Key summary points
To investigate the prevalence of non-pharmacological interventions (NPIs) in older homecare recipients in six European countries.
AbstractSection FindingsThe prevalence of NPIs varied considerably between homecare users in different European countries. Interventions with a potential positive impact on health outcomes show a relatively low prevalence.
AbstractSection MessageFurther research into better implementation of potentially beneficial interventions in treatment guidelines might be needed, in order to optimize functioning and quality of life of older homecare recipients.
Abstract
Purpose
Non-pharmacological interventions (NPIs) play an important role in the management of older people receiving homecare. However, little is known about how often specific NPIs are being used and to what extent usage varies between countries. The aim of the current study was to investigate the prevalence of NPIs in older homecare recipients in six European countries.
Methods
This is a cross-sectional study of older homecare recipients (65+) using baseline data from the longitudinal cohort study ‘Identifying best practices for care-dependent elderly by Benchmarking Costs and outcomes of community care’ (IBenC). The analyzed NPIs are based on the interRAI Home Care instrument, a comprehensive geriatric assessment instrument. The prevalence of 24 NPIs was analyzed in Belgium, Germany, Finland, Iceland, Italy and the Netherlands. NPIs from seven groups were considered: psychosocial interventions, physical activity, regular care interventions, special therapies, preventive measures, special aids and environmental interventions.
Results
A total of 2884 homecare recipients were included. The mean age at baseline was 82.9 years and of all participants, 66.9% were female. The intervention with the highest prevalence in the study sample was ‘emergency assistance available’ (74%). Two other highly prevalent interventions were ‘physical activity’ (69%) and ‘home nurse’ (62%). Large differences between countries in the use of NPIs were observed and included, for example, ‘going outside’ (range 7–82%), ‘home health aids’ (range 12–93%), and ‘physician visit’ (range 24–94%).
Conclusions
The use of NPIs varied considerably between homecare users in different European countries. It is important to better understand the barriers and facilitators of use of these potentially beneficial interventions in order to design successful uptake strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In aging societies, the number of people living with complex chronic conditions is increasing rapidly. This increase will most likely lead to a rising number of people in need of long-term care, due to, for example, dependency in activities of daily living (ADLs) and/or instrumental activities of daily living (IADLs) [1].
Over the last decades, homecare has been marked as an effective alternative to long-term institutional care [2]. Homecare is not only a potentially cost-effective way of providing care, it is also the type of care preferred by care recipients [3]. This makes homecare one of the most important services to provide healthcare to older people with complex chronic conditions [2]. Studies have shown that there are still large differences in homecare policies and in the organization of homecare between different European countries, as well as in the availability of homecare services [4, 5].
Optimal care for older adults with chronic conditions includes both pharmacological and non-pharmacological interventions (NPIs) [6]. Some advantages of NPIs are that they can be combined with other NPIs as well as with pharmacological treatment without causing much interference and with minimal adverse side effects [7]. It is widely acknowledged that NPIs can be as effective as pharmacological therapies in the treatment of multiple chronic conditions [8, 9]. Traditionally, pharmacological interventions have received more attention through our disease-oriented healthcare system, even though NPIs are an important part of treatment according to clinical guidelines [10,11,12]. This may be due to multiple reasons, such as the lack of a common definition for NPIs, as well as methodological problems such as lack of a clear definition of interventions and how they are administered, and the lack of a theoretical model to explain the working mechanism of NPIs [13, 14]. In addition, there is also a perception that medication is easier to administer, and there may be a lack of reimbursement for NPIs. Moreover, funding sources for studying NPIs as compared to pharmacological interventions, are scarce [15].
While the emphasis is still on pharmacological treatment, the amount of research into the effectiveness of NPIs in the older population is growing [16,17,18,19,20]. However, insight into the use of NPIs in the wider homecare population is still lacking. Better insight into the use of NPIs may contribute to specific recommendations for NPI use and the application of treatment guidance in the older homecare population.
Therefore, the aim of this study was to describe the prevalence of NPIs in the older homecare population in six European countries.
