Abstract
Objective
The aim was to evaluate the cost-effectiveness of oral and subcutaneous semaglutide versus other oral glucose-lowering drugs (i.e., empagliflozin, canagliflozin, and sitagliptin) for the management of type 2 diabetes (T2D) in Denmark using clinically relevant treatment intensification rules.
Methods
A Markov-type cohort model for evaluating the cost-effectiveness of treatment pathways for T2D was used to produce cost-effectiveness estimates based on four head-to-head trials. Evidence from PIONEER 2 and 3 trials was used to evaluate the cost-effectiveness of oral semaglutide vs. empagliflozin and sitagliptin. Evidence from SUSTAIN 2 and 8 trials was used to evaluate the cost-effectiveness of subcutaneous semaglutide vs. sitagliptin and canagliflozin. Base case analyses used trial product estimands of treatment efficacy to avoid the confounding effects of rescue medication use during trials. Deterministic scenario analyses and probabilistic sensitivity analyses were conducted to assess robustness of cost-effectiveness estimates.
Results
Semaglutide-based treatment regimens were consistently associated with higher lifetime diabetes treatment costs, lower costs of complications, and higher lifetime accumulated QALYs. The PIONEER 2 analysis estimated the cost-effectiveness of oral semaglutide vs. empagliflozin was DKK 150,618/QALY (€20,189). The PIONEER 3 analysis estimated the cost-effectiveness of oral semaglutide vs. sitagliptin was DKK 95,093/QALY (€12,746). The SUSTAIN 2 analysis estimated the cost-effectiveness of subcutaneous semaglutide vs. sitagliptin was DKK 79,982/QALY (€10,721). The SUSTAIN 8 analysis estimated the cost-effectiveness of subcutaneous semaglutide vs. canagliflozin was DKK 167,664/QALY (€22,474).
Conclusions
Daily oral and weekly subcutaneous semaglutide are likely to both increase cost and health benefits, but are likely to do so under commonly considered cost-effectiveness thresholds.
Trial Registrations
Clinicaltrials.gov: NCT02863328 (PIONEER 2; registered August 11, 2016); NCT02607865 (PIONEER 3; registered November 18, 2015); NCT01930188 (SUSTAIN 2; registered August 28, 2013); NCT03136484 (SUSTAIN 8; registered May 2, 2017).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Evidence from four large multi-centre randomized controlled trials which examined the clinical efficacy of oral and subcutaneous formulations of the GLP-1RA semaglutide, in comparison with SGLT-2is empagliflozin and canagliflozin, as well as the DDP-4i sitagliptin, was used to populate a validated commercially available cohort-based T2D cost-effectiveness model. |
Considering clinically relevant treatment intensification rules and known patterns of treatment discontinuation for patients with T2D in Denmark, both oral and subcutaneous semaglutide are likely to be associated with greater lifetime costs and health benefits, at rates falling under commonly considered cost-effectiveness thresholds. |
1 Introduction
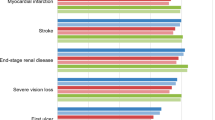
Type 2 diabetes (T2D) is a chronic and progressive disease associated with numerous risk factors, including obesity, and prognosis is related to lifestyle factors [1]. Numerous micro- [2] and macrovascular [3] complications of T2D are associated with costly increases in morbidity and mortality [4]. Important somatic complications include stroke, myocardial infarction, renal disease, visual loss, and amputations [2, 3]. Psychological complications are common, with important implications for quality of life and adherence to treatment [5]. Lost productivity associated with diabetes and diabetic complications also impose a substantial economic burden on society. In Denmark, approximately 262,750 people had a T2D diagnosis as of 2021 [6], equal to 4.5% of the Danish population [7]. This increases every year in Denmark, as elsewhere [8]. A Danish real-world evidence study found total societal costs attributable to diabetes in Denmark estimated around €4.27 billion in 2011, approximately €1.77 billion of which was due to productivity losses, and healthcare costs strongly driven by diabetes-related complications [9].
Prevention and delay of complications, maintaining quality of life as high as possible for as long as possible, is the goal of T2D treatment [10]. Early detection and proper disease management, including regular follow-up and a patient-centred approach to strengthen patient self-care [10], can substantially affect disease progression and development of complications [11]. In particular, glycaemic control is considered a key target of treatments for T2D patients, with high glycated haemoglobin (HbA1c) levels associated with disease progression [12].
For treatment of T2D amongst patients without pre-existing cardiovascular or renal complications who are not adequately controlled on metformin (with or without sulfonylurea), in order to reduce HbA1c levels, international [13] and Danish [14] guidelines recommend intensifying with anti-diabetic treatment options such as dipeptidyl peptidase-4 inhibitors (DPP4is), sodium–glucose cotransporter 2 inhibitors (SGLT-2is) and glucagon-like peptide 1 receptor agonists (GLP-1RAs). While SGLT-2is (e.g., empagliflozin, canagliflozin) and DDP-4is (e.g., sitagliptin) are exclusively available as orally administered medications, both oral and subcutaneous formulations of the GPL-1RA semaglutide are available.
Amongst T2D patients inadequately controlled by metformin (with or without sulfonylurea), the efficacy and safety of oral semaglutide have been demonstrated across the PIONEER clinical trials program [15, 16], and the efficacy and safety of subcutaneous semaglutide have been demonstrated across the SUSTAIN clinical trials program [17, 18].
