Abstract
Metacognitive therapy (MCT) is a transdiagnostic treatment approach with substantial empirical support that is well suited to be delivered in a group format. The present study reports on data from a service evaluation of generic group metacognitive therapy delivered to individuals seeking treatment for major depressive disorder (MDD) at a specialized mental health outpatient clinic. A total of 17 patients diagnosed with MDD where comorbidity was frequent received 10 sessions of generic group MCT delivered by two therapists. Group MCT was associated with large effect sizes for symptoms of depression, anxiety, interpersonal problems, self-esteem, general functioning, dysfunctional metacognitions, and treatment satisfaction was very high. The average number of therapist sessions used to treat each patient was seven. These preliminary findings support the continued use and evaluation of group MCT for patients seeking treatment for depression in specialized mental health care which likely is a cost-effective treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depression refers to the presence of depressed mood or diminished interest in activities for at least 2 weeks with a range of associated emotional, cognitive, physical, and behavioral symptoms (ICD-11; World Health Organization, 2019; DSM-5; American Psychological Association, 2013). Depression severity exists along a continuum and is composed of symptoms which may vary in frequency and intensity, duration of the disorder, and the impact on personal and social functioning (National Institute for Health and Care Excellence [NICE], 2022). Among individuals with major depressive disorder (MDD), comorbidity is common and anxiety disorders (Saha et al., 2021), substance use (Hunt et al., 2020), and personality disorders (Friborg et al., 2014) are frequent. In Norway’s specialized mental health care services, depression is the most common cause of treatment (Norwegian Institute of Public Health, 2021) and cost-effective interventions that can effectively modify the mechanisms of disorder in this context are therefore highly needed.
One promising treatment approach is metacognitive therapy (MCT; Wells, 2009) which is based on the Self-Regulatory Executive Functioning (S-REF) model (Wells & Matthews, 1994). For a brief history on the development and theoretical basis of the metacognitive model and treatment, see Capobianco and Nordahl (2023). This model asserts that psychological disorder results from a common set of processes called the cognitive attentional syndrome (CAS) which includes perseverative negative thinking (e.g., rumination and worry), inflexible attention and threat monitoring, and dysfunctional behavioral strategies that maintains extended negative styles of thinking.
The content/themes of the CAS may vary across disorders (e.g., worrying is more linked to anxiety and rumination more to depression; some worry about health and others about social interaction) but more important than the themes are the extent and duration of these processes. Thus, the CAS may account for the overlap between symptom domains and comorbidity. The configuration of the CAS is assumed to stem from biases in underlying metacognition, which can be observed in the form of beliefs about thinking hypothesized to be stored in an underlying metacognitive control system (Wells, 2019). Specific metacognitions concerning the uncontrollability of thoughts (e.g., “I cannot control my thinking”) are considered central, occurring in most disorders, while others are more specific in content, making additional contributions to particular disorders.
In specialized mental health care settings, cases with repeated depressive episodes, treatment resistance, ambivalence to change, and comorbidity/complex presentations are common. These patients often hold metacognitive beliefs that the mind/brain is defective or damaged. In some cases, metacognitive beliefs about self-knowledge are important in strategy selection (i.e., CAS activation) and related to personality difficulties, while in others, dysfunctional metacognitive goals interferes with disengagement from rigid self-attention and CAS strategies. On the surface, these more complex dynamics of positive and negative metacognitive beliefs can be seen as self-sabotage, ambivalence, or resistance to improvement and change (Wells, 2019). Nonetheless, these dynamics of dysfunctional metacognitive knowledge prevent the individual discovering and applying the metacognitive control that they have and thus prevents reflexive self-regulation and recovery.
MCT was specifically developed to modify dysfunctional metacognitions and remove the CAS in response to cognitive events (i.e., thoughts), feelings, and stressors. There is growing evidence including data from several randomized controlled trials showing that MCT is an effective and brief treatment for a range of disorders (Normann & Morina, 2018). MCT for MDD is associated with substantial improvement and is a feasible approach for individuals with different presentations of depression and can also be delivered in a group format (see Wells & Nordahl, 2023 for a summary of the evidence).
