Abstract
Objectives
To perform a budget impact analysis (BIA) of introducing olaparib as maintenance therapy in women who have BRCA mutations (BRCAm) with platinum-sensitive recurrent ovarian cancer (PSROC) in combination with bevacizumab in Argentina.
Methods
A BIA model was used to analyse over a 5-year time horizon the change in the health system’s budget following the adoption of olaparib as maintenance therapy in BRCAm patients with PSROC. The BIA for each year was estimated by comparing the cost difference between the current scenario (treatment with bevacizumab) and the new scenario (the addition of olaparib) for a third-party payer. The BIA is estimated at the national health system level, and by healthcare sectors in Argentina (public sector, social security and private sector). International and national epidemiological data were used to determine the target patient population. Clinical efficacy, safety outcomes and duration of treatments were obtained from the pivotal clinical study report. Relevant direct medical costs were obtained from public data in Argentina and expert consultation. All the costs are reported in US dollars as of October 2022 ($1 = 152.59 Argentine pesos). A scenario analysis assessed the full coverage of the homologous recombination deficiency (HRD) test in Argentina. In addition, one-way sensitivity analysis was conducted to evaluate the model robustness.
Results
For a third-party payer with a cohort of 1,000,000 women covered, the estimated target population was 2 individuals in year 1 and 6 individuals in year 5. The incorporation of olaparib, with a wholesale price per pack of $3176.32, was associated with a weighted average of the budget impact per member per month (PMPM) of $0.062 for the national health system, being above the estimated health system budget impact threshold ($0.0153). By healthcare sector, the results of budget impact PMPM for year 5 ranged between $0.08 (public sector) and $0.114 (private sector). For all perspectives, the variables that most influenced the budget impact was the incidence of ovarian cancer, the drug acquisition cost and the treatment duration.
Conclusions
The introduction of olaparib for the treatment of BRCAm women with PSROC has a high budget impact for all three health systems in Argentina.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over a 5-year period, the budget impact associated with the incorporation of olaparib for the treatment mix of ovarian cancer steadily increased across all three healthcare sectors, i.e. public, social security and private, signifying a growing financial burden on the healthcare system. |
Managed entry agreements (MEAs) may represent potential mechanisms to further explore to address the financial challenges associated with introducing new drugs, particularly in the context of fragmented healthcare systems such as Argentina. |
There is a need for further research, particularly in assessing the cost-effectiveness of olaparib treatment in the Argentine context to complement the findings presented here. |
1 Introduction
Ovarian cancer (OC) is the eighth most frequent cancer in women in Argentina, representing 3.5% of all cancers among women and ranking sixth in mortality in the overall population. In 2020, 1393 deaths associated with OC were estimated in Argentina (approximately six deaths per 100,000 inhabitants per year), representing 4.1% of cancer deaths in women [1, 2]. Moreover, in Argentina, OC represents the fifteenth cause of loss of disability-adjusted life years (DALYs) with an estimate of 100.4 DALYs per 100,000 inhabitants [2]. Given that symptoms (gastrointestinal dysfunction and ascites, abdominal distention, abdominal or pelvic pain, fatigue and peripheral neuropathies) usually appear late or are attributed to other diseases [3], approximately 75% of OC are diagnosed in advanced stages (III and IV) [4, 5], with a 5-year survival from diagnosis of approximately 46%.
Treatment for advanced stages is complete or optimal cytoreductive surgery (whenever possible) followed by platinum-based chemotherapy (cisplatin or carboplatin) plus taxanes (paclitaxel or docetaxel). Although most OCs usually respond well to this approach, it is estimated that 80% of advanced cases will suffer a recurrence of the primary cancer, which is generally incurable [4,5,6]. In part, the severity of the recurrence is determined by the sensitivity to treatment with platinum-based chemotherapy, dividing patients into platinum-sensitive and platinum-resistant depending on whether the recurrence occurs after or before 6 months, respectively. For those patients with optimal surgery, chemotherapy treatment is usually accompanied by bevacizumab. The use of maintenance therapies is aimed at prolonging life, delaying progression and improving the patient's quality of life. Among the maintenance therapies are inhibitors of the enzyme poly (ADP-ribose) polymerase (PARP) [4]. This family is composed of olaparib, rucaparib, niraparib and veliparib. For those patients who received bevacizumab during treatment, the same technology is used as maintenance therapy, and the only drug in addition to bevacizumab tested for these patients is olaparib.
The combination of olaparib with bevacizumab as maintenance therapy has shown clinical improvements in this population (overall survival, progression-free survival and time to second relapse) [7, 8]. However, the economic evidence is mixed in the international literature and scant in Argentina. In the USA, in a cost-effectiveness analysis of olaparib in combination with bevacizumab compared with bevacizumab monotherapy for the first-line maintenance treatment of homologous recombination deficiency-positive advanced OC, the authors estimated an incremental cost-effectiveness ratio (ICER) of $56,863 per quality-adjusted life year (QALY), which is well below the willingness-to-pay threshold of $100,000 per QALY [9]. On the other hand, the UK National Institute for Health and Care Excellence (NICE) in its appraisal TA693 did not recommend olaparib plus bevacizumab maintenance treatment for routine National Health Service use since the ICER is above the cost-effectiveness threshold (£30,000 per QALY) [10]. In the Latin American region, Torres-Toala and colleagues [11] estimated the budget impact of introducing olaparib as maintenance therapy in BRCA-mutated (BRCAm) women with platinum-sensitive recurrent OC, from the perspective of the Peruvian Social Health Insurance. The authors found that the clinical benefit of replacing the ‘watch and wait’ strategy with olaparib in a group of patients without any current therapeutic option available provides predictable costs for supporting the planning and decision-making process of payers in Peru. Lastly, in Argentina, Alcaraz and colleagues estimated the budget impact for olaparib as maintenance therapy in patients with epithelial OC who have responded to first-line platinum-based chemotherapy treatment [12]. They found that the budget impact was high.