As GPL-1RAs are priced higher than both SGLT-2is and DDP-4is, whether semaglutide represents a cost-effective treatment relative to comparator DDP-4i and SGLT-2is is of interest. Using the treatment effects observed in the PIONEER 2 and 3, as well as SUSTAIN 2 and 8 trials, this study is designed to evaluate the long-term cost-effectiveness of oral and subcutaneous semaglutide in Denmark versus empagliflozin, canagliflozin, or sitagliptin with clinically relevant treatment intensification rules.
2 Methods
2.1 Modelling Approach
The Swedish Institute for Health Economics’ Diabetes Cohort Model (IHE-DCM) was used to conduct the analyses reported in this study. The IHE-DCM is an easy to use, transparent, and externally validated [19, 20] Excel-based model which has an established international history of being used for reimbursement decisions associated with HTA submissions in T2D [21,22,23,24,25].
The IHE-DCM is a Markov-type cost-effectiveness model, which includes many important health states associated with T2D (e.g., 22 micro- and macrovascular comorbidities). The model is designed for users to define baseline characteristics of patient cohorts, select from a range of macrovascular and mortality risk equations which drive the extrapolation through health states, define treatment pathways, unit costs and quality of life inputs. Transitions between health states are based on 1-year cycle lengths, up to a maximum of a 40-year time horizon.
Cohort characteristics drive the risk equations which determine the transitions between and distributions across health states over time. Baseline cohort definitions include demographic characteristics (e.g., age, sex, race/ethnicity, diabetes duration, smoking rate), relevant biomarkers (e.g., HbA1c, systolic and diastolic blood pressure, total cholesterol, low- and high-density lipoprotein, triglycerides, BMI, heart rate, white blood cell count, and estimated glomerular filtration rate), and history of micro- and macrovascular complications (e.g., eye disease, diseases of the lower extremities, kidney disease, heart disease, heart attack, heart failure, and stroke).
Microvascular risk equations are not user selectable, and are based on models by Eastman et al. (1997) [26] and Bagust et al. (2001) [27]. Four sets of user-selectable macrovascular risk equations are available, based on the UKPDS 68 [28], UKPDS 82 [29], the Swedish National Diabetes Registry (NDR) [30] and the Australian Fremantle Diabetes Study (FDS) [31]. Furthermore, two sets of mortality risk equations are available in the model based on the UKPDS 68 [28] and UKPDS 82 [29] studies.
The model compares user-specified treatment algorithms (pathways) that are defined by treatment efficacy indicators (i.e., changes in HbA1c and other biomarkers), as well as conditions under which treatments are switched/intensified (i.e., an HbA1c threshold, or specified time on treatment).
The model can be run both deterministically and probabilistically. Outputs from the model include total (discounted) direct healthcare costs associated with treatments for diabetes and treating complications, as well as indirect costs (i.e., societal perspective costs associated with labour market productivity losses), cumulative histories of complications, total (discounted) life-years and quality-adjusted life years, and incremental cost-effectiveness ratios.
To support transparency and reporting quality, the Diabetes Modelling Input Checklist resulting from the Eighth Mount Hood Diabetes Challenge [32] and the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) [33] checklist were completed.
2.2 Base Cases
Diabetes trial programs have used a number of definitions of ‘estimands’ to estimate treatment efficacy (i.e., change in % HbA1c). ‘Treatment policy’ estimands reflect the intention-to-treat principle. ‘Treatment policy’ estimands report treatment efficacy estimates which do not account for discontinuation of study medications and/or use of additional antidiabetic medications over the course of the trial. In contrast, ‘trial product’ estimands reflect a modified intention-to-treat approach. ‘Trial product’ estimands report treatment efficacy estimates which under the assumption that patients receive the study drug for the duration of the trial without receiving any additional antidiabetic medications. Because the effects of rescue medications (e.g., basal and bolus insulin) are already included in ‘treatment policy’ estimands, disease modelling which equally applies treatment effects of subsequent treatments (e.g., basal and bolus insulin) following formally modelled treatment switching/intensification biases results against better-performing treatments with lower use of rescue medications. Consequently, use of ‘treatment policy’ estimands was not considered appropriate for the base case analyses, and ‘trial product’ estimands were used in the base case. The PIONEER trial program [15, 16], evaluating oral semaglutide, reported both a ‘treatment policy’ estimand and a ‘trial product’ estimand. The SUSTAIN trials [17, 18] did not report ‘treatment policy’ estimands.
Patients enrolled in the PIONEER 2 [15], PIONEER 3 [16], SUSTAIN 2 [17], and SUSTAIN 8 [18] trials had type 2 diabetes that was uncontrolled by metformin (with or without sulfonylurea) and were treated with an additional oral/subcutaneous GLP-1RA (semaglutide), oral SGLT-2i (empagliflozin/canagliflozin), or oral DDP-4i (sitagliptin). Respectively, doses of each considered trial medication were: daily oral semaglutide 14 mg; weekly subcutaneous semaglutide 1.0 mg; daily oral empagliflozin 25 mg; daily oral canagliflozin 300 mg; daily oral sitagliptin 100 mg. Across the four clinical trials, mean baseline ages ranged between 55.1 and 57.8 with between 6.6 and 8.6 years of historical diabetes diagnoses, and baseline HbA1c levels ranging between 8.1 and 8.3. Baseline patient characteristics, including biomarkers and rates of micro- and macrovascular complications are extensively detailed in Supplementary Appendix Tables 1, 2, 3, and 4.
Considering the Danish payer perspective to estimate incremental cost-effectiveness ratios (DKK/QALY), base case deterministic analyses were conducted using a 40-year time horizon, where Swedish NDR macrovascular and UKPDS 82 mortality risk equations were selected. Discounting of both costs and health benefits were set at 3.5% per annum based on Danish Finance Ministry requirements [34].
