Abstract
Purpose
Dysregulation of the stress system via incidental long exposure to glucocorticoids (GCs) can lead to weight gain. In addition, family and maternal stress can also have an impact on children’s weight. Hair is used in several studies to evaluate cortisol (GC) levels in children and adolescents with excess weight as a retrospective stress biomarker, depending on the hair length the cortisol measurement depicting different time periods. We aimed to investigate whether there is a difference among segmental hair cortisol concentration (HCC) analysis between children and adolescents with overweight and obesity, their mothers, and normal weight peers.
Methods
This study recruited 25 children aged 6–14 years with a body mass index (BMI) ≥ 85th centile and their mothers, as well as 20 children of the same age with a BMI < 85th centile. Hair cortisol concentration was measured using electrochemiluminescence immunoassay.
Results
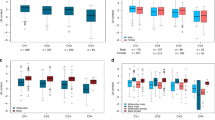
Segmental HCC analysis exhibited gradually decreasing values in all participants as segments of hair were more distantly located from the scalp. A positive correlation was found between BMI z-score and HCC of the first segment of hair in children and adolescents with elevated BMI (b = 1.84, p = 0.033), as well as with maternal HCC / of an only child (b = 15.77, p = 0.01). There were no associations between mother-child dyads and children and adolescents of different BMI groups, even though minors with excess weight exhibited higher HCC levels in all segments of hair in comparison to their normal weight counterparts.
Conclusions
Hair cortisol of all participants exhibited a gradually declining concentration. More studies with larger samples and more sensitive methods of analysis are warranted in order to draw firmer conclusions.

Similar content being viewed by others
References
World Health Organization (2021) Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed on 14 January 2023
NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390:2627–2642. https://doi.org/10.1016/S0140-6736(17)32129-3
Hampl SE, Hassink SG, Skinner AC, Armstrong SC, Barlow SE, Bolling CF, Avila Edwards KC, Eneli I, Hamre R, Joseph MM et al (2023) Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151:e2022060640. https://doi.org/10.1542/peds.2022-060640
Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, Yanovski JA (2017) Pediatric obesity—assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 102:709–757. https://doi.org/10.1210/jc.2016-2573
Valaiyapathi B, Gower B, Ashraf AP (2020) Pathophysiology of type 2 diabetes in children and adolescents. Curr Diabetes Rev 16:220–229. https://doi.org/10.2174/1573399814666180608074510
Tyson N, Frank M (2018) Childhood and adolescent obesity definitions as related to BMI, evaluation and management options. Best Pract Res Clin Obstet Gynaecol 48:158–164. https://doi.org/10.1016/j.bpobgyn.2017.06.003
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, Baker JS (2016) Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health Med Ther 7:125–146. https://doi.org/10.2147/AHMT.S101631
Kokka I, Mourikis I, Bacopoulou F (2023) Psychiatric disorders and obesity in childhood and adolescence—a systematic review of cross-sectional studies. Children 10:285. https://doi.org/10.3390/children10020285
Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS (2015) Childhood obesity: causes and consequences. J Family Med Prim Care 4:187–192. https://doi.org/10.4103/2249-4863.154628
Gurnani M, Birken C, Hamilton J (2015) Childhood obesity: causes, consequences, and management. Pediatr Clin N Am 62:821–840. https://doi.org/10.1016/j.pcl.2015.04.001
