Abstract
Purpose
The purpose was to evaluate the association between medication adherence and health-related quality of life (HRQoL) of patients with diabetes.
Methods
In this cross-sectional study, a total of 518 patients were recruited from the outpatient departments of different general public and private hospitals in Greece during the COVID-19 pandemic using a consecutive sampling method. HRQoL was assessed with the EQ-5D-5L instrument and medication adherence with the corresponding subscale of the Adherence Starts with Knowledge 20 questionnaire. The relationship between HRQoL and adherence was explored by employing Spearman’s correlations and multiple binary logistic and linear stepwise regressions using robust standard errors.
Results
A total of 15.1 and 1.9% of the patients reported that they had taken a medicine either more or less often than prescribed in the last month and week, respectively. Statistically significant but modest correlations of medication non-adherence with the EQ-5D index (rho = − 0.223), EQ-VAS (rho = − 0.230), and all the HRQoL domains (rho ranging from 0.211, for pain/discomfort, to 0.136, for mobility issues) were found. These significant associations persisted even after controlling for several other known potential factors of HRQoL in the multivariable analyses, except for the mobility and anxiety/depression dimensions.
Conclusion
Medication non-adherence appears to be independently associated with lower HRQoL and health levels in patients with diabetes. It is crucial to plan interventions to enhance medication adherence not only to obtain greater value from the available resources, but also to improve HRQoL of patients with diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a chronic disorder characterized by hyperglycemia, i.e., raised levels of blood glucose [1]. DM and its associated health complications pose a considerable challenge to healthcare service providers in Greece, with a national prevalence of approximately 7% [2]. Despite the advances in its treatment over the past few decades, DM continues to impose a significant clinical burden, while the economic consequences to the health care system are also substantial. DM-related healthcare spending in Greece was estimated at USD 3.9 billion in 2010, i.e., approximately 9% of the total healthcare expenditure, and it is projected to rise to USD 4.6 billion by 2030 [3].
DM is a complex condition that requires self-care activities and continuous long-term attention to self-monitoring of blood glucose, food intake, emotional stress, physical activity, and medication taking [4]. Optimal glycemic control and long-term disease management in DM depends largely on the patient’s overall adherence to treatment behavior, which includes lifestyle and behavioral changes, keeping medical appointments, and taking medication as prescribed [5]. However, medication non-adherence is quite a common problem in patients with chronic conditions, the rate having been estimated at only 50% on average in developed countries and even lower in the developing world [4]. In particular, medication non-adherence constitutes a major challenge in the treatment of DM, with a number of studies showing high rates of discontinuation and incorrect administration and medicine dosages [6,7,8]. Good medication adherence can improve glycemic control, whereas suboptimal adherence can lead to poor treatment responses, progression of disease symptoms, and development of several diabetes-related complications (e.g., neuropathy, kidney failure, and cardiovascular events) [7, 9]. Furthermore, as a consequence of deteriorating health outcomes and related adverse events, medication non-adherence results in increased consumption of healthcare resources (e.g., unnecessary hospital admissions). A study has estimated that improving medication adherence could result in annual cost savings ranging from $661 million to $1.16 billion in the USA alone [10].
Health-related quality of life (HRQoL) represents people’s subjective appraisal of their sense of well-being and ability to perform social roles and how are these influenced by their illness or its treatment [11]. Interestingly, although there appears to be a consensus concerning the substantial HRQoL burden associated with the majority of non-communicable diseases (NCDs), their impact differs depending on the type of chronic condition [12]. In recent decades, interest in improving the HRQoL of patients with chronic illnesses has been growing, as the lack of an adequate cure has shifted the care for these NCDs from problem-oriented to goal-oriented [13, 14]. Understanding the association between patients’ HRQoL and their chronic conditions is important as it provides the tools to develop better management strategies for these diseases.
Several studies have investigated the impact of DM on patients’ HRQoL. It is clear that HRQoL in patients with DM is greatly compromised by the chronic burden of the illness and the combined effect of related complications in various dimensions of well-being [15]. Diabetes is a complex condition which requires continual attention and control of blood glucose levels, and, importantly, enhanced medication adherence has been associated with better glycemic control and lower healthcare resource utilization [16]. In this framework, adherence can be considered as an intermediate or process variable, while HRQoL is the ultimate outcome [17]. Although it is expected that improved medication adherence has a positive impact on HRQoL in DM through better clinical outcomes, the findings in the literature are contradictory. While some past research has demonstrated a positive relationship between medication adherence and HRQoL [18], other studies have found no association between them [19, 20]. Therefore, it is important to provide some further insight into the HRQoL impact on adherence to antidiabetic medication treatment. The main purpose of this study is to evaluate the association between medication adherence and HRQoL of patients with DM in Greece. The secondary objectives are to investigate the effect of other factors that influence HRQoL in diabetic patients.
