Abstract
Indian HIV/AIDS numbers during the 2000s did not reach the high proportion of estimations provided by the WHO and UNAIDS. The number of HIV infections was high around 2.4 million in the 2020s, but given the country’s population of 1.38 billion, the general positivity rate remained very low compared with several countries. There were several reasons for a successful control of the epidemic in India, for example, setting-up of the National AIDS Control Programs, strategic priorities, surveillance and data management, mathematical modeling, and coordinating with the civil society and galvanizing public response. In this review article, we will provide a recollection of India’s response and management of the HIV/AIDS epidemic, challenges, and successful model building, and future challenges that play important role in sustaining the epidemic at a lower level and plan for reducing the future transmissions.
Similar content being viewed by others
1 Introduction
The National AIDS Control Programme (NACP) of India for its fourth phase 2012–2017 had budgeted a resource envelope of Rs. 143 billion ($2.70 billion). The resource envelope of NACP has been dominated by the donor support over its previous phases. The funding gaps of NACP were sufficiently large, and within the mandate of MDGs, various donor partners provided support to create capacities for effective implementation of the programme. Even though the controversial projections of US-based National Intelligence Council state that India would have 25 million HIV (about 5% of adult population) by 2010, it did not affect developing close links with the international community.
Overall, India's response to HIV/AIDS was successful in controlling the epidemic and it was well documented.1,2,3,4,5 The challenge now lies in maintaining success due to the emergence of newer pandemics like COVID-19. Since 2010, many donors started modulating their allocations globally to push the transition away from reliance on external resources, especially countries where the national economy could potentially support a greater share of HIV funding.6
Department for International Development (DFID), The United States Agency for International Development (USAID), Gates Foundation, and Global Fund all joined in this approach based on disease burden and country’s ability to increase allocations. Even though the projections of US National Intelligence Council issuing a controversial projection and Gates Foundation support them that India would have 25 million HIV (about 5% of adult population) by 20101, it did not discourage developing close links with the international community.1 As contrary to this, the estimated number of people living with HIV/AIDS in 2011 was 2.08 million.
One of the imperatives for moving towards sustainable development goals is ensuring the local ownership of the programmes and finding the relevance and appropriateness of financial envelope supporting those programmes. Over the years for several economic and political reasons, there has been growing feeling and pressure of transiting to having more share of domestic budgetary support. Ensuring that we achieve greater sustainability of our response and make sure we have predictable sources of funding, NACP during its fourth phase (2012–2017) transited from external financing in favour of domestic budgetary support. The planning and development of strategic plans for the transition from external funding to domestic support, however, was not straightforward.
The objective of this paper is to discuss the transition and examine the assumptions made during the process of developing the plan. The paper also compares and analyzes the difference between the plan and actual allocations after the transition plan was put in place. The learning may be useful to countries and other programmes which are planning such transition. We also discuss implications of this development in terms whether this change has created any critical gaps, especially for the key populations and whether the process has been transparent and predictable.
2 IHIV/AIDS Programme in India
The presence of HIV infection was first detected in India in 1986 when two doctors found about 10 HIV positive samples out of a group of 102 female sex workers from Chennai. At that time, the threat from the disease was not perceived to be high. With time and increasing surveys of blood donors, female sex workers, and injecting drug users, it became apparent that HIV infection was already present among different risk groups in India. Consequently, India embarked on with a chain of 62 AIDS surveillance centres to understand the geographical extent of the infection and identify the main routes of transmission.7
Inception Phase AIDS Task Force under the aegis of the Indian Council of Medical Research (ICMR) was constituted to look into the HIV infection issue. The government also established a National AIDS Committee (NAC) for overall policy-making and overseeing the programme performance. Given the urgency to halt the spread of infection, the Government initiated a 3-year medium-term plan that was followed by implementation of the National AIDS Control Programme (NACP) in 1987. With the support from the WHO, NACP focused on coordinating the national response to HIV/AIDS. During this inception phase, the programme’s key focus remained on the screening of the sexually promiscuous population and blood donors. Along with these activities, the programme also carried out educational programmes to increase the awareness. Till 1992, the bulk of funds for AIDS-related projects was used for improving blood testing and surveillance facilities. The testing facilities were set up for screening transfused blood for HIV to assure the safety of donated blood and prevent HIV infection from this source. ELISA machines and HIV test kits were supplied to blood banks throughout the country.
Donor Support The background of NACP’s financing through donor support goes back to the 1980s. WHO in 1985 supported the initiative to provide support for doing research in HIV/AIDS. Immediately after this in 1987, the government started NACP. By 1989, the WHO began working with the government to implement prevention policies. The National AIDS Control Organization (NACO) was established in June 1992 for the implementation of the programme. National AIDS Control Board was constituted for approval of NACO policies, expediting sanctions and for approval of significant financial and administrative decisions. In 1992, the World Bank joined in supporting the NACP by providing a loan of $84 million. This was followed by another loan of $191 million in 1999 and government’s contribution was $14 million. The key components’ NACP focused was improving the blood supply, increasing awareness of HIV transmission, and creating State AIDS Control Societies (SACS) to help implement programme components.
The inception phase of NACP made it apparent that India is dealing with a major challenge. The broad estimates indicated prevalence more than what was expected and the incidence was growing. It was felt critical to initiate the process of developing a strategic plan. Accordingly, the first strategic plan for the prevention and control of AIDS in India was prepared for the period 1992–97, the first phase of the NACP. This phase was extended to 1999 when, in 1997, it was realized that barely half of earmarked funds had been utilized.
NACP I was the first effort in India to develop a national public health programme in HIV/AIDS prevention and control. The aims of the programme were to prevent HIV transmission, decrease the morbidity and mortality associated with HIV infection, and minimize the socio-economic impact of HIV infection. After that, the National AIDS Programme took off in full gear. NACP I was followed by NACP II (1999–2006), NACP III (2007–2012), and NACP IV (2012–2017). Each of the phases of the NACP in India had a carved out strategy, a focus and programme goals addressing preventive and curative aspects of the HIV epidemic in efforts to contain the spread of the disease.
During its several phases, NACP received technical and financial assistance from bilateral agencies, such as USAID, DFID, and AUSAID. USAID support focused on providing assistance to NGOs for targeted interventions for AIDS prevention. During the early 1990s, DFID also played a key role in providing with prevention and treatment services, and since 1999, DFID also provided funding support to NACO and the state governments. By 2002, the bulk of funding for NACO came from the World Bank, an estimated $84.2 million. The government contributed $7.8 million, and approximately $10 million came from other bilateral donors. NACO continued to strengthen its partnership with various international partners. For phase III in 2007, NACO approached the Bank for credit of $250 million dollars, a threefold increase from its earlier phase. The objective of this phase was to create a more comprehensive strategy with better coordination between NACO, SACS, and NGOs and with significant scale-up of the operations. The Global Fund to fight AIDS, TB, and Malaria, a multilateral effort started providing assistance since 2004. The Global Fund has provided grants to help mothers with HIV, PLWHA, and ARV treatment. In addition, the Global Fund also provided a grant to address the TB-HIV co-infection problem. The Gates Foundation through a private philanthropy provided $258 million for the Avahan initiative; a prevention program focused on Indian truck drivers and the six highest prevalence states in India. The Clinton Foundation in 2006 provided funding to help NACO work with nurses in small communities.