Methods
Study design and data collection
For this cross-sectional analysis, we analyzed baseline data from the longitudinal cohort study ‘Identifying best practices for care-dependent elderly by Benchmarking Costs and outcomes of community care’ (IBenC). Data collection for this study was performed between January 2014 and August 2016, and the aim was to develop a benchmarking method for costs and quality of care of homecare organizations. The study rationale and protocol were described in detail elsewhere [21]. In short, a total of 2884 older adults receiving homecare (65 years and over) were enrolled from home healthcare organizations in Belgium, Finland, Germany, Iceland, Italy and the Netherlands. Participants were excluded if they (1) were terminally ill, (2) were expected to receive care only for a short term (< 6 months), (3) had planned institutionalization within 6 months, or 4) if they had no known informal caregiver or legal representative in the case of cognitive impairment [score on the Cognitive Performance Scale (CPS) ≥ 3] [19]. Detailed information was collected with the interRAI Home Care (HC) instrument. This instrument is a validated comprehensive geriatric assessment [22,23,24,25]. It consists of assessments of medical, psychological and social functional domains and service use, and assesses the needs of care-dependent older adults living in the community. The assessments were performed by trained nurses. Ethical approval was obtained before the start of the IBenC study from authorized medical ethical committees according to local regulations in each of the participating countries. Belgium (Flanders): Commissie Medische Ethiek van de Universitair Medische Ziekenhuizen Katholieke Universiteit Leuven, No. ML10265; Finland: Tutkimuseettinen työryhmä, No. THL/796/6.02.01/ 533/2014; Germany: Ethikkommission des Institut für Psychologie und Arbeitswissenschaft der Technische Universtität Berlin, No. GH_01_20131022; Iceland: Vísindasiðanefnd, No. 13–176-S1; Italy: Comitato Etico Università Cattolica del Sacro Cuore, No. 2365/14; The Netherlands: Medical Ethics Review Committee VU University Medical Center, No. 2013.333.
Non-pharmacological interventions
The outcome measure was the use of non-pharmacological interventions (NPIs) and description of differences across analyzed countries. The prevalence of use of these interventions in the study population was analyzed using the interRAI HC instrument, which is an updated version of the interRAI MDS 2.0.
To determine which interventions could be defined as ‘non-pharmacological’, we held multiple consensus meetings with a multidisciplinary team of researchers and healthcare professionals from several European countries (the Netherlands, Poland and the Czech Republic). First, we discussed which descriptions of NPIs in the literature we agreed with [14, 26,27,28], since no clear definition of NPIs is available yet. Then, the teams from the different countries independently reported whether they considered the interRAI HC items NPIs or not (using the agreed definition/criteria for NPIs) and provided their argumentation. Subsequently, several consensus meetings were organized to discuss within the entire team which items were finally considered NPIs.
During these consensus meetings, we agreed that NPIs (1) involve interventions whose purpose is to improve, maintain or promote health or functioning; (2) aim to prevent, care or cure health problems, and have a measurable impact on health, quality of life, behavioral and/or socioeconomic markers; (3) are treatments which do not involve the use of drugs (but may be used in conjunction with pharmacological treatment); (4) are wide ranging in approach and encompass psychological, psychosocial, interpersonal, behavioral, emotional, exercise and environmental interventions; and (5) reflect a variety of approaches, and the creativity and commitment of many professional and lay carers of persons receiving care around the world.
We excluded diagnostic tools such as body sensors or pedometers, health campaigns focused on national level, variables that described a status more than something you could intervene with, such as walking performance or eating performance, and we excluded therapies we felt were pharmacological, such as oxygen therapy.
This eventually led to defining a list of 24 interventions we considered to be non-pharmacological among the available interRAI HC items. We assigned the interventions to seven groups by consensus: environmental interventions, physical activities, preventive measures, psychosocial interventions, regular care interventions, special aids and special therapies. The groups with corresponding NPIs can be found in Table 1.
For analysis, all NPIs were transformed into dichotomous variables, stating whether a person received a certain NPI or not. Some NPIs that were measured in number of days given, were assigned as provided if the specified NPI was provided at least 1 day of the week. Extensive descriptions of the content of the interventions and of the period of measurement of the NPIs can be found in Supplementary Table 1.