Methods
Study design and participants
This was a multicenter, cross-sectional, non-interventional epidemiological study and no specific treatment protocol, diagnostic/therapeutic procedure, or visit program was imposed. The survey was conducted between March 2020 and March 2021 using a consecutive sampling method. Participants were recruited from patients attending the outpatient departments of different general public and private hospitals, community pharmacies, and private practices, and from patient groups and medical societies in Greece, thus ensuring the representativeness of the sample.
The study participants were adult patients (≥ 18 years) who were medically diagnosed with DM, at various degrees of severity, and had been receiving antidiabetic treatment for at least 6 months. Patients who were not mentally capable of responding to the survey questionnaire or not able or willing to provide written consent, pregnant women, and persons suffering from acute life-threatening conditions were excluded.
The study was designed according to the principles of the Declaration of Helsinki. Participation in the survey was completely anonymous. Eligible and willing participating patients were fully informed about the aims of the study, and those who agreed to participate provided written informed consent. Ethical approval for conducting this study was obtained from the scientific boards of the respective institutions.
Data collection
Study participants were interviewed by trained investigators using a structured questionnaire. The survey questionnaire was developed specifically for this study based on a comprehensive review of the international literature and in collaboration with health experts. A pilot study was conducted before the launch of the main fieldwork to assess the feasibility of the questionnaire in terms of readability, comprehensibility, and time to complete the survey, and expert reviews were also used to evaluate the questionnaire. Data were collected concerning sociodemographics, clinical characteristics (e.g., time since diagnosis and time since starting medication treatment), medication adherence, and HRQoL.
HRQoL instrument
HRQoL was assessed with the EQ-5D-5L questionnaire, which is a generic measure of HRQoL and has been validated in the Greek setting [21]. The EQ-5D-5L is a preference-based generic measure of HRQoL which consists of the following: (a) the EQ-5D descriptive system and (b) the EQ-VAS. The EQ-5D descriptive system includes five domains of health, i.e., mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is measured on a five-level scale, with higher levels representing more health problems. Domain scores were also dichotomized to identify the presence of problems (level 1 vs. levels 2–5). A single utility score is obtained by applying societal value sets, derived from population-based valuation studies, to the state of health vectors ranging between 11,111 (full health) and 55,555 (worst health). The preference-based index typically varies from states worse than dead (< 0) to full health (1). As the Greek value sets have not yet been developed, health utilities were obtained based on time trade-off valuations from a general population study conducted in the UK which have been found applicable to the Greek setting [21]. The VAS is used to rate respondents’ current self-rated health on a 20 cm visual analog scale ranging from 0 (worst imaginable health) to 100 (best imaginable health) [21].
Medication adherence assessment
Medication adherence was assessed with the Adherence Starts with Knowledge 20 (ASK-20) questionnaire, which was developed to identify barriers to treatment adherence [22, 23]. It comprises 20 items, which are rated on a 5-point scale that can be classified into the following domains: lifestyle (items Q1‒Q6), attitude and behavior (Q7‒Q8), support from others or communication with the healthcare team (Q9‒Q12), barriers to medicine use (Q13‒Q15), and adherence to medicines (Q16‒Q20). We specifically used the medication adherence subscale, which ranges from 5 to 25, with higher scores indicating a greater degree of medication non-adherence. The derived Likert subscale was found to have good internal consistency (standardized Cronbach alpha: 0.77).
Statistical analysis
Descriptive statistics were performed to characterize the sample. Chi-square (and Fisher’s exact) tests were conducted to identify significant associations between categorical variables. Group differences with respect to continuous variables were investigated using the independent sample t-test and the Mann–Whitney U-test for normally and non-normally distributed variables, respectively. For variables with three or more groups, the ANOVA and Kruskal–Wallis tests were used, respectively. Normality of the distribution was explored with the Shapiro–Wilk normality test. Spearman’s rank correlation coefficient was employed to assess the association between HRQoL and medication adherence variables. Multiple binary logistic and linear stepwise regressions using robust standard errors were carried out to identify the independent predictors of the presence of problems in each HRQoL domain and the EQ-5D index and VAS, respectively. The factors that were used in the univariate analysis were entered into each model with a p-value < 0.05 and were removed with a p-value > 0.1.