In 2020, the US Food and Drug Administration (FDA) granted approval to olaparib to include its use in combination with bevacizumab for first‐line maintenance treatment of homologous recombination deficient (HRD)-positive advanced OC [13], based on the findings from PAOLA-1 [7]. Similarly, the European Medicines Agency (EMA) approved olaparib for the HRD-positive advanced OC population [14]. The National Administration of Drugs, Food, and Technology (ANMAT) is a decentralised entity of the Ministry of Health of Argentina, tasked with primary responsibilities including the oversight and regulation of the health and quality standards of medical products, encompassing monitoring of adverse effects and activities associated with their production and distribution, as well as initiatives aimed at prevention and protection of public health. In Argentina, ANMAT approved olaparib for the maintenance treatment in patients with ovarian cancer who have positive BRCA mutation and a partial or positive response to the first treatment with chemotherapy [15]. Yet, there is no approval for the HRD-positive advanced OC population, and there is no evidence whether this combination of olaparib to bevacizumab provides additional clinical benefits with reasonable cost.
This study aimed to estimate the budget impact of the addition of olaparib to bevacizumab for the first-line maintenance treatment of patients with advanced OC. In the base-case results, we estimated the budget impact for the BRCA mutation and partial or positive response to the first treatment with chemotherapy OC population. In a scenario analysis, we included the HRD-positive advanced OC population to provide insights on the potential budget impact of olaparib combined with bevacizumab. This latter scenario further extends the estimates previously provided by Alcaraz and colleagues [12] and provides economic evidence to inform policy decision-making related to the approval or inclusion of the treatment in the national benefit package in Argentina.
2 Methods
2.1 Model Structure
A global budget impact model (BIM) was developed in Microsoft Excel 2010 by AstraZeneca following the principles of good practice in budget impact modelling [16]. The global BIM model was adapted and evaluated to the Argentinian settings to estimate two scenarios over a 5-year time horizon: one where the current first-line maintenance treatment landscape continues without the addition of olaparib (current scenario) and the other where olaparib was added to bevacizumab in the first-line maintenance treatment landscape (projected scenario). The 5-year time horizon was defined on the basis of both the relevance for the budget holder and in line with the principles of good practices for reporting BIAs [16]. All the epidemiological parameters and the market shares input of the model were estimated and validated on the basis of the local clinical oncologist expert member of the research team. The BIM estimates the budget impact in terms of absolute terms, relative terms (the ratio of the projected scenario and the current scenario) and per-member per-month (PMPM) terms under the perspective of the third-party health system payer. In this paper, when referring to PMPM, we are considering one million women covered. In other words, we refer to per-women per-month. Therefore, we adjusted the PMPM estimates by sex applying the following formula:
In Eq. (1), \(\beta_{i}\) represent the net budget impact for the healthcare sector ‘i’.
In addition, the results were presented disaggregated by healthcare sectors. In Argentina, the healthcare system is decentralised and fragmented into three sectors: public, social security and private. The social security sector is the largest and provides healthcare coverage to approximately 46% of the Argentine population. The social security sector provides coverage to public and private workers, and there is one nationwide social health insurance fund for retired workers [Programa de Asistencia Médica Integral (PAMI)], which is broadly comparable to Medicare in the USA. On the other hand, 16% of individuals are covered by the private sector. This sector provides coverage to people from social security coverage contracting private supplementary plans but also people enrolled on an individual basis through direct and voluntary payments. Lastly, approximately 38% of the population is covered by the public sector [17]. All Argentinian citizens and residents, including foreign workers or tourists, can get healthcare from public facilities.
The model followed the Professional Society for Health Economics and Outcomes Research (ISPOR) Task Force for reporting budget impact analysis in health [16]. No discount rates nor adjustment for inflation were considered. The analytical structure of the BIM is reported in Fig. 1.
2.2 Target Population
The target population for analysis was adult women with advanced [International Federation of Gynaecology and Obstetrics (FIGO) stage III and IV] high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer who are in complete or partial response to first-line platinum-based chemotherapy and whose cancer is associated with a positive tumour homologous recombination deficiency (HRD) status. However, due the limited access of the HRD test in Argentina at the time of analysis, in the base-case analysis the population was estimated on the basis of a positive BRCA gene test.
In a scenario analysis, we assessed the HDR-positive advanced OC population.