de Guia RM, Rose AJ, Herzig S (2014) Glucocorticoid hormones and energy homeostasis. Horm Mol Biol Clin Invest 19:117–128. https://doi.org/10.1515/hmbci-2014-0021
Pervanidou P, Chrousos GP (2016) Stress and pediatric obesity: neurobiology and behavior. Fam Relat 65:85–93. https://doi.org/10.1111/fare.12181
Kuckuck S, van der Valk ES, Scheurink AJW, van der Voorn B, Iyer AM, Visser JA, Delhanty PJD, van den Berg SAA, van Rossum EFC (2022) Glucocorticoids, stress and eating: the mediating role of appetite-regulating hormones. Obes Rev 24:e13539. https://doi.org/10.1111/obr.13539
Ulrich-Lai YM, Fulton S, Wilson M, Petrovich G, Rinaman L (2015) Stress exposure, food intake and emotional state. Stress 18:381–399. https://doi.org/10.3109/10253890.2015.1062981
García-Eguren G, Sala-Vila A, Giró O, Vega-Beyhart A, Hanzu FA (2020) Long-term hypercortisolism induces lipogenesis promoting palmitic acid accumulation and inflammation in visceral adipose tissue compared with HFD-induced obesity. Am J Physiol Endocrinol Metab 318:E995–E1003. https://doi.org/10.1152/ajpendo.00516.2019
Lustig RH, Collier D, Kassotis C, Roepke TA, Kim MJ, Blanc E, Barouki R, Bansal A, Cave MC, Chatterjee S et al (2022) Obesity I: overview and molecular and biochemical mechanisms. Biochem Pharmacol 199:115012. https://doi.org/10.1016/j.bcp.2022.115012
Lee M-J, Pramyothin P, Karastergiou K, Fried SK (2014) Deconstructing the roles of glucocorticoids in adipose tissue biology and the development of central obesity. Biochim Biophys Acta 1842:473–481. https://doi.org/10.1016/j.bbadis.2013.05.029
Daniels LA (2019) Feeding practices and parenting: a pathway to child health and family happiness. Ann Nutr Metab 74:29–42. https://doi.org/10.1159/000499145
Balantekin KN, Anzman-Frasca S, Francis LA, Ventura AK, Fisher JO, Johnson SL (2020) Positive parenting approaches and their association with child eating and weight: a narrative review from infancy to adolescence. Pediatr Obes 15:e12722. https://doi.org/10.1111/ijpo.12722
O’Connor SG, Maher JP, Belcher BR, Leventhal AM, Margolin G, Shonkoff ET, Dunton GF (2017) Associations of maternal stress with children’s weight-related behaviours: a systematic literature review. Obes Rev 18:514–525. https://doi.org/10.1111/obr.12522
Tate EB, Wood W, Liao Y, Dunton GF (2015) Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index. Obes Rev 16:351–361. https://doi.org/10.1111/obr.12262
Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A (2012) Influence of stress in parents on child obesity and related behaviors. Pediatrics 130:e1096–e1104. https://doi.org/10.1542/peds.2012-0895
Nicolaides NC, Kyratzi E, Lamprokostopoulou A, Chrousos GP, Charmandari E (2015) Stress, the stress system and the role of glucocorticoids. Neuroimmunomodulation 22:6–19. https://doi.org/10.1159/000362736
Gatti R, Antonelli G, Prearo M, Spinella P, Cappellin E, De Palo EF (2009) Cortisol assays and diagnostic laboratory procedures in human biological fluids. Clin Biochem 42:1205–1217. https://doi.org/10.1016/j.clinbiochem.2009.04.011
Russell E, Koren G, Rieder M, Van Uum S (2012) Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology 37:589–601. https://doi.org/10.1016/j.psyneuen.2011.09.009
Wosu AC, Valdimarsdóttir U, Shields AE, Williams DR, Williams MA (2013) Correlates of cortisol in human hair: implications for epidemiologic studies on health effects of chronic stress. Ann Epidemiol 23:797–811.e2. https://doi.org/10.1016/j.annepidem.2013.09.006
Kitani RA, Letsou K, Kokka I, Kanaka-Gantenbein C, Bacopoulou F (2022) Difference in hair cortisol concentrations between obese and non-obese children and adolescents: a systematic review. Children (Basel) 9:715. https://doi.org/10.3390/children9050715