The level of significance was set at α = 0.05. Statistical analysis was conducted using the SPSS® v.26 and STATA® v.16.
Results
A total of 518 patients with DM were recruited for this study. The sociodemographic and clinical characteristics of the subjects are presented in Table 1. The mean age of the sample was 47.4 (± 41.8) years and 331 (63.9%) of the participants were females. Two-thirds (66%) of the sample had been diagnosed with type 1 diabetes and the mean duration of the disease was 17.94 (± 11) years. Furthermore, the HbA1c last reading was equal to or greater than 7% for more than half of the patients (57.3%) and 60.4% of the participants reported having at least one comorbidity.
The distribution of the responses for the EQ-5D descriptive system is summarized in Table 2. Overall, the dimension with the highest prevalence of problems was anxiety/depression (72.6%), followed by pain/discomfort (38.6%), while self-care was the least frequently reported limitation (8.5%). The mean value of the EQ-5D index was 0.78 (± 0.2) and the mean EQ-VAS score was 71.31 (± 16.74). The mean ASK-20 medication non-adherence score was 8.07 (± 3.37). Furthermore, 15.1 and 1.9% of the patients stated that they had taken a medicine more or less often than prescribed in the last month and week, respectively, preceding the interview.
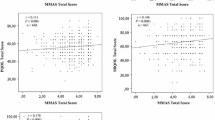
The correlation analysis showed a significant negative correlation of medication non-adherence with the EQ-5D index and VAS, though the magnitude of the associations was small (rho = − 0.223 and rho = − 0.230, respectively, p-value < 0.01 for both) (Table 3). Significant but weak positive correlations were also found between medication non-adherence and all the EQ-5D domains; the strongest relation was detected with pain/discomfort problems (rho = 0.211, p-value < 0.01) and the weakest with mobility issues (rho = 0.136, p-value < 0.01). The strength of the association between medication non-adherence and HRQoL varied across the individual items of the medication non-adherence scale.
Tables 4 and 5 present the results of the univariate analysis of HRQoL. Low medication non-adherence, as it was indicated using the median score of the sample as a cutoff, was significantly associated with a higher proportion of patients reporting problems in all EQ-5D domains and lower EQ-5D index and VAS scores. The univariate effect of the other factors varied with respect to the dependent variable.
The results of the multivariable analyses revealed that patients who were older, inactive, or unemployed, living alone, obese, less physically active, with type 1 diabetes, and taking oral only antidiabetic medications and who had two or more comorbidities were more likely to report mobility problems (Table 6). A higher likelihood of self-care issues was associated with older age, inactivity or unemployment, making ends meet very easily or easily, being married, not having children, living alone, fewer days exercising per week, bad glycemic control, and having two or more comorbidities and worse medication adherence. Participants who were female, older, inactive or unemployed, with worse economic status, living alone, less physically active, and less adherent to antidiabetic medication were associated with a higher probability, and those who were overweight with a lower likelihood of reporting difficulties in the usual activities’ dimension. Increased risk of pain/discomfort issues was established for patients who were older, with better economic status, those with a 5–9-year duration of disease, two or more comorbidities, and less medication adherence.
Multivariable regression analysis showed that higher medication adherence was an independent predictor of higher EQ-5D index and VAS (Table 7). Furthermore, female gender, older age, economic inactivity or unemployment, obesity, and having comorbidities were associated with lower EQ-5D index, and higher education, better economic status, and physical activity with increased EQ-5D index. On the other hand, female gender, being inactive or unemployed, obesity, type 2 diabetes, poor glycemic control, and having two or more comorbidities were independent risk factors decreasing VAS, whereas better economic status and physical activity positively influenced VAS.
Discussion
This was a multicenter, cross-sectional, non-interventional study with a primary aim to investigate the impact of medication adherence on the HRQoL of patients with DM. Our results revealed a modest negative correlation between medication non-adherence and HRQoL and health status, based on measurements using the EQ-5D index and EQ-VAS, respectively. However, this association persisted even after controlling for several other known potential factors of HRQoL. Furthermore, the positive association of medication adherence with HRQoL in diabetic patients was found to be mainly driven by the impact of medication adherence on the dimensions of pain/discomfort, usual activities, and self-care, as these were the only domains for which medication adherence maintained its statistical significance in the multivariable analysis.