Demographics
Demographic characteristics included age, gender, living situation and country of residence. Living situation was defined as living alone or living with a person (e.g., partner, friend or other relative).
Clinical characteristics
Functional status was measured using the Activities of Daily Living Hierarchy scale (ADLH), with scores ranging from 0 (no impairment) to 6 (total dependence). Higher scores indicate more ADL limitations, and a score of ≥ 3 indicates the need for extensive ADL support [21, 29]. To assess the self-performance on IADL (Instrumental Activities of Daily Living) tasks, the Instrumental Activities of Daily Living Capacity scale (IADLC) was used. This scale consists of eight IADL tasks that can be rated from independent (0) to complete dependence (6). The scores for each of the tasks were cumulated and range from 0 (independent) to 48 (total dependence) [23].
Cognitive impairment was evaluated using the Cognitive Performance Scale (CPS), with scores ranging from 0 (no cognitive impairment) to 6 (very severe cognitive impairment) [30]. Cut-off scores of ≥ 3 were used to indicate presence of moderate to severe cognitive impairment.
Presence of depressive symptoms was assessed using the 15-point Depression Rating Scale (DRS) [31]. A score of ≥ 3 indicates presence of clinically relevant depressive disorders.
The interRAI instrument has been linguistically validated with forward and back translations in many languages including Dutch, Finnish, German, Icelandic and Italian [32]. Also, interrater and test retest reliability was studied extensively in many countries and found to be very good [22, 32]. The cognition and depression scales are calculated from specific items from the interRAI instrument.
Other clinical characteristics taken into account included falls in the last 30 days, presence of incontinence, dyspnea, pain and fatigue, and self-reported health.
Statistical analysis
Baseline characteristics were described using descriptive statistics such as mean and median. Descriptive statistics also provided an overview of the prevalence of NPIs in both the total sample and across the different European countries. We also counted the percentage of participants who received zero, one or more NPIs within each (previously defined) group of NPIs. All analyses were conducted with IBM SPSS statistics version 26 (IBM Corp., Armonk, NY, USA).
Results
In total, 2884 participants from six European countries were included. The mean age at baseline was 82.9 years. Of all participants, 66.9% were female, and 57.7% were living alone. The percentage of participants needing extensive support in ADL was 41.4% in the total sample (range 8.4–82%). In the total sample, 16.6% suffered from moderate to severe cognitive impairment (range 1.8–37.1%). There was also a large variability in IADL capacity score between country samples (range 15.6–38.9). The participants’ characteristics are presented in Table 2.
Prevalence of non-pharmacological interventions
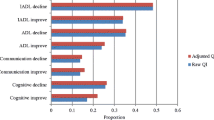
Supplementary Fig. 1 presents the ten most prevalent NPIs in the total homecare sample. The intervention with the highest prevalence was ‘emergency assistance available’ (74.1%), followed by ‘exercise or physical activity’ (68.9%) and ‘home nurse’ (61.9%).
Table 3 shows the prevalence of all NPIs in the total study sample, and within the six European countries. ‘Psychological therapy’ (0.6%) had quite a low prevalence. The proportion of older homecare clients receiving physical therapy was 14.6%, and the prevalence of occupational therapy was 5.6%. Physical restraints were present in 9.2% of the study sample.
Prevalence of non-pharmacological interventions in different European countries
As can be seen from Supplementary Fig. 1 and Table 3, there were considerable differences in the prevalence of NPIs between the different European countries. NPIs with large differences between countries (i.e., large range in prevalence) were ‘participation in social activities’ (8.5–58.8%.), ‘exercise or physical activity’ (17.0–96.7%), ‘home health aids’ (12.0–93.0%), ‘eye exam’ (16.7–59.8%), and ‘emergency assistance available’ (29.2–91.4%).