2.3 Treatment Algorithm
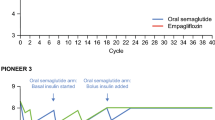
Starting from the defined baseline cohort characteristics, the treatment algorithms modelled an initial year of HbA1c reduction equal to the reported efficacy of one of the medications as reported in the key trials (i.e., semaglutide/empagliflozin/canagliflozin/sitagliptin), as well as changes in other key biomarkers including systolic blood pressure, total cholesterol, low-density lipoprotein, high-density lipoprotein, triglycerides, body mass index (BMI), estimated glomerular filtration rate, and non-severe and severe hypoglycaemic events for patients. Efficacy estimands were those reported at 52 weeks [15, 16, 18], or at 56 weeks in the case of the SUSTAIN 2 [17] trial (Appendix Table 5). Based on HbA1c drift amongst T2D patients treated with metformin reported from the ADOPT study [35], which has been accepted in clinical submissions [36, 37], an upwards 0.14% HbA1c annual drift was applied. Based on the low rates observed in the trials [15,16,17,18], it was assumed that there were no hypoglycaemia events associated with the use of trial medications. In line with Danish clinical guidelines, patients were modelled as remaining on the trial medications until the HbA1c level target of 7.5% was exceeded by 0.5% [38] (i.e., when the HbA1c level crossed 8.0%), at which point a switch to a basal insulin (+ metformin) regimen was estimated and treatment effects of trial medications were reversed across biomarkers. Transition to basal insulin was modelled as resulting in an initial period − 1.44% HbA1c change [39]. The same annual HbA1c drift was assumed to continue, and once the HbA1c threshold of 9% (i.e., target 8.5% exceeded by 0.5%) was crossed, a switch to a basal + bolus insulin (+ metformin) regimen was modelled with an initial period − 0.71% HbA1c change [39]. When the continuing annual HbA1c drift reached 9%, it was assumed that use of bolus insulin would be able to maintain HbA1c level and modelled to remain at that level throughout the model’s remaining time horizon. Rates of severe and non-severe hypoglycaemia events associated with basal and basal + bolus insulin treatment regimens were based on those reported by Willis et al. [39].
2.4 Costs and Utilities
Costs of trial medicines, insulin, and metformin were taken from pharmacy purchase prices (apotekets indkøbspris, AIP) listed in the Danish medicines database (www.medicinpriser.dk) on October 17, 2022. Annual costs of all treatment steps were calculated to include an appropriate level of blood-sugar testing (Appendix Tables 6, 7, 8). Costs of blood-sugar testing and insulin administration consumables were based on publicly published prices (www.webapoteket.dk), which were assumed to be available to the public payer at an 80% discount based on bulk purchasing. Costs of treating medical complications (microvascular, macrovascular, hypoglycaemia) associated with type 2 diabetes events (year 1) and health states (years 2+) were based on appropriate Danish-sourced estimates [40,41,42,43] or Swedish-sourced estimates [44] that were converted to Danish estimates (Appendix Table 9).
Productivity losses, which were only considered in ‘societal perspective’ scenarios, were based on the latest estimated annual productivity of labour from Statistics Denmark (www.dst.dk) across ages and gender, in combination with estimates of the % productivity loss per year associated with diabetes complications from Danish [45] and Swedish [46] sources (Appendix Tables 10 and 11). Costs were inflation-adjusted to 2022 DKK.
Utilities and disutilities associated with complications, including overweight, in the model are calculated based on corresponding HRQoL values identified in a review of utility values for economic modelling in type 2 diabetes [47,48,49,50,51], and disutilities associated with serious and non-serious hypoglycaemia events identified in a report [52] which was published after the main review article (Appendix Table 12). Based on EQ-5D questionnaire responses, UK patients with T2D participating in the UKPDS study provided baseline utility as well as many health-state related disutilities [48]. Retinopathy and macular oedema related disutilities were based on EQ-5D responses of Australian patients attending specialized eye clinics [50]. Disutilities associated with symptomatic neuropathy, peripheral vascular disease, macroalbuminuria, and high BMI were based on EQ-5D responses from European T2D patients [49]. Disutility associated with end-stage renal disease was based on EQ-5D responses from Swiss patients attending dialysis centres [51]. In all cases the UK EQ-5D tariffs were reported as being used. Disutilities associated with hypoglycaemia were from a North American and European T2D patient population participating in a time-trade-off study [52].
2.5 Scenario and Sensitivity Analyses
Model results can be substantially affected by the initially specified conditions and parameterization. To address uncertainty in model results, deterministic scenario and probabilistic sensitivity analyses were conducted. Furthermore, a set of scenario analyses were conducted to investigate key changes from base-case that may affect model results. Scenarios considered differences in values of cost inputs, quality of life parameters, time horizon, discount rates, and treatment intensification strategies. For the PIONEER 2 [15] and PIONEER 3 [16] trials, treatment policy estimands, which include the effects of rescue medications, were also considered in the scenario analyses. For each of the trials, probabilistic sensitivity analyses based on 2500 simulations were conducted (convergence plots: Appendix Figs. 1, 2, 3, 4). Distributional details are presented in Appendix Table 13, and where not otherwise available, standard errors were assumed equal to 10% of the mean parameter value (e.g., costs of complications).