Ma L, Liu X, Yan N, Gan Y, Wu Y, Li Y, Chu M, Chiu DT, Ma L (2022) Associations between different cortisol measures and adiposity in children: a systematic review and meta-analysis. Front Nutr 9:879256. https://doi.org/10.3389/fnut.2022.879256
Veldhorst MAB, Noppe G, Jongejan MHTM, Kok CBM, Mekic S, Koper JW, van Rossum EFC, van den Akker ELT (2014) Increased scalp hair cortisol concentrations in obese children. J Clin Endocrinol Metab 99:285–290. https://doi.org/10.1210/jc.2013-2924
Olstad DL, Ball K, Wright C, Abbott G, Brown E, Turner AI (2016) Hair cortisol levels, perceived stress and body mass index in women and children living in socioeconomically disadvantaged neighborhoods: the READI study. Stress 19:158–167. https://doi.org/10.3109/10253890.2016.1160282
Larsen SC, Fahrenkrug J, Olsen NJ, Heitmann BL (2016) Association between hair cortisol concentration and adiposity measures among children and parents from the “healthy start” study. PLoS One 11:e0163639. https://doi.org/10.1371/journal.pone.0163639
Papafotiou C, Christaki E, van den Akker ELT, Wester VL, Apostolakou F, Papassotiriou I, Chrousos GP, Pervanidou P (2017) Hair cortisol concentrations exhibit a positive association with salivary cortisol profiles and are increased in obese prepubertal girls. Stress 20:217–222. https://doi.org/10.1080/10253890.2017.1303830
Noppe G, van den Akker ELT, de Rijke YB, Koper JW, Jaddoe VW (2005) van Rossum EFC (2016) Long-term glucocorticoid concentrations as a risk factor for childhood obesity and adverse body-fat distribution. Int J Obes 40:1503–1509. https://doi.org/10.1038/ijo.2016.113
Bryson HE, Mensah F, Goldfeld S, Price AMH (2020) Using hair cortisol to examine the role of stress in children’s health inequalities at 3 years. Acad Pediatr 20:193–202. https://doi.org/10.1016/j.acap.2019.05.008
Genitsaridi S-M, Karampatsou S, Papageorgiou I, Mantzou A, Papathanasiou C, Kassari P, Paltoglou G, Kourkouti C, Charmandari E (2019) Hair cortisol concentrations in overweight and obese children and adolescents. Horm Res Paediatr 92:229–236. https://doi.org/10.1159/000504913
Distel LML, Egbert AH, Bohnert AM, Santiago CD (2019) Chronic stress and food insecurity: examining key environmental family factors related to body mass index among low-income Mexican-origin youth. Fam Community Health 42:213–220. https://doi.org/10.1097/FCH.0000000000000228
Christaki EV, Pervanidou P, Papassotiriou I, Bastaki D, Valavani E, Mantzou A, Giannakakis G, Boschiero D, Chrousos GP (2022) Stress, inflammation and metabolic biomarkers are associated with body composition measures in lean, overweight, and obese children and adolescents. Children (Basel) 9:291. https://doi.org/10.3390/children9020291
Stalder T, Kirschbaum C (2012) Analysis of cortisol in hair – state of the art and future directions. Brain Behav Immun 26:1019–1029. https://doi.org/10.1016/j.bbi.2012.02.002
Hodes A, Lodish MB, Tirosh A, Meyer J, Belyavskaya E, Lyssikatos C, Rosenberg K, Demidowich A, Swan J, Jonas N et al (2017) Hair cortisol in the evaluation of cushing syndrome. Endocrine 56:164–174. https://doi.org/10.1007/s12020-017-1231-7
Zarkogianni K, Chatzidaki E, Polychronaki N, Kalafatis E, Nicolaides NC, Voutetakis A, Chioti V, Kitani RA, Mitsis K, Perakis Κ et al (2023) The ENDORSE feasibility study: exploring the use of m-Health, artificial intelligence and serious games for the management of childhood obesity. Nutrients 15:1451. https://doi.org/10.3390/nu15061451