Diagnosis-specific MCT has been developed for several disorders including MDD (Wells, 2009). However, in heterogenous and comorbid samples, generic/transdiagnostic (i.e., not disorder specific) MCT may be a good treatment approach as it provides balance between sufficient specificity in addressing universal metacognitive mechanisms of change (i.e., uncontrollability beliefs) and individual presentations of dysfunctional metacognitive knowledge and personal needs (Wells, 2009). In support of this notion, Johnson et al. (2017) found that transdiagnostic MCT was more effective than disorder-specific CBT from pre- to post-treatment in a sample of patients with anxiety disorders and substantial comorbidity. Furthermore, a generic approach may be especially suitable in a group format where patients present with overlapping but also different symptoms and disorders and where the aim is to formulate and address symptoms and low function across diagnostic categories.
Adding to the benefits of taking a generic approach, delivering MCT in a group format may be a good alternative as it is an effective use of therapists’ time, and it facilitates emphasizing the importance of thinking style and similarities between disorders rather than the differences between them which may be a useful discovery (i.e., normalization). Two previous studies have evaluated transdiagnostic MCT delivered in a group format. In the first, Capobianco et al. (2018) reported that transdiagnostic group MCT was associated with large effect sizes and that the treatment was more effective than Mindfulness Based Stress Reduction in treating symptoms of anxiety and depression in patients recruited from mental health and counselling services. In the second, Callesen et al. (2019) reported that transdiagnostic group MCT was associated with large effect sizes for symptoms of anxiety and depression in patients seeking treatment at a private outpatient clinic. While these two studies report encouraging results, both included patients based on self-report rather than a thorough clinical assessment and may therefore not generalize to specialized mental health care samples.
An important question is whether group MCT can be an effective and cost-effective treatment option in naturalistic settings where those seeking treatment for depression often present with comorbid disorders, heterogenous backgrounds in terms of duration and severity of disorder, and treatment history. We argue that heterogeneity is the norm among those being referred to treatment for depression in specialized mental health care. Therefore, the aim of the current study was to evaluate the effects associated with generic group MCT for MDD and related symptoms and dysfunction delivered in a routine specialized mental health care service where data was collected as part of a larger service evaluation. Evaluating treatment effects in naturalistic settings may be especially informative as it relates directly to what effects can be achieved in “the real world” and thus be perceived as particularly relevant by clinicians working in this type of services. Consistent with metacognitive theory (Wells, 2019), we expected that the treatment would be associated with improvements in depression but also in a broad range of symptoms and dysfunction, and with change in dysfunctional metacognitive beliefs. In addition, we report on resource requirements and client satisfaction as important parameters in evaluating the relevance of the approach in this type of setting.
Methods
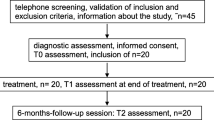
Design and Procedure
The study was conducted as part of an ongoing service evaluation of treatments offered at a specialized mental health outpatient clinic in Trondheim, Norway. A total of 17 patients (three groups of patients consisting of 5, 6, and 6 patients) seeking treatment for and diagnosed with MDD received generic group MCT. The Regional Committees for Medical and Health Research Ethics approved the service evaluation (Ref no: 31836/2019) and all participants provided informed consent to participate.
All patients were referred to the outpatient clinic from their general practitioner due to major depression and evaluated by the hospital intake team before being assessed at the clinic in accordance with standard procedure. All patients underwent a thorough diagnostic assessment using MINI-plus (Sheehan et al., 1998) and SCID-II (First et al., 1997), a battery of self-report measures, and assessment of any risk for harm or suicide. To be eligible for the treatment, participants were evaluated up against the following inclusion criteria: (1) signed written informed consent, (2) seeking help for depressive symptoms and diagnosed with major depressive disorder (DSM-5; APA, 2013), (3) 18 years or older. Exclusion criteria included (1) unable to participate at the scheduled times for the treatment, (2) known somatic diseases in need of medical treatment or that could interfere with treatment delivery, (3) psychosis, (4) current suicide intent in need of special treatment/assessment, (5) diagnosed cluster A or B personality disorder, (6) developmental disorders/cognitive disability, (7) substance dependence, and (8) patients not stable (started up or quit medication later than 3 months prior to referral) or not willing to remain stable on psychotropic medication during the treatment.