Although one would anticipate that improved medication adherence would have a positive impact on HRQoL, the findings of the literature are not always consistent. A number of studies have identified a positive relationship between medication adherence and HRQoL and improvements in patient-centered outcomes following medication adherence enhancing interventions [18, 24,25,26,27,28]. However, other studies have not arrived at the same conclusion [17. 19, 20]. One reason for these inconsistent findings may be the different study populations, settings, and instruments used for measuring HRQoL and adherence [18]. The choice of the method employed to measure HRQoL may be quite important. An instrument designed specifically for a population or a disease may be more responsive to changes in HRQoL compared with a generic measure [17], such as the EQ-5D-5L questionnaire that was used in this study.
There are at least two explanations for how better medication adherence may promote HRQoL. According to the most plausible interpretation, the full benefit of most medicines can only be achieved if patients closely follow their prescribed regimen [29]. As patients become more adherent, debilitating symptoms decrease and clinical outcomes improve in the short term and disease control increases in the longer term, thus resulting in better HRQoL. In contrast, an uncontrolled course of the disease may impair patients’ well-being [28]. In a more indirect way, HRQoL, which is a psychosocial construct, may be positively influenced by patients’ belief that they are actively contributing to the management of their disease by following their prescribed treatment [24]. On the other hand, a more adherent patient may face short-term detrimental effects on their HRQoL due to treatment-related adverse events and daily routine limitations [30, 31]. The self-regulatory model assumes that patients continually evaluate the consequences of being adherent and adjust their behavior accordingly [17]. However, a possibility of reverse causality, where it is the HRQoL that influences adherence, may also be true [31]. For instance, patients may stop taking their medications because they feel better and their quality of life has improved, which they presume to be a sign of a cured disease. Moreover, patients may also stop taking their medications because they feel worse, and they perceive this as the result of an ineffective treatment. These cases describe situations where it is changes in HRQoL that precede changes in adherence behavior [32]. To add even more complexity to the matter, there could also be a circular relationship between adherence and HRQoL, as non-adherence may impair HRQoL, which in turn may trigger further non-adherence [33]. Additionally, other research has identified motivational constructs of health behavior, such as autonomous self-regulation and perceived competence, as factors of both HRQoL and adherence [34, 35].
In our study, 17% of patients with DM stated that they had taken a medicine more or less often than prescribed at least once in the previous month. Furthermore, 2.2 and 6.5% had skipped or stopped taking a medicine because they believed that it did not work and due to its side effects, respectively. In a recent study, also conducted during the COVID-19 pandemic, 25.1% of patients with hypertension and dyslipidemia reported that they sometimes forget to take their prescribed medications [27]. In general, several factors have been identified in the literature as potential barriers to medication adherence, such as the complexity of the medication regimen, patients’ forgetfulness, poor awareness concerning the significance of medication adherence, and negative beliefs or insufficient knowledge about their medications [14, 36,37,38,39]. Reassuringly, just 4.4% reported poor medication adherence owing to economic reasons, which is lower than the estimate of 10.1% during the economic crisis [40]. Starting in 2014, a series of measures were implemented to expand health coverage to all uninsured citizens, while a full exemption from or a reduction to the co-payments of extremely vulnerable individuals was legislated in 2017 [41]. However, it should be noted that the above findings may be affected by greater health awareness during the pandemic [27], although there are also reports of foregoing or postponing necessary treatment during this time period [42].
Several studies have investigated the impact of DM on patients’ HRQoL. It is clear that HRQoL in patients with DM is greatly compromised by the chronic burden of the illness and the combined effect of related complications on various dimensions of well-being [15]. Regarding the dimensions of the EQ-5D instrument, anxiety/depression was the most frequently reported limitation, followed by pain/discomfort, while self-care was the domain with the lowest prevalence of problems, which is consistent with a previous study conducted in Greece [15]. The average HRQoL and health status were higher in our survey, which can be attributed to the lower mean age of our sample.