Nicolaides NC, Makridakis M, Kitani RA, Letsou K, Kressou E, Angelopoulou E, Vasilakis I, Mantzou A, Papassotiriou I, Varvogli L, Zoidakis I, Kanana-Gantenbein C (2022) Proteomics analysis in children and adolescents with type I diabetes mellitus and assosiation with cognitive function levels. In: 20th Hellinic Diabetes Congress, Greece
World Medical Association Declaration of Helsinki (2013) ethical principles for medical research involving human subjects. JAMA 310:2191–2194. https://doi.org/10.1001/jama.2013.281053
Tanner JM, Whitehouse RH (1976) Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child 51:170–179. https://doi.org/10.1136/adc.51.3.170
Must A, Anderson SE (2006) Body mass index in children and adolescents: considerations for population-based applications. Int J Obes 30:590–594. https://doi.org/10.1038/sj.ijo.0803300
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240–1243. https://doi.org/10.1136/bmj.320.7244.1240
Cole TJ, Lobstein T (2012) Extended International (IOTF) Body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7:284–294. https://doi.org/10.1111/j.2047-6310.2012.00064.x
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL (2002) 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11(246):1–190
Freedman DS, Berenson GS (2017) Tracking of bmi z scores for severe obesity. Pediatrics 140:e20171072. https://doi.org/10.1542/peds.2017-1072
Sauvé B, Koren G, Walsh G, Tokmakejian S, Van Uum SHM (2007) Measurement of cortisol in human hair as a biomarker of systemic exposure. Clin Invest Med 30:E183–E191. https://doi.org/10.25011/cim.v30i5.2894
Thomson S, Koren G, Fraser L-A, Rieder M, Friedman TC, Van Uum SHM (2009) Hair analysis provides a historical record of cortisol levels in Cushing’s syndrome. Exp Clin Endocrinol Diabetes 118:133–138. https://doi.org/10.1055/s-0029-1220771
Vehmeijer FOL, Santos S, Gaillard R, de Rijke YB, Voortman T, van den Akker ELT, Felix JF, van Rossum EFC, Jaddoe VWV (2021) Associations of hair cortisol concentrations with general and organ fat measures in childhood. J Clin Endocrinol Metab 106:e551–e561. https://doi.org/10.1210/clinem/dgaa785
Gray NA, Dhana A, Van Der Vyver L, Van Wyk J, Khumalo NP, Stein DJ (2018) Determinants of hair cortisol concentration in children: a systematic review. Psychoneuroendocrinology 87:204–214. https://doi.org/10.1016/j.psyneuen.2017.10.022
Stalder T, Steudte-Schmiedgen S, Alexander N, Klucken T, Vater A, Wichmann S, Kirschbaum C, Miller R (2017) Stress-related and basic determinants of hair cortisol in humans: a meta-analysis. Psychoneuroendocrinology 77:261–274. https://doi.org/10.1016/j.psyneuen.2016.12.017
Lembcke H, Buchmüller T, Leyendecker B (2020) Refugee mother-child dyads’ hair cortisol, post-traumatic stress, and affectionate parenting. Psychoneuroendocrinology 111:104470. https://doi.org/10.1016/j.psyneuen.2019.104470
Gherlone N, Hill DR, Feinn R, Hollenbach JP (2021) Hair cortisol concentrations among urban and rural-dwelling mother–child dyads, La Romana, Dominican Republic. Stress 24:413–420. https://doi.org/10.1080/10253890.2020.1846028
Bryson HE, Mensah F, Goldfeld S, Price AMH, Giallo R (2021) Hair cortisol in mother–child dyads: examining the roles of maternal parenting and stress in the context of early childhood adversity. Eur Child Adolesc Psychiatry 30:563–577. https://doi.org/10.1007/s00787-020-01537-0
Karlén J, Frostell A, Theodorsson E, Faresjö T, Ludvigsson J (2013) Maternal influence on child HPA axis: a prospective study of cortisol levels in hair. Pediatrics 132:e1333–e1340. https://doi.org/10.1542/peds.2013-1178
Liu CH, Snidman N, Leonard A, Meyer J, Tronick E (2016) Intra-individual stability and developmental change in hair cortisol among postpartum mothers and infants: implications for understanding chronic stress: hair cortisol stability in mothers and infants. Dev Psychobiol 58:509–518. https://doi.org/10.1002/dev.21394
