Abstract
Purpose
One of the aspects of lifestyle affecting weight and metabolic factors is the sleep pattern that is most neglected. Sleep pattern includes the quality and quantity of sleep throughout the day. According to studies, a high prevalence of disorders in sleep pattern is seen in people, especially obese. The goal of this review is to highlight the link between sleep pattern and anthropometric indicators and metabolic risk factors.
Method
We performed a search of journals and articles by utilizing the Institute for Scientific Information database available under the banner of the Web of Science, SCOPUS, and Google Scholar database through keywords such as: Sleep quality, Sleep duration, Obesity, Fasting blood sugar, Lipid profile. Next, we manually reviewed the contents of these articles.
Results
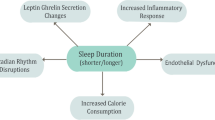
Bedtime, shift work, sleep duration, daytime sleep, and sleep quality can be considered as important factors in human health. All of this indicates the importance of circadian rhythms in the body. Given the accumulating evidence for profound effects of sleep pattern, one important area of investigation is to scrutinize its roles in weight, body composition, appetite, and metabolic variables modulation. There are also several mechanisms for expressing these effects.
Conclusion
There is ample evidence to suggest that enough sleep and early bedtime exert several beneficial effects on health. In contrast, insufficient and untimely sleep is known to cause obesity and metabolic disorders. In light of this, management of sleep has become a priority in recent years.
Similar content being viewed by others
References
Lemma S, Gelaye B, Berhane Y, et al. Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC Psychiatry. 2012;12:237.
Paine S, Gander P, Travier N. The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years). J Biol Rhythms. 2006;21(1):68–76.
Barceló A, Barbé F, Llompart E, de la Peña M, Durán-Cantolla J, Ladaria A, et al. Neuropeptide Y and leptin in patients with obstructive sleep apnea syndrome: role of obesity. Am J Respir Crit Care Med. 2005;171(2):183–7.
Chaput JP, Bouchard C, Tremblay A. Change in sleep duration and visceral fat accumulation over 6 years in adults. Obesity (Silver Spring, Md). 2014;22(5):E9-12.
Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012;157(8):549–57.
Ohkuma T, Fujii H, Iwase M, Ogata-Kaizu S, Ide H, Kikuchi Y, et al. U-shaped association of sleep duration with metabolic syndrome and insulin resistance in patients with type 2 diabetes: the Fukuoka Diabetes Registry. Metabolism: Clin Experimental. 2014;63(4):484–91.
Benedict C, Hallschmid M, Lassen A, Mahnke C, Schultes B, Schiöth HB, et al. Acute sleep deprivation reduces energy expenditure in healthy men. Am J Clin Nutr. 2011;93(6):1229–36.
Mokarrar MH, Afsharmanesh A, Afshari M, Mohammadi F. Prevalence of sleep disorder among medical students in an Eastern University in Iran. Iran-J-Health-Sci. 2017;5(1):49–54.
Sleep Disorders. https://medlineplus.gov/sleepdisorders.html. Page last updated: 2021
Laermans J, Depoortere I. Chronobesity: role of the circadian system in the obesity epidemic. Obesity Rev. 2016;17(2):108–25.
Potter GDM, Skene DJ, Arendt J, Cade JE, Grant PJ, Hardie LJ. Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr Rev. 2016;37(6):584–608.
Chittora R, Jain A, Suhalka P, Sharma C, Jaiswal N, Bhatnagar M. Sleep deprivation: neural regulation and consequences. Sleep Biol Rhythms. 2015;13(3):210–8.
Cipolla-Neto J, Amaral FG, Afeche SC, Tan DX, Reiter RJ. Melatonin, energy metabolism, and obesity: a review. J Pineal Res. 2014;56(4):371–81.
Claustrat B, Brun J, Chazot G. The basic physiology and pathophysiology of melatonin. Sleep Med Rev. 2005;9(1):11–24.
Rahe C, Czira ME, Teismann H, Berger K. Associations between poor sleep quality and different measures of obesity. Sleep Med. 2015;16(10):1225–8.
Ferranti R, Marventano S, Castellano S, Giogianni G, Nolfo F, Rametta S, et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Science. 2016;9(2):117–22.
Kahlhöfer J, Karschin J, Breusing N, Bosy-Westphal A. Relationship between actigraphy-assessed sleep quality and fat mass in college students. Obesity (Silver Spring, Md). 2016;24(2):335–41.
Jehan S, Zizi F, Pandi-Perumal SR, Wall S, Auguste E, Myers AK, et al. Obstructive sleep apnea and obesity: implications for public health. Sleep Med Disord. 2017;1(4):00019.
Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: analysis of the 2002 national health interview survey data. Arch Intern Med. 2006;166(16):1775–82.
Mullington JM, Chan JL, Van Dongen HP, Szuba MP, Samaras J, Price NJ, et al. Sleep loss reduces diurnal rhythm amplitude of leptin in healthy men. J Neuroendocrinol. 2003;15(9):851–4.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50.