As India's partnership with the Global Fund, World Bank, and other donors progressed, NACP leveraged on this support to strengthen the programme implementation. NACO through their targeted intervention approach increased their partnership with NGOs in reaching out to female sex workers (FSW), men having sex with men (MSM), injection drug users (IDU), truckers, and migrants to strengthen the prevention effort. SACs played a pivotal role in harnessing the strength of NGOs in different parts of the country. The progressive leadership at NACO and The Government of India (GoI) also contributed to this effort.
The goals, objectives, and strategies of NACP were informed by selected guiding principles. One of them is the unifying credo of “Three Ones” which focused on (a) one agreed action framework, (b) one national HIV/AIDS coordinating authority, and (c) one agreed national monitoring and evaluation system and guided the donor engagement work in HIV/AIDS sector.
3 Financial Resource Envelope of NACP
Globally, HIV/AIDS control initiatives have demonstrated some path-breaking innovations in areas of advocacy and civil society engagement and social mobilization. The political commitment towards drug pricing, solidarity, and affordability in limited resource settings has been significant. Such initiatives would not have been possible without adequate resource planning and allocations. The programme has been able to mobilize financial resources effectively using evidence and highlighting the emerging priorities.
The externally aided component of the resource envelop of NACP progressively increased over the first three phases. The national strategy and the financial and technical assistance from the World Bank, DFID, USAID, Global Fund, and Gates were well aligned and focused on prevention and institutional capacity building. This collaboration also facilitated the decentralization process including administrative and financial management systems and partnership with Non-Governmental Organizations (NGOs) to saturate prevention interventions among the high-risk groups. The targeted interventions implemented by NGOs focusing on prevention covered weaker and marginalized sections of high-risk groups. Ensuring clean and safe blood, creating awareness and demand generation for HIV prevention services, and promotion of condoms were the key areas that the IDA credit covered under the national programme and contributed to the decline in HIV infection. While the World Bank remained an important partner, various bilateral and multilateral agencies have also entered into agreements with GoI and provided technical support to specific components of the NACP. Effective leveraging of the financial resources available from different development partners to support the national strategy enabled the national programme to strategically allocate financial resources and maximize the impact (NACP IV Strategic Plan).
Concept of Resource Envelope The total of all the sources of funding to finance various components of the programme refers to as the resource envelope. In India, the NACP programme had following elements of resource envelope:
-
Direct Budgetary Support (DBS) The Government's financial allocations to the central plan for financing requirements of NACP. The DBS includes the tax receipts and other sources of revenue raised by the Government. The Niti Ayog aggregates all budgetary support required by various ministries and puts forward the demand to the Finance Ministry. This request is vetted and then approved by the Finance Ministry. The HIV/AIDS, budgetary support for NACP also includes funds allocated under National Rural Health Mission (NRHM) for meeting expenditures for establishment, blood safety, condom promotion, and STD.
-
External Aid Component (EAC) This component of resource envelope is pool fund that provides funds to GoI thorough a mechanism of a special account in which pool fund partners deposit funds for the project. These funds are used exclusively to cover the Pool Fund Partners’ share of the eligible expenditure on the project. The Controller of Aid, Accounts and Audit (CAAA), Department of Economic Affairs, Ministry of Finance operates the special account. Based on the amount of claim raised in respect of the expenditure incurred on the project (as per the reimbursement claim filed by NACO), CAAA issues an advice to the Reserve Bank of India for transfer of the amount from the special account of the project to the Consolidated Fund of India. Pool Partners replenish the special account at regular intervals as per the agreed percentages of expenditure. This component of resource envelope includes funds received from GFATM grants (various rounds), pooled funds comprising from the World Bank, DFID, USAID, Bilateral, and The UN Development Program (UNDP). These funds are routed through the government treasury system.
-
Extra-budgetary Support (EBS) This refers to the financial assistance from various development partners, such as World Bank, DFID, USAID, GFATM, and Gates Foundation grants to NGO. EBS funds are directly provided by donor agencies to various implementing agencies to support technical assistance components of the programme.
Table 1 provides resource envelope of NACP for all four phases of the programme since 1992 (see Figs. 1 and 2).
The DBS component over the four phases of NACP increased from 9% in Phase II to 75% in Phase IV. The reduction in EAC of resource envelope happened along with the Global Fund, DFID, and Gates Foundation reducing their contributions to the India’s AIDS programme. For example, the Global Fund reduced the budget for the period April 2010 to March 2016 from $530 million to $420 million. Similarly, the Gates Foundation had in 2011 announced its decision to wrap up its $338 million fund programme after 2012. As a result of this, the EAC component got reduced to Rs. 1699 crores from Rs. 4148 crores in NACP III, a reduction of about 60%. These developments were in sharp contrast to the earlier patterns, wherein India was dependent to the extent of 90% on international donors. Many of these events unfolding at that time created a challenge to sustain the national response to HIV epidemic and also an opportunity for the transition.
4 Plan for Finance Transition
The timing and process of transition from donor funding vary considerably.7 Improving economic conditions and lower disease burden may be considered a set of few factors contributing to the transition, but given the complexity of resource allocations process within the countries and the political economy of HIV/AIDS funding and issues in procurement, the predictability of transition remains less understood. The process of transition also needs to consider risks which may emanate as some of the components of the programme may not get required financing after the transition. Also, donor managed/implemented components or sub-components of the programme face risk of defunding because of mismatch/differences in budgets of government and donors for selected components. Based on the experience of NACP IV programme planning process, we present India experience of transition and possible explanation what led to the transition. These are discussed below.
Integration of Services The spread of HIV/AIDS poses complex development challenges. This epidemic mainly affects the population in their most productive years and thereby lowers productivity leading to persistence of poverty across many regions. Integration of some key components of HIV/AIDS into general health and other national programmes is considered a critical approach to manage and address the direct and indirect causes of the epidemic.
Towards the development of the strategic plan for NACP IV, a concept note in the initial stages discussed the integration strategy and its approach. Besides bringing in economies and getting a better handle on the epidemic, the integration of selected components of the programme with the National Rural Health Mission (NRHM) had the potential of providing an opportunity to leverage on resources. Over the years, India implemented the HIV/AIDS programme as a vertical programme. Vertical programmes have a separate administration, budget, and a structure. As opposed to this, the integrated programmes and responses are managed and implemented through the existing health care system and facilities.7 The integrated programmes leverage on collective resources and are expected to generate economies. Since they operate within the general health framework, the integration is expected to address priorities of the local communities in an efficient manner and share common resources with minimum wastage. It also creates a single system for addressing long-term problems in a sustainable way by avoiding duplication of work.