Participants
Of the 17 patients, 7 (41.2%) were women and 10 (58.8%) were men. Ages ranged from 22 to 55 (M = 31.1, SD = 8.9). The mean average number of diagnoses per patient was 2.12 (SD = 0.86) where 5 had a depressive disorder as their sole diagnosis, 5 had two diagnoses, and 7 had 3 diagnoses. Regarding diagnoses of depression, 11 had a recurrent depressive disorder (current episode moderate) and 6 had a moderate depressive episode. The most common comorbid axis 1 disorder was social phobia (N = 5) followed by generalized anxiety disorder (N = 4) and obsessive–compulsive disorder (N = 2). The most common comorbid axis II disorder was obsessive–compulsive personality disorder (N = 4) followed by avoidant personality disorder (N = 2), and mixed personality disorder (avoidant and obsessive–compulsive personality disorder) (N = 2). Two patients in addition had a problematic use of substances (mainly cannabis and alcohol) which did not meet criteria for a substance use disorder. Eight patients had received treatment before either in the specialized mental health service or private clinics as adults and 3 were on stable doses of antidepressant medication. We did not have a complete record of treatment received during childhood and adolescence, but several (at least 4) had also received treatment before adulthood. In terms of civil status, 3 were in a relationship, 4 cohabitants, 6 single, and 4 married. Regarding work status before treatment, 8 were either partially (n = 3) or completely (n = 5) on sick leave due to mental health problems, 9 were either students (n = 4) or working (n = 5). Those that were students all struggled with their ability to study and according to self-report underperformed in study activities compared to normal.
Measures
Self-report measures were administered at pre- and post-treatment. Pre-treatment scores were obtained during the last 2 weeks before starting the treatment, while post-treatment scores were obtained during the first week after the last session.
The primary outcome measures were the Patient Health Questionnaire (PHQ-9: Kroenke et al., 2001) which assesses depression severity, and the Generalized Anxiety Disorder 7 (GAD-7; Spitzer et al., 2006) which assesses symptoms of generalized anxiety. In addition, several secondary outcome measures were used to evaluate the transdiagnostic effects associated with group MCT: The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) assesses social anxiety symptoms, the Inventory of Interpersonal Problems (IIP-32; Barkham et al., 1996) assesses levels of interpersonal problems, the Work and Social Adjustment Scale (WSAS; Mundt et al., 2002) assesses impairments in general functioning, the Rosenberg Self-Esteem Scale (SES; Rosenberg, 2015) assesses self-esteem, and the Metacognitions Questionnaire-30 (MCQ-30; Wells & Cartwright-Hatton, 2004) assesses general dysfunctional metacognitive beliefs. In addition, the Client Satisfaction Questionnaire (CSQ-8; Attkisson & Greenfield, 2004) was administered at post-treatment to evaluate treatment satisfaction.
Group Metacognitive Therapy
The treatment was provided by the first and last authors who are clinical psychologists. ERS is accredited as an MCT-I® registered level I therapist, and HN is accredited as an MCT-I® registered level II therapist. Generic group MCT comprised 10 weekly sessions of approximately 90-min duration (2 × 45 min with a 15-min break). MCT followed the generic treatment plan outlined in Wells (2009, p. 250–255) and included identification and modification of more advanced level positive and negative metacognitive beliefs that are taught as part of MCT masterclass level II training provided by MCT Institute® and Adrian Wells. The generic approach was chosen by means to address both universal (e.g., beliefs about uncontrollability of thinking) and more specific/individual metacognitive beliefs (e.g., beliefs that negative thinking can hinder negative life events) among our patients in a group setting. The goal was to exploit the transdiagnostic potential in group MCT as much as possible with an aim to achieve a broad impact on symptom domains for all the individuals across individual diagnostic status, severity, vulnerabilities, background, and treatment history.
Throughout the treatment, we emphasized the separation between external stressors, symptoms/cognitive events (i.e., “trigger thoughts”), metacognitive strategies (i.e., the CAS), and dysfunctional metacognitive beliefs. This separation helps with shaping participants’ expectations about change and treatment content and facilitates the discovery that one has control over thinking, irrespective of negative thoughts, feelings, and external stressors. A key point here is that external stressors, feelings, or negative thoughts are not the central issue, but rather how we respond and self-regulate which again can be traced back to metacognitive knowledge. In each session, we addressed metacognitive beliefs (through a combination of verbal and experimental techniques), metacognitive awareness (e.g., become aware that negative thoughts are separate from the self and the world), and CAS strategies (getting to know their consequences and contrasting CAS strategies with detached mindfulness (DM; Wells, 2005)). Patients were given homework between every session (e.g., DM and worry postponement) and shared their experiences with the group in the following session (e.g., what do these experiences tell us about mental control). In the final treatment phase, therapy blueprints were developed which contained summaries of the material covered in treatment and plans for how to respond to cognitive events, feelings, and stressors in the future. More details about MCT can be found in Wells (2009).