2.3 Epidemiological Parameters
The starting point was a hypothetical cohort of 1,000,000 women. Of these, the incidence of OC was estimated at 97 per 1,000,000 women [18], with 75% being advanced stages (n = 73) [3]. Of these, 67.5% [4] were considered as high-grade serious disease (n = 49). The BRCA test was estimated to be performed for the initial year in 40% of the women. For the following years, we assume an increasing testing rate. Thus, for year 2, year 3, year 4 and year 5, the testing rate is 60%, 80%, 100% and 100%, respectively. The assumption was based on the local clinical oncologist expert opinion. The assumption was relaxed in the sensitivity analysis to estimate the impact of the assumption in the outcomes of the model. It was estimated that 24.1% [19] of these patients are BCRA1 and BCRA2 receptor positive. For both cases, 68% [20] were estimated to have received first-line chemotherapy with bevacizumab and 69% [21] showed a positive response to this treatment.
2.4 Intervention and Comparators
The intervention was olaparib in combination with bevacizumab. The dose, frequency and treatment duration were based on the PAOLA-1 trial [7]. The mean duration of treatment with olaparib was equal to 18.14 months, according to the analysis of PAOLA-1 trial [7]. Comparators were chosen on the basis of the current treatment landscape for patients with advanced high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer. In Argentina, bevacizumab is the therapy currently indicated for patients with advanced high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer. The dosing, frequency and treatment duration were based on the trial publication [22].
2.5 Market Share
Patients were distributed to the different treatment regimens according to specified current and projected market shares that were estimated by the local clinical oncologist expert opinion. Annual budget impact for olaparib was determined for a current market share analysis (current scenario), in which olaparib had zero market shares versus comparator, and a projected market share analysis (projected scenario), in which olaparib and the comparator treatment had market shares. Market shares are reported according to each healthcare sector of the Argentine health system (third-party public payer, third-party social security payer and third-party private payer). The market share data are reported in Supporting Information Table S1.
2.6 Cost Parameters
The direct medical costs considered in the model were classified into the following categories: testing cost, drug acquisition costs, drug administration costs, monitoring costs and adverse events costs. All costs were estimated in Argentine pesos (ARS) as for October 2022 and were expressed in USD ($1 = 152.59 ARS) [23].
For the base-case analysis, testing costs considered the cost of the BRCA test. Based on the Institute for Clinical Effectiveness and Health Policy (IECS) Unit Cost database [24], the cost of the BRCA test was $351, $640 and $681 for the third-party public payer, third-party social security payer and third-party private payer, respectively.
Drug acquisition costs were obtained from public databases that report the retail price of drugs marketed in Argentina [25]. We used the most recent retail price at the moment to perform the analysis (October 2022), and we converted the retail prices to ex-factory prices by applying the conversion factor suggested by the Argentinian Ministry of Economy [26]. For each drug, the total drug acquisition cost was estimated from the ex-factory prices, the dosage of the therapy administered and the mean duration of treatment. For all drugs, we assumed there was no wastage. The drug acquisition costs are the same for the three healthcare sectors. For drugs administered according to weight, a mean patient weight of 72.62 kg was used. The mean age of patients with OC [7, 8] and the weight information of the women were retrieved using the National Survey for Risk Factors in Argentina [27]. The cost per-pack and monthly treatment costs per-patient for the interventions and comparators are presented in Table 1.
The cost of each intravenous drug administration is estimated for the third-party public payer, the third-party social security payer and the third-party private payer at $73, $116 and $132, respectively. This cost included the use of the oncologic room to administer the drugs. We assume that oral administration has not cost. The costs were estimated on the basis of the IECS Unit Cost database [24].
The monitoring costs and the costs of adverse events were estimated using the micro-costing approach. The identification, rate of use and measurement of health resources used for the disease management were estimated by the opinion of a local expert, and the unit costs by health sector were obtained from the Institute for Clinical Effectiveness and Health Policy (IECS) unit cost database [24]. The health resources include medical consultations (oncologist), laboratory tests (blood count) and images (chest CT scan with contrast). The cost of disease management is presented in Table 2. The unit cost per health resource and the quantities used in the estimation of disease management are available in Supporting Information Table S2.
The adverse events (AEs) included in the model were hypertension, anaemia, febrile neutropenia and diarrhoea. The included adverse events are grade 3/4 AEs with incidences of greater than 2% and are in line with those reported in the clinical trials for each treatment [7]. The AEs excluded are lymphopenia as it is not considered a treatment-relevant toxicity, and fatigue as it is an adverse event whose management does not require associated clinical practices. The cost per AE is presented in Table 2, and the prevalence rates per AEs are reported in Supporting Information Table S3.
2.7 Model Validation
The model structure and calculations were reviewed and validated by the research team composed of health economists, a decision-analytic modeller, public health researchers, epidemiologists and a clinical oncologist. All input parameters were initially reviewed and validated by the local clinical oncologist expert. Suggestions for revision and/or adaptation were addressed prior to conducting the analysis.
2.8 Sensitivity Analysis
To evaluate the effect of uncertainty associated with the parameters of the model on the budget impact results, deterministic (one-way) sensitivity analyses (DSAs) were performed. The parameters were varied according to its confidence interval or, when this information was missing, by ± 20%. For the market shares values, we varied the first-year base-case value by ± 20%. To vary the base-case value for year 2 onward, we used the same variation between year 1 and the rest of the years reported in the base-case values. When necessary for year 2 onward, we capped the market share upper value at 100%.
