Abstract
This study examines the effectiveness of health expenditure on healthcare goals in South-East Asia Region for the period from 2000 to 2014 using system generalized method of moment model. In this study, aggregate health expenditure data have been divided into two components—public and private. Both public and private health expenditure components are segregated into four categories of expenditure—government health expenditure from domestic sources, external assistance of health to the government, private out-of-pocket (i.e., household expenditure), and private not out-of-pocket (i.e., insurance). Certain health status indicators have been adopted as healthcare goals—life expectancy, infant mortality, universal health coverage index; immunization coverage, the prevalence of undernourishment, and Tb cases detection rate. The empirical result finds that aggregate health expenditure, especially public health expenditure, shows positive effects on the improvement in life expectancy and reduction of infant mortality. But the relationship between health expenditure and healthcare goals is weak (i.e., inelastic) and the elasticity values are numerically small than the non-health factors especially female education and per capita income. We have found a strong positive association between health expenditure and universal health coverage index that implies a 1% increase in public health expenditure leads to a 0.26% rise in healthcare services coverage. Further, female education has shown strong effects on the reduction of undernourishment population and increase immunization coverage. Increased public expenditure on health through domestic revenue generation and improved government effectiveness could be suggestive policy implications for achieving better health outcomes.

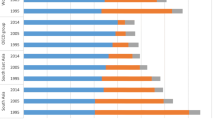
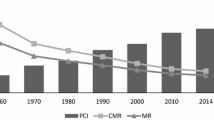
Source: Author’s estimation from the database from WHO (2017)

Similar content being viewed by others
Notes
Access to basic primary health care services to developing counties, which involved universal, community-based preventive and curative services, with substantial community involvement, was affirmed as a fundamental human rights by the Declaration of Alma-Ata in 1978 (Hall and Taylor 2003).
Table 4 (Appendix) provides the list of SEAR countries and the performance of certain healthcare goals—life expectancy, infant mortality, universal health coverage index, immunization coverage index, Tb cases detection rate and prevalence of undernourishment between the period 2000 and 2014.
For the detailed analysis about measuring universal health coverage index, please follow Tracking Universal Health Coverage (2017) Global monitoring report of World Health Organization, and World Bank.
We have excluded one of the SEAR countiries namely Democratic People’s Republic of Korea due to unavailability of sufficient data.
References
Akinkugbe O, Mohanoe M (2009) Public health expenditure as a determinant of health status in Lesotho. Soc Work Public Health 24(1–2):131–147
Anyanwu JC, Erhijakpor AE (2009) Health expenditures and health outcomes in Africa. Afr Dev Rev 21(2):400–433
Baldacci E, Clements B, Gupta S, Cui Q (2008) Social spending, human capital, and growth in developing countries. World Dev 36(8):1317–1341
Barlow R, Vissandje´e B (1999) Determinants of national life expectancy. Can J Dev Stud 20(1):9–29
Behera DK, Dash U (2018) Healthcare financing in South-East Asia: Does fiscal capacity matter? Int J Healthc Manag. https://doi.org/10.1080/20479700.2018.1548159
Behera DK, Dash U (2019) Impact of macro-fiscal determinants on health financing: empirical evidence from low-and middle-income countries. Glob Health Res Policy 4(1):21
Behera DK, Mohanty RK, Dash U (2020) Cyclicality of public health expenditure in India: role of fiscal transfer and domestic revenue mobilization. Int Rev Econ 67(1):87–110
Bhalotra S (2007) Spending to save? State health expenditure and infant mortality in India. Health Econ 16(9):911–928
Blundell R, Bond S (1998) Initial conditions and moment restrictions in dynamic panel data models. J Econom 87(1):115–143
Boerma T, Colin M, Carla AbouZahr, Somnath C, Daniel H, Gretchen S (2015) Health in 2015 from MDGs millennium development goals to SDGs sustainable development goals. World Health Organization, Switzerland
Bryce J, El Arifeen S, Pariyo G, Lanata CF, Gwatkin D, Habicht JP, Multi-Country Evaluation of IMCI Study Group (2003) Reducing child mortality: can public health deliver? Lancet 362(9378):159–164
Ciccone DK, Vian T, Maurer L, Bradley EH (2014) Linking governance mechanisms to health outcomes: a review of the literature in low and middle-income countries. Soc Sci Med 117:86–95
Crémieux PY, Ouellette P, Pilon C (1999) Health care spending as determinants of health outcomes. Health Econ 8(7):627–639
Farag M, Nandakumar AK, Wallack S, Hodgkin D, Gaumer G, Erbil C (2013) Health expenditures, health outcomes and the role of good governance. Int J Health Care Financ Econ 13(1):33–52
Filmer D, Pritchett L (1999) The impact of public spending on health: does money matter? Soc Sci Med 49(10):1309–1323
Grossman M (1972) On the concept of health capital and the demand for health. J Polit Econ 80(2):223–255
Gupta I, Guin P (2010) Communicable diseases in the South-East Asia Region of the World Health Organization: towards a more effective response. Bull World Health Organ 88(3):199–205
Gupta S, Verhoeven M, Tiongson ER (2003) Public spending on health care and the poor. Health Econ 12(8):685–696
Hall JJ, Taylor R (2003) Health for all beyond 2000: the demise of the Alma-Ata Declaration and primary health care in developing countries. Med J Aust 178(1):17–20
