Abstract
Introduction
This review aims to critically appraise differences in methodology and quality of model-based and empirical-data-based cost-utility studies to address key limitations, opportunities, and challenges to inform future cost-utility analyses of continuous glucose monitoring (CGM) in type 1 diabetes. This protocol is registered at PROSPERO (CRD42023391284).
Methods
The review will be conducted in accordance with the PRISMA guideline for systematic reviews. Searches will be conducted in MEDLINE, Embase, Web of Science, Cochrane Library, and Econlit from 2000 to January 2023. Model and empirical data-based studies evaluating the cost-utility of any CGM system in type 1 diabetes will be considered for inclusion. Studies that only report on cost per life year or any other clinical outcome, or reporting only costs or only clinical outcomes studies in type 2 diabetes populations, and studies on bi-hormonal closed loops and do-it-yourself hybrid closed loop devices will be excluded. Two reviewers will independently screen each study for inclusion. Data on the intervention, population, model settings (such as perspective, time horizon), model type and structure, clinical outcomes used to populate the model, validation, and uncertainty will be extracted and qualitatively synthesised. Quality will be assessed using the Philips et al. 2006 (model-based studies) or Consensus Health Economic Criteria (empirical data-based studies) checklists. Model validation will be assessed using the AdViSHE checklist.
Discussion
Now that CGM is being used more broadly in practice, critical appraisal of existing cost-utility methodology and quality is important to inform future cost-utility analyses of CGM in type 1 diabetes in various settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Continuous glucose monitoring (CGM) devices have improved the quality of glucose management, and have potentially improved quality of life, decreased disease burden and diabetes related hospital admissions in individuals with diabetes type 1 [1, 2]. Although it has been shown that the devices improve glucose control, the affordability of these devices remain a point of discussion [3, 4]. Cost-effectiveness analysis is a commonly used method in decision making to assess on a patient- or population-level if the incremental costs of a new intervention outweigh the health benefits compared with the current standard of care. When the health benefits are measured in terms of quality adjusted life years, these studies are often referred to as cost-utility analyses. Multiple cost-utility and cost-effectiveness analyses for different CGM devices have been published. A systematic review on the cost-utility of various types of CGM in individuals with diabetes type 1 was published recently [5]. Their results showed that CGM appears to be a cost-effective tool for individuals with type 1 diabetes, especially in the subgroup of individuals with suboptimal management or at risk of severe hypoglycaemia. However, they found that the incremental cost-effectiveness ratio (ICER) and quality-adjusted life year (QALY) ranges varied widely (US$18,734–US$99,941 per QALY gained and 0.76–2.99, respectively), which may be related to (1) differences in devices, with rapid developments over the past period in CGM systems, and (2) differences in modelling methodology used. This was not further analysed in the above review, which mostly focused on a straightforward overview of studies performed and their outcomes. Therefore, the current review aims to critically appraise differences in methodology and quality of model and empirical data-based studies to try and explain some of the variety in outcomes and to address key limitations, opportunities, and challenges that need to be addressed for future cost-utility analyses of CGM in individuals with type 1 diabetes. Our objectives are as follows:
-
1.
To systematically summarise published model-based and empirical data-based cost-utility studies of CGM in individuals with type 1 diabetes, by type of device.
-
2.
To systematically assess the quality and validity of the cost-utility methods applied using best practice guidelines for economic evaluations in healthcare.
-
3.
To critically appraise the differences in methodology and quality of model and empirical data-based cost-utility analysis of CGM in individuals with type 1 diabetes.
2 Methods
2.1 Protocol and Registration
The protocol was developed based on the PRISMA protocol guideline and written in accordance with the PRISMA-P checklist [6, 7]. The review will be conducted and reported in accordance with the updated PRISMA 2020 statement: an updated guideline for reporting systematic reviews [8]. The protocol was registered with PROSPERO (registration number: CRD42023391284) [9]. The review will be conducted in accordance with the PRISMA guideline for systematic review and meta-analysis. Any noteworthy amendments to this protocol will be tracked and reported in the final review.
2.2 Eligibility Criteria
2.2.1 Type of Studies
Model-based and empirical data-based (i.e. trial-based or observational data-based) cost-utility studies will be considered for inclusion. Studies that report results only in terms of cost per life year gained or cost per other clinical outcomes, or studies reporting only costs or clinical outcomes will be excluded. The first CGM device was approved by the FDA in June 1999, therefore articles published after 1st January 2000 will be included [10]. Articles will be restricted to English language.