3 Results
3.1 Base Case Analyses
In the PIONEER 2 trial, add-on oral semaglutide was compared with add-on empagliflozin in patients uncontrolled on metformin [15]. The baseline HbA1c level was 8.10%, and oral semaglutide was better at reducing HbA1c levels at 52 weeks (trial product estimands: − 1.30%, s.e. = 0.05 vs. − 0.79%, s.e. = 0.05). Total lifetime treatment costs for semaglutide were estimated as DKK 402,098 vs. DKK 375,299 for empagliflozin (Table 1). Total lifetime QALYs for semaglutide were estimated as 8.513 vs. 8.335 for empagliflozin. The base case ICER was estimated as DKK 150,618/QALY (€20,189).
In the PIONEER 3 trial, add-on oral semaglutide was compared with add-on sitagliptin in patients uncontrolled on metformin [16]. The baseline HbA1c level was 8.30%, and once daily oral semaglutide was better at reducing HbA1c levels at 52 weeks (trial product estimands: − 1.25%, s.e. 0.05 vs. − 0.52, s.e. 0.05). Total lifetime treatment costs for semaglutide were estimated as DKK 428,579 vs. DKK 405,643 for sitagliptin (Table 1). Total lifetime QALYs for semaglutide were estimated as 7.996 vs. 7.755 for sitagliptin. The base case ICER was estimated as DKK 95,093/QALY (€12,746).
In the SUSTAIN 2 trial, once-weekly add-on subcutaneous semaglutide was compared with add-on sitagliptin [17]. The baseline HbA1c level was 8.10%, and patients taking subcutaneous semaglutide experienced greater reductions in HbA1c at 56 weeks (trial product estimand: − 1.61%, s.e. 0.05 vs. − 0.55%, s.e. 0.05). The 56-week estimand was assumed equal to the 52-week estimand required for modelling. Total lifetime treatment costs for semaglutide were estimated as DKK 403,439 vs. DKK 368,961 for sitagliptin (Table 1). Total lifetime QALYs for semaglutide were estimated as 9.412 vs. 8.981 for sitagliptin. The base case ICER was estimated as DKK 79,982/QALY (€10,721).
In the SUSTAIN 8 trial, once-weekly add-on subcutaneous semaglutide was compared with add-on canagliflozin [18]. The baseline HbA1c level was 8.30%, and patients taking subcutaneous semaglutide experienced greater reductions in HbA1c at 52 weeks (trial product estimands: − 1.46%, s.e. 0.06 vs. − 0.98%, s.e. 0.06). Total lifetime treatment costs for semaglutide were estimated as DKK 586,322 vs. DKK 596,423 for canagliflozin (Table 1). Total lifetime QALYs for semaglutide were estimated as 9.150 vs. 8.961 for canagliflozin. The base case ICER was estimated as DKK 167,664/QALY (€22,474).
Across all analyses, greater initial HbA1c reductions associated with semaglutide resulted in greater time on treatment for semaglutide vs. comparator treatments (i.e., delayed treatment intensification to basal insulin treatment) (Table 1). Direct diabetes treatment costs were higher, which was partly offset by lower costs of both microvascular and macrovascular complications. Higher lifetime treatment costs are consistently accompanied by greater expected life expectancies and quality of life for treatment pathways initiated with semaglutide.
3.2 Sensitivity and Scenario Analyses
Compared with the base cases, the likelihood of semaglutide’s cost-effectiveness increased with increased costs of complications, lower discount rates, use of UKPDS-OM2 macrovascular risk equations [29] (Table 2). Adopting a societal perspective strongly supported the case of semaglutide’s cost-effectiveness and considering fixed 3-year treatment durations for the respective anti-diabetes treatments resulted in dominant results for semaglutide.
Considering shorter time horizons and discounting future costs and benefits at greater rates, as well as using UKPDS-OM1 mortality risk equation [28], reduce the likelihood of semaglutide-based treatment being cost-effective. Treatment policy estimands were available for the PIONEER 2 [15] and PIONEER 3 [16] studies, but not the SUSTAIN 2 [17] or SUSTAIN 8 [18] studies. Modelling using treatment policy estimands, which are affected by the confounding effects of additional diabetes medications (both from the cost and efficacy perspective), favours treatments where patients receive rescue medication at greater rates and reduces the likelihood of semaglutide’s cost-effectiveness.
A variety of analyses (Table 2: scenario sets 17–24) explored alternative assumptions about HbA1c thresholds triggering treatment intensification to basal and basal + bolus insulin regimens, as well as the extent to which interventional drugs were continued alongside insulin regimens prior to patient death. Compared with base case analyses, life-long treatment with interventional medicines was associated with higher incremental costs for semaglutide treatments. Only in scenarios which assumed that interventional medications were continued until death did estimated ICERs approach the upper end of what has been commonly considered cost-effectiveness threshold of 357,000 DKK (around €50,000) per QALY [53,54,55].
Cost-effectiveness planes and corresponding cost-effectiveness acceptability curves from probabilistic sensitivity analyses (1000 iterations per study) are presented in Fig. 1. Differences between ICERs from deterministic base cases and probabilistic sensitivity analyses are minimal and with the exception of the PIONEER 3 analysis, increase the likelihood that semaglutide represents a cost-effective treatment strategy.
As it is likely that the list prices of both oral and subcutaneous semaglutide will fall over time, scenario analyses were conducted for each trial reducing the list price of semaglutide (Fig. 2). Across all trials, treatment pathways involving semaglutide are modelled to become dominant treatment strategies at approximately a 40% discount.
The results of all sensitivity and scenario analyses provide consistent cost-effectiveness estimates below a commonly considered threshold of 357,000 DKK (around €50,000) per QALY [53,54,55].
