Abstract
The ultimate aim of periodontal plastic surgery is to create optimal pink esthetics through the reconstruction of gingival recessions. Application of autogenous soft tissue grafts is considered as a gold standard treatment modality with predictable esthetic outcomes for gingival recession coverage. Harvesting a free soft tissue graft from an esthetically irrelevant region of the oral mucosa using various techniques can prevent donor site complications around the adjacent teeth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Quick reference/description
The ultimate aim of periodontal plastic surgery is to create optimal pink esthetics through the reconstruction of gingival recessions. Application of autogenous soft tissue grafts is considered as a gold standard treatment modality with predictable esthetic outcomes for gingival recession coverage. Harvesting a free soft tissue graft from an esthetically irrelevant region of the oral mucosa using various techniques can prevent donor site complications around the adjacent teeth.
Overview
Modalities for harvesting of autogenous soft tissue grafts | Indications |
|---|---|
Free gingival graft (FGG) harvesting technique | Harvesting FGG and partly epithelialized free gingival graft (PE-FGG) for coverage of gingival recession in esthetically less demanding regions |
Trap door technique | Harvesting subepithelial connective tissue graft (SCTG) for coverage of gingival recession in esthetically demanding regions |
Parallel incision technique | Harvesting SCTG for coverage of gingival recession Harvesting epithelialized-subepithelial connective tissue graft (ESCTG) and PE-FGG for gingival recession coverage |
Single incision technique | Harvesting SCTG with or without periosteum for coverage of gingival recessions |
Distal wedge technique | Harvesting FGG, SCTG or partly epithelialized connective tissue graft from maxillary tuberosity and mandibular alveolar tuberculum For esthetically intended graft harvesting indications, it can be adapted to individual patient characteristics |
Materials/instruments
-
No.15/C surgical blade
-
No.12 surgical blade
Procedure
Recreation of optimal pink esthetics is the final goal of periodontal plastic surgery by the reconstruction of gingival recessions. For augmentation of the gingival biotype and long-term maintenance of esthetics, while keeping patient morbidity at minimum, selection of the most appropriate grafting technique is a critical consideration in treatment planning. The most effective treatment approach for complete coverage of root surfaces with long-term tissue stability is autogenous soft tissue graft application that enhances the thickness and width of keratinized gingiva.
Autogenous free soft tissue grafts are obtained from a remote and esthetically unimportant part of the oral mucosa and are entirely detached from their donor region. This is useful in avoiding donor site complications surrounding the adjacent teeth. Therefore, minimal risk of impaired esthetics and root hypersensitivity is present by avoiding wound healing via secondary intention at the adjacent sites.
I. Autogenous soft tissue grafts
Free gingival graft
Nabers first used the term free gingival graft (FGG). Autogenous grafts are mainly harvested from the palate. FGG is nowadays less frequently used for the treatment of gingival recessions. It has high predictability of post-operative tissue stability and graft survival. Following transplantation to the recipient site, maintenance of the original tissue characteristics by the palatal soft tissue grafts with epithelial coverage is of immense clinical importance. Use of FGG induces favorable amount of keratinization, although with impaired esthetics due to differences in surface color and texture compared to adjacent sites.
Subepithelial connective tissue graft
The first grafting approach of choice for root coverage is subepithelial connective tissue graft (SCTG). In periodontal plastic surgery, one of the most esthetically predictable and versatile grafting procedures is transplantation of SCTG. For coverage of denuded root surfaces using the bilaminar reconstruction of lost gingival tissues, SCTG can be applied in conjunction with split-thickness pedicle-, tunnel-type or envelope flaps. SCTG application results in enhanced root coverage due to optimal blood supply. Excellent predictability and esthetics may be obtained with SCTG.
In case a change in gingival tissue surface characteristics is required or a significant increase in the width and thickness of keratinized gingiva is essential, SCTGs are not considered as the first grafts of choice, instead, FGG, PE-FGG or ESCTG may be applied. In cases with thin palatal masticatory mucosa and reduced amount of donor tissues, allogeneic and xenogeneic grafts should be considered instead of harvesting connective tissue from the hard palate.
The advantages of SCTG are:
Enhanced color match and improved esthetic results as the surface characteristics of the overlying flap are similar to that of the adjacent recipient gingiva.
Wound healing in the donor and recipient sites mostly occurs by primary intention when SCTG is covered by coronally advanced- or tunneled flaps via partial-thickness flap preparation.
This healing by primary intention can facilitate tissue maturation and decrease postoperative discomfort.