Prevalence of non-pharmacological interventions within the defined NPI groups
The prevalence of NPIs within different European countries was also analyzed with respect to previously defined NPI groups (Table 3 and Supplementary Fig. 1). Within the psychosocial interventions, ‘psychological therapy’ was rarely provided in all countries (0.2–1.2%). In the German sample, the prevalence of ‘occupational therapy’ was highest (22.3%) compared to the other countries (0.0–8.2%). Within the NPI group with regular interventions, there were large differences between the countries, with lowest prevalence in the Italian sample. In the German sample, there was a high prevalence of ‘physician visits’ (94.1%). In the group with special therapies, ‘wound care’ was most prevalent in the Belgian (15.8%) and the Italian samples (22.8%), ‘turning program’ and ‘toileting program’ were most prevalent in the Italian sample (15.2%; 6.8%). In the Finnish sample, nobody used a ‘turning program’ (0.0%). The group of NPIs with preventive measures included ‘physical restraints’, of which the prevalence was highest in the Italian sample (27.7%) and lowest in the Finnish sample (0.4%). Within the group with special aids a ‘urinary collection device’ was quite low prevalent, ranging from 1.3% in the Finnish sample to 18.0% in the Italian sample. The prevalence of ‘emergency assistance available’ within the environmental NPI group was high (74.1%), but ranges from 29.2% in the German sample to 91.4% in the Icelandic sample.
Number of interventions within the different groups of NPIs
In Table 4, the proportion of people receiving a certain number of interventions is shown across the different NPI groups. People in the Dutch sample received the highest number of physical activity interventions (15.9% receiving three or more interventions), and the highest number of preventive measure interventions (30.3% with two interventions and 8.7% with three or more interventions). The number of physical activity interventions was lowest in the Italian sample, with 79.0% receiving no interventions. In the Finnish sample, the number of preventive measures was the lowest with 71.3% of the study sample receiving no interventions from this group. The number of environmental interventions was highest in Iceland, with 48.7% of the sample receiving two interventions. Within the regular care group, the German sample showed 46.6% of the people receiving four or more interventions. Within the special aids group and the special therapies group, the differences between countries were smaller.
Discussion
This study described the prevalence of the provision or use of NPIs in homecare recipients across six European countries, as well as the number of homecare recipients receiving zero, one or more interventions within the different NPI groups. The prevalence of NPIs varied substantially, both within and across countries. Low prevalent interventions concerned ‘participation in social activities’, ‘psychological therapy’, ‘physical therapy’ and ‘occupational therapy’. The use of physical restraints was relatively high in the Italian and German samples. The fewest number of interventions per person occurred in the Italian sample.
In this homecare European study sample, the prevalence of certain interventions, such as ‘social participation’, ‘physical therapy’ and ‘occupational therapy’ was low. This is striking, because these are all interventions that may have a positive effect on different health outcomes. Physical and occupational therapy positively impact reducing the recurrence of falls and subsequent morbidity and mortality [33], and occupational therapy improves mobility, social participation and ADL functioning [34], and also daily functioning, particularly in people with dementia [35]. Moreover, physical activity improves ADL functioning in older people [36]. Social participation has a positive effect on cognitive, emotional and physical functioning in older people [37].
The relatively high prevalence of use of physical restraints in Italy and Germany may have a negative effect on health outcomes such as emotional wellbeing and physical functioning while evidence for their effectiveness on for instance fall prevention is lacking. Use of physical restraints has been associated with increased risk of falls, a decline in physical functioning, pain, mental health problems, a higher risk of pressure ulcers, incontinence and injuries [38,39,40,41].
When interpreting our results, it is important to consider that the organization and availability of care as well as the characteristics of the samples differ across European countries. Previous research has shown that the amount of formal care is higher in the Netherlands, Belgium and Scandinavian countries compared to Mediterranean countries where people receive more informal care [42]. In this study, the amount of informal care given in the Italian sample is also higher than in the other countries [21]. The ratio of formal and informal care varied substantially [43]. Future research may explore whether and how this may have impacted the uptake of various types of NPIs.
