, Yong C (2018) 3D printing temporary crown and bridge by temperature controlled mask image projection stereolithography. Proc Manuf 26:1023–1033. https://doi.org/10.1016/j.promfg.2018.07.134
Sears NA, Seshadri DR, Dhavalikar PS, Cosgriff-Hernandez E (2016) A review of three-dimensional printing in tissue engineering. Tissue Eng Part B-Rev 22(4):298–310. https://doi.org/10.1089/ten.teb.2015.0464
Shusteff M, Browar AE, Kelly BE, Henriksson J, Weisgraber TH, Panas RM, Fang N, Spadaccini CM (2017) One-step volumetric additive manufacturing of complex polymer structures. Sci Adv 3(12):eaao5496. https://doi.org/10.1126/sciadv.aao5496
Kelly BE, Bhattacharya I, Heidari H, Shusteff M, Spadaccini CM, Taylor HK (2019) Volumetric additive manufacturing via tomographic reconstruction. Science 363(6431):1075–1079. https://doi.org/10.1126/science.aau7114
Castro NJ, O’Brien J, Zhang LG (2015) Integrating biologically inspired nanomaterials and table-top stereolithography for 3D printed biomimetic osteochondral scaffolds. Nanoscale 7(33):14010–14022. https://doi.org/10.1039/c5nr03425f
Cheng CH, Chen YW, Lee AKX, Yao CH, Shie MY (2019) Development of mussel-inspired 3D-printed poly(lactic acid) scaffold grafted with bone morphogenetic protein-2 for stimulating osteogenesis. J Mater Sci Mater Med 30(7):78. https://doi.org/10.1007/s10856-019-6279-x
Ni J, Ling H, Zhang S, Wang Z, Peng Z, Benyshek C et al (2019) Three-dimensional printing of metals for biomedical applications. Mater Today Biol 3:100024. https://doi.org/10.1016/j.mtbio.2019.100024
Pati F, Jang J, Ha DH, Kim SW, Rhie JW, Shim JH et al (2014) Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat Commun 5(1):1–11. https://doi.org/10.1038/ncomms4935
Grolman JM, Zhang D, Smith AM, Moore JS, Kilian KA (2015) Rapid 3D extrusion of synthetic tumor microenvironments. Adv Mater 27(37):5512–5517. https://doi.org/10.1002/adma.201501729
Zema L, Melocchi A, Maroni A, Gazzaniga A (2017) Three-dimensional printing of medicinal products and the challenge of personalized therapy. J Pharm Sci 106(7):1697–1705. https://doi.org/10.1016/j.xphs.2017.03.021
Han D, Morde RS, Mariani S, La Mattina AA, Vignali E, Yang C et al (2020) 4D printing of a bioinspired microneedle array with backward-facing barbs for enhanced tissue adhesion. Adv Funct Mater 30(11):1909197. https://doi.org/10.1002/adfm.201909197
Christensen K, Xu C, Chai W, Zhang Z, Fu J, Huang Y (2015) Freeform inkjet printing of cellular structures with bifurcations. Biotechnol Bioeng 112(5):1047–1055. https://doi.org/10.1002/bit.25501
Mannoor MS, Jiang Z, James T, Kong YL, Malatesta KA, Soboyejo WO et al (2013) 3D printed bionic ears. Nano Lett 13(6):2634–2639. https://doi.org/10.1021/nl4007744
Perera AS, Coppens M-O (2019) Re-designing materials for biomedical applications: from biomimicry to nature-inspired chemical engineering. Philos Trans R Soc A Math Phys Eng Sci 377(2138):20180268. https://doi.org/10.1098/rsta.2018.0268
Karbalaei A, Cho HJ (2018) Microfluidic devices developed for and inspired by thermotaxis and chemotaxis. Micromachines 9(4):149. https://doi.org/10.3390/mi9040149
Acknowledgements
The authors acknowledge Arizona State University for the start-up funding support.
Author information
Authors and Affiliations
Contributions
YZ, DJ, XL wrote the sections of introduction, summary, and outlook. WS wrote 3D printing of biomimetic lab-on-chip. YC wrote 3D printing of biomimetic medicine. JR wrote 3D printing of biomimetic microvascular network. HZ wrote 3D printing of biomimetic scaffold-based implants. SX wore 3D printing of artificial organs. All authors discussed and commented on the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This review does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Zhu, Y., Joralmon, D., Shan, W. et al. 3D printing biomimetic materials and structures for biomedical applications. Bio-des. Manuf. 4, 405–428 (2021). https://doi.org/10.1007/s42242-020-00117-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-020-00117-0