4 Discussion
In this paper, we present results of lifetime cost-effectiveness analyses on four head-to-head clinical trials investigating the efficacy of oral (PIONEER 2 and PIONEER 3) and subcutaneous semaglutide (SUSTAIN 2 and SUSTAIN 8) compared to empagliflozin, canagliflozin, and sitagliptin. In all the head-to-head clinical trials, semaglutide was demonstrated to be clinically superior relative to the comparator with regards to the main trial outcome (i.e., % HbA1c reduction) [15,16,17,18].
Denmark does not have an official cost-effectiveness threshold by which to determine whether a treatment is ‘cost-effective’, but a threshold of 357,000 DKK (around €50,000) per QALY is sometimes assumed [53,54,55]. Considering Danish costs of medications, diabetes consumables, and treatment of diabetes-associated complications, modelling all four trials over a 40-year horizon, these analyses indicated that treatment with either oral or subcutaneous semaglutide (a GPL-1RA) was likely to increase both costs and health benefits relative to empagliflozin, canagliflozin (SGLT-2is), and sitagliptin (DDP-4i) for treatment of patients with type 2 diabetes that is not adequately controlled with metformin (with or without sulfonylurea) in Denmark. Base case ICERs ranged between 79,982 DKK/QALY (€10,720) and 167,664 DKK/QALY (€22,474) depending on the clinical trial being modelled.
As modelled, costs of diabetes treatments (i.e., medications and associated consumables) represent only approximately 15–30% of healthcare costs, with the remainder explained by costs of treating micro- and macrovascular complications. Higher costs in initial years of treatment with semaglutide (relative to empagliflozin, canagliflozin, and sitagliptin) are modelled to be partially offset by reduced costs treating comorbidities. Reduced incidences and delays to onset of diabetes-related complications associated with semaglutide-based treatment amounted to clinical benefits and greater expected quality of life for patients over the modelled time horizon.
There have been a number of publications discussing the cost-effectiveness of semaglutide which report conflicting headline results over the past years. The result of this set of analyses, suggesting that semaglutide is likely to be a cost-effective treatment in Denmark, are supported by publications supporting the cost-effectiveness of semaglutide based on some of the same clinical trials (PIONEER 2 and PIONEER 3) in the context of UK [56] and Swedish [57] healthcare systems. In contrast, two other recently published cost-effectiveness models considering the Danish context incorporating data from the PIONEER 2, SUSTAIN 2, and SUSTAIN 8 trials have reported that either oral [55] or subcutaneous semaglutide [54] is not likely to be cost-effective relative to empagliflozin.
The most obvious difference between modelling studies concerns handling time on treatment. In the two recent studies reporting that semaglutide is not likely to be cost-effective, the base case modelling assumes that treatment with empagliflozin or semaglutide would continue indefinitely [54, 55]. However, without reporting estimates, the same studies also discuss that when treatment with empagliflozin or semaglutide is modelled as discontinuing, semaglutide based treatment would be expected to be cost-effective in Denmark [54, 55]. The UK [56] and Sweden-based [57] studies model interventional treatments as discontinuing when treatment is intensified to insulin rather than continuing until patients death. While Danish [14] and international [13] guidelines do not recommend discontinuation of GPL1-RAs or SGLT-2is, based on Danish real-world evidence of the limits of treatment adherence to GLP-1RAs and SGLT-2is [58], it is believed that modelling the discontinuation of these medications at treatment intensification is the appropriate assumption. At 3 years post treatment initiation, adherence to SGLT-2is was 49.9% compared with 65.0% for GLP-1RAs [58]. This is both evidence that treatments such as SGLT-2is and GLP-1RAs should not be modelled as continuing indefinitely, and that model results which predict longer adherence to semaglutide are supported by real world evidence. As shown in Table 1, the modelled average years on semaglutide (ranging between 6.6 and 10.3 years) and empagliflozin (4.8 years) are longer than the suggested averages in Denmark based on the available real-world evidence for GPL1-RAs and SGLT-2is [58]. Only the Sweden-based study reported cost-effectiveness of semaglutide (oral) vs. sitagliptin [57].
Another area of inter-study differences in modelling has to do with the base case estimand used for modelling expected treatment efficacies. In the Danish modelling study comparing empagliflozin vs. oral semaglutide based on the PIONEER 2 study [55], the treatment policy estimand for HbA1c impacts was used in the base case, which includes the use of rescue medications (e.g., including insulin). The modelled estimated impacts of intensification to basal insulin are described as based on a formula [39] which excludes the potential prior exposure to insulin [55]. Furthermore, modelling studies assuming patients would not discontinue trial treatments is incoherent with use of treatment policy estimands which are estimated including reported HbA1c measures amongst patients who have discontinued trial medications. In contrast, the base case UK [56] and Swedish [57] modelling studies adopted the same trial product estimands as this modelling study has taken.
Danish and international guidelines state treatment goals for patients with T2D should be individualized, and because treatment guidelines suggest target ranges of HbA1c for different treatment goals, modelling treatment intensification varies between studies. In this study, base case intensification to insulin treatment has been modelled as occurring when HbA1c exceeds a target HbA1c level by 0.5% (i.e., > 5mmol/mol) corresponding with Danish treatment intensification recommendations [38]. In comparison, some modelling studies have implemented treatment intensification with insulin immediately upon reaching a target (e.g., intensification to basal insulin at HbA1c = 7.5% vs. 8%). Some of these studies find that semaglutide is unlikely to be cost-effective [54, 55], while others reported support for the likely cost-effectiveness of semaglutide [56]. Base case implementation of intensification with basal insulin at HbA1c = 8% was used in the Swedish modelling study [57]. Along with different criteria for discontinuation of treatment medications, intensification with basal and basal + bolus insulin at the HbA1c = 7.5% was explored across the four clinical trials (scenario sets 19–21). In the set of scenarios which included costs of investigational treatments (i.e., semaglutide, empagliflozin, canagliflozin, and sitagliptin) until patient death, the cited threshold of 357,000 DKK/QALY was approached, and slightly exceeded in the comparison of oral semaglutide and sitagliptin. Scenarios with investigational treatments discontinued prior to treatment intensification to basal + bolus insulin estimate ICERs approximately 10% lower (i.e., more favourable to semaglutide).