There were also sample differences between the different countries that might in part explain the differences between the use of NPIs. The Italian and Belgian samples had the highest numbers of people needing extensive ADL support (80.3 and 82.0%). Also, the number of people with moderate to severe cognitive impairment was highest in Italy, with 37.1%. This might partly explain the high number of physical restraints compared to the other countries, since one of the major risk factors for physical restraints use is cognitive impairment or dementia [40, 41]. It may also explain the low number of physical activity NPIs, because physical restraints are also more prevalent in people with impaired ADL or higher care dependency [40, 41]. Apart from this, there were also different eligibility criteria for homecare in different countries. In Italy, the indication for receiving homecare is aimed more at ADL-dependent and cognitively impaired persons. In the participating Italian region, the indication for receiving homecare was aimed at relatively severe ADL-dependence and cognitive impairment. As there is very little nursing home capacity in the Italian region (Umbria) included in this study, people are cared for at home much longer compared to the other countries. At the same time, homecare capacity is rather limited as well leaving much of the daily care with informal carers. Informal carers may be less aware of supportive interventions. Likely, this context drives the limited uptake of NPIs in Italy despite serving very care-dependent clients. In the Netherlands, Finland and Iceland, less impaired people are also eligible for homecare service provision. The differences between homecare eligibility and levels of dependency in these countries have been described previously [44].
Our study has some strengths and limitations. The strengths of our study are that data were collected using the standardized and validated interRAI HC instrument, available in various country-specific editions, in which assessors are specifically trained to ensure appropriate research and clinical use of this instrument. An advantage was also that all NPIs were explicitly and uniformly defined before analyses based on consensus of experts from several countries on the definition and selection of NPIs from the interRAI HC tool and classification of these NPIs into specific groups.
One of the limitations of the study is that the data are from 2014 to 2016, with no access to data from during or after the COVID-19 pandemic. However, comprehensive data on NPIs from multiple countries are relatively scarce. Our dataset is one of the few that allow such detailed international comparisons. Another limitation is that in some countries the sampling procedure might have contributed to selection bias. For example, in the Dutch study sample, one of the main reasons for refusal to participate in two of the three study sites was cognitive impairment, likely causing an underrepresentation of older persons with cognitive impairment [21]. The Belgian study sample was recruited from a nursing homecare organization, possibly causing the higher levels of ADL-dependency and cognitive impairment. This would also explain why all participants had a home nurse. Also, one of the inclusion criteria for this study was the expectation that participants would receive care for more than 6 months, so the results relate to people who received “long-term” homecare. This may influence the generalizability of the present study. People with acute or subacute conditions might require different NPIs such as physical or occupational therapy, psychological or speech therapy, pads or briefs worn or urinary collection device. Terminally ill persons were also excluded from the study population, so people receiving palliative care in this study sample were underrepresented. Another limitation is the fact that countries differ in their spending on and eligibility criteria for homecare, which may cause populations eligible for provision of homecare services to differ from country to country. Also, specific customs in provision of some NPIs may play a significant role in their higher provision, but these findings are also part of the results of our study.
Concerning the NPIs, we were dependent on the NPIs listed in the interRAI HC instrument. As a result, the list of NPIs might be incomplete. For example, specific nutritional interventions were not captured with this instrument. This can be seen as a limitation to the current study. Also, details about intensity and performance of NPIs were largely unknown. The assessment using the HC instrument is a snapshot, so we do not know if more NPIs are deployed during the treatment trajectory.
Also, we did not consider whether the study population did or did not have an indication for a particular NPI, which might cause an over- or underestimation of their prevalence.
There were large differences in the prevalence of different NPIs across European countries. Some interventions with positive effects were hardly used, such as ‘participation in social activities’, ‘psychological therapy’, ‘physical therapy’ and ‘occupational therapy’. Interventions such as ‘physical restraints’ were highly prevalent in the Italian and the German study samples but might have a negative impact on health outcomes such as emotional wellbeing.
Remarkably, several interventions with proven benefit were deployed only on a modest scale. The allocation criteria for NPIs differ substantially across countries. Nevertheless, it seems important to better understand the impeding and facilitating factors in the use of these potentially beneficial interventions in order to design successful uptake strategies. Also, further research into better implementation of these interventions in treatment guidelines might be needed. In most countries, better uptake of NPIs seems to be a window of opportunity to improve functioning and quality of life of homecare recipients.