2.9 Scenario Analyses
To be eligible to receive olaparib, it is required to test the HRD. However, as the accessibility to the test is limited in Argentina, in our base-case analyses we included patients with BRCA test. Despite that the assumption is not far distant from the Argentinian current clinical practice, we evaluated a scenario where the HRD test is fully available for the population. We assume that 58.3% of the patients who performed the HRD test were positive [7], and we included the cost of the HDR test. All the remaining parameters remained fixed.
To obtain an estimate of the cost for the HRD test in Argentina, an indirect estimation was performed in which the ratio between BRCA test cost and HRD test cost in Uruguay was applied to the cost of the BRCA test in Argentina. The cost estimates were estimated on the basis of the database of the sponsor of the study. Thereby, HRD testing costs for the public sector, social security and the private sector correspond to $1609, $2945 and $3122, respectively.
2.10 Decision Rule—Budgetary Impact Threshold
This study used the methodology for estimating a threshold of high budgetary impact proposed by Pichón-Riviere and colleagues for countries without their own estimates [28]. According to this report, the reference value of the high budgetary impact threshold is estimated at 0.00016 health spending units (0.00008–0.00024). The estimation of the threshold of high budget impact in Argentina for 2022 was made using the reference value and the estimation of total health expenditure. This latter is estimated using data from the gross domestic product (GDP) and total population of Argentina, and the average of the last 10 available years of healthcare expenditure as a percentage of GDP [29, 30]. The threshold estimation was carried out for each health perspective, using the per capita healthcare expenditures estimated and reported in the study by Espinola and colleagues [31]. Accordingly, it was estimated that the PMPM threshold of high budget impact is $ 0.0153 for the health system. In addition, the per capita healthcare expenditure values were used to quantify conversion factors and thus estimate the threshold of high budget impact for each healthcare sector perspective. So, the PMPM threshold was estimated as $0.0110 for the public sector, $0.0146 for social security and $0.0261 for the private sector.
3 Results
3.1 Target Population
For a cohort of 1,000,000 women, the target population is estimated as 2 for year 1 and 6 for year 5, because there is an assumption around the growth in the application of the BRCA, starting in year 1 with a rate of testing of 40% and rising to 100% in year 4. Further details can be found in Supporting Information Table S4.
3.2 Budget Impact Results
Table 3 presents the budget impact detail by year, health security system and cost component. The net impact is positive for every year and increases through time. For the third-party public payer, the absolute budget impact was $147,590 in year 1 and $952,090 in year 5. For the third-party social security payer, the absolute budget impact is $229,981 in year 1 and increases up to $1,318,848 in year 5. Finally, for the third-party private payer, the absolute budget impact is $255,134 in year 1 and $1,373,834 in year 5.
For all perspectives of analyses, drug costs and testing costs were the most relevant cost drivers. The drug acquisition costs and the testing costs together concentrated, on average, 98% of the total absolute budget impact in the three sectors, respectively. In addition, the relative budget impact (the ratio of the projected scenario and the current scenario) for the third-party public payer is 83% and 214% for year 1 and year 5, respectively. For the third-party social security payer, the relative budget impact for year 1 is 128% and for year 5 is 294%. For the third-party private payer, the relative budget impact for year 1 is 141% and for year 5 is 304%.
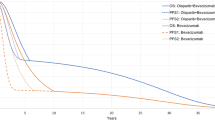
In Fig. 2, we show the projected PMPM (or, as stated previously, per-women per-month) budget impact associated with the addition of olaparib to the regular treatment with bevacizumab for the three perspectives of the analysis, and the total national health system. As an average for the 5-year horizon time, the introduction of olaparib increased the per-year cost to $0.047 PMPM, $0.069 PMPM and $0.074 PMPM for the public, social security and private sector, respectively. Except for year 1 in the third-party private payer, in all the years and for all the healthcare subsystems, the PMPM budget impact surpassed the budgetary impact threshold.
Budget impact per-member per-month (PMPM) associated with the inclusion of olaparib for each health security system. Costs are expressed in USD ($), as for October 2022. In this paper, we refer to PMPM as per-women per-month, so the estimates are adjusted by sex (see Eq. 1 in the methods section)
To obtain the budgetary impact PMPM of the total health system, we made a weighted average of the results of the three health sectors and their coverage rates (38%, 46% and 16% public sector, social security and private sector, respectively). For the health system average, the 5-year mean PMPM budget impact equals to $0.0618, which is above the health system budgetary impact threshold equal to $0.0153.
3.3 Sensitivity Analyses
Figure 3 reports the tornado diagram for all the three perspectives of analyses. For all perspectives, the variables that most influence the results of the budget impact analysis are the incidence of OC, the drug acquisition cost and the treatment duration. When we varied the incidence of OC by ± 20%, the absolute budget impact for year 5 varied from $761,672 to $1,142,509, from $1,054,974 to $1,582,460 and from $1,099,067 to $1,648,601 for the third-party public payer, the third-party social security payer and the third-party private payer, respectively. Moreover, when we varied the drug acquisition cost by ± 20%, the absolute budget impact for year 5 varied from $831,593 to $1,072,588, from $1,181,979 to $1,455,455 and from $1,234,716 to $1,512,952 for the third-party public payer, the third-party social security payer and the third-party private payer, respectively. Lastly, varying the treatment duration by ±20% yields an absolute budget impact that ranges from $840,376 to $1,063,805, from $1,186,104 to $1,451,592 and from $1,233,935 to $1,513,733 for the third-party public payer, the third-party social security payer and the third-party private payer, respectively. In Supporting Information Fig. 1, we reported the tornado diagrams for year 5 using the PMPM results.