Banks S, Dinges D. Behavioral and physiological consequences of sleep restriction. JCSM. 2007;3(5):519–28.
Flier JS, Maratos-Flier E. The stomach speaks–ghrelin and weight regulation. N Engl J Med. 2002;346(21):1662–3.
Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62.
Sinha M, Ohannesian J, Heiman M, Kriauciunas A, Stephens T, Magosin S, et al. Nocturnal rise of leptin in lean, obese, and non-insulin-dependent diabetes mellitus subjects. J Clin Invest. 1996;97:1344–7.
Schoeller D, Cella L, Sinha M, Caro JG. Entrainment of the diurnal rhythm of plasma leptin to meal timin. J Clin Invest. 1997;100:1882–7.
Simon C, Gronfier C, Schlienger J, Brandenberger G. Circadian and ultradian variations of leptin in normal man under continuous enteral nutrition: relationship to sleep and body temperature. J Clin Endocrinol Metab. 1998;83:1893–9.
Rayner D, Trayhurn P. Regulation of leptin production: sympathetic nervous system interactions. J Mol Med. 2001;79:8–20.
Jurado-Fasoli L, Amaro-Gahete FJ, De-la OA, Dote-Montero M, Gutiérrez Á, Castillo MJ. Association between sleep quality and body composition in sedentary middle-aged adults. Medicina (Kaunas). 2018;54(5):91.
Goodin BR, Smith MT, Quinn NB, King CD, McGuire L. Poor sleep quality and exaggerated salivary cortisol reactivity to the cold pressor task predict greater acute pain severity in a non-clinical sample. Biol Psychol. 2012;91(1):36–41.
Peeters GM, van Schoor NM, van Rossum EF, Visser M, Lips P. The relationship between cortisol, muscle mass and muscle strength in older persons and the role of genetic variations in the glucocorticoid receptor. Clin Endocrinol. 2008;69(4):673–82.
Banks S, Dinges D. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3(5):519–28.
Sandri M. Signaling in muscle atrophy and hypertrophy. Physiology (Bethesda). 2008;23:160–70.
Pyykkönen A, Isomaa B, Pesonen A, Eriksson J, Groop L, Tuomi T, et al. Subjective sleep complaints are associated with insulin resistance in individuals without diabetes: the PPP-Botnia Study. Diabetes Care. 2012;35(11):2271–8.
Gordon B, Kelleher A, Kimball S. Regulation of muscle protein synthesis and the effects of catabolic states. Int J Biochem Cell Biol. 2013;45(10):2147–57.
Patel S, Malhotra A, White D, Gottlieb D, Hu F. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164(10):947–54.
Weinger M, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. 2002;287(8):955–7.
Sivak M. Sleeping more as a way to lose weight. Obesity Rev. 2006;7(3):295–6.
Chaput JP, Després JP, Bouchard C, Tremblay A. Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia. 2007;50(11):2298–304.
Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–7.
Tare A, Lane JM, Cade BE, Grant SF, Chen TH, Punjabi NM, et al. Sleep duration does not mediate or modify association of common genetic variants with type 2 diabetes. Diabetologia. 2014;57(2):339–46.
Gozashti MHM, Eslami NM, Radfar MHM, Pakmanesh HM. Sleep pattern, duration and quality in relation with glycemic control in people with type 2 diabetes mellitus. Iran J Med Sci. 2016;41(6):531–8.
Koren D, Dumin M, Gozal D. Role of sleep quality in the metabolic syndrome. Diabetes Metab Syndr Obes. 2016;9:281–310.
Donga E, van Dijk M, van Dijk J, et al. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95(6):2963–8.
Ferrie J, Kivimaki M, Akbaraly T, et al. Associations between change in sleep duration and inflammation: findings on C-reactive protein and interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013;178(6):956–61.
St-Onge M, O’Keeffe M, Roberts A, RoyChoudhury A, Laferrere B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35(11):1503–10.
Mi SJ, Kelly NR, Brychta RJ, Grammer AC, Jaramillo M, Chen KY, et al. Associations of sleep patterns with metabolic syndrome indices, body composition, and energy intake in children and adolescents. Pediatr Obes. 2019;14(6):e12507.
Kim K, Shin D, Jung G, Lee D, Park S. Association between sleep duration, fat mass, lean mass and obesity in Korean adults: the fourth and fifth Korea National Health and Nutrition Examination Surveys. J Sleep Res. 2017;26(4):453–60.
Lin P, Chang K-T, Lin Y-A, Tzeng I, Chuang H-H, Chen J-Y. Association between self-reported sleep duration and serum lipid profile in a middle-aged and elderly population in Taiwan: a community-based, cross-sectional study. BMJ. 2017;7(10):e015964.