References
European C, Directorate-General for Employment SA, Inclusion (2021) Long-term care report: trends, challenges and opportunities in an ageing society. Volume II, Country profiles: Publications Office
Leichsenring K, Billings J, Nies H (eds) (2013) Long-term care in europe: improving policy and practice. Palgrave McMillan, Houndmills
Tarricone RT, Agis D (2008) Home care in Europe: the solid facts: World Health Organization. Regional Office for Europe
Henrard JC, Ankri J, Frijters D, Carpenter I et al (2006) Proposal of a service delivery integration index of home care for older persons: application in several European cities. Int J Integr Care. https://doi.org/10.5334/ijic.159
Genet N, Boerma WGW, Kringos DS, Bouman A et al (2011) Home care in Europe: a systematic literature review. BMC Health Serv Res. https://doi.org/10.1186/1472-6963-11-207
Abraha I, Cruz-Jentoft A, Soiza RL, O’Mahony D, Cherubini A (2015) Evidence of and recommendations for non-pharmacological interventions for common geriatric conditions: the SENATOR-ONTOP systematic review protocol. BMJ Open 5(1):e007488. https://doi.org/10.1136/bmjopen-2014-007488
Sikkes SAM, Tang Y, Jutten RJ et al (2021) Toward a theory-based specification of non-pharmacological treatments in aging and dementia: focused reviews and methodological recommendations. Alzheimers Dement 17(2):255–270. https://doi.org/10.1002/alz.12188
Blackman J, Swirski M, Clynes J, Harding S, Leng Y, Coulthard E (2021) Pharmacological and non-pharmacological interventions to enhance sleep in mild cognitive impairment and mild Alzheimer’s disease: a systematic review. J Sleep Res 30(4):e13229. https://doi.org/10.1111/jsr.13229
Naci H, Ioannidis JP (2015) Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. Br J Sports Med 49(21):1414–1422. https://doi.org/10.1136/bjsports-2015-f5577rep
Montero-Odasso M, van der Velde N, Martin FC et al (2022) World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. https://doi.org/10.1093/ageing/afac205
National Institute for Health and Care Excellence (NICE) (2016) Multimorbidity: clinical assessment and management NG56. NICE, London. Available from: https://www.nice.org.uk/guidance/ng56
Bennett S, Laver K, MacAndrew M et al (2021) Implementation of evidence-based, non-pharmacological interventions addressing behavior and psychological symptoms of dementia: a systematic review focused on implementation strategies. Int Psychogeriatr 33(9):947–975. https://doi.org/10.1017/s1041610220001702
Zeisel J, Reisberg B, Whitehouse P, Woods R, Verheul A (2016) Ecopsychosocial interventions in cognitive decline and dementia: a new terminology and a new paradigm. Am J Alzheimers Dis Other Dement 31(6):502–507. https://doi.org/10.1177/1533317516650806
Olazarán J, Reisberg B, Clare L et al (2010) Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord 30(2):161–178. https://doi.org/10.1159/000316119
Cohen-Mansfield J (2001) Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique. Am J Geriatr Psychiatry 9(4):361–381
Abraha I, Rimland JM, Trotta FM et al (2017) Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia The SENATOR-OnTop series. BMJ Open 7(3):e012759. https://doi.org/10.1136/bmjopen-2016-012759
de Oliveira AM, Radanovic M, de Mello PC et al (2015) Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: a systematic review. Biomed Res Int 2015:218980. https://doi.org/10.1155/2015/218980
Kilpatrick KA, Paton P, Subbarayan S et al (2020) Non-pharmacological, non-surgical interventions for urinary incontinence in older persons: a systematic review of systematic reviews. The SENATOR project ONTOP series. Maturitas 133:42–48. https://doi.org/10.1016/j.maturitas.2019.12.010
Abraha I, Trotta F, Rimland JM et al (2015) Efficacy of non-pharmacological interventions to prevent and treat delirium in older patients: a systematic overview. The SENATOR project ONTOP series. PLoS ONE 10(6):e0123090. https://doi.org/10.1371/journal.pone.0123090
Rimland JM, Abraha I, Dell’Aquila G et al (2016) Effectiveness of non-pharmacological interventions to prevent falls in older people: a systematic overview. The SENATOR project ONTOP series. PLoS ONE 11(8):e0161579. https://doi.org/10.1371/journal.pone.0161579