In our study, female participants had lower both HRQoL and health status compared with male patients. It has been suggested that men may cope better with the chronic character of the disease [27]. Age and not having children were risk factors of impaired HRQoL but they did not reach statistical significance for health status. In line with previous studies [14, 27], better socioeconomic status, i.e., higher education (although not statistically significant for health status) and economic status and being employed, were associated with improved HRQoL and health. Furthermore, a healthier lifestyle, i.e., lower BMI and more physical activity, led to better HRQoL and health, which confirms the value of behavior adjustments in enhancing the well-being of patients with DM [27]. Interestingly, lower HbA1c values and type 2 diabetes were independently associated with higher VAS levels, while they were not a significant predictor of the EQ-5D index. Several previous studies have found a negative relationship between HbA1c levels and HRQoL using either generic or diabetes-specific measures [43,44,45]. Finally, based on the literature [15], a higher number of comorbidities were associated with impaired HRQoL and health.
There are some limitations of the current study that need to be acknowledged. First, our findings are based on survey data, which are susceptible to several biases (i.e., report, recall). Second, the survey was conducted during the pandemic, which may have influenced both the medication adherence and the HRQoL of patients as well as their relationship. Third, due to the cross-sectional design of the study, the possibility of reverse causality between HRQoL and medication adherence cannot be rejected. Fourth, we employed a self-reported medication adherence measure, which may have influenced the observed relationship between HRQoL and adherence. Fifth, a generic measure of HRQoL was employed, which may not be as sensitive to differences as a disease-specific instrument.
Conclusions
Managing a chronic condition such as diabetes requires long-term treatment, which involves lifelong pharmacotherapy and lifestyle adjustments. Although clinical outcomes can provide a valuable insight concerning the level of disease control, the ultimate goal of diabetes care should be HRQoL improvement, since diabetes exerts a considerable impact on key dimensions of patients’ well-being. Medication non-adherence is an important contributor to morbidity, mortality, and waste of resources throughout the world. Our study demonstrated that medication non-adherence is independently associated with lower HRQoL and health levels in patients with diabetes. While clinicians tend to talk to their patients about the clinical outcome improvements related to taking medications correctly, greater focus on patient-centered benefits would likely be a more effective strategy to promote medication adherence [24]. In the context of pharmaceutical care, it appears to be crucial to plan and employ interventions to enhance medication adherence in order to obtain greater value from the available resources as well as to improve the HRQoL of patients with diabetes. For this purpose, adopting patient-centered and individualized interventions and establishing a partnership between health professionals and patients, along with pursuing systematic monitoring, are necessary to promote both medication adherence and HRQoL [46,47,48]. Treatment adherence is a multifaceted phenomenon that is influenced by multiple factors related to the patient, healthcare system, condition, therapy, and socioeconomic background that interact with each other in multiple ways [4]. Future research should explore more thoroughly the barriers to medication adherence among Greek diabetic patients and determine the most cost-effective interventions for improving medication adherence and HRQoL of patients in the Greek setting.
References
National Institute for Health and Clinical Excellence (2009) Clinical Guideline 87: Type 2 diabetes: the management of type 2 diabetes. Available at: http://www.nice.org.uk/guidance/ta203/resources/nice-recommends-liraglutide-for-type-2-diabetes-mellitus4
International Diabetes Federation (2013) IDF Diabetes Atlas, 6th edn. International Diabetes Federation, Brussels, Belgium
Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, Nichols G (2010) Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract 87(3):293–301
World Health Organization (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Saleh F, Mumu SJ, Ara F, Hafez MA, Ali L (2014) Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: a cross-sectional study. BMC Public Health 14:431