3.4 Scenario Analysis
A hypothetical scenario was made where the HRD testing is available and marketed for patients in Argentina. In this case, the target population was 5 in year 1, and increases up to 13 in year 5. Further details can be found in Supporting Information Table S5. Table 4 presents the absolute and PMPM budget impact for the three healthcare sectors. The absolute budget impact is increasing over the years and for all the healthcare sectors. For example, for the third-party public payer, the absolute budget impact is $476,390 in year 1 and increases up to $3,049,165 in year 5. On the other hand, the PMPM budget impact exceeded the budget impact threshold for all the years and all the perspectives.
When we compared the budget impact between the base-case results and the scenario results, we found that the budget impact is approximately 2.2 times higher in the scenario results. The difference is driven by the differences in the target population size.
4 Discussion
This study sought to evaluate the budget impact of introduction of olaparib to treat patients with OC in Argentina. Our results showed a high budget impact for the three perspectives analysed since the budget impact surpassed the indicative and preliminary budget impact threshold for Argentina. Thus, our findings can provide budget impact evidence to payers who are considering incorporating olaparib onto their formulary to treat OC, as well as a tool to inform value-based price negotiations or risk-sharing agreements.
Our results here reported are similar to the one reported in a Peruvian study [11] that assessed the cost of changing the current standard of care (‘watch and wait’) with the adoption of olaparib as maintenance therapy in BRCA-mutated (BRCAm) women with platinum-sensitive recurrent ovarian cancer. However, further comparisons are missing given the different comparators defined in both studies. When we compared our results with a previous Health Technology Assessment report from the ANMAT regulatory body in Argentina [12], we found similar findings to the ones we reported. Our modelling expands the previous budget impact evidence by providing findings for each subsector of the health system in Argentina, adjusting the market share according to each subsector of the health system and performing a scenario analysis to test how the budget impact changes when the HRD testing is fully available and marketed in Argentina. The scenario analysis allowed us to test the major assumption to use the positive BRCA mutation population in the base-case analysis, and not use the HDR-positive population as is recommended [10]. The assumption was based on consultations with the research team composed of health economists, the decision-analytic modeller, public health researchers, epidemiologists and a clinical oncologist in order to adapt the model closer to the clinical reality in Argentina. The team reached consensus when the iterative process ensured that the model addressed and reflected the group’s collective opinion.
It is important to highlight, as biomarkers are expected to be more widespread in the forthcoming future in Argentina, that more patients are expected to be eligible to receive olaparib plus bevacizumab as a treatment. This will have implications in the budget impact since, as we confirmed in the scenario analyses, as the more patients are eligible for the treatment, the higher is the budget impact. Besides increasing the target population size, another factor that yields the higher budget impact is that olaparib in combination with bevacizumab demonstrated clinical advantages compared with bevacizumab alone when considering the entire span of a person's life [7]. The benefits were primarily observed in terms of extended progression-free years. Although the administration of olaparib was limited to a duration of 2 years, a considerable number of patients experienced continued benefits even after surpassing this time frame, which yields more consumption of olaparib. The resulting higher budget impact might be offset if the long-term patient benefits are below the willingness-to-pay (WTP) per one unit of clinical benefit. Until now, this cost-effectiveness evidence is mixed. In the USA, Elsea and colleagues reported that, at a WTP of $100,000 and $150,000 per quality-adjusted life year gained, olaparib plus bevacizumab had a 97.0% and 99.5% chance of being cost effective versus bevacizumab maintenance, respectively [9]. On the other hand, for the UK, NICE stated that olaparib plus bevacizumab maintenance treatment cannot be recommended for routine commissioning given its cost-effectiveness evidence [10]. In Argentina, expanding our budget impact evidence to cost-effectiveness evidence is considered necessary to analyse whether the biomarker-guided approach leads to optimal clinical outcomes with good economic value or not.
An important tool applied in several countries around the world to support decision-making in the introduction of new drugs are managed entry agreements (MEAs) (also known as risk-sharing agreements). In the Latin American region, MEAs are gaining traction, which have been applied mainly to antineoplastic drugs [32, 33]. In fact, during the latest Health Technology Assessment International Latin America Policy Forum was devoted specifically to this topic, and some examples were reported from Argentina (onasemnogene, abeparvovec and nusinersen for spinal muscular atrophy) [34, 35]. Although there are some initial experiences in Argentina, the obstacles to its implementation are high given the fragmentation of the health system. Besides these MEA experiences from the Ministry of Health and Central Government, there are increasing uses of MEAs in the private healthcare sector. At the same time, the advantages and challenges of MEAs are still being explored, and the added value for patients and the healthcare system of the interventions approved with MEAs in comparison with other available interventions remains unknown [36].