As with the disease itself, T2D economic models are complex. Underlying structural differences will affect modelled cost-effectiveness outcomes to some extent. For example, there may be differences in the sets of complications that are captured [59]. Models may also differ in implementations of treatment switching trigger conditions. Use of patient-level microsimulations may produce differences compared with cohort-level models such as the IHE-DCM. In a comparative study, Willis et al. [20], simulated analogous scenarios with both the IHE-DCM and ECHO-T2DM patient-level microsimulation model. The IHE-DCM was found to produced higher absolute life-years, QALYs, and cost for both treatment arms, which resulted in lower incremental costs and QALYs. However, incremental cost-effectiveness estimates were considered remarkably similar. User-friendliness and faster simulation times of a cohort model can be valuable for stakeholders evaluating the cost-effectiveness of T2D interventions [20].
Some patients with T2D will have established cardiovascular risks at the point that their treatment is intensified beyond first-line metformin. On the basis of cardiovascular outcomes trials (CVOTs) demonstrating reduced risks of major cardiovascular events (MACE), both GPL-1RAs and SGLT-2is are recommended for T2D patients with high cardiovascular risk [13]. Use of SGLT-2is have also demonstrated benefits and are recommended for patients with heart failure and chronic kidney disease [13]. The analyses presented in this paper are based on trial populations largely without baseline cardiovascular risks, and we have not investigated the potential impacts of including cardiovascular effects captured in CVOTs. Some relevant CVOTs are: EMPA-REG OUTCOME (empagliflozin) [60], CANVAS (canagliflozin) [61], TECOS (sitagliptin) [62], PIONEER 6 (oral semaglutide) [63], and SUSTAIN 6 (subcutaneous semaglutide) [64]. Differences in the outcomes reported across these CVOTs makes comparisons difficult, but the SGLT-2i [60, 61] and semaglutide [63, 64] CVOTs all reported reduced cardiovascular events for their trial medicines. Currently available diabetes health economic models have limitations accounting for cardiovascular effects [65, 66], but incorporation of cardioprotective effects remains important. Cost-effectiveness modelling in the Swedish context found that exploratory inclusion of effects reported from CVOTs moderately increased the likelihood that treatment with oral semaglutide was cost-effective relative to empagliflozin and sitagliptin [57]. Because cardiovascular disease is the most common cause of death amongst adults with diabetes in Denmark [67], further consideration of cardiovascular effects is relevant.
The true cost-effectiveness of any treatment is empirical, and it is a limitation that analyses of both costs and clinical outcomes are modelled rather than based on long-term empirical studies. Generalization of inputs into modelling studies is an inherent limitation. For example, it is unknown what differences between the baseline characteristics of patients in the clinical trials and those of the Danish population who would begin treatment with the trial medications would be, nor what differences this might have on average efficacy of treatments amongst patients being treated in Denmark (e.g., average reductions of % HbA1c). It is also a limitation that the baseline utility estimates, and utility decrements were not estimated from a Danish population.
Another limitation to be aware of is that the risk equations used in the IHE-DCM to model distributions across health states were not developed from a Danish population. The microvascular risk equations were developed from US [26] and UK [27] populations, macrovascular risk equations were developed from a Swedish population [30], and mortality risk equations were developed from a UK population [29].
However, there are no a priori reasons to expect that these limitations or the model used would systematically bias the results in favour of or against any of the treatments in the four trials modelled in this paper.
While reimbursement of hospital-based medicines in Denmark requires submission of cost-effectiveness models and accompanying analyses, this is not currently required for outpatient medicines such as the diabetes treatments discussed in this analysis. For countries where submission of models would be required for reimbursement of medications to treat type 2 diabetes, use of validated models such as the IHE-DCM has the advantage of being a discrete computer file which can be shared and verified by a reviewer.
5 Conclusion
This study shows that amongst patients with T2D which is inadequately controlled on metformin alone, in comparison with empagliflozin, canagliflozin, and sitagliptin, treatment with semaglutide (both daily 14 mg oral and weekly 1.0 mg subcutaneous injection) is likely to be associated with both increased cost and health benefits. It is also likely that this would occur under commonly considered cost-effectiveness thresholds. This is especially likely amongst patients who do not continue treatment with investigational medicines until death. As fewer complications associated with treatment with semaglutide lead to reduced productivity losses, the likelihood of semaglutide being cost-effective in Denmark is even higher considering a societal perspective.
References
Han H, et al. Association of a healthy lifestyle with all-cause and cause-specific mortality among individuals with type 2 diabetes: a prospective study in UK Biobank. Diabetes Care. 2022;45(2):319–29.
Faselis C, et al. Microvascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):117–24.
Viigimaa M, et al. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):110–6.
Magliano DJ, et al. Young-onset type 2 diabetes mellitus—implications for morbidity and mortality. Nat Rev Endocrinol. 2020;16(6):321–31.