Romanova Z, Karailievova L, Garafova A, Hlavacova N, Oravcova H, Jezova D (2022) Testosterone but not cortisol concentrations in hair correlate between mothers and their prepubertal children under real-life stress conditions. Psychoneuroendocrinology 143:105844. https://doi.org/10.1016/j.psyneuen.2022.105844
Larsen SC, Turicchi J, Christensen GL, Larsen CS, Jørgensen NR, Mikkelsen MLK, Horgan G, O’Driscoll R, Michalowska J, Duarte C et al (2021) Hair cortisol concentration, weight loss maintenance and body weight variability: a prospective study based on data from the European NoHoW trial. Front Endocrinol 12:655197. https://doi.org/10.3389/fendo.2021.655197
Ling J, Xu D, Robbins LB, Kao TSA (2020) Obesity and hair cortisol: relationships varied between low-income preschoolers and mothers. Matern Child Health J 24:1495–1504. https://doi.org/10.1007/s10995-020-03008-z
Qian G, Mei J, Tian L, Dou G (2020) Assessing mothers’ parenting stress: differences between one- and two-child families in China. Front Psychol 11:609715. https://doi.org/10.3389/fpsyg.2020.609715
van der Valk E, Abawi O, Mohseni M, Abdelmoumen A, Wester V, van der Voorn B, Iyer A, van den Akker E, Hoeks S, van den Berg S et al (2022) Cross-sectional relation of long-term glucocorticoids in hair with anthropometric measurements and their possible determinants: a systematic review and meta-analysis. Obes Rev Off J Int Assoc Study Obes 23:e13376. https://doi.org/10.1111/obr.13376
Handelsman DJ, Wartofsky L (2013) Requirement for mass spectrometry sex steroid assays in the journal of clinical endocrinology and metabolism. J Clin Endocrinol Metab 98:3971–3973. https://doi.org/10.1210/jc.2013-3375
Russell E, Kirschbaum C, Laudenslager ML, Stalder T, de Rijke Y, van Rossum EFC, Van Uum S, Koren G (2015) Toward standardization of hair cortisol measurement: results of the first international interlaboratory round robin. Ther Drug Monit 37:71–75. https://doi.org/10.1097/FTD.0000000000000148
Greff MJE, Levine JM, Abuzgaia AM, Elzagallaai AA, Rieder MJ, van Uum SHM (2019) Hair cortisol analysis: an update on methodological considerations and clinical applications. Clin Biochem 63:1–9. https://doi.org/10.1016/j.clinbiochem.2018.09.010
Funding
The work was supported by the postgraduate course on the Science of Stress and Health Promotion of the National and Kapodistrian University of Athens and the First Department of Pediatrics of the Medical School on the National and Kapodistrian University of Athens at “Aghia Sophia” Children’s Hospital, Athens, Greece.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the Research Ethics Committee of “Aghia Sophia” Children’s Hospital (protocol number: 23234; date:18 November 2021), the procedures of which were in accordance with the standards of the Declaration of Helsinki for human experimentation [43]. All mothers of mother-child dyads signed a written informed consent form for their own and their child’s participation. Likewise, the parents of children in the control group were also informed about the purpose of this study and signed a written consent form. In addition, adolescents gave oral consent for their participation in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kitani, RA., Nicolaides, N.C., Mantzou, A. et al. Differences in segmental hair cortisol concentration analysis among children and adolescents with overweight and obesity, their parents, and normal weight peers. Hormones 22, 623–632 (2023). https://doi.org/10.1007/s42000-023-00482-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-023-00482-2