2.2.2 Type of Population
The review will be restricted to cost-utility studies of CGM for a population of individuals diagnosed with type 1 diabetes. Type 1 diabetes is characterised by deficient insulin production and requires daily administration of insulin [11]. We will consider all studies, irrespective of individuals’ baseline characteristics (age, ethnicity), comorbidities and background therapy or study approach applied. Studies considering both type 1 and type 2 diabetes will only be considered for inclusion if results were described for both populations separately (i.e. data can be extracted for type 1 diabetes separately).
2.2.3 Type of Interventions
Any CGM intervention will be considered for inclusion in the review. CGM is defined as systems capable of monitoring blood glucose concentrations on a “continuous basis”, including both flash CGM and real-time CGM (RT–CGM) [12, 13]. In addition, we will include all kinds of interventions combined with CGM, including multiple daily injections, continuous subcutaneous insulin infusion, and the hybrid closed loop (HCL) system, which includes CGM, an algorithm and an insulin pump for continuous subcutaneous insulin infusion to function as an artificial pancreas [13, 14]. Studies on bi-hormonal closed loops (e.g. artificial pancreas) and do-it-yourself hybrid closed loop devices will be excluded as these interventions are still in development.
2.2.4 Type of Comparators
In this review, we will consider cost-utility studies comparing CGM to any comparator. This will include conventional blood glucose monitoring care, such as self-monitoring of blood glucose (SMBG) with finger prick, either with or without an insulin pump, as well as studies comparing different CGM devices with each other and comparisons between studies with/without HCL. Attention will be paid to the fast developments in the field.
2.2.5 Type of Outcomes
We will only include studies reporting health benefits in terms of QALYs gained. The outcomes of the review will focus on the methodology and quality of the cost-utility analyses rather than on the comparison of quantitative results. Various data will be extracted to obtain insights into the current methodologies used and quality and model validation will be assessed using relevant checklists. The methodology data will be focused on the model structure and the diabetes-related complications considered in the cost-utility analysis, the data used to incorporate the effectiveness of CGM, input data used for costs and quality-of-life, and how validation and uncertainty is handled. Details on the data extraction process and quality assessment are described below.
2.3 Information Sources
The following electronic databases will be searched: MEDLINE, Embase, Web of Science, Cochrane Library [for Cochrane Central Register of Controlled Trials (CENTRAL)], and Econlit. Two other bibliographic databases specifically developed for economic evaluations, the National Health Service Economic Evaluation Database (NHS EED) and the Health Economic Evaluation Database (HEED), are no longer updated (NHS EED) or accessible (HEED), and will therefore not be considered in this review [16,17,18]. Additionally, a grey literature search will be conducted using Google Scholar. We will check the references of previous systematic literature reviews on this topic and the reference lists of identified papers for additional articles.
2.4 Search Strategy
The search strategy is developed in collaboration with an information specialist (S.v.d.W.). The structure of the search strategy is based on three concepts: (1) type 1 diabetes, (2) continuous glucose monitoring and (3) cost-utility. For each concept a broad search block is developed combining subject headings and free text words including synonyms and related terms. To develop the search strategy, we started with a list of 19 key articles potentially relevant for inclusion. Relevant indexing terms and text words were derived from these key articles together with keywords suggested by (co)authors. The initial search strategy was then tested and further developed. Testing included checking whether all 19 key articles were retrieved. The search strategy excludes animal studies, comments and meeting abstracts and is limited to articles published between 2000 and 2023. The preliminary search for Medline is presented in Table 1.
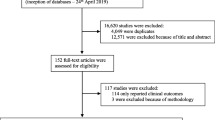
2.5 Study Selection
The database results will be imported in EndNote. Duplicates are detected and removed following a structured method [19]. Titles and abstracts will be exported from EndNote to Rayyan format for screening purposes [20]. All studies identified in the search will be assessed against the eligibility criteria. Two reviewers will independently review the titles and abstracts. To increase screening efficiency, the automation tool Rayyan Prediction Classifier for priority screening [7, 20] will be employed. The list of 19 key articles potentially relevant for inclusion used to develop the search strategy will be screened first to enable the automation tool to learn faster what articles are relevant. Next, full-text screening based on the eligibility criteria will be performed independently by the same two reviewers. Any disagreement between the two reviewers will be resolved through discussion with a third independent reviewer.