Statistical Analyses
IBM SPSS version 27 was used to conduct all the analyses. We had no missing data. To examine potential changes in the outcome variables from pre- to post-treatment, we applied paired samples t-tests and evaluated effect sizes based on Cohen’s d (Cohen, 1988). Jacobson and Truax (1991) criteria for defining recovery and clinically significant change were applied to classify patients in four categories (recovered, improved, no change, worsened) for depression (PHQ-9) and anxiety (GAD-7) at post-treatment based on norm data (Kroenke et al., 2001; Löwe et al., 2008). For PHQ-9, reliable change is 6 points and in addition a total score of 6 or less at post-treatment is required for classifying patients as recovered. For GAD-7, reliable change is 4 points and in addition a total score of 7 or less at post-treatment is required for classifying patients as recovered.
Results
Treatment Attendance and Resource Requirements
All patients completed the treatment, and session attendance was high. Four of the patients had absences due to sickness of which one missed three sessions while the others missed one session. This observation suggests that group MCT was acceptable and lacked significant problems linked to engaging with the treatment.
The mean number of therapist hours required to treat each patient in our study was calculated with the following formulae: number of treatment sessions (i.e., 10) × number of hours per treatment session (i.e., 2 × 45 min) × number of therapists (i.e., 2) × number of groups (i.e., 3) divided by number of patients treated (i.e., 17) which is equal to 7.06 treatment sessions (of 45 min) to treat each patient and to achieve the following results.
Treatment Outcomes
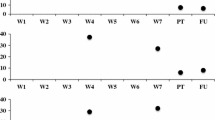
Table 1 presents mean scores at pre- and post-treatment on the included measures as well as change scores, t-statistics, and effect size calculations with Cohen’s d. The average depression score in the sample at pre-treatment was high, and 14 of the participants had a score of 16 or above on the PHQ-9 which is considered severe depression according to NICE (2022). In total, the treatment was associated with a significant and large improvement in depressive symptoms from pre- to post-treatment (d = 1.85). The sample also significantly improved on all other outcome measures, and the effect sizes were large with the exception of social anxiety which showed a moderate effect size.
Regarding sick leave, three out of the eight (37.5%) that were on sick leave before treatment remained on sick leave following treatment, while the five others (62.5%) returned to work.
Clinically Significant Change
To evaluate the level of clinically significant change, we applied the criteria by Jacobson and Truax (1991) to (1) the PHQ-9 where a change of ± 6 indicates a reliable and clinically significant change, and a score of ≤ 6 indicates normal levels of depression based on norm data (Kroenke et al., 2001); and (2) the GAD-7 where a change of ± 4 indicates a reliable and clinically significant change, and a score of ≤ 7 indicates normal levels of anxiety based on norm data (Löwe et al., 2008). By comparing individual pre- and post-treatment scores, a patient can be classified as (1) worsened, (2) no change, (3) improved, and (4) recovered, for each of these measures. Table 2 shows the number of patients falling into the different categories for the PHQ-9 and GAD-7 separately.
Client Satisfaction
We utilized the Client Satisfaction Questionnaire (CSQ-8) to assess overall levels of satisfaction with the treatment received. The CSQ-8 total score ranges from 8 to 32. At post-treatment, the mean score in our samples was 26.94 (SD = 3.34, range from 22 to 32), indicating high overall levels of satisfaction across the participants.
Discussion
The results of this preliminary evaluation of generic group MCT for individuals with MDD treated in specialized mental health care are promising and suggest it is cost-effective in terms of therapist’ time while retaining large and clinically meaningful improvements across a range of outcome measures.
A generic MCT approach was chosen due to the heterogenous presentations that are typical of individuals with depression in specialized mental health care settings with the aim to address important metacognitive mechanisms of change across disorders and symptom domains. There was no drop-out from the treatment, attendance was high, and client satisfaction was very good, indicating that the treatment was well received.