van der Roest HG, van Eenoo L, van Lier LI et al (2019) Development of a novel benchmark method to identify and characterize best practices in home care across six European countries: design, baseline, and rationale of the IBenC project. BMC Health Serv Res 19(1):310. https://doi.org/10.1186/s12913-019-4109-y
Hirdes JP, Ljunggren G, Morris JN et al (2008) Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res 8(1):277. https://doi.org/10.1186/1472-6963-8-277
Landi F, Tua E, Onder G et al (2000) Minimum data set for home care: a valid instrument to assess frail older people living in the community. Med Care 38(12):1184–1190. https://doi.org/10.1097/00005650-200012000-00005
Morris JN, Fries BE, Steel K et al (1997) Comprehensive clinical assessment in community setting: applicability of the MDS-HC. J Am Geriatr Soc 45(8):1017–1024. https://doi.org/10.1111/j.1532-5415.1997.tb02975.x
InterRAI group. Secondary InterRAI group. http://www.interrai.org
Ninot G (2021) Defining non-pharmacological interventions. Non-pharmacological interventions: an essential answer to current demographic, health, and environmental transitions. Springer International Publishing, Berlin
Zucchella C, Sinforiani E, Tamburin S et al (2018) The multidisciplinary approach to Alzheimer’s disease and dementia. A narrative review of non-pharmacological treatment. Front Neurol 9:1058. https://doi.org/10.3389/fneur.2018.01058
Boutron I, Ravaud P, Moher D (2012) Randomized clinical trials of nonpharmacological treatments. Chapman and Hall/CRC, New York
Morris JN, Fries BE, Morris SA (1999) Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci 54(11):546–553. https://doi.org/10.1093/gerona/54.11.m546
Morris JN, Fries BE, Mehr DR et al (1994) MDS cognitive performance scale. J Gerontol 49(4):M174–M182. https://doi.org/10.1093/geronj/49.4.m174
Burrows AB, Morris JN, Simon SE, Hirdes JP, Phillips C (2000) Development of a minimum data set-based depression rating scale for use in nursing homes. Age Ageing 29(2):165–172. https://doi.org/10.1093/ageing/29.2.165
Onder G, Carpenter I, Finne-Soveri H et al (2012) Assessment of nursing home residents in Europe: the Services and Health for Elderly in Long TERm care (SHELTER) study. BMC Health Serv Res 12:5. https://doi.org/10.1186/1472-6963-12-5
Attar M, Alsinnari YM, Alqarni MS et al (2021) Common types of falls in the elderly population, their associated risk factors and prevention in a tertiary care center. Cureus 13(5):e14863. https://doi.org/10.7759/cureus.14863
De Coninck L, Bekkering GE, Bouckaert L, Declercq A, Graff MJL, Aertgeerts B (2017) Home- and community-based occupational therapy improves functioning in frail older people: a systematic review. J Am Geriatr Soc 65(8):1863–1869. https://doi.org/10.1111/jgs.14889
Graff MJ, Vernooij-Dassen MJ, Thijssen M, Dekker J, Hoefnagels WH, Rikkert MG (2006) Community based occupational therapy for patients with dementia and their care givers: randomised controlled trial. BMJ 333(7580):1196. https://doi.org/10.1136/bmj.39001.688843.BE
Chou CH, Hwang CL, Wu YT (2012) Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil 93(2):237–244. https://doi.org/10.1016/j.apmr.2011.08.042
Townsend BG, Chen JT, Wuthrich VM (2021) Barriers and facilitators to social participation in older adults: a systematic literature review. Clin Gerontol 44(4):359–380. https://doi.org/10.1080/07317115.2020.1863890
Abraham J, Hirt J, Richter C, Köpke S, Meyer G, Möhler R (2022) Interventions for preventing and reducing the use of physical restraints of older people in general hospital settings. Cochrane Database Syst Rev 8(8):Cd012476. https://doi.org/10.1002/14651858.CD012476.pub2
Spennato U, Lerjen N, Siegwart J et al (2023) Prevalence, risk factors and outcomes associated with physical restraint in acute medical inpatients over 4 years—a retrospective cohort study. Geriatrics (Basel). https://doi.org/10.3390/geriatrics8010015