The Glion Consultation on strengthening the linkages between reproductive health and HIV/AIDS and other studies8,9,10,11 suggest a clear linkage between reproductive health and HIV prevention, treatment, and care. There is a need to comprehend the scope of family planning approaches globally to safeguard the reproductive options of women along with mitigating the risk of spread of HIV among women and children. The findings from these studies also suggest that integration of sexual and reproductive health care with HIV programmes helps increasing access to services and information and they are cost-effective. This approach helps in reducing sexually transmitted infections, prevention of mother-to-child transmission of HIV, unintended pregnancies, and maternal and new-born deaths. Clients seeking HIV services may have needs for family planning services, and they share common concerns. Providers can address and service the client needs more comprehensively after integration. Similarly, integrating counselling and testing for HIV into family planning at health facilities enhance voluntary counselling and testing uptake and improving the quality of care. A number of studies also highlighted the lessons from HIV integration with TB, maternal, new-born, and child health services in different settings.8,9 The integration strategy also helps in mitigating the consequences of the widespread stigma and discrimination experienced by people who are at risk of or living with HIV. By ensuring the integration of planning, resources, and programming issues, mainstreaming enables a multi-sectoral and multi-stakeholder response.6
At the time of developing the strategic plan, there was a convincing case for integration and concept notes highlighted this. At the same time, there were several examples of integration being tested in the field. As part of Avahan project, FHI operated an Astha project providing integrated STI and family planning services at their project clinics in few urban districts of Maharashtra. It was found that service uptake increased after services were integrated9 Similarly, RISHTA Project also demonstrated a community-level intervention program on an integration of HIV and SRH services at urban slums of Mumbai.9 Maharashtra AIDS Control Society (MSACS) in Satara district had also rolled out the prevention of parent-to-child transmission (PPTCT) programme under NRHM through the integrated testing and counselling centres (ICTCs) located at tertiary-/secondary-level government hospitals, facility-based ICTCs, and public–private partnership facilities, and shown a dramatic intake of services and counselling.
There was general acceptance towards the need for integration of selected components of NACP with the general health programmes. The NACP IV followed the strategy of integration as one of the important priorities. Among the five key priorities mentioned in the guideline of NACP IV, integration of HIV with other health programmes was adopted as an important strategy.9 However, it was recognized that it would be possible only through phased implementation to integrate components of NACP with the existing health programmes such as NRHM or with the proposed programme National Urban Health Mission (NUHM)).9 It was assured that the integration would be done without compromising on quality and coverage. Departments, such as (PPTCT), sexually transmitted infections (STI), Targeted Interventions (Tis), and integrated counselling and testing centers (ICTC), were identified for this purpose. The integration of National Opioid Substitution (OST) interventions with Ministry of Health, and harm reduction and social protection strategies with Ministry of Social Justice and Empowerment were also included for integration purpose. Similarly, the integration of STI care of general population, counselling and testing services, and care, support and treatment (CST) services with the general health care services were also included. In summary, the plan preparation discussion listed the following key benefits emanating from the integration strategy: (a) more efficient system for HIV/AIDS with other integrated services and better quality of care, (b) reduction in repetitive registration, (c) reduction in duplications of services, (d) reduction in stigma and discrimination, (e) greater access to integrated services at one centre rather than running for different treatments at different centres and hospitals, and (f) economies of scale that go with above-mentioned advantages, and therefore cost effectiveness.
Besides these, the integration strategy contributed to the resource augmentation as MRHM and MUHM, both having a centre and state share in implementing the programmes. NACP was centrally funded programme. Through the integration of various components of NACP, it was expected that the programme would provide an opportunity to leverage on resources from both the Centre and the State, thereby reducing the dependence on the EAC component of the budget. The transition plan was based on the integration assumption fundamentally.
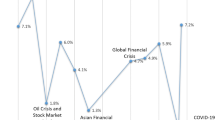
Macro-economy and Fiscal Situation Changes in the macro-economic condition and relatively improving fiscal management before 2012 led to resource availability to increase the allocation of resources to NACP IV programme. The Indian economy achieved a record annual GDP growth of 8.9% in the year 2010–11. This high growth phase was also accompanied by a consolidation of key macro-economic parameters.10 Indicator such as fiscal-deficit ratio to GDP was brought down from 6.5 to 4.3%. This had happened within the backdrop of suffering a setback with the onset of the North Atlantic financial crisis in 2008. After this crisis, growth rebounded in response to large monetary and fiscal stimuli. Moreover, a substantial widening of the current account and fiscal deficits occurred from 2008 to 2009, along with inflation climbing to an elevated level. India’s real GDP growth rebounded sharply during 2009–11. The NACP IV phase 2012–17 preparation had started in 2011, and the macro-economic conditions were also showing improving results (see Table 2).
There was also a view that global growth in the pre-crisis period was well-above potential and the post-crisis slowdown was a return to the underlying potential growth path, which itself was seen as below the pre-crisis potential growth rates. Potential growth of developing countries was 6.3% during 2005–07, whereas the actual growth during this period averaged two percentage points higher at 8.3%.10
The domestic financial sector exhibited remarkable resilience to the American financial crisis, reflecting India’s prudent approach to domestic and external financial liberalization.10,11,12 It was perhaps due to the monetary and fiscal stimulus measures that the Indian economy was among the first to recover from the crisis with growth during 2009–11 being almost the same as during the pre-crisis high growth phase 2003–08.
A number of monetary and liquidity measures led to a significant release of liquidity. For example, the effective policy rate was cut sharply from 9% in September 2008 to 3.25% by April 2009, and the cash reserve ratio was reduced from 9.0 to 5.0% over the same period.7 On the fiscal side, the Government, inter alia, cut the central indirect tax rate from 14 to 8% between December 2008 and February 2009 and also increased plan expenditure. Reflecting these actions as well as others, the Central government’s headline gross fiscal deficit (GFD) decreased from 6.5% of GDP in 2009–10 to 4.8% in 2010–11. Thus, both monetary policy and fiscal policy provided strong support—excessive with hindsight—to the domestic economy in 2010–11. While accommodative monetary and fiscal policies promoted growth during 2009–11, the phased reversal of these policies, partial so far in the case of fiscal policy, contributed to the growth rebounding in 2009–11.
Economic growth tends to be associated with not only a higher overall level of resources but also a higher share of public resources devoted to the social sector including health. There are several reasons why the government share of health spending tends to increase with income.
Rising incomes are often associated with a greater demand for, and supply of, health care. However, despite years of strong economic growth, India’s public health expenditure did not increase until there was a strong political commitment,11 seen post-2005–06. The central government expenditure on social services and rural development increased from 14.77% in 2007–08 to 17.39% in 2012–13. Expenditure on social services by the government also showed an increase in reflecting the higher priority given to this sector. As a proportion of the GDP expenditure on social services increased from 5.91% in 2007–08 to 6.79% in 2010–11 and further to 7.09% in 2012–13. Expenditure on health as a proportion of GDP increased from 1.27% in 2007–08 to 1.36% in 2012–13.12 As percent of total expenditure, the expenditure on health was 4.8%, and as percent of social services expenditure, the expenditure on health was 19.2% in 2012–13.12
The improving macro-economic parameters and relatively better fiscal conditions facilitated the development of plan with higher allocation of government budgetary support.
Health Finance The health spending, both public and private, in India is 4.02% of GDP.7 However, public spending on health spending in India is comparatively low slightly over 1% of GDP.13 India’s dependence on external assistance for health has traditionally been low relative to other developing countries. For example, in 2006, only about 0.7% of total health spending (public as well as private) was externally contributed. Low public health spending over the years has led to high private health spending.13 The out-of-pocket expenditure as a percent of private expenditure on health was as high as 92.2% in 2000, which reduced to 74.4% in 2008 but is nonetheless high.