Partly epithelialized soft tissue grafts
Epithelialized-subepithelial connective tissue graft (ESCTG) combined with an envelope type flap is a treatment alternative combining the advantages of FGGs and SCTGs. In this technique, the epithelialized grafts are placed to cover the exposed root surfaces. Another grafting procedure is the partly epithelialized free gingival graft (PE-FGG) that is used for gingival recessions of the anterior mandible in conjunction with an apically repositioned flap. Both these grafting approaches provide:
Increased resistance against the tension of the muscular–mucosal environment
Lowering the risk for displacement of the mucogingival junction (MGJ) or flattening of the vestibule
Increased amount of keratinized tissues
Acceptable color blending compared to FGG
II. Anatomical considerations of choosing autogenous soft tissue graft donor sites
Harvesting autogenous soft tissue grafts is a technique sensitive procedure. Detailed knowledge of the donor region anatomy is crucial to avoid surgical complications. Hard palate is the donor site of choice in daily clinical practice; however, it can increase post-surgical patient morbidity. The various sites for harvesting autogenous soft tissue grafts are:
Hard palate
Maxillary tuberosity
Posterior part of the hard palate
Edentulous ridges (e.g., mandibular alveolar tuberculum)
Rarely, gingival donor site
An endodontic needle with a silicon stop can be utilized for evaluation of the tissue thickness at palatal donor sites. The masticatory mucosa in the maxillary tuberosity can be thicker (over 4 mm) as compared to the palate (3 mm) that permits harvesting of grafts of more volume in the absence of third molars, particularly if graft retrieval is performed 2–3 months after tooth extraction. It is indicated for coverage of gingival recession and the excessive volume also may enable graft harvesting for complete unilateral root coverage. SCTGs harvested from the maxillary tuberosity are firm with less post-surgical shrinkage and pronounced tendency for postoperative hyperplasia.
Another alternative to the hard palate as a donor site for autogenous soft tissue harvesting is the mandibular alveolar tuberculum in the absence of third molars. Graft harvesting from this site is less traumatic and can be used for treating mandibular recessions as the donor site is located close to the recipient teeth.
III. Soft tissue graft harvesting techniques
Free gingival graft harvesting
The hard palate as a donor site for harvesting FGG was first used by Sullivan and Atkins in 1968. The region distal from the canines, commencing at least 2 mm from the gingival margin with a width of 5–8 mm and a desirable length to cover the entire recipient site is an ideal site for harvesting a FGG from the hard palate for root coverage (Fig. 1). Harvesting of FGG is performed as follows:
The graft is prepared by outlining with two parallel longitudinal incisions that are interconnected with vertical incisions.
Graft deliberation is initiated along the paramarginal incision in a split-thickness fashion with a goal of removing an FGG of 1.5–2-mm thickness without touching the periosteum.
The harvested graft tissue can be utilized as a ready-to-use FGG, or it can be de-epithelialized to obtain an SCTG.
The donor site wound usually heals by secondary intention. Hence, epithelial ingrowth and shortening of healing time can be facilitated by several methods like:
Placement of native collagen sponges or matrices
Wound fixation with horizontal or crossed mattress sutures
Use of prefabricated acrylic plate for palate coverage to enhance blood clot stabilization
Trap door technique
In the trap door technique, first reported by Edel, the epithelium is not removed from the palate for harvesting a SCTG. The trap door technique includes (Fig. 2):
Mesial and distal vertical incisions are placed as per the graft dimensions.
A longitudinal incision extending from the mesial to distal aspect along the palate is placed to connect the releasing incisions and elevate a partial-thickness trap door.
Vertical incisions are extended 1 mm further over the intended apico-coronal graft dimension for improved access to the apical incision line that is used for harvesting a SCTG from below the trap door via a split-thickness sharp dissection as in the single incision technique.
Wound closure can be achieved by single interrupted or horizontal/modified crossed mattress sutures after harvesting the connective graft.
Parallel incision technique
The parallel incision technique was introduced by Langer and Calagna and is as follows (Fig. 3):
Two longitudinal parallel split-thickness incisions (similar to single incision technique) 8–10-mm deep into the palate are placed at 2- and 4-mm distances from the gingival margin with vertical releases at the mesial and distal ends of the incisions.
An incision is made at the connective tissue base between the vertical incisions to deliberate the graft from the palatal bone.
By removing the epithelial collar defined by the initial parallel incisions, a SCTG is obtained. In case ESCTG/PE-FGG is required, the parallel incision harvesting technique depicts a favorable approach without de-epithelialization.
Single-incision technique
The single-incision technique was introduced by Hürzeler and Weng in 1999 and is described as (Fig. 4):
A single full-thickness incision is made with a no. 15 surgical blade at 90º to the palatal bone.
The blade is then angled from 135° to 180º for undermining the palatal masticatory mucosa in split thickness, not deeper than 8 mm from the single incision, towards the palatal midline. Note: A no. 15 scalpel blade can be used as a reference as it has a cutting edge length of 8 mm.