Baoying H, Hongjie C, Changsheng Q, Peijian W, Qingfei L, Yinghua L, et al. Association of napping and night-time sleep with impaired glucose regulation, insulin resistance and glycated haemoglobin in Chinese middle-aged adults with no diabetes: a cross-sectional study. BMJ Open. 2014;4(7):e004419.
Ford E, Li C, Wheaton A, Chapman D, Perry G, Croft J. Sleep duration and body mass index and waist circumference among US adults. Obesity (Silver Spring, Md). 2014;22(2):598–607.
Kaneita Y, Uchiyama M, Yoshiike N, Ohida T. Associations of usual sleep duration with serum lipid and lipoprotein levels. Sleep. 2008;31(5):645–52.
Geovanini G, Lorenzi-Filho G, de Paula L, Oliveira C, de Oliveira AR, Beijamini F, et al. Poor sleep quality and lipid profile in a rural cohort (The Baependi Heart Study). Sleep Med Disord. 2019;57:30–5.
Barikani A, Javadi M, Rafiei S. Sleep quality and blood lipid composition among patients with diabetes. Int J Endocrinol Metab. 2019;17(3):81062.
Khorasani M, Mohammadpoorasl A, Javadi M. The association between sleep quality and metabolic factors and anthropometric measurements. Biotechnol Health Sci. 2016;3(4):25–31.
Zhu B-Q, Li X-M, Wang D, Yu X-F. Sleep quality and its impact on glycaemic control in patients with type 2 diabetes mellitus. Int J Nurs Sci. 2014;1(3):260–5.
Jennings J, Muldoon M, Hall M, Buysse D, Manuck S. Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007;30(2):219–23.
Yu YH, Vasselli JR, Zhang Y, Mechanick JI, Korner J, Peterli R. Metabolic vs hedonic obesity: a conceptual distinction and its clinical implications. Obesity Rev. 2015;16(3):234–47.
Chaput J-P, St-Onge M-P. Increased food intake by insufficient sleep in humans: are we jumping the gun on the hormonal explanation? Front Endocrinol (Lausanne). 2014;5:116.
Kim RH, Kim KI, Kim JH, Park YS. Association between sleep duration and body composition measures in Korean Adults: The Korea National Health and Nutrition Examination Survey 2010. Korean J Fam Med. 2018;39(4):219–24.
Garaulet M, Esteban Tardito A, Lee Y, Smith C, Parnell L, Ordovas J. SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. Int J Obes. 2005;2012(36):1436–41.
Scott E, Carter A, Grant P. Association between polymorphisms in the Clock gene, obesity and the metabolic syndrome in man. Int J Obes. 2005;2008(32):658–62.
Wehrens SMT, Christou S, Isherwood C, Middleton B, Gibbs MA, Archer SN, et al. Meal timing regulates the human circadian system. Current Biol. 2017;27(12):1768-75.e3.
Tayfun Güldür T, Otlu G. Circadian rhythm in mammals: time to eat & time to sleep. Biol Rhythm Res. 2017;48(2):243–61.
Arble D, Bass J, Laposky A, et al. Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring, Md). 2009;17(11):2100–2.
Bray MS, Ratcliffe WF, Grenett MH, Brewer RA, Gamble KL, Young ME. Quantitative analysis of light-phase restricted feeding reveals metabolic dyssynchrony in mice. Int J Obes. 2013;37(6):843–52.
Olsen MK, Choi MH, Kulseng B, Zhao C-M, Chen D. Time-restricted feeding on weekdays restricts weight gain: a study using rat models of high-fat diet-induced obesity. Physiol Behav. 2017;173:298–304.
Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, Lee YC, Ordovás JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. Int J Obes. 2013;37(4):604–11.
Yasumoto Y, Hashimoto C, Nakao R, Yamazaki H, Hiroyama H, Nemoto T, et al. Short-term feeding at the wrong time is sufficient to desynchronize peripheral clocks and induce obesity with hyperphagia, physical inactivity and metabolic disorders in mice. Metabolism. 2016;65(5):714–27.
Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL, et al. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care. 2013;36(9):2523–9.
Lund J, Arendt J, Hampton SM, English J, Morgan LM. Postprandial hormone and metabolic responses amongst shift workers in Antarctica. J Endocrinol. 2001;171(3):557–64.
Damiola F, Le Minh N, Preitner N, Kornmann B, Fleury-Olela F, Schibler U. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000;14(23):2950–61.
Author information
Authors and Affiliations
Contributions
ZY collaborated in searching and writing the manuscript. SR designed the study, wrote and revised the manuscript. Both authors, approved the version to be published. They agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical Approval
Ethical approval is not required for this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yari, Z., Rabiei, S. Association Between Sleep Pattern, Anthropometric Indicators, and Metabolic Risk Factors. Sleep Vigilance 6, 7–13 (2022). https://doi.org/10.1007/s41782-021-00177-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41782-021-00177-x