2.6 Data Extraction
Various data will be extracted on the methodology used in existing model and empirical data-based cost-utility analyses on CGM. The extraction data will be used to obtain insights on the model structure and diabetes-related complications considered, how the effectiveness of CGM was incorporated, input data used for costs and quality-of-life, and how uncertainty is handled. Additionally, model results such as incremental costs and QALYs and the ICER will be collected to put decisions made on the methodology and quality of the cost-utility analyses into perspective. Data extraction will be conducted independently by two reviewers using a standardised form. Each article will be seen by two reviewers. The data extracted will be performed in Excel. The data extraction form was developed based on a previous review on decision models in pre-diabetes [21], but adapted to also cover studies using empirical data. The form includes the following extraction data:
-
1.
Study details: title, authors, publication year
-
2.
Economic evaluation details: study design, perspective, time horizon, setting, discount rates used
-
3.
If applicable: model type/structure – model structure, model type, included health states, cycle length; if applicable: study design details for empirical data [randomised controlled trial (RCT), fully blinded or not; observational data/methods used to correct for bias]
-
4.
Data: methods for data collection, data sources used to populate the model (if applicable); follow-up time and selection criteria for empirical studies
-
5.
Outcomes: ICER, incremental costs, incremental effects (QALYs)
-
6.
Uncertainty: sensitivity analyses used, scenario analysis (subgroups)
A draft extraction table can be found in Appendix 1. Any disagreements between the reviewers will be solved through discussion with a third researcher. Any missing data will be reported as such.
2.7 Quality Assessment
Based on recommendations by Wijnen et al. (2016) [26], the methodological quality of the cost-utility analyses will be assessed using the Philips et al. 2006 checklist [24] for model-based evaluations and the Consensus Health Economic Criteria (CHEC)-extended checklist [22, 23] for trial and observational data-based economic evaluations. The Philips et al. 2006 checklist consists of 15 main items covering the structure, data and consistency. The items are subdivided in several topics and the checklist has a total of 59 sub-questions. The CHEC-extended checklist is a checklist specifically designed for the assessment of methodological quality of health economic evaluations and consists of 19 yes-or-no questions, covering 19 topics. Both checklists were not designed to be used as a points system to score the quality of a study, but ask questions regarding all elements of the study design and its reporting. They provide general guidance for the developers of models and empirical data-based studies regarding issues of importance. Therefore, these checklists are suitable for the aim of our study. The checklists will be used to identify the main methodological issues of cost-utility analyses in the field of CGM and will therefore provide valuable information for future cost-utility analyses. See Appendix 2 for the draft checklists and how each item from the checklist will be employed.
2.8 Model Validation
Model validation is an important step in the development of a cost-utility model to provide insight into the credibility of model outcomes. However, research has shown that the validation of cost-utility models is limited [27]. The Assessment of the Validation Status of Health-Economic decision models (AdViSHE) checklist was developed as a validation assessment tool in which model developers report on both validation efforts performed and on their outcomes in a systematic way [15]. The checklist consists of 13 items covering the validation of the conceptual model, the input data, the implemented software program, and model outcomes. We used this checklist to gain insight into the reporting of model validation efforts of the included cost-utility models. This checklist will only be applied to the included model-based studies. Appendix 3 presents the AdViSHE checklist and how each item from the checklist will be assessed. Of note, we will only be checking what is published regarding model validation, and will not ask study authors for any efforts performed but not reported, since the main focus of the current review is not on model validation.
2.9 Data Synthesis
The extracted data from the included studies will be qualitatively synthesised. The different aspects of the cost-utility methods and models applied and their quality will be summarised in table format. We will critically appraise the differences in methodology and quality to identify key limitations, opportunities and challenges that need to be addressed for future cost-utility analyses of CGM in individuals with type 1 diabetes. The data will be analysed and presented in different tables to focus on five main topics:
-
1.
Model structure – for model-based studies only: which model was used, which diabetes-related complications were included, type of model, time horizon, cycle length, perspective;
-
2.