Following a palatal envelope opening, a SCTG is harvested by making incisions on the mesial, distal, and apical aspects of the connective tissue within the opened envelope.
This technique should be performed carefully to avoid the greater and lesser palatine nerves and vessels. Incisions should be limited to the distal of the canine to avoid the greater palatine nerve and artery.
The incision should be placed at least 2 mm apical from the gingival margin of the teeth while harvesting a graft to prevent necrosis of the marginal tissues during donor site healing due to impaired collateral blood supply.
The SCTG can be harvested with or without periosteum. A SCTG without periosteum has better mechanical properties; however, in case of a thin masticatory mucosa, can have high negative postoperative consequences. The single-incision technique provides the most favorable postoperative healing when achieving primary intention wound healing. The chief advantages of the single incision technique are:
Simplified closure of the wound
Postoperative healing of donor site by primary intention
Decrease in blood supply compromise
Distal wedge technique
The distal wedge technique was originally introduced for correction of soft tissue excess on the distal sides of maxillary second molars during resective procedures for periodontal pocket elimination. As per individual patient characteristics, this technique can be adapted for esthetically intended graft harvesting indications. The graft harvesting site can be extended if the most distal tooth is a first molar, while graft dimensions are limited in the presence of the third molar.
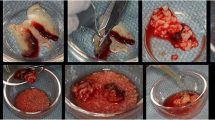
The distal wedge technique can also be applied to harvest FGGs, SCTGs, or partly epithelialized connective tissue grafts from the maxillary tuberosity and the mandibular alveolar tuberculum. The distal wedge procedure is performed as follows (Fig. 5):
Two mesio-distal, apically diverging incisions are place for outlining the graft region with a trapezoid cross section. The incisions should begin from the distal surface of the last adjacent tooth and are extended to the most distal aspect within the masticatory mucosa.
The incisions can be placed in a way that they outline a rectangular or a triangular graft shape from the occlusal view.
The distal wedge technique can be performed simultaneously with wisdom tooth extraction. However, it is preferable that graft harvesting be performed approximately 2 months after tooth extraction for increased amount of connective tissue at the donor site. The donor wound can be closed after a slight buccal split-thickness flap mobilization in most cases. In only few cases, limited patient complaints are associated with secondary intention wound healing. Hence, the distal wedge technique is one of the most preferred autogenous graft harvesting approaches due to high quality of harvested tissues and low patient morbidity.
IV. Healing of autogenous soft tissue grafts
A long epithelial junction is formed due to reparative healing during integration of the autogenous soft tissue grafts. Actual periodontal regeneration is observed only at the crest of alveolar bone.
Pitfalls and complications
-
Two major common complications associated with FGG use are over-augmentation of tissue contours due to graft hyperplasia and impaired color blending between the graft and recipient site. Therefore, the use of FGG is not a valid treatment alternative in esthetically demanding situations.
-
SCTGs when used in combination with tunneled or pedicle flaps can result in impairment of graft stability leading to graft failure in case of intense muscle pull or high frenal attachments.
-
SCTGs harvested from the maxillary tuberosity may be associated with graft hyperplasia and scar formation.
-
Complications of palatal FGG harvesting are:
Donor site pain
Post-operative bleeding
Prolonged healing
-
Donor site-associated complications following the use of the trap door technique due to vertical incisions are:
Secondary intention wound healing
Post-operative bleeding
-
In certain cases, donor site necrosis and pain can occur following the single incision or with the parallel incision technique.
Further reading
A. Kasaj (ed.), Gingival Recession Management, https://doi.org/10.1007/978-3-319-70719-8_8 Recession Coverage Using Autogenous Grafts
Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi GE, Stavropoulos A, Sculean A (2012) Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions- a systematic review. Quintessence Int 43(7):545–554
Zuhr O, Bäumer D, Hürzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol 41(Suppl 15):S123–S142
Benninger B, Andrews K, Carter W (2012) Clinical measurements of hard palate and implications for subepithelial connective tissue grafts with suggestions for palatal nomenclature. J Oral Maxillofac Surg 70(1):149–153
Cairo F, Nieri M, Pagliaro U (2014) Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J Clin Periodontol. 41(Suppl 15):S44–S62
Acknowledgements
Open access funding provided by Semmelweis University (SE). This work was supported by the Hungarian Human Resources Development Operational Program (EFOP-3.6.2-16-2017-00006).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Windisch, P., Molnar, B. Harvesting of autogenous grafts for gingival recession coverage. Clin Dent Rev 3, 17 (2019). https://doi.org/10.1007/s41894-019-0056-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41894-019-0056-6