Vanelli M, Pedan A, Liu N, Hoar J, Messier D, Kiarsis K (2009) The role of patient inexperience in medication discontinuation: a retrospective analysis of medication nonpersistence in seven chronic illnesses. Clin Ther 31(11):2628–2652
Zullig LL, Gellad WF, Moaddeb J, Crowley MJ, Shrank W, Granger BB, Granger CB, Trygstad T, Liu LZ, Bosworth HB (2015) Improving diabetes medication adherence: successful, scalable interventions. Patient Prefer Adherence 9:139–149
Hüther J, von Wolff A, Stange D, Härter M, Baehr M, Dartsch DC, Kriston L (2013) Incomplete medication adherence of chronically ill patients in German primary care. Patient Prefer Adherence 7:237–244
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW (2002) Patient adherence and medical treatment outcomes: a meta-analysis. Med Care 40(9):794–811
Egede LE, Gebregziabher M, Dismuke CE, Lynch CP, Axon RN, Zhao Y, Mauldin PD (2012) Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care 35(12):2533–2539
Wang HM, Beyer M, Gensichen J, Gerlach FM (2008) Health-related quality of life among general practice patients with differing chronic diseases in Germany: cross sectional survey. BMC Public Health 8:246
Van Wilder L, Rammant E, Clays E, Devleesschauwer B, Pauwels N, De Smedt D (2019) A comprehensive catalogue of EQ-5D scores in chronic disease: results of a systematic review. Qual Life Res 28(12):3153–3161
Van Wilder L, Clays E, Devleesschauwer B, Pype P, Boeckxstaens P, Schrans D, De Smedt D (2020) Health-related quality of life in patients with non-communicable disease: study protocol of a cross-sectional survey. BMJ Open 10(9):e037131
Khayyat SM, Mohamed MMA, Khayyat SMS, Hyat Alhazmi RS, Korani MF, Allugmani EB, Saleh SF, Mansouri DA, Lamfon QA, Beshiri OM, Abdul Hadi M (2019) Association between medication adherence and quality of life of patients with diabetes and hypertension attending primary care clinics: a cross-sectional survey. Qual Life Res 28(4):1053–1061
Yfantopoulos J, Chantzaras A (2020) Health-related quality of life and health utilities in insulin-treated type 2 diabetes: the impact of related comorbidities/complications. Eur J Health Econ 21(5):729–743
Asche C, LaFleur J, Conner C (2011) A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther 33(1):74–109
Côté I, Farris K, Feeny D (2003) Is adherence to drug treatment correlated with health-related quality of life? Qual Life Res 12(6):621–633
Alfian SD, Sukandar H, Lestari K, Abdulah R (2016) Medication adherence contributes to an improved quality of life in type 2 diabetes mellitus patients: a cross-sectional study. Diabetes Therapy 7(4):755–764
Martínez YV, Prado-Aguilar CA, Rascón-Pacheco RA, Valdivia-Martínez JJ (2008) Quality of life associated with treatment adherence in patients with type 2 diabetes: a cross-sectional study. BMC Health Serv Res 8:164
Smits KPJ, Sidorenkov G, Kleefstra N, Hendriks SH, Bouma M, Meulepas M, Navis G, Bilo HJG, Denig P (2018) Is guideline-adherent prescribing associated with quality of life in patients with type 2 diabetes? PLoS ONE 13(8):e0202319
Yfantopoulos JN, Chantzaras AE (2017) Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. Eur J Health Econ 18(4):519–531
Matza LS, Yu-Isenberg KS, Coyne KS, Park J, Wakefield J, Skinner EP, Wolever RQ (2008) Further testing of the reliability and validity of the ASK-20 adherence barrier questionnaire in a medical center outpatient population. Curr Med Res Opin 24(11):3197–3206
Hahn SR, Park J, Skinner EP, Yu-Isenberg KS, Weaver MB, Crawford B, Flowers PW (2008) Development of the ASK-20 adherence barrier survey. Curr Med Res Opin 24(7):2127–2138
Conn VS, Ruppar TM, Enriquez M, Cooper PS (2016) Patient-centered outcomes of medication adherence interventions: systematic review and meta-analysis. Value Health 19(2):277–285
Farhat R, Assaf J, Jabbour H, Licha H, Hajj A, Hallit S, Khabbaz LR (2019) Adherence to oral glucose lowering drugs, quality of life, treatment satisfaction and illness perception: a cross-sectional study in patients with type 2 diabetes. Saudi Pharm J 27(1):126–132
Zioga E, Kazakos K, Dimopoulos E, Koutras C, Marmara K, Marmara E-E, Marmaras A, Lavdaniti M (2016) Adherence and quality of life in patients with type II diabetes mellitus in Northern Greece. Materia socio-medica 28(4):258–262
Souliotis K, Giannouchos TV, Golna C, Liberopoulos E (2021) Assessing forgetfulness and polypharmacy and their impact on health-related quality of life among patients with hypertension and dyslipidemia in Greece during the COVID-19 pandemic. Qual Life Res 31(1):193–204
Chew B-H (2015) Medication adherence on quality of life among adults with type 2 diabetes mellitus: an exploratory analysis on the EDDMQoL study. Qual Life Res 24(11):2723–2731