Lam K, Kwan JSK, Wai Kwan C et al (2017) Factors associated with the trend of physical and chemical restraint use among long-term care facility residents in Hong Kong: data from an 11-year observational study. J Am Med Dir Assoc 18(12):1043–1048. https://doi.org/10.1016/j.jamda.2017.06.018
Gottschalk S, Meyer G, Haastert B, Abraham J (2023) Prevention of physical restraints in the acute care setting (PROTECT): study protocol for a cluster-randomised controlled pilot study. BMJ Open 13(1):e066291. https://doi.org/10.1136/bmjopen-2022-066291
Suanet B, Van Groenou MB, Van Tilburg T (2012) Informal and formal home-care use among older adults in Europe: can cross-national differences be explained by societal context and composition? Ageing Soc 32(3):491–515. https://doi.org/10.1017/S0144686X11000390[publishedOnlineFirst:2011/05/20]
van Hout HP, van Lier L, Draisma S et al (2019) Signs of inequality? Variations in providing home health care across care organizations and across European countries in the IBenC study. Health Serv Insights 12:1178632919837632. https://doi.org/10.1177/1178632919837632
Carpenter I, Gambassi G, Topinkova E et al (2004) Community care in Europe. The Aged in Home Care project (AdHOC). Aging Clin Exp Res 16(4):259–269. https://doi.org/10.1007/bf03324550
Funding
This study was carried out as part of the I-CARE4OLD project. I-CARE4OLD has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 965341. Views and opinions expressed are, however, those of the authors only and do not necessarily reflect those of the European Union. Neither the European Union nor the granting authority can be held responsible for them. More information on the I-CARE4OLD project can be found at http://www.icare4old.eu and https://cordis.europa.eu/project/id/965341. The IBenC project was funded by the 7th Framework Programme of the European Commission (Grant no. 305912). The contents of this article reflect only the authors’ views and the European Commission is not liable for any use that may be made of the information contained therein. JP and DF were supported by the Cooperation research program of the Faculty of Pharmacy, Charles University, Czech Republic.
Author information
Authors and Affiliations
Contributions
Study concept and design: HvH, KJ, EH. Acquisition of data: GO, AD, HF-S. Statistical analysis: EK. Drafting of the manuscript: EK. Data interpretation, critical revision, and approval of final version: EK, EH, JP, LS, KS, IB, AZ, DF, GO, AD, HF-S, MH, HvH, KJ.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and with permission from the IBenC consortium.
Ethical approval
Ethical approval was obtained before the start of the IBenC study from authorized medical ethical committees in each of the participating countries. Belgium (Flanders): Commissie Medische Ethiek van de Universitair Medische Ziekenhuizen Katholieke Universiteit Leuven, No. ML10265; Finland: Tutkimuseettinen työryhmä, No. THL/796/6.02.01/ 533/2014; Germany: Ethikkommission des Institut für Psychologie und Arbeitswissenschaft der Technische Universtität Berlin, No. GH_01_20131022; Iceland: Vísindasiðanefnd, No. 13–176-S1; Italy: Comitato Etico Università Cattolica del Sacro Cuore, No. 2365/14; The Netherlands: Medical Ethics Review Committee VU University Medical Center, No. 2013.333.
Informed consent
Informed consent was obtained from all study participants, except from routine care sites in Italy, Finland and one site in the Netherlands. In line with local regulations, informed consent from routine care clients was not necessarily required as these assessments were performed for clinical purposes by organizations’ own staff. Directly identifiable information of these clients was removed before transfer to the research teams, resulting in pseudonymized data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kooijmans, E.C.M., Hoogendijk, E.O., Pokladníková, J. et al. The prevalence of non-pharmacological interventions in older homecare recipients: an overview from six European countries. Eur Geriatr Med 15, 243–252 (2024). https://doi.org/10.1007/s41999-023-00868-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00868-w