Owens-Gary MD, et al. The importance of addressing depression and diabetes distress in adults with type 2 diabetes. J Gen Intern Med. 2019;34(2):320–4.
Danish Health Data Authority. Register of selected chronic diseases and severe mental disorders. 2022. https://www.esundhed.dk/Registre/Udvalgte-kroniske-sygdomme-og-svaere-psykiske-lidelser. Accessed 2022 January 25.
Statistics Denmark, Befolkningstal. 2022.
Guariguata L, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–49.
Sortsø C, et al. Societal costs of diabetes mellitus in Denmark. Diabet Med. 2016;33(7):877–85.
American Diabetes Association and the European Association for the Study of Diabetes, A.E., Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2022;45(1): S125–S143.
Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–51.
Ikeda M, Shimazawa R. Challenges to hemoglobin A1c as a therapeutic target for type 2 diabetes mellitus. J Gen Fam Med. 2019;20(4):129–38.
Davies MJ, et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Dansk Endokronologisk Selskab. Type 2 Diabetes. 2022. https://endocrinology.dk/nbv/diabetes-melitus/behandling-og-kontrol-af-type-2-diabetes/. Accessed 2022.
Rodbard HW, et al. Oral semaglutide versus empagliflozin in patients with type 2 diabetes uncontrolled on metformin: the PIONEER 2 Trial. Diabetes Care. 2019;42(12):2272–81.
Rosenstock J, et al. Effect of additional oral semaglutide vs sitagliptin on glycated hemoglobin in adults with type 2 diabetes uncontrolled with metformin alone or with sulfonylurea: the PIONEER 3 Randomized Clinical Trial. JAMA. 2019;321(15):1466–80.
Ahrén B, et al. Efficacy and safety of once-weekly semaglutide versus once-daily sitagliptin as an add-on to metformin, thiazolidinediones, or both, in patients with type 2 diabetes (SUSTAIN 2): a 56-week, double-blind, phase 3a, randomised trial. Lancet Diabetes Endocrinol. 2017;5(5):341–54.
Lingvay I, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(11):834–44.
Lundqvist A, et al. Validation of the IHE Cohort model of type 2 diabetes and the impact of choice of macrovascular risk equations. PLoS One. 2014;9(10): e110235.
Willis M, et al. Comparing the cohort and micro-simulation modeling approaches in cost-effectiveness modeling of type 2 diabetes mellitus: a case study of the ihe diabetes cohort model and the economics and health outcomes model of T2DM. Pharmacoeconomics. 2020;38(9):953–69.
NoMA, Hurtig metodevurdering ved forhåndsgodkjent refusjon—Ozempic (semaglutid) til behandling av type 2 diabetes mellitus. 2019.
TLV, Underlag för beslut om subvention—Ozempic (semaglutide). 2018.
TLV, Underlag för beslut om subvention—Xultophy. 2015. 2015.
TLV, Luxusia is included in the reimbursement system with limitation (Lyxumia ingår i högkostnadsskyddet med begränsning). 2018.
CADTH, Pharmacoeconomic Review Report - Semaglutide: For the treatment of adults patients with type 2 diabetes mellitus to improve glycemic control, in combination with metformin (second-line treatment), and in combination with metformin and sulfonylurea (third-line treatment). 2019, CADTH. p. 38.
Eastman RC, et al. Model of complications of NIDDM. I. Model construction and assumptions. Diabetes Care. 1997;20(5):725–34.
Bagust A, et al. An economic model of the long-term health care burden of type II diabetes. Diabetologia. 2001;44(12):2140–55.
Clarke PM, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom prospective diabetes study (UKPDS) outcomes model (UKPDS no. 68). Diabetologia. 2004;47(10):1747–59.
Hayes AJ, et al. UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia. 2013;56(9):1925–33.
Ahmad Kiadaliri A, et al. Towards renewed health economic simulation of type 2 diabetes: risk equations for first and second cardiovascular events from Swedish register data. PLoS One. 2013;8(5): e62650.
Davis WA, Knuiman MW, Davis TM. An Australian cardiovascular risk equation for type 2 diabetes: the Fremantle Diabetes Study. Intern Med J. 2010;40(4):286–92.
Palmer AJ, et al. Computer modeling of diabetes and its transparency: a report on the eighth Mount Hood challenge. Value Health. 2018;21(6):724–31.
Husereau D, et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics. 2022;40(6):601–9.
Danish Finance Ministery, Nøgletalskatalog. 2021.
Kahn SE, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355(23):2427–43.
NICE, Canagliflozin in combination therapy for treating type 2 diabetes (TA315), National Institute for Health and Care Excellence, Editor. 2014.
NICE, Canagliflozin, dapagliflozin and empagliflozin as monotherapies for treating type 2 diabetes [TA390]. National Institute for Health and Care Excellence, Editor. 2015.
Dansk Selskab for Almen Medicin (DSAM), Klinisk vejledning for almen praksis: type 2-diabetes—opfølgning og behandling. 2019. p. 82.
Willis M, et al. Multivariate prediction equations for HbA(1c) lowering, weight change, and hypoglycemic events associated with insulin rescue medication in type 2 diabetes mellitus: informing economic modeling. Value Health. 2017;20(3):357–71.
Brorholt G, et al. VIVE Rapport: En helhjertet indsats. VIVE: Copenhagen; 2018.
Jennum P, et al. Cost of stroke: a controlled national study evaluating societal effects on patients and their partners. BMC Health Serv Res. 2015;15:466.