Type of intervention and comparator: the intervention and comparator will be categorised into the method of CGM [self-measurement of blood glucose (finger pricks), intermittently scanned (is-) CGM (also known as Flash CGM with Freestyle libre) and/or real-time (rt-) CGM] and insulin administration [insulin injections, insulin pump without connectivity to rt-CGM, insulin pump with connectivity to rt-CGM – low glucose suspend, insulin pump with connectivity to rt-CGM – hybrid closed loop (HCL)];
-
3.
Effectiveness data: what type of effects were included and what sources were used to inform the effect size and the duration of the effect of CGM;
-
4.
Input parameters: what type of costs were included in the analysis (direct medical costs, direct non-medical costs, productivity losses, any other costs). Extra attention will be paid to CGM and insulin costs, highlighting the assumptions on strip and sensor use, and whether device replacement costs were considered. Other points of attention will be: what sources and quality of life (QoL) instruments were used for utilities and whether disutility values for hypoglycaemia or fear of hypoglycaemia were included;
-
5.
Results and uncertainty: what are the economic outcomes of the studies, and whether and how the study authors accounted for methodological, structural and parameter uncertainty and heterogeneity. Which sensitivity analyses were conducted.
The results from the quality and validation checklists will be analysed, with discussion among reviewers in case of lack of consensus, to provide one final answer to each item in the checklist: yes, no, not applicable, or not reported. The results of the checklists will be summarised in bar charts and diagrams.
3 Discussion
Now that CGM is being used more often in practice, the knowledge about how, when and for whom to use it cost-effectively is of key clinical and budgetary significance. Especially in jurisdictions with limited healthcare resources, cost-utility results are relevant to support decisions about which interventions or devices should be implemented and for whom they should be reimbursed. With CGM having a high cost, but a beneficial impact on the persons with diabetes (improved glycaemic control and quality of life) and society (possibly less diabetes related admissions and work absenteeism), it is of significant interest to investigate whether different CGM devices are cost-effective in type 1 diabetes or any sub-population. Given the chronic nature of diabetes type 1, the possible preventive effect on diabetes complications, and the constraints of clinical trials, evidence of cost-utility primarily relies on health economic models and their input parameters. This systematic review will focus on the methodology of the health economic models, the evidence used to inform them, model uncertainty and their validation, to assess their suitability for use in evaluating CGM in type 1 diabetes. The existing cost-utility studies that use empirical data without further modelling – and hence a shorter time horizon – will also be assessed and compared with the model-based studies.
A previous review has been conducted on the cost-utility outcomes and this showed a wide range of ICERs [5]. Therefore, comparison of quantitative results is not within the scope of the current review. However, incremental costs, incremental QALYs, and the ICER (or dominance) will be extracted from the included studies in this review as well, because these data are needed to put methodological choices of the cost-utility analyses reviewed into perspective. We will especially investigate how and whether assumptions regarding effectiveness, healthcare costs, perspectives, time horizons, and discount rates may affect the cost-utility outcomes.
The findings of this review will inform future health economic evaluation studies of CGM and possibly decision models that simulate the long-term costs and health outcomes of CGM in type 1 diabetes. In addition, the review will aim to identify the challenges and opportunities for reimbursement decisions about CGM in type 1 diabetes.
References
Lameijer A, Fokkert MJ, Edens MA, Gans ROB, Bilo HJG, van Dijk PR. Two-year use of flash glucose monitoring is associated with sustained improvement of glycemic control and quality of life (FLARE-NL-6). BMJ Open Diabetes Res Care. 2021;9: e002124.
Fokkert M, van Dijk P, Edens M, Barents E, Mollema J, Slingerland R, et al. Improved well-being and decreased disease burden after 1-year use of flash glucose monitoring (FLARE-NL4). BMJ Open Diabetes Res Care. 2019;7: e000809.
Holt RIG, DeVries JH, Hess-Fischl A, Hirsch IB, Kirkman MS, Klupa T, et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2021;64:2609–52.
Emamipour S, van Dijk PR, Bilo HJG, Edens MA, van der Galiën O, Postma MJ, et al. Personalizing the use of a intermittently scanned continuous glucose monitoring (isCGM) device in individuals with type 1 diabetes: a cost-effectiveness perspective in the Netherlands (FLARE-NL 9). J Diabetes Sci Technol. 2022;9:19322968221109840.