In specialized mental health services, the amount of treatment required to achieve significant clinical improvement is an important factor as resources are scarce compared to referrals. Group delivery of treatment can therefore be a good option if the clinical response achieved is not inferior to more traditional ways of delivering treatment. In our study, the mean number of therapist sessions (45 min) required to treat each patient was seven.
With a mean number of seven therapist sessions to treat each patient in this study, generic group MCT was associated with a large improvement in depression and anxiety symptoms from pre- to post-treatment at the group level. Using stringent criteria to assess clinically significant change based on norm data from the general population, six of the patients were classified as recovered and eight as improved using the PHQ-9, while 11 were classified as recovered and four as improved using the GAD-7. Note that using Jacobson and Truax (1991) criteria with the PHQ-9 based on norm data from the general population to classify someone as recovered is very stringent taking into consideration the severity levels and PHQ-9 pre-scores of our patients, that the post-assessment was conducted in the first week following the last session (i.e., little time for reflexive adaptation following removal of the CAS and dysfunctional metacognitions), and as the PHQ-9 corresponds to diagnostic criteria of depression (Kroenke et al., 2001) to a larger extent than some other self-report measures frequently used in depression research (Fried, 2017).
The finding that more patients were classified as recovered from their anxiety symptoms compared to depression could be related to the fact that MDD was the primary disorder of the participants, and thus it could be more difficult to achieve a full recovered status with regard to symptoms of depression as assessed with self-report. However, the effect size was largest for symptoms of depression compared to symptoms of anxiety for the group as a whole. In addition, the combined number of patients in the categories recovered or showing a reliable clinical improvement was similar across anxiety and depression. None of the patients deteriorated on any of the included measures.
Furthermore, generic group MCT was associated with large improvements in interpersonal problems, general functioning, and self-esteem. Social anxiety symptoms improved moderately at the group level which could be related to the mean score and standard deviation for SIAS at pre-treatment indicating that the level of social anxiety at the group level was moderate before treatment but with high variation, which suggests that the social anxiety scores among the participants were heterogenous. At post-treatment, there is a significant reduction at the group level, but the individual variation is still high (as indicated by the standard deviation). Overall, the results indicate broad effects of the treatment across several domains of symptoms and functioning. This finding concurs with a recent meta-analysis by Normann and Morina (2018) where they found that MCT in addition to producing large effects on primary outcome measures also produced large effects on comorbid problems which is in line with the notion that MCT targets transdiagnostic processes for psychopathology (Wells, 2019). Participants also demonstrated significant and large reductions in dysfunctional metacognitive beliefs, a finding that is consistent with the idea that metacognitive change is a mechanism of symptomatic change, and that dysfunctional metacognitions underlie a range of symptom domains and psychological dysfunction (Wells, 2019).
Our results are encouraging considering that the treatment was delivered in a naturalistic setting within a specialized mental health service and as several of the cases treated presented with comorbid disorders and various backgrounds and challenges. However, we note that the effect size for self-reported depression symptoms pre- to post-treatment in our trial is somewhat lower than what have been reported in previous open trials of disorder-specific MCT for MDD, including samples with more severe cases. In patients with treatment-resistant depression, Wells et al. (2012) reported an effect size of 1.65 and 2.71 (Cohen’s d) for depression measures from pre- to post-treatment. In a sample of patients with MDD and comorbid disorders, Hjemdal et al. (2017) reported an effect size of 2.89 (Hedge’s g) from pre- to post-treatment. Winter et al. (2019) reported that patients with persistent depressive disorder responded equally well to MCT as those with MDD and reported a within-group effect size of 3.40 (Cohen’s d). One explanation could be that disorder-specific MCT is more effective than a generic approach. Alternatively, group MCT may be less effective than individual MCT, but this suggestion does not fit with previous group MCT studies for MDD. For example, Papageorgiou and Wells (2015) treated treatment-resistant depression over 12 weekly group sessions of 2 h and two booster sessions and reported an effect size (Hedge’s g) of 2.88 pre- to post-treatment. However, when we compare our results to the two studies reporting on the effects of transdiagnostic/generic MCT delivered in a group format, they are quite similar. Capobianco et al. (2018) reported a pre- to post-treatment effect size of 1.38 on the Hospital Anxiety and Depression Scale (HADS), and 65% showed a reliable change according to Jacobson’s criteria. Callesen et al. (2019) similarly treated 131 self-diagnosed patients with 6 sessions of group MCT and reported an effect size of 1.73 (Cohen’s d) for treatment completers on the HADS from pre- to post-treatment. In this study conducted in a private practice setting, 66.7% of the completers were classified as recovered, 12.9% as improved, 17.2% with no change, and none as worsened based on Jacobsen criteria.