The share of total government health spending (in GDP) showed a decline from over 1.1% in 1990 to less than 0.9% in 2005. This decline was mainly on account of the decline in government health spending at the state level. The center’s share showed a marginal increase between 1990 and 2005. The year 2005, however, marked a turning point when the share of government health expenditure in GDP began to rise due to strong political commitment to increase public spending on health from about 1% of GDP to 3% of GDP by 2012.13 In keeping with this goal, the central government increased its health spending. The total plan allocation and expenditure incurred by the Central Government for public health for the years 2007–08 to 2010–11 is shown in Table 3.
As seen from the table above, the Government increased the plan allocation for the public health spending to Rs. 26,760 crore in 2011–12 from Rs. 22,300 crore in 2010–11 and Rs. 19,534 crore in 2009–10, respectively. India’s health budget showed an increase of 75% between the period 2007–08 and 2011–12.
Government’s resolve to increase the allocation to health sector post-2005 by which the government expenditure on public health increased and this paved the way for increased allocations to NACP and helped in drafting the transition strategy.
ARV Medication Prices Under NACP II, the focus was given on low-cost care, support, and treatment including common opportunistic infections. The free distribution of ARV medications was started in 2004. Since then, this intervention has been scaled up and, as on 31st May 2006, India had set up 54 ART centres with 33,638 patients (including 1352 children) receiving free ART at these centres. However, at that time, this covered only 10% of the estimated eligible patients needing treatment. NACP III adopted a comprehensive strategy to strengthen family and community care, provide psycho-social support to patients. The programme ensured accessible, affordable, and sustainable treatment services. It was expected that expanding CST component will not only help reduce AIDS-related mortality but also positively impact on reduction in poverty, stigma, and discrimination. Furthermore, this would have helped to achieve the objective of controlling the spread of the epidemic. The strategy included identification of institutions, strengthening referral linkages for CD4 testing, capacity building of ART teams and procurement of ARV drugs. More than 300,000 patients were receiving free ART by the end of NACP III in 2011 through approximately 250 ART centres. During NACP II and NACP III, drug prices to treat using ART remained prohibitively high. The second line of ART though available was not envisaged during phase III of the programme. It is only at the end of phase III; the second line of ART was introduced. At the time of planning of the fourth phase of the programme, the prices of both first line and second-line ARV medications had significantly come down.
India has a long history of producing generic medication and it is distributing throughout Asia. Having a strong domestic infrastructure for manufacturing medicines and after joining the TRIPS in 1995, India moderated its stand that only new drugs deemed to be “new and innovative” can be patented and sold in Indian markets.12 For example, India’s denial to recognize the patented drug Novartis for Leukemia in January 2006 suggested that the government might follow the same for ART medication. Pharmaceutical companies, such as Cipla, Ranbaxy Laboratories, Matrix Laboratories, and Hetero drugs, all produce ARV medicine at cheap and affordable prices. India also has strong medical research institutions, such as the National AIDS Research Institute (NARI), and talented pool of scientists. Under these conditions, NACP IV planning considered and reflected that eventually India is in a good position to guarantee and provide ART medications at affordable prices, thereby reducing the burden on resource requirements. Therefore, declining prices of ARV medications reduced the overall financial burden and influenced the decision to support this component of the programme through domestic budgetary support.
High Prevention Focus in Previous Phases Focus on prevention components of the programme remained one of the core strategies of NACP implementation throughout its various phases. Table 4 presents a synoptic view of the allocation of planned resources to prevention components of the NACP in India. During NACP III, 67% of the budget was allocated to the prevention, and for NACP IV phase, it remained as high as 60%.
The HIV estimates at the time of NACP IV preparation suggested an overall reduction in adult HIV prevalence, HIV incidence (new infections), and AIDS-related deaths in India. The adult HIV prevalence at the national level had continued its steady decline from the estimated level of 0.41% in 2001 to 0.33% in 2006 to 0.27% in 2011. Similar declining trends were noted both among men and women at the national level. The estimated number of new annual HIV infections had declined by more than 50% over the past decade. It was estimated that India had approximately 116,000 new HIV infections in 2011, as against 270,000 in 2000. This was one of the most important evidence on the impact of the various interventions under NACP with scaled-up prevention strategies. This was possible due to rapid scale-up of interventions and with prevention focus, which resulted in bringing hard to reach populations into the ambit of the programme and a strong evidenced-based approach including mapping of high-risk populations.
The total number of People Living with HIV/AIDS (PLHIV) in India was estimated at around 2.09 Million in 2011. Children, less than 15 years of age, accounted for 7% (0.15 million) of all HIV infections, while 86% of infected individuals were in the 15–49 year age group. Of all HIV infections, 39% (0.82 million) are among women. The estimated number of PLHIV in India maintained a steady declining trend from 2.32 million in 2006 to 2.09 million in 2011 (Fig. 3). All the high prevalence states showed a clear declining trend in adult HIV prevalence.
High prevention focus during previous three phases of the programme was instrumental in creating lesser disease burden and, therefore, lesser financial requirement in subsequent phases.
Ownership Throughout the implementation of NACP, India remained committed reducing HIV mortality, prevalence, and new infections. By the end of NACP III, the India had made significant progress towards achieving this goal.14 The NACP III, which had the goal of “halt and reverse” the HIV epidemic in India, made a steady decline in overall prevalence and nearly 50% decline in new infections. The NACP demonstrated the community involvement and ownership in developing appropriate strategies and in reaching out to high-risk and vulnerable populations’ works. The programme immensely benefited by the key role played by all stakeholders.
In 2010, the Supreme Court of India directed the Government to provide second line of ART to all AIDS patients in the country. Invoking Article 21 of the Indian Constitution and stating that it was an issue of the right to health, and the judiciary had warned the ministry abdicating its constitutional responsibility.
A substantial scale-up of coverage of FSW (81%), MSM (67%), and IDU (81%) through a total of around 1821 targeted interventions (TIs) for high-risk groups and bridge populations during NACP III laid down a sound foundation. The Link Worker Scheme was established to reach out to rural HRGs and their partners and vulnerable groups. Condom promotion had achieved 85% of the target of 3.5 billion through 1.2 million retail outlets and 25 social marketing organizations. The coverage of STI services has been scaled up through 1100 designated STI/RTI clinics, 4,036 preferred private providers for HRGs and CHC/PHC under NRHM. Regular screening of HRG for STI had been initiated. About 80% of an estimated 10 million units of safe blood had been achieved through blood banks of which 80% was through voluntary blood donations. Counseling and testing services were rapidly scaled up through 10,515 ICTCs and covered 88% the total target of 22 million. The program reached 8.56 million pregnant mothers and provided treatment to 13,013 infected mother–baby pairs at the time of delivery. At the end of phase III, 516,412 PLHIV were receiving ART. CST services were being provided through 355 ART centres, 725 Link ART Centres (LACs), and 253 Community Care Centres (CCC). These facilities had been set up based on increased uptake of CST services, surpassing the original NACP III targets. The program had also started providing 2nd-line ART in a phased manner, and more than 4,208 persons were receiving 2nd-line ART. The ICTC and ART centres were not stand-alone entities, but were located on the premises of facilities belonging to the larger health system. The capacities of State AIDS Control Societies (SACS) and District AIDS Prevention and Control Units (DAPCUs) had been strengthened. At National and State levels, Technical Support Units (TSUs) were established to assist in programme monitoring and technical areas. A dedicated Northeast Regional Office had been established for focused attention to the North Eastern States. State Training Resource Centers (STRC) were set up to help the state-level implementation units and functionaries. Strategic Information Management System (SIMS) had been established, and nation-wide rollout was under way with about 15,000 reporting units across the country. The next phase of NACP, therefore, was ready to be planned on these achievements, huge ownership, and ensure that these gains are consolidated and sustained.14,15,16,17,18,19,20,21
NACP V strategic plan started building on the motivation of these stakeholders, particularly at the community level (NGOs, social activists, service providers, consumers, and policymakers) to engage actively with complex issues of HIV with complete ownership. Funding from Development Partners had played a significant role in supporting the NACP programme interventions in building this ownership. During NACP III, external resources were substantial. In the coming years, the programme strategized to be primarily funded through domestic resources. This was expected to give greater impetus to the need to move towards more effective and efficient integration approaches in the next phase of programme implementation.