As for any budget impact model, the uncertainty around the inputs is present. For instance, a major limitation is the immaturity of the data regarding the overall survival and first and second progression time. This immaturity has been also highlighted by Elsea and colleagues [9] and by NICE [10]. In our study, to model the treatment duration, we use the mean time to treatment discontinuation equal to 18.14 months, and we tested in the sensitivity analysis by varying the base-case value ± 20%. We acknowledge that the treatment duration has a strong influence on the overall budget impact, and thus, further trials will help to address this uncertainty. Furthermore, it should also be considered that the model was populated using estimated parameters rather than real-world evidence parameters. For example, parameters such as the incidence rate ideally should be calculated using tailored real-world parameters and, thus, prevent inaccurate estimates. Previously it has been highlighted that there can be significant differences between budget impact analyses derived with estimated parameters versus real-world parameters budget impact analyses [37]. Unfortunately, we found real-world evidence for Sweden [38] but not for Argentina. Despite this, we tried our best to meet the international recommendation on budget impact analysis and adhere to the methodological guidelines, as previous authors have highlighted [39].
Another limitation was the information on the dynamics of treatment mix over time, which is hard to predict at this point. To address this uncertainty, we relied on market shares predicted by a local clinical expert. Then, considering that the market shares for oncologic drugs can be different according to each sub-sector health system [40], we differentiate the market shares by healthcare sectors in the health system. We predicted the most aggressive market penetration for the third-party private payer and the least aggressive market penetration for the third-party public payer. A ± 20% variation in the base-case values was applied in the sensitivity analysis to address the uncertainty. In any case, in the worst scenario, we may have overestimated the market penetration and, thus, the values should be seen as ceiling market shares. Moreover, in our model, we assumed a 100% compliance rate for the drugs, without accounting for compliance. However, in real-world scenarios, compliance is often lower since clinical trials are typically closely monitored and followed. In addition, discrepancies in the cost estimation may arise with different payers included. However, to address this limitation, we used standard sources for the cost estimation. Lastly, the study proposed an estimate of a high budgetary impact threshold to guide decision-makers, although it is important to note that it is only a reference value that must be taken with caution considering that the budget impact threshold was based on preliminary empirical estimates done by Pichon-Riviere and colleagues [28]. To obtain more precise estimates, further research is required to estimate the threshold on the basis of the economic productivity for each health system perspective. Furthermore, given the current macroeconomic conditions in Argentina, it is important to approach the presented results with caution and give particular attention to the fluctuation of drug prices and the clinical management of the condition.
5 Conclusion
The introduction of olaparib for the treatment of BRCAm women with PSROC has a high budget impact for all three health systems in Argentina, with an increasing trend during the 5-year time horizon. These findings are informative to support policy decisions aimed at expanding current ovarian cancer treatment.
References
World Health Organization (WHO). International Agency for Research on Cancer. International Agency for Research on Cancer. Incidence, mortality and prevalence by cancer site, 5-years prevalence (all ages). https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=continents&population=900&populations=32&key=asr&sex=0&cancer=39&type=1&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&include_nmsc=0&include_nmsc_other=1.
Institute for Health Metrics and Evaluation (IHME). Institute for Health Metrics and Evaluation (IHME). [cited 2021 Sep 13]. GBD Compare. https://vizhub.healthdata.org/gbd-compare/.
Lheureux S, Gourley C, Vergote I, Oza AM. Epithelial ovarian cancer. Lancet. 2019;393(10177):1240–53. https://doi.org/10.1016/S0140-6736(18)32552-2.
Matulonis UA, Sood AK, Fallowfield L, Howitt BE, Sehouli J, Karlan BY. Ovarian cancer. Nat Rev Dis Primers. 2016;25(2):16061. https://doi.org/10.1038/nrdp.2016.61.
Chase DM, Wenzel L. Health-related quality of life in ovarian cancer patients and its impact on clinical management. Expert Rev Pharmacoecon Outcomes Res. 2011;11(4):421–31. https://doi.org/10.1586/erp.11.41.
Thomas J Herzog MKA. UpToDate. [cited 2021 Sep 13]. First-line chemotherapy for advanced (stage III or IV) epithelial ovarian, fallopian tube, and peritoneal cancer—UpToDate. https://www.uptodate.com/contents/first-line-chemotherapy-for-advanced-stage-iii-or-iv-epithelial-ovarian-fallopian-tube-and-peritoneal-cancer?search=Medical.
Ray-Coquard I, Pautier P, Pignata S, Pérol D, González-Martín A, Berger R, et al. Olaparib plus bevacizumab as first-line maintenance in ovarian cancer. N Engl J Med. 2019;381(25):2416–28. https://doi.org/10.1056/NEJMoa1911361.
González-Martín A, Desauw C, Heitz F, Cropet C, Gargiulo P, Berger R, et al. Maintenance olaparib plus bevacizumab in patients with newly diagnosed advanced high-grade ovarian cancer: main analysis of second progression-free survival in the phase III PAOLA-1/ENGOT-ov25 trial. Eur J Cancer. 2022;174:221–31. https://doi.org/10.1016/j.ejca.2022.07.022.
Elsea D, Fan L, Mihai A, Moustaid FE, Simmons D, Monberg M, et al. Cost-effectiveness analysis of olaparib in combination with bevacizumab compared with bevacizumab monotherapy for the first-line maintenance treatment of homologous recombination deficiency-positive advanced ovarian cancer. Pharmacoecon Open. 2022;6(6):811–22. https://doi.org/10.1007/s41669-022-00338-2.