Strengths with our study includes the naturalistic setting that the treatment was delivered in, and that we were able to assess clinical diagnoses before treatment and a range of symptom domains and difficulties before and after treatment. However, there are several important limitations to our study that must be acknowledged. We did not have a baseline period to offer some control for symptom fluctuations before treatment started. The uncontrolled design means that we cannot partial out the effects of treatment from non-treatment-related influences on symptoms. As the study was part of a routine service evaluation, no post-assessment of diagnoses was conducted, and the patients were not followed up after being discharged from the clinic. Therefore, we cannot evaluate diagnostic status of the participants following the intervention and we do not have information about the long-term effects. Since patients with MDD are especially prone to experience relapse of depressive episodes, it must be considered a major limitation that we did not collect follow-up data. The sample size was relatively low and only three groups were included in this preliminary evaluation. The same two therapists delivered all the treatment. Reliability data for the diagnostic assessments were not available although they were confirmed following discussions among clinicians and specialists in clinical psychology at the clinic. We did however use the PHQ-9 as the primary outcome measure which is directly related to the diagnostic criteria of MDD in the DSM-IV/5 (Kroenke et al., 2001). Nonetheless, our study indicates that group MCT may be a good and potentially cost-effective treatment option for patients with MDD in specialized mental health care. Future studies with a stronger research design, assessment of long-term effects, and larger samples are warranted to further evaluate the effectiveness of group MCT in this setting. Further, as we in the current study utilized the generic MCT approach to accommodate for heterogeneity among the patients, future studies could also evaluate the specific treatment protocol for depression versus a generic approach in a similar treatment context to determine which are the most suitable and effective.
Data Availability
Data for the current study were collected as part of routine clinical care and are therefore not available for dissemination.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington. https://doi.org/10.1176/appi.books.9780890425596
Attkisson, C. C., & Greenfield, T. K. (2004). The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (pp. 799–811). Lawrence Erlbaum Associates Publishers
Barkham, M., Hardy, G. E., & Startup, M. (1996). The IIP-32: A short version of the Inventory of Interpersonal Problems. British Journal of Clinical Psychology, 35(1), 21–35. https://doi.org/10.1111/j.2044-8260.1996.tb01159.x
Callesen, P., Capobianco, L., Heal, C., Juul, C., Find Nielsen, S., & Wells, A. (2019). A preliminary evaluation of transdiagnostic group metacognitive therapy in a mixed psychological disorder sample. Frontiers in Psychology, 10, 1341. https://doi.org/10.3389/fpsyg.2019.01341
Capobianco, L., & Nordahl, H. (2023). A brief history of metacognitive therapy: From cognitive science to clinical practice. Cognitive and Behavioral Practice. https://doi.org/10.1016/j.cbpra.2021.11.002
Capobianco, L., Reeves, D., Morrison, A. P., & Wells, A. (2018). Group metacognitive therapy vs. mindfulness meditation therapy in a transdiagnostic patient sample: A randomised feasibility trial. Psychiatry Research, 259, 554–561. https://doi.org/10.1016/j.psychres.2017.11.045
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic.
First, M. B., Gibbon, M. L., Spitzer, R. L., Williams, J. B. W., & Benjamin, L. S. (1997). Structured clinical interview for DSM-IV Axis II personality disorders, (SCID-II). Washington, DC: American Psychiatric Press, Inc.