5 NACP IV Implementation Challenge and Lessons
The NACP IV and financing transition plan was based on a set of assumptions discussed in the previous section. However, these were fraught with some risks and changes that may take place as implementation unfolds. In this section, we discuss how the NACP IV implementation unfolded and what is the way forward.22,23,24,25,26
Budget Allocations and Actual Expenditure NACP IV experienced a significant reduction in actual allocations as compared to what was originally budgeted. Only 67% of the plan approved amount of Rs. 11,394 crore (2012–17) was allocated to the programme. Of the approved amount, Rs. 5679 crore was spent which is nearly 91% of allotted amount in last 4 years (2012–2016). The scheduled start date for NACP IV was April 1, 2012. There was a delay in obtaining of various clearances and approval of NACP IV and it was formally launched in February 2014. As a result, many of the key initiatives and innovations planned under NACP IV could not be started for almost 18 months. This adversely affected the resource availability, and funds’ allocation was also not according to the approved plan. In a 5-year programme, the initial 2 years are critical to establishing the operational guidelines and strategic directions but, unfortunately, both regarding the allocation of funds and implementation timelines, NACO suffered a major setback; see also Fig. 4. (See Table 5)
The following important points can be highlighted from above data: (a) original budget as per the strategic plan developed was Rs. 146 billion, (b) EFC approved budget was 92% of the strategic plan budget, (c) the budget without Extra-Budgetary Support (EBS) was Rs. 113.94 billion which was 85% of EFC approved budget, (d) budget allocation for NACP IV was finally Rs. 76.72 billion which was 67% of the Government budget, and (e) the expenditure is Rs. 73.43 billion which is 96% of total allocated amount. The NACP IV could not maintain the promised budget allocations and only 67% of government budget was allocated. The year-wise situation exhibits the same pattern (see Fig. 5).
It may also be noted that macro-economic parameters dwindled after 2011–12 as the GDP growth rates declined from a high of 9–4.9% during 2013–14 (see Table 6).
During the implementation of NACP IV, the fund flow mechanism also created some impediments in the smooth functioning of the programme. The decision to route funds through the state treasury mechanism resulted in yet another setback for NACP IV. Because of inordinate delays in accessing funds, the administration response slowed down the pace of programme implementation in several states. See Table 7 for NACP targets and achievements as of 2015–16. As a consequence, many interventions got affected because of the slowdown of programme interventions and leaving of trained healthcare providers from the system. This adversely impacted the programmatic coverage and outcomes. Recently, NACO has been allowed to directly fund the State AIDS Control Societies (SACS).
Taking account of the actual allocation of resources to NACO, systemic delays, achieving the global targets and the unfinished agenda, there is need to rework on the targets which are yet to be achieved and set a revised plan as well as the timeline. A more careful fiscal management system as recommended in the mid-term appraisal is critical at the national, state, and district levels to maximize the effort and reaching the targets. Also, NACO needs to think of innovative resource mobilization. Now, it is the time to establish and create an appropriate mechanism at the national level, which can be used as a buffer fund to mitigate risks such as budget cuts, any unforeseen issues, etc. Any economy planning for the resource transition needs to consider setting-up of creating such mechanisms. NACO needs to leverage the extra-budgetary support to harmonize the efforts regarding partnerships with private sector and public sector units.27,28,29,30,31,32
NACO needs to focus all the efforts in revitalizing the interventions and improving the pace of programme implementation. In addition, there is need to ensure highest quality and effectiveness in all interventions. To facilitate this, NACO has to ensure adequate funds availability, timely transfer of resources to states, set-up new service delivery points where required and strengthen on-going interventions, and develop capacities of health care providers.7,33,34,35
Mathematical Modeling For the first in India, it was decided to build localized mathematical models for HIV/AIDS that utilize the information collected on various parameters and transmissions dynamics explained in previous sections. Such an exercise was done during NACPII when two of the co-authors of this article (K. Sudhakar and Arni S.R. S Rao) served as the World Bank consultants. Later during the NACPIII period 2006–2011, it was decided by NACLPIII team members (K Sudhakar and T Kurien) to invite Arni S.RS Rao to lead and to collaborate on the mathematical modeling efforts for the national HIV/AIDS response in India.
The success of our AIDS modeling efforts and their utilization by the Government of India and NACO during the third and fourth phases of planning were well documented.5,36,37,38,39 This is the first time, mathematical models were built for national health planning since the independence of India in 1947. However, statistical data collection and related methods were applied in several other situations in national planning in India.40,41,42,43,44,45,46,47 Modeling HIV/AIDS for Indian scenario was also conducted using modeling packages and useful conclusions were drawn; see for example.46,47,48,49,50,51,52 For a successful mathematical, the associated data and parameter estimations are essential. Several HIV/AIDS studies of India provided a rich set of data that helped to fit the models, and for fine calibrations, see for example.5,42,44,47,48,49,50,53,54,55,56,57 In addition to the transmission dynamics models, spread dynamics of HIV in India, there were successful models for cost–benefit analysis and related modeling that assisted in budget preparations; see for example.58,59,60,61,62,63,64,65,66
India became one of the few countries in the world, where localized mathematical models were successfully built, tried, and adopted, and this has paved the way for other models in India and outside to try such exercises for their own populations for several other epidemics, such as avian influenza, swine flu, etc.,
The Novelty of the Indian HIV/AIDS Model We have developed a transmission dynamics model that considers all possible modes of transmissions within India that were agreed upon by experts during the mid-2000s. Since the modeling was done with experts from the disciplines of mathematics, medicine, public health, and economics, it was made as much as comprehensive as possible to accommodate NACP II and NACP III interventions. Later, the same models were used to understand the impact of first-line and second-line ARTs in India.67 In addition to the comprehensive spread models, we also build transmission dynamics among two sub-groups, namely, the transmission among MSMs, and IDUs. Refer to5 for the details, and the parameter estimations. A brief description of our models was explained below:
The general HIV transmission dynamics model for the adults in India had four compartments \(X:\) susceptible, \({Y}_{1}:\) iSTD infected (other than HIV), \({Y}_{2}:\) HIV infected, and, \(Z:\) AIDS and described in the system of Eq. (1)
In model (1), \(r, \phi , \mu , \delta ,\) and, \(\gamma\) are positive constants, and the values of the parameter spaces \({\Theta }_{1},\) \({\Theta }_{2}\), \({\Theta }_{3}\), and, \({\Theta }_{4}\) are positive. The four functions \({f}_{1}, {f}_{2},\) \({f}_{3}\), and, \({f}_{4}\) specify transmission functions from \(X\) to \({Y}_{1}\), growth in \({Y}_{1}\), from \({Y}_{1}\) to \({Y}_{2},\) and, from \({Y}_{2}\) to \(Z\), respectively. The quantities \(r\) describe the growth rate within \(X,\) \(\phi\) is the recovery rate of STDs, \(\mu\) and \(\delta\) are death rates among STDs (other than HIV), and HIV/AIDS, respectively, and, \(\gamma\) is the rate of disease progression from HIV to AIDS. The sub-model for MSMs was developed similar to the model equations in (1) with MSMs related to four population compartments and parameters. The sub-model for the spread among IDU is described using the system of equations in (2)
The parameters and variables in (2) are having similar descriptions as in (1) but for IDU populations. All three models were considered separately for males and females. Also, the age-specific structures were considered without violating the model structures of (1) and (2). In the age-structure model, any infected with STDs or HIV could transmit the virus/infection to any other age individual.