National Institute for Health Care and Excellence (NICE). Olaparib plus bevacizumab for maintenance treatment of advanced ovarian, fallopian tube or primary peritoneal cancer [Internet]. London: National Institute for Health Care and Excellence (NICE); 2021 Apr. Report No.: TA693. https://www.nice.org.uk/guidance/ta693/resources/olaparib-plus-bevacizumab-for-maintenance-treatment-of-advanced-ovarian-fallopian-tube-or-primary-peritoneal-cancer-pdf-82609438840261.
Torres Toala FG, Solorzano J, Baldi J. Budget impact for olaparib maintenance therapy for brca-mutated platinum sensitive recurrent ovarian cancer in Peru. Value Health. 2018;21:S22. https://linkinghub.elsevier.com/retrieve/pii/S1098301518304339.
Alcaraz A, Argento F, Rojas-Roque C, Cerminagni L, Perelli L, Alfie V. Olaparib in maintenance of epithelial ovarian cancer [Internet]. Buenos Aires: National Administration of Drugs, Food and Technology (ANMAT); 2022. Report No.: Health Technology Assessment report No.20. https://www.argentina.gob.ar/sites/default/files/informe-20-olaparib.pdf.
Arora S, Balasubramaniam S, Zhang H, Berman T, Narayan P, Suzman D, et al. FDA approval summary: olaparib monotherapy or in combination with bevacizumab for the maintenance treatment of patients with advanced ovarian cancer. Oncologist. 2021;26(1):e164–72. https://doi.org/10.1002/onco.13551.
European Medicines Agency (EMA). European Medicines Agency (EMA). 2022 [cited 2022 Nov]. Lynparza authorization details. https://www.ema.europa.eu/en/medicines/human/EPAR/lynparza.
National Administration of Drugs, Food and Technology (ANMAT). Disposition number DI-2021-2484-APN-DGA-ANMAT#MS [Internet]. Buenos Aires: National Administration of Drugs, Food and Technology (ANMAT); 2021. https://boletin.anmat.gob.ar/Abril_2021/Dispo_2484-21.pdf.
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014;17(1):5–14. https://doi.org/10.1016/j.jval.2013.08.2291.
Ministry of Health. [Health situation analysis: Argentina 2018]. [Internet] Buenos Aires; 2018. https://bancos.salud.gob.ar/sites/default/files/2019-12/0000001392cnt-anlisis_de_situacin_de_salud_-_repblica_argentina_-_asis_2018_compressed.pdf.
Source B. Globocan Incidence, Mortality and Prevalence by Cancer Site. [Internet] Geneva, 2021. https://gco.iarc.fr/en.
Cardoso FC, Goncalves S, Mele PG, Liria NC, Sganga L, Diaz Perez I, et al. BRCA1 and BRCA2 mutations and clinical interpretation in 398 ovarian cancer patients: comparison with breast cancer variants in a similar population. Hum Genom. 2018;12(1):39. https://doi.org/10.1186/s40246-018-0171-5.
Odetto D, Cortez JP, Saadi JM, Zamora LB, Riggi MC, Lamm M, et al. Tratamiento de tumores malignos epiteliales de ovario en estadios avanzados. Experiencia del Hospital Italiano de Buenos Aires. Medicina [Internet]. 2021 [cited 2023 May 11];81(4):565–73. http://www.scielo.org.ar/scielo.php?pid=S0025-76802021000400565&script=sci_abstract&tlng=en.
Hall M, Bertelli G, Li L, Green C, Chan S, Yeoh CC, et al. Role of front-line bevacizumab in advanced ovarian cancer: the OSCAR study. Int J Gynecol Cancer. 2020;30(2):213–20. https://doi.org/10.1136/ijgc-2019-000512.
Tewari KS, Burger RA, Enserro D, Norquist BM, Swisher EM, Brady MF, et al. Final overall survival of a randomized trial of bevacizumab for primary treatment of ovarian cancer. J Clin Oncol. 2019;37(26):2317–28. https://doi.org/10.1200/JCO.19.01009.
Central Bank of Argentina. Central Bank of Argentina. [cited 2022 Oct]. Exchange rate by date. https://www.bcra.gob.ar/MediosPago/Tipos_de_Cambio_SML.asp.
Palacios A, Balan D, Garay OU, Mena M, Souto A, Augustovski F, et al. Base de costos unitarios en salud en argentina: una fuente de información continuamente actualizada para evaluaciones economicas y analisis de impacto presupuestario en un sistema de salud fragmentado [Internet]. Vol. 19, Value in Health Regional Issues. 2019. p. S8. https://doi.org/10.1016/j.vhri.2019.08.042.
Beta A. ALFA BETA. [cited 2022 Oct]. Precios de medicamentos. https://www.alfabeta.net/home.
Garfinkel F, Méndez Y. Value Chain Reports: Health, Pharmacy and Medical Equipment. Buenos Aires, Argentina: Office for Economic Policy and Development Planning; 2016 Dec. Report No.: 21.