Hanmer L, Lensink R, White H (2003) Infant and child mortality in developing countries: analysing the data for robust determinants. J Dev Stud 40(1):101–118
Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Bellagio Child Survival Study Group (2003) How many child deaths can we prevent this year? Lancet 362(9377):65–71
Ke X, Saksena P, Holly A (2011) The determinants of health expenditure: a country-level panel data analysis. World Health Organization, Geneva, p 26
Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N (2012) Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet 380(9845):933–943
Lewis M (2006) Governance and corruption in public health care systems. Center for Global Development, Working Paper No 78
Mathauer I, Carrin G (2011) The role of institutional design and organizational practice for health financing performance and universal coverage. Health Policy 99(3):183–192
McGuire JW (2006) Basic health care provision and under-5 mortality: a cross-national study of developing countries. World Dev 34(3):405–425
Mishra P, Newhouse D (2009) Does health aid matter? J Health Econ 28(4):855–872
Moreno-Serra R, Smith PC (2012) Does progress towards universal health coverage improve population health? Lancet 380(9845):917–923
Musgrove P (1996) Public and private roles in health: Theory and financing patterns. World Bank Discussion Paper No. 339, World Bank Health, Nutrition and Population (HNP) Division, Washington, DC
Nair N, Wares F, Sahu S (2010) Tuberculosis in the WHO Southeast Asia region. Bull World Health Organ 88(3):164–164
Nixon J, Ulmann P (2006) The relationship between health care expenditure and health outcomes. Eur J Health Econ 7(1):7–18
Novignon J, Olakojo SA, Nonvignon J (2012) The effects of public and private health care expenditure on health status in sub-Saharan Africa: new evidence from panel data analysis. Health Econ Rev 2(1):22
Obrizan M, Wehby GL (2018) Health expenditures and global inequalities in longevity. World Dev 101:28–36
Rajkumar AS, Swaroop V (2008) Public spending and outcomes: does governance matter? J Dev Econ 86(1):96–111
Ranis G, Stewart F, Ramirez A (2000) Economic growth and human development. World Dev 28(2):197–219
Razvi S, Chakraborty D (2016) Does economic freedom influence major health indicators in India? Cross-state panel estimation results. J Dev Policy Practice 1(2):203–221
Reeves A, Gourtsoyannis Y, Basu S, McCoy D, McKee M, Stuckler D (2015) Financing universal health coverage—effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries. Lancet 386(9990):274–280
Rodriguez LG, Sobrino CR (2015) Public HEs, diminishing returns, and life expectancy in Latin American and Caribbean countries: a panel data analysis. J Bras Econ Saúde 7(2):91–98
Roodman D (2009) A note on the theme of too many instruments. Oxford Bull Econ Stat 71(1):135–158
Sargan JD (1975) A suggested technique for computing approximations to Wald criteria with application to testing dynamic specifications” discussion paper A2. London School of Economics, London
Self S, Grabowski R (2003) How effective is public health expenditure in improving overall health? A cross-country analysis. Appl Econ 35(7):835–845
Shaw JW, Horrace W, Vogel RJ (2005) The determinants of life expectancy: an analysis of the OECD health data. South Econ J 71(4):768–783
Soriano B, Garrido A (2016) How important is economic growth for reducing undernourishment in developing countries? Food Policy 63:87–101
Ssozi J, Amlani S (2015) The effectiveness of health expenditure on the proximate and ultimate goals of health care in Sub-Saharan Africa. World Dev 76:165–179
Suri T, Boozer MA, Ranis G, Stewart F (2011) Paths to success: the relationship between human development and economic growth. World Dev 39(4):506–522
Tracking Universal Health Coverage (2017) Global monitoring report. World Health Organization and International Bank for Reconstruction and Development/The World Bank.
Van den Heuvel WJ, Olaroiu M (2017) How important are health care expenditures for life expectancy? A comparative, European analysis. J Am Med Dir Assoc 18(3):276–e9
Ventelou B, Abu-Zaineh M (2016) Medicine and democracy: the importance of institutional quality in the relationship between health expenditure and health outcomes in the MENA region. Health Policy 120(8):928–935
WHO (2010) Health systems financing: the path to universal coverage. World Health Report. World Health Organization, Geneva
WHO (2016)Health in the Sustainable Development Goals: Where are we now in the South-East Asia Region? What Next? World Health Organization, Regional Office for South-East Asia, New Delhi
WHO (2017) Global Health Expenditure Data Base. World Health Organization. https://apps.who.int/nha/database for the most recent updates
Wolfe BL (1986) Health status and medical expenditures: is there a link? Soc Sci Med 22(10):993–999
World Bank (2017) World development indicators. The World Bank Group, Washington
Acknowledgements
The earlier version of the manuscript had presented in the 3rd International Public Policy Association (IPPA) conference at the Lee Kuan Yew (LKY) School of Public Policy, National University of Singapore, 2017. This work had started when I was a doctoral scholar in the Department of Humanities and Social Sciences, IIT Madras, Chennai. We are thankful to the conference participants and anonymous reviewers as well as the editor of the journal for useful comments and suggestions on the paper. All error is ours.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author (s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Behera, D.K., Dash, U. Is health expenditure effective for achieving healthcare goals? Empirical evidence from South-East Asia Region. Asia-Pac J Reg Sci 4, 593–618 (2020). https://doi.org/10.1007/s41685-020-00158-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41685-020-00158-4