Disease progression parameter \(\gamma\) was estimated using a likelihood equation \(L\) using the reported AIDS cases over several years, and constructing the conditional multinomial probabilities.5 There were other assumptions and models were tried for Indian disease progression parameters; see for example.68
Suppose \({R}_{1}, {R}_{2},\dots ,\) \({R}_{k}\) are reported AIDS cases over \(k\)-years, then the conditional probability is obtained as
for the \(j{\text{th}}\) sub-group of the model, and for \(i = 1,2, \ldots ,k.\) The likelihood \(L\) is given by
The likelihood function is maximized to obtain disease transmission parameter for the each sub-group.
The model predictions those were provided in 2007 for the NACPIII during 2006–2011 were found to be closer to the actual HIV numbers reported for the period.37,38,39
Integration Experience NACP envisaged integrating the response to many components of the programme with the larger health system. As per the mid-term appraisal, all the service delivery units except targeted interventions have been set up within the government health system. The evaluation suggests that the work has remained limited to the development of joint guidelines for management of STI/RTI, setting-up of integrated ICTCs. Integration was expected to generate economies of scale and leverage on common funding. However, there is no evidence of this experience generating any benefits. The experience suggests that integration challenge is fraught with several challenges and inter alia; they include: (a) coordination and management of all the programmes and services under the same umbrella and streamlining the priorities, (b) preparation of strong guidelines for service delivery which should be adhered by different departments of health, and (c) the shortage of trained health workers at different levels having multidimensional skills and expertise. However, this could have been overcome by providing better incentive and proper skill building training for integrated service approach.
Establishing and maintaining a better Health Information Management System (HMIS), supportive governance, fund availability, and a strong managerial leadership are highly required for the success of integrated service approach. Many of these fell short of actual play on ground level. Even though the condom promotion component has recently been merged with the general health, there have been suggestions, however, to keep the supply of condoms to TI with NACO/SACS. Similarly, there has been no effort on developing operational guidelines for condom promotion, HIV-TB coordination, and blood transfusion services in post-integration set-up.
For any integration strategy, a transition plan on the mechanism and modalities need to be developed in consultation with the integrating departments. This needs to be developed at a fast pace, so that smooth transition can be implemented. For the next phase of NACP, it is suggested that the programme develops an outline and new model with a programme design that should focus on modifications and strengthening of monitoring and evaluation aimed at achieving the goals of integration in full. The plan must include a new type of management structure, more functionally oriented and accountable for outcomes.
HIV Epidemic Situation: Current Status The epidemic is concentrated in key populations including people who inject drugs (PWID), transgender people (TG), MSM, FSW, and their clients. HIV prevalence is in general higher in PWID, TG, and MSM than in FSW. Prevalence in FSW has declined, but pockets of high HIV concentration remain. In India, the epidemic has stabilized with declining new HIV infections. There has been a 32% reduction in new infections from 2007 to 2015. AIDS-related deaths have also decreased by 54% in this period, largely because of the significant scale-up in ART and better survival of PLHIV. Given the reduction in budget, we can say whether the declining trend of infection can be maintained. The effect of budget cuts will get reflected with a lag and as and when new data gets generated. At the sub-national level, the epidemic trends and vulnerabilities vary considerably across the country and districts. Keeping in view the variations in socio-economic and cultural situations across geographical areas, the HIV situation and public health response must be examined and location specific solutions need to be identified. Modes of transmission of HIV vary across India because of differences in risk behavior and vulnerabilities and the size of key populations (KPs) at higher risk of HIV infection.
The epidemic in southern states continues to be driven by sexual transmission as they have the largest MSM, TG, and FSW populations in the country. Latest data from IBBS 2014–15 show that HIV prevalence in these groups was high at 10.1% and 4.9% among MSM in Andhra Pradesh and Maharashtra, respectively. It was 7.4%, 6.3%, and 5.8% among FSW in Maharashtra, Andhra Pradesh, and Karnataka, respectively. The main drivers of the epidemic in the southern states are unsafe sexual behavior, especially low levels of consistent condom use by TG, MSM, and FSW. Consistent condom use is particularly low by members of these KPs with their spouses and/or regular partners, though condom use with paid partners is also unsatisfactorily low as shown by IBBS 2014–15. Various unprotected sexual practices among KPs and their intimate partners categorized under ‘bridge population’ (i.e., migrants and truck drivers) and general population (i.e., spouses and regular partners), including relatively high levels of anal sex without consistent condom use, contribute significantly to spreading the virus beyond hotspots where risk is highly concentrated.
Instead, in north-west, central, and north-east regions, unsafe injecting behavior among PWID involving the sharing of unsterile needles and syringes is the main mode of transmission of HIV. This risk behavior is also associated with unprotected vaginal and anal sex. Transmission of HIV from men who visit FSW, especially migrants, and from male injecting drug users to their spouses or regular partners is also an important route of HIV transmission that cannot be neglected.
Other Challenges and Way Forward There have been concerns about the monitoring and evaluation of the processes to improve the quality and effectiveness of the programme. The scope and size of the monitoring and evaluation could not keep pace with the demands and requirements and concerns were raised that it needed strengthening. The structural reforms to ensure direct reporting, better inter-divisional coordination with NACO and an intensified and critical role in reviewing the programmes particularly in the poorly performing states/districts and facilitate the improvement in quality and outcomes remained high on the agenda.
Given that we had more devolution of finances to states now, it is an appropriate time to look forward to developing next phase of the programme based on centre-state sharing of finances to overcome budget constraints. For some components, which are under national health mission, there is already a mechanism for sharing the resources. This will be important to create ownership at the state level. To encourage shared responsibility, the states particularly the developed States may be requested to contribute over and above to their allotted budget of central government. Also, as a result of financial devolution, the states have got higher central allocations a part of this increase is expected to lead to higher allocations to the health sector in particular. Given the programme moves to largely domestic support, the programme should introduce the budget tracking system to ensure that the donor exit does not create any void in programme implementation in future.
It is important to understand that donor funding provided flexibility with the programme implementation particularly for components, which had significant civil society and private sector interaction. To ensure we preserve what created success, the programme plans need to focus on ensuring that they are there and the programme does not suffer. The donor funds having a significant focus on civil society and human rights issues should not get diluted. Given the HIV Act now in place, a strong monitoring system at NACO needs to be created to ensure that the transition has not diluted some of the social issues. One important condition of transitioning is creating predictability. During the NACP IV, it has either got diluted, or allocations have been reduced. This has created more uncertainty affecting the programme performance.