Friborg, O., Martinsen, E. W., Martinussen, M., Kaiser, S., Øvergård, K. T., & Rosenvinge, J. H. (2014). Comorbidity of personality disorders in mood disorders: A meta-analytic review of 122 studies from 1988 to 2010. Journal of Affective Disorders, 152, 1–11. https://doi.org/10.1016/j.jad.2013.08.023
Fried, E. I. (2017). The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders, 208, 191–197. https://doi.org/10.1016/j.jad.2016.10.019
Hjemdal, O., Hagen, R., Solem, S., Nordahl, H., Kennair, L. E. O., Ryum, T., ... & Wells, A. (2017). Metacognitive therapy in major depression: An open trial of comorbid cases. Cognitive and Behavioral Practice, 24(3), 312–318. https://doi.org/10.1016/j.cbpra.2016.06.006
Hunt, G. E., Malhi, G. S., Lai, H. M. X., & Cleary, M. (2020). Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: Systematic review and meta-analysis. Journal of Affective Disorders, 266, 288–304. https://doi.org/10.1016/j.jad.2020.01.141
Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006X.59.1.12
Johnson, S. U., Hoffart, A., Nordahl, H. M., & Wampold, B. E. (2017). Metacognitive therapy versus disorder-specific CBT for comorbid anxiety disorders: A randomized controlled trial. Journal of Anxiety Disorders, 50, 103–112. https://doi.org/10.1016/j.janxdis.2017.06.004
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 266–274. https://www.jstor.org/stable/40221654
Mattick, R. P., & Clarke, J. C. (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36, 455–470. https://doi.org/10.1016/S0005-7967(97)10031-6
Mundt, J. C., Marks, I. M., Shear, M. K., & Greist, J. M. (2002). The Work and Social Adjustment Scale: A simple measure of impairment in functioning. The British Journal of Psychiatry, 180(5), 461–464. https://doi.org/10.1192/bjp.180.5.461
National Institute for Health and Care Excellence. (2022). Depression in adults: Treatment and management. [NICE Guideline No. NG222]. https://www.nice.org.uk/guidance/ng222
Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: A systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. https://doi.org/10.3389/fpsyg.2018.02211
Norwegian Institute of Public Health. (2021). Psykiske lidelser hos voksne. https://www.fhi.no/nettpub/hin/psykisk-helse/psykiske-lidelser-voksne/
Papageorgiou, C., & Wells, A. (2015). Group metacognitive therapy for severe antidepressant and CBT resistant depression: A baseline-controlled trial. Cognitive Therapy and Research, 39, 14–22. https://doi.org/10.1007/s10608-014-9632-x
Rosenberg, M. (2015). Society and the adolescent self-image. Princeton University Press.
Saha, S., Lim, C. C., Cannon, D. L., Burton, L., Bremner, M., Cosgrove, P., ... & J McGrath, J. (2021). Co‐morbidity between mood and anxiety disorders: A systematic review and meta‐analysis. Depression and Anxiety, 38(3), 286–306. https://doi.org/10.1002/da.23113
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., ... & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Wells, A. (2005). Detached mindfulness in cognitive therapy: A metacognitive analysis and ten techniques. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 23, 337–355. https://doi.org/10.1007/s10942-005-0018-6
Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford press.
Wells, A. (2019). Breaking the cybernetic code: Understanding and treating the human metacognitive control system to enhance mental health. Frontiers in Psychology, 10, 2621. https://doi.org/10.3389/fpsyg.2019.02621
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42(4), 385–396. https://doi.org/10.1016/s0005-7967(03)00147-5
Wells, A., & Matthews, G. (1994). Attention and Emotion: A clinical perspective. Erlbaum.
Wells, A., & Nordahl, H. (2023). Metacognition and mental regulation. In D. J. A. Dozois & K. S. Dobson (Eds.), Treatment of Psychosocial Risk Factors in Depression (pp. 383–406). American Psychological Association.
Wells, A., Fisher, P., Myers, S., Wheatley, J., Patel, T., & Brewin, C. R. (2012). Metacognitive therapy in treatment-resistant depression: A platform trial. Behaviour Research and Therapy., 50(6), 367–373. https://doi.org/10.1016/j.brat.2012.02.004
Winter, L., Gottschalk, J., Nielsen, J., Wells, A., Schweiger, U., & Kahl, K. G. (2019). A comparison of metacognitive therapy in current versus persistent depressive disorder – A pilot outpatient study. Frontiers in Psychology, 10, 1714. https://doi.org/10.3389/fpsyg.2019.01714
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strand, E.R., Veium, L.T., Engvik, L.S.S. et al. Generic Group Metacognitive Therapy for Patients with Major Depressive Disorder and Related Problems: a Preliminary Evaluation in Specialized Mental Health Care. J Cogn Ther 16, 497–509 (2023). https://doi.org/10.1007/s41811-023-00175-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41811-023-00175-z