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497
Nazir SR, Hassali MA, Saleem F, Bashir S, Aljadhey H (2017) Does adherence to the therapeutic regimen associate with health related quality of life: findings from an observational study of type 2 diabetes mellitus patients in Pakistan. Pak J Pharm Sci 30(6):2159–2165
Ágh T, Dömötör P, Bártfai Z, Inotai A, Fujsz E, Mészáros Á (2015) Relationship between medication adherence and health-related quality of life in subjects with COPD: a systematic review. Respir Care 60(2):297–303
Kastien-Hilka T, Rosenkranz B, Schwenkglenks M, Bennett BM, Sinanovic E (2017) Association between health-related quality of life and medication adherence in pulmonary tuberculosis in South Africa. Front Pharmacol 8:919
Cleemput I, Kesteloot K, DeGeest S (2002) A review of the literature on the economics of noncompliance Room for methodological improvement. Health Policy 59(1):65–94
Williams GC, Patrick H, Niemiec CP, Williams LK, Divine G, Lafata JE, Heisler M, Tunceli K, Pladevall M (2009) Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and quality of life. Diabetes Educator 35(3):484–492
Walker RJ, Smalls BL, Hernandez-Tejada MA, Campbell JA, Egede LE (2014) Effect of diabetes self-efficacy on glycemic control, medication adherence, self-care behaviors, and quality of life in a predominantly low-income, minority population. Ethn Dis 24(3):349–355
Marcum ZA, Sevick MA, Handler SM (2013) Medication nonadherence: a diagnosable and treatable medical condition. JAMA 309(20):2105–2106
Kontochristopoulos G, Chantzaras A, Yfantopoulos J, Kouris A, Petridis A (2016) Improvement of health-related quality of life and adherence to treatment with calcipotriol-betamethasone dipropionate gel in patients with psoriasis vulgaris. An Bras Dermatol 91(2):160–166
Yfantopoulos J, Protopapa M, Chantzaras A, Stavropoulos G, Yfantopoulos P, Tsioufis K (2021) Greek cardiologists’ interventions to manage patients’ adherence. Hellenic J Cardiol. 62(6):466–469
Yfantopoulos J, Protopapa M, Mantalias K, Chantzaras A, Koutsogianni K, Yfantopoulos P, Vassilopoulos D (2020) Patients’ and doctors’ beliefs about treatment and long-term adherence in rheumatic diseases. Mediterr J Rheumatol 31(Suppl 1):152–162
Yfantopoulos J, Chantzaras A, Ollandezos M (2017) Unmet pharmaceutical needs during the economic crisis in Greece. Value in Health 20(9):A510
Yfantopoulos JN, Chantzaras A (2018) Drug policy in Greece. Value in Health Regional Issues 16:66–73
Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B (2021) Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med 40:20–26
Shim YT, Lee J, Toh MPHS, Tang WE, Ko Y (2012) Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in Singapore. Diabet Med 29(8):e241–e248
Rubin RR, Peyrot M (1999) Quality of life and diabetes. Diabetes Metab Res Rev 15(3):205–218
Chew BH, Sherina MS, Hassan NH (2015) Association of diabetes-related distress, depression, medication adherence, and health-related quality of life with glycated hemoglobin, blood pressure, and lipids in adult patients with type 2 diabetes: a cross-sectional study. Ther Clin Risk Manag 11:669–681
Yfantopoulos J, Protopapa M, Chantzaras A, Yfantopoulos P (2021) Doctors’ views and strategies to improve patients’ adherence to medication. Hormones 20:603–611
Yfantopoulos J (2020) Awaiting the “catharsis.” Eur J Health Econ 22(4):499–504. https://doi.org/10.1007/s10198-020-01193-w
Yfantopoulos P, Yfantopoulos J (2015) The Greek tragedy in the health sector: social and health implications. Virteljiahrshefer zur Wirtschaftsforforschung DIW Berlin 84(03):165–182
Author information
Authors and Affiliations
Contributions
All authors participated in critically revising the manuscript, and all authors approved the final version of the manuscript for submission. John Yfantopoulos designed the study, develop the questionnaire, participated in the statistical analysis, and supervised the execution of the research. Athanasios Chantzaras participated in the design of the study, development of the questionnaire, and writing of the paper; he conducted the statistical analysis.
Corresponding author
Ethics declarations
Ethical approval
In accordance with the design of the survey, an Ethics Committee approval was not needed.
Informed consent
Due to the anonymity of the survey, no individual informed consent was needed.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chantzaras, A., Yfantopoulos, J. Association between medication adherence and health-related quality of life of patients with diabetes. Hormones 21, 691–705 (2022). https://doi.org/10.1007/s42000-022-00400-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-022-00400-y