Building on the experience gained in strategic planning, innovative financing, and mathematical modeling over the past 3 decades, a systematic approach could be institutionalized to strengthen the public health response. Using the programmatic information and data collected from different parts of the country and observing the evolving trends in the key parameters of the program, mathematical modeling exercise can be conducted periodically at national and sub-national levels to make predictions and develop estimates which will be of invaluable help in developing appropriate strategic plans and in successful implementation of public health programmes.
References
Bachani D, Sogarwal R (2010) National Response to HIV/AIDS in India. Indian J Community Med 35(4):469–472. https://doi.org/10.4103/0970-0218.74341
Palchaudhuri R, Niggl M, Palmer CS (2016) Eliminating HIV & AIDS in India: A roadmap to zero new HIV infections, zero discrimination & zero AIDS-related deaths. Indian J Med Res 144(6):789–792. https://doi.org/10.4103/ijmr.IJMR_1902_16
Tanwar S, Rewari BB, Rao CD, Seguy N (2016) India’s HIV programme: successes and challenges. J Virus Erad 2(Suppl 4):15–19
Paranjape RS, Thakar MR, Ghate MV et al (2012) Current status of research on HIV epidemic, pathogenesis, management and prevention in India. Proc Natl Acad Sci Sect B Biol Sci 82:167–180. https://doi.org/10.1007/s40011-011-0013-x
Rao ASRS, Thomas K, Sudhakar K, Maini PK (2009) HIV/AIDS epidemic in India and predicting the impact of the national response: mathematical modeling and analysis. Math Biosci Eng 6(4):779–813
Jon C (2004) HIV/AIDS: India's many epidemics. Science
Gómez EJ The politics of receptivity and resistance: how Brazil, India, China, and Russia strategically use the International health Community in response to HIV/AIDS: a theory
http://infochangeindia.org/hiv-aids/response/the-national-aids-control-programme-1-2-3.html. Accessed 15 Oct 2021
Burrows D, Oberth G, Parsons D, McCallum L (2016) Transitions from donor funding to domestic reliance for HIV responses: Recommendations for transitioning countries. APMGlobal Health
Tanwar SSS, Rewari BB (2013) Integration of healthcare programs: A long-term policy perspective for a sustainable. HIV Program India 57(3):166–168
WHO and UNFPA (2006) Glion consultation on strengthening the linkages between reproductive health and HIV/AIDS: family planning and HIV/AIDS in women and children. http://www.unfpa.org/public/global/pid/1103
Population Action International (2012) The benefits of integrating HIV and family planning programs. policy and issue brief. Healthy Family Healthy Planet, Population Action International. Washington DC, USA. http://populationaction.org/policy-briefs/the-benefits-ofintegrating-hiv-and-family-planning-programs/. Accessed 15 Oct 2021
PATH (2009) Convergence of sexual and reproductive health (SRH) and HIV/AIDS services in India. HIV-SRH Convergence: Policy and Practice Update 3. New Delhi, India. http://www.path.org/publications/detail.php?i=1720. Accessed 15 Oct 2021
FHI (2010) Study of family planning and hiv integrated services in five countries. Family Health International, Durham
Population Action International (2012) Promoting FP/RH-HIV/AIDS integration: a summary of global health initiative strategies in Ethiopia, Kenya, Tanzania, and Zambia. Healthy Family Healthy Planet, Population Action International. Washington DC, USA. http://populationaction.org/wpcontent/uploads/2012/07/GHI_Analysis_FINAL.pdf. Accessed 15 Oct 2021
USAID (2006) Are cost savings incurred by offering family planning services at emergency plan HIV/AIDS care and treatment facilities? United States Agency for International Development, Washington, DC
Liambila W, Askew I, Ayisi R, Gathitu M, Mwangi J, Homan R, et al (2008) Feasibility, acceptability, effect and cost of integrating counselling and testing for HIV within family planning services in Kenya. FRONTIERS Final Report, Washington DC, Population Council. 2008
Patel SK (2014) Integration of HIV and other health programmes: implications and challenges. Int J Med Sci Public Health 3(6): 643–648 http://www.ejmanager.com/mnstemps/67/67-1392802472.pdf?t=1441951805
PATH (2009) Convergence of Sexual and Reproductive Health (SRH) and HIV/AIDS Services in India. HIV-SRH Convergence: Policy and Practice Update 3. New Delhi, India. 2009. http://www.path.org/publications/detail.php?i=1720. Accessed 15 Oct 2021
Schensul SL, Saggurti N, Singh R, Verma R, Nastasi BK, Mazumder PG (2009) Multilevel perspectives on community intervention: an example from an Indo-US HIV Prevention Project in Mumbai, India. Am J Community Psychol 43:277–291
Planning Commission of India. Report of the Working Group on AIDS Control for the 12th Five Year Plan (2012–2017). WG 6 AIDS Control. Planning Commission, Government of India. 2011. http://planningcommission.gov.in/aboutus/committee/wrkgrp12/health/WG_6_aids_control.pdf. Accessed 15 Oct 2021
Patel SK (2014) Integration of HIV and other health programmes: implications and challenges. Review Article. Int J Med Sci Public Health 3(6):1–7
Tanwar SS, Rewari BB (2015) Integration of healthcare programs: a long-term policy perspective for a sustainable HIV program for India. Downloaded from http://www.ijph.in on July 05, 2015. Accessed 15 Oct 2021
Kapur M, Mohan R (2014) India’s recent macroeconomic performance. an assessment and way forward. IMF Working Paper April 2014
Mohan R (2011) Growth with financial stability. Oxford University Press, New Delhi
Mohan R (2011) The growth record of the indian economy: a story of sustained savings and investment. In: Mohan R (ed) Growth with financial stability. Oxford University Press, New Delhi
Mohan R (2011) The global financial crisis: causes, impact, policy responses, and lessons. In: Mohan R (ed) Growth with financial stability. Oxford University Press, New Delhi
HIV/AIDS treatment and prevention in India: modeling the costs and consequences M Over The World Bank
Ministry of Finance (Budget Division), Government of India. Annual Report 2012–2013. http://mospi.nic.in/Mospi_New/upload/SAARC_Development_Goals_%20India_Country_Report_29aug13.pdf. Accessed 15 Oct 2021
Situation Analysis: Backdrop of the National Health Policy 2017, Ministry of Health and Family Welfare, Government of India
Berman P, Ahuja R, Tandon A, Sparkes S, Gottret P (2010) Government Health Financing in India: Challenges in Achieving Ambitious Goals. Health, Nutrition and Population (HNP) Discussion Paper of World Bank's Human Development Network. © 2010 The International Bank for Reconstruction and Development/The World Bank
http://mospi.nic.in/Mospi_New/upload/SAARC_Development_Goals_%20India_Country_Report_29aug13.pdf. Accessed 15 Oct 2021
Manmohan Singh ref
http://arthapedia.in/index.php?title=Gross_Budgetary_Support_(GBS)NACPIVProgrammeImplementationPlan. Accessed 15 Oct 2021