Jiao Y, Lin R, Hua X, Churilov L, Gaca MJ, James S, et al. A systematic review: Cost-effectiveness of continuous glucose monitoring compared to self-monitoring of blood glucose in type 1 diabetes. Endocrinol Diabetes Metab. 2022;5(6): e369.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:148–60.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
PROSPERO. Cited 2022 Oct 18. Available from: https://www.crd.york.ac.uk/prospero/#searchadvanced
Reddy N, Verma N, Dungan K. Monitoring technologies-continuous glucose monitoring, mobile technology, biomarkers of Glycemic control. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000. Last update: 8 Jul 2023.
Diabetes. Cited 2022 Oct 20. https://www.who.int/news-room/fact-sheets/detail/diabetes
Girardin CM, Huot C, Gonthier M, Delvin E. Continuous glucose monitoring: a review of biochemical perspectives and clinical use in type 1 diabetes. Clin Biochem. 2009;42:136–42.
Dicembrini I, Cosentino C, Monami M, Mannucci E, Pala L. Effects of real-time continuous glucose monitoring in type 1 diabetes: a meta-analysis of randomized controlled trials. Acta Diabetol. 2020;58:401–10.
Rodbard D. Continuous glucose monitoring: a review of recent studies demonstrating improved Glycemic outcomes. Diabetes Technol Ther. 2017;19:S-25.
Vemer P, Corro Ramos I, van Voorn GAK, Al MJ, Feenstra TL. AdViSHE: a validation-assessment tool of health-economic models for decision makers and model users. Pharmacoeconomics. 2016;34:349.
van Mastrigt GAPG, Hiligsmann M, Arts JJC, Broos PH, Kleijnen J, Evers SMAA, et al. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: a five-step approach (part 1/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16:689–704.
Chapter 20: Economic evidence | Cochrane Training. Cited 2023 Jun 12. Available from: https://training.cochrane.org/handbook/current/chapter-20#section-20-3
CRD Database Info | Cochrane Library. Cited 2023 Jun 12. Available from: https://www.cochranelibrary.com/about/CRD-database-info
Bramer WM, Giustini D, de Jong GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104:240–3 (A).
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016. https://doi.org/10.1186/s13643-016-0384-4.
Leal J, Morrow LM, Khurshid W, Pagano E, Feenstra T. Decision models of prediabetes populations: a systematic review. Diabetes Obes Metab. 2019;21:1558–69.
Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on Health Economic Criteria - PubMed. Int J Technol Assess Health Care. 2005;21:240–5.
Odnoletkova I. Cost-effectiveness of therapeutic education to prevent the development and progression of type 2 diabetes: systematic review. J Diabetes Metab. 2014. https://doi.org/10.4172/2155-6156.1000438.
Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics. 2006;24:355–71.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Explanation and Elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25:10–31.
Wijnen B, van Mastrigt G, Redekop W, Majoie H, de Kinderen R, Evers SMAA. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: data extraction, risk of bias, and transferability (part 3/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16:723–32.
de Boer PT, Frederix GWJ, Feenstra TL, Vemer P. Unremarked or unperformed? Systematic review on reporting of validation efforts of health economic decision models in seasonal influenza and early breast cancer. Pharmacoeconomics. 2016;34:833–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No financial support was received for this study.
Conflict of Interest
De Jong L.A., Li X., Emamipour S., van der Werf S., Postma M.J. and Feenstra T.L. declare that they have no conflict of interest. Van Dijk P.R. declares to have received financial support and study materials from Menarini Diagnostics and study materials from Abbott Diabetes Care and Dexcom Inc.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author Contributions
All authors contributed to the study conception and design of the review. The search strategy was developed by de Jong L.A., Li X., and van der Werf S. The first draft of the manuscript was written by de Jong L.A. and Li X., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication (from Patients/Participants)
Not applicable.
Code Availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
de Jong, L.A., Li, X., Emamipour, S. et al. Model and Empirical Data-Based Cost-Utility Studies of Continuous Glucose Monitoring in Individuals with Type 1 Diabetes: A Protocol of a Systematic Review on Methodology and Quality. PharmacoEconomics Open 7, 1007–1013 (2023). https://doi.org/10.1007/s41669-023-00428-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-023-00428-9