Kjellberg J, et al. Short-term societal economic burden of first-incident type 2 diabetes-related complications—a nationwide cohort study. Expert Rev Pharmacoecon Outcomes Res. 2020;20(6):577–86.
Hoskins N, Tikkanen CK, Pedersen-Bjergaard U. The economic impact of insulin-related hypoglycemia in Denmark: an analysis using the local impact of hypoglycemia tool. J Med Econ. 2017;20(4):363–70.
Carlsson SK, et al. Påverkbara kostnader för typ 2-diabetes år 2020 och år 2030 i Sverige. Prognoser med IHE Cohort Model of Type 2 Diabetes. Lund, Sweden; 2015.
Sørensen J, Ploug UJ. The cost of diabetes-related complications: registry-based analysis of days absent from work. Econ Res Int. 2013;2013:1–8.
Persson S, et al. Days absent from work as a result of complications associated with type 2 diabetes: evidence from 20 years of linked national registry data in Sweden. Diabetes Obes Metab. 2020;22(9):1586–97.
Beaudet A, et al. Review of utility values for economic modeling in type 2 diabetes. Value Health. 2014;17(4):462–70.
Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Mak. 2002;22(4):340–9.
Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ. 2005;14(3):217–30.
Fenwick EK, et al. The impact of diabetic retinopathy and diabetic macular edema on health-related quality of life in type 1 and type 2 diabetes. Investig Ophthalmol Vis Sci. 2012;53(2):677–84.
Wasserfallen JB, et al. Quality of life on chronic dialysis: comparison between haemodialysis and peritoneal dialysis. Nephrol Dial Transplant. 2004;19(6):1594–9.
Evans M, et al. Health-related quality of life associated with daytime and nocturnal hypoglycaemic events: a time trade-off survey in five countries. Health Qual Life Outcomes. 2013;11:90.
Ehlers LH, et al. The cost-effectiveness of empagliflozin versus liraglutide treatment in people with type 2 diabetes and established cardiovascular disease. Diabetes Ther. 2021;12(5):1523–34.
Ehlers LH, et al. The cost-effectiveness of subcutaneous semaglutide versus empagliflozin in type 2 diabetes uncontrolled on Metformin Alone in Denmark. Diabetes Ther. 2022;13(3):489–503.
Ehlers LH, et al. The cost-effectiveness of oral semaglutide versus empagliflozin in Type 2 diabetes in Denmark. J Comp Eff Res. 2022;11(1):29–37.
Bain SC, et al. Oral semaglutide versus empagliflozin, sitagliptin and liraglutide in the UK: long-term cost-effectiveness analyses based on the PIONEER clinical trial programme. Diabetes Ther. 2020;11(1):259–77.
Eliasson B, et al. Long-term cost effectiveness of oral semaglutide versus empagliflozin and sitagliptin for the treatment of type 2 diabetes in the swedish setting. Pharmacoecon Open. 2022;6(3):343–54.
Nørgaard CH, et al. Cardiovascular outcomes with GLP-1 receptor agonists versus SGLT-2 inhibitors in patients with type 2 diabetes. Eur Heart J Cardiovasc Pharmacother. 2021;8:549–56.
Yi Y, et al. Economic models in type 2 diabetes. Curr Med Res Opin. 2010;26(9):2105–18.
Zinman B, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Rådholm K, et al. Canagliflozin and heart failure in type 2 diabetes mellitus: results from the CANVAS program. Circulation. 2018;138(5):458–68.
Green JB, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–42.
Husain M, et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2019;381(9):841–51.
Leiter LA, et al. Cardiovascular risk reduction with once-weekly semaglutide in subjects with type 2 diabetes: a post hoc analysis of gender, age, and baseline CV risk profile in the SUSTAIN 6 trial. Cardiovasc Diabetol. 2019;18(1):73.
Si L, et al. Evaluating the ability of economic models of diabetes to simulate new cardiovascular outcomes trials: a report on the ninth Mount Hood diabetes challenge. Value Health. 2020;23(9):1163–70.
Willis M, et al. Challenges and opportunities associated with incorporating new evidence of drug-mediated cardioprotection in the economic modeling of type 2 diabetes: a literature review. Diabetes Ther. 2019;10(5):1753–69.
Hansen MB, Jensen ML, Carstensen B. Causes of death among diabetic patients in Denmark. Diabetologia. 2012;55(2):294–302.
Acknowledgements
Thanks are given to Christian Tikkanen and Pierre Johansen, from Novo Nordisk, for reviewing model assumptions and providing feedback on a draft manuscript. Thanks are given to Asger Lindvig, from NHTA, for strategic advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funded by Novo Nordisk Denmark, Denmark.
Conflict of interest
RP and NL are employed by NHTA, which provides consulting services for commercial life-sciences enterprises, including funding from Novo Nordisk.
Data availability
All data used in the analyses are available in the article tables and/or online appendices.
Code availability
The economic model has been used under licence and is proprietary intellectual property of the Swedish Institute for Health Economics, Lund, Sweden. For access, please contact Sofie Persson at IHE (sofie.persson@ihe.se).
Authors contributions
RP and NL were involved in data extraction, modelling, results interpretation, and creating the manuscript.
Ethics approval
Not applicable.
Consent for participation
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pulleyblank, R., Larsen, N.B. Cost-Effectiveness of Semaglutide vs. Empagliflozin, Canagliflozin, and Sitagliptin for Treatment of Patients with Type 2 Diabetes in Denmark: A Decision-Analytic Modelling Study. PharmacoEconomics Open 7, 579–591 (2023). https://doi.org/10.1007/s41669-023-00416-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-023-00416-z