IBBS 2014-15, NACO; HIV prevalence has been assessed for clusters of states as per groupings listed here
Rao ASRS, Thomas K, Bhat R, Sudhakar K Towards reversal of HIV epidemic and optimal program response in India: models, data science and implications (unpublished report)
Srinivasa Rao ASR, Maini PK (2016) Influencing HIV/AIDS policy in India through mathematical modelling. In: Aston P, Mulholland A, Tant K (eds) UK success stories in industrial mathematics. Springer, Cham. https://doi.org/10.1007/978-3-319-25454-8_33
Krishnamurthy R (2018) How mathematical modelling helped control AIDS in India. Connect, IISc, 5(3): 36–39. https://connect.iisc.ac.in/2018/10/how-mathematical-modelling-helped-control-aids-in-india/. Accessed 15 Oct 2021
Mukherjee S, Saberwal G (2018) Managing India’s AIDS Crisis in the 2000s: quantitative modelling had impact. Curr Sci 114(10):2005–2006
Ghate MV, Mehendale SM, Mahajan BA et al (2000) Relationship between clinical conditions and CD4 counts in HIV-infected persons in Pune, Maharashtra, India. Natl Med J Ind 13:183–187
Dandona L, Lakshmi V, Sudha T, Kumar GA, Dandona R (2006) A population-based study of human immunodeficiency virus in south India reveals major differences from sentinel surveillance-based estimates. BMC Med 4:31
Godbole S, Mehendale SM (2005) HIV/AIDS epidemic in India: risk factors, risk behaviour & strategies for prevention & control. Ind J Med Res 121:356–368
John TJ, Babu PG, Pulimood BR, Jayakumari H (1989) Prevalence of human immunodeficiency virus infection among voluntary blood donors. Indian J Med Res 89:1–3
Hira SK, Rao ASRS, Thanekar J (1999) Evidence of AIDS-related mortality in Mumbai, India. The Lancet 354(9185):1175–1176
Prinja S, Bahuguna P, Rudra S et al (2011) Cost effectiveness of targeted HIV prevention interventions for female sex workers in India. Sex Transmit Infect 87:354–361
Hira SK, Shroff HJ, Lanjewar DN et al (2003) The natural history of human immunodeficiency virus infection among adults in Mumbai. Natl Med J Ind 16:126–131
Ranjan A, Bhatnagar T, Babu GR, Detels R (2017) Sexual Behavior, HIV prevalence and awareness among wives of migrant workers: results from cross-sectional survey in rural North India. Indian J Community Med 42(1):24–29. https://doi.org/10.4103/0970-0218.199794
Pandey A, Reddy DC, Ghys PD et al (2009) Improved estimates of India’s HIV burden in 2006. Indian J Med Res 129:50–58
Bhatnagar T, Dutta T, Stover J, Godbole S, Sahu D, Boopathi K et al (2016) Fitting HIV prevalence 1981 onwards for three Indian states using the goals model and the estimation and projection package. PLoS ONE 11(10):e0164001. https://doi.org/10.1371/journal.pone.0164001
Paranjape RS, Tripathy SP, Menon PA, Mehendale SM, Khatavkar P, Joshi DR et al (1997) Increasing trend of HIV sero prevalence among pulmonary tuberculosis patients in Pune, India. Indian J Med Res 106:207–211
Basavarajaiah DM, Narasimha Murthy B (2020) Predictive model approach to HIV TB Co-infection in vertical transmission. In: HIV Transmission. Springer, Singapore. https://doi.org/10.1007/978-981-15-0151-7_7
Kumar R, Mehendale SM, Panda S et al (2011) Impact of targeted interventions on heterosexual transmission of HIV in India. BMC Public Health 11:549. https://doi.org/10.1186/1471-2458-11-549
Prasada Rao JVR, Ganguly NK, Mehendale SM, Bollinger RC (2004) India’s response to the HIV epidemic. Lancet 364:1296–1297
Reddy DCS (2006) Projections on HIV Epidemic in India. Prepared for NACP III projection implementation plan
Balk D, Lahiri S (1997) Awareness and knowledge of AIDS among Indian women: evidence from 13 states. Health Transit Rev 7:421–465
Panda S (2003) HIV in IDUs: should we bother. Int J Drug Policy 14:83–85
Singh SK, Schensul JJ, Gupta K et al (2010) Determinants of alcohol use, risky sexual behavior and sexual health problems among men in low income communities of Mumbai, India. AIDS Behav 14:48–60. https://doi.org/10.1007/s10461-010-9732-x
Bhat R, Maheshwari SK, Saha S (2004) Treating HIV/AIDS patients in India with antiretroviral therapy: a management challenge. Indian Institute of Management, Ahmedabad
Muniyandi M, Ramachandran R, Balasubramanian R (2006) An economic commentary on the occurrence and control of HIV/AIDS in developing countries: special reference to India. Expert Opin Pharmacother 7:2447–2454
Over M, Marseille E, Sudhakar K et al (2006) Antiretroviral Therapy and HIV Prevention in India: Modeling Costs and Consequences of Policy Options. Sex Transm Dis 33(10):S145–S152. https://doi.org/10.1097/01.olq.0000238457.93426.0d
Dandona L, Kumar SP, Ramesh Y et al (2008) Changing cost of HIV interventions in the context of scaling-up in India. AIDS 22 Suppl 1(0 1):S43–S49. https://doi.org/10.1097/01.aids.0000327622.24232.aa
Mahal A, Rao B (2005) HIV/AIDS epidemic in India: an economic perspective. Indian J Med Res 121(4): 582–600. Retrieved from https://www.proquest.com/scholarly-journals/hiv-aids-epidemic-india-economic-perspective/docview/195972016/se-2. Accessed 15 Oct 2021
Panovska-Griffiths J, Vassall A, Prudden HJ, Lépine A, Boily M-C, Chandrashekar S et al (2014) Optimal allocation of resources in female sex worker targeted HIV prevention interventions: model insights from Avahan in South India. PLoS ONE 9(10):e107066. https://doi.org/10.1371/journal.pone.0107066
Kurien M, Thomas K, Ahuja RC et al (2007) Screening for HIV infection by health professionals in India. Nat Med J India 20(2):59–66 (PMID: 17802983)
Meitei MH, Latashori K, Gopal K (2005) Awareness and prevalence of reproductive tract infections in north-east districts of India. Health and Popul Perspect Issues 28(3):132–145
Reza-Paul S, Beattie T, Syed HUR et al (2008) Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS 22:S91–S100. https://doi.org/10.1097/01.aids.0000343767.08197.18
Srinivasa Rao ASR, Thomsas K, Kurapati S, Bhat R (2012) Improvement in survival of people living with HIV/AIDS and requirement for 1st- and 2nd-Line ART in India: a mathematical model. Not Am Math Soc 59:560–562
Rao Arni SR (2015) Incubation periods under various anti-retroviral therapies in homogeneous mixing and age-structured dynamical models: a theoretical approach. Rocky Mt J Math 45(3):973–1031
Acknowledgements
We thank one anonymous referee for providing editorial comments that helped in improvising the exposition of the article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhat, R., Sudhakar, K., Kurien, T. et al. Strengthening India’s Response to HIV/AIDS Epidemic Through Strategic Planning, Innovative Financing, and Mathematical Modeling: Key Achievements over the Last 3 Decades. J Indian Inst Sci 102, 791–809 (2022). https://doi.org/10.1007/s41745-022-00331-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41745-022-00331-y