Ministerio de Salud y Desarrollo Social de la Nación, el Instituto Nacional de Estadística y Censos (INDEC) y las direcciones provinciales de estadística (DPE). INDEC. 2019. 4ta Encuesta Nacional de Factores de Riesgo. https://www.indec.gob.ar/indec/web/Nivel4-Tema-4-32-68.
Pichon-Riviere A, Drummond M, García Martí S, Augustovski F. Application of economic evidence in health technology assessment and decision-making for the allocation of health resources in Latin America: Seven key topics and a preliminary proposal for implementation [Internet]. Inter-American Development Bank; 2021 Jul [cited 2023 Jun 9]. https://publications.iadb.org/publications/spanish/document/Aplicacion-de-la-evidencia-economica-en-la-evaluacion-de-tecnologias-sanitarias-y-la-toma-de-decisiones-sobre-asignacion-de-recursos-sanitarios-en-America-Latina-siete-temas-clave-y-una-propuesta-preliminar-de-implementacion.pdf.
National Institute of Statistics and Censuses (INDEC). Population statistics. 2022 [cited 2022 Jun]. Census 2022. https://www.indec.gob.ar/indec/web/Nivel4-Tema-2-41-165.
World Bank. World Bank Open Data. 2023 [cited 2023 May 18]. World Bank Open Data. https://data.worldbank.org/.
Espinola N, Palacios A, Pichon-Riviere A, Augustovski, F. Estimation of health expenditure per capita by type of coverage in Argentina: proposal and initial estimates. Institute for Clinical Effectiveness and Health Policy (IECS); 2019.
Zampirolli Dias C, Godman B, Gargano LP, Azevedo PS, Garcia MM, Souza Cazarim M, et al. Integrative review of managed entry agreements: chances and limitations. Pharmacoeconomics. 2020;38(11):1165–85. https://doi.org/10.1007/s40273-020-00943-1.
Pauwels K, Huys I, Vogler S, Casteels M, Simoens S. Managed entry agreements for oncology drugs: lessons from the European experience to inform the future. Front Pharmacol. 2017;4(8):171. https://doi.org/10.3389/fphar.2017.00171.
Garcia Marti S, Alcaraz A, Perelli L, Augustovski F, Pichon-Riviere A. HTAi 2023 Latin America Health Technology Assessment Policy Forum. In: How can managed entry agreements can contribute to coverage decisions? Chile; 2023.
Ministry of Health. Secretary of Medicine and Strategic Information. 2021 [cited 2024 Feb 23]. [Disposition 2/2021, DI-2021-2-APN-SSMEIE#MS]. https://www.argentina.gob.ar/normativa/nacional/disposici%C3%B3n-2-2021-346519/texto.
Efthymiadou O, Kanavos P. Impact of Managed Entry Agreements on availability of and timely access to medicines: an ex-post evaluation of agreements implemented for oncology therapies in four countries. BMC Health Serv Res. 2022;22(1):1066. https://doi.org/10.1186/s12913-022-08437-w.
Faleiros DR, Alvares-Teodoro J, da Silva EN, Godman BB, Gonçalves Pereira R, Andrade EIG, et al. Budget impact analysis of medicines: estimated values versus real-world evidence and the implications. Expert Rev Pharmacoecon Outcomes Res. 2022;22(2):271–81. https://doi.org/10.1080/14737167.2021.1927716.
Eriksson I, Wettermark B, Bergfeldt K. Real-world use and outcomes of olaparib: a population-based cohort study. Target Oncol. 2018;13(6):725–33. https://doi.org/10.1007/s11523-018-0604-z.
Faleiros DR, Álvares J, Almeida AM, de Araújo VE, Andrade EIG, Godman BB, et al. Budget impact analysis of medicines: updated systematic review and implications. Expert Rev Pharmacoecon Outcomes Res. 2016;16(2):257–66. https://doi.org/10.1586/14737167.2016.1159958.
Palacios A, Espinola N, Rojas-Roque C. Need and inequality in the use of health care services in a fragmented and decentralized health system: evidence for Argentina. Int J Equity Health. 2020;19(1):67. https://doi.org/10.1186/s12939-020-01168-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was made possible by the support of AstraZeneca Argentina S.A. through an independent research grant. The sponsor of the study had no role in the study design, data collection, data analysis, data interpretation or writing of the manuscript.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Availability of data and material
All data involved in this study are included in the main manuscript and its supplementary information files.
Code availability
The model used during the current study is available from the corresponding author upon reasonable request.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
Concept and design, N.E., C.R.R. Formal analysis, C.S., D.S., C.R.R. Review, interpretation and discussion of the results, N.E., C.R.R., C.S., D.S., F.AR., J.C. Writing the original draft, C.S., D.S., C.R.R. Writing, reviewing and editing, N.E., C.R.R., C.S., D.S., F.AR., F.AU., J.C. Approval of the final version of the manuscript, N.E., C.R.R., C.S., D.S., F.AR., F.AU., J.C.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rojas-Roque, C., Silvestrini, C., Argento, F. et al. Budget Impact Analysis of Olaparib in Combination with Bevacizumab for Maintenance Therapy for Ovarian Cancer in Argentina. PharmacoEconomics Open 8, 585–598 (2024). https://doi.org/10.1007/s41669-024-00495-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-024-00495-6