Abstract
Background
In low- and middle-income countries (LMICs), provisioning for surgical care is a public health priority. Ayushman Bharat Pradhan Mantri-Jan Aarogya Yojana (AB PM-JAY) is India’s largest national insurance scheme providing free surgical and medical care. In this paper, we present the costs of surgical health benefit packages (HBPs) for secondary care in public district hospitals.
Methods
The costs were estimated using mixed (top-down and bottom-up) micro-costing methods. In phase II of the Costing of Health Services in India (CHSI) study, data were collected from a sample of 27 district hospitals from nine states of India. The district hospitals were selected using stratified random sampling based on the district’s composite development score. We estimated unit costs for individual services—outpatient (OP) visit, per bed-day in inpatient (IP) and intensive care unit (ICU) stays, and surgical procedures. Together, this was used to estimate the cost of 250 AB PM-JAY HBPs.
Results
At the current level of utilization, the mean cost per OP consultation varied from US$4.10 to US$2.60 among different surgical specialities. The mean unit cost per IP bed-day ranged from US$13.40 to US$35.60. For the ICU, the mean unit cost per bed-day was US$74. Further, the unit cost of HBPs varied from US$564 for bone tumour excision to US$49 for lid tear repair.
Conclusions
Data on the cost of delivering surgical care at the level of district hospitals is of critical value for evidence-based policymaking, price-setting for surgical care and planning to strengthen the availability of high quality and cost-effective surgical care in district hospitals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Provision of safe, timely and affordable access to surgical care is a key strategy to achieve universal health coverage in low-and middle-income countries. |
The phase II of the Costing of Health Services (CHSI) study—a nationally representative study, is the first in India to generate evidence on cost of surgical care in public sector secondary care hospitals. |
The cost evidence presented in our paper is critical for the implementation of the India’s national insurance program (AB PM-JAY) including its price setting, planning to scale-up public sector district hospitals to provide comprehensive surgical care, as well as determining efficiency of surgical interventions. |
1 Background
The provisioning of surgical care has become a public health priority with the disease pattern transitioning towards chronic and non-communicable diseases [1]. The Lancet Commission on Global Surgery estimated a requirement of 5000 surgeries per 100,000 population in low- and middle-income countries (LMICs) [2]. However, 5 billion people worldwide do not have access to safe surgical care. In India, the number of surgical procedures per 100,000 population is among the lowest in the world (50–499 surgeries per 100,000) [3]. It is estimated that 90% of the rural population in India lacks safe and timely access to surgical care [4]. Most patients visit the doctor to seek health care, but 42% cannot get surgical care for various reasons, with one of the major being financial constraints (34.5%) [5].
To achieve universal health coverage (UHC), the Indian federal and state governments offer several surgical treatments for common conditions, such as obstetrics, cataracts and general surgical procedures through their public sector hospitals [6]. However, a large section of the Indian population reportedly lacks access to safe and timely surgical interventions [4]. To address this unmet need, the Government of India in September 2018 launched Ayushman Bharat Pradhan Mantri-Jan Aarogya Yojana (AB PM-JAY), the largest tax-funded national health insurance scheme, to provide free coverage of hospitalization care for 100 million families. The AB PM-JAY could become an important vehicle for ensuring accessible and affordable surgical care in India.
AB PM-JAY provides coverage of 500,000 Indian rupees (₹) (US$7000, approximately) per family per year for secondary and tertiary care hospitalization services [7]. The services are provided through the empanelled public and private hospitals. About 60% of the health benefit packages (HBPs) covered under AB PM-JAY are for the disease categories/conditions that require surgical interventions [8]. This is a significant step forward to provide cashless treatment and to reduce the unmet need for surgical care.
One of the critical operational aspects for the successful implementation of AB PM-JAY is appropriate price setting. The empanelled health care providers (EHCPs) under the AB PM-JAY are paid based on case-based bundled payments specific to a given procedure. The payment is inclusive of any outpatient diagnostics before the procedure, procedure cost, subsequent hospitalization, and medicines for 15 days following hospitalization. AB PM-JAY coverage is currently available for hospitalization involving 1949 surgical and medical procedures [9, 10]. This is important to set the right incentives from both the demand and supply side for providing surgical care [11]. However, price setting is critically dependent on good quality evidence on the cost of providing health care [12]. A recent paper alluded to gross deficiency of good quality evidence on the cost of surgical care services [13]. Although a national database for healthcare costs has been established, it does not have evidence on tertiary care [14]. Moreover, surgical costs at the secondary level are available as speciality level estimates of outpatient and inpatient costs instead of procedure-specific costs. Such procedure-specific costs are critical for price-setting of surgical care as well as assessing the cost effectiveness of alternative surgical techniques.
In order to fill this evidence gap, the ‘Costing of Healthcare Services in India’ (CHSI) study was commissioned [15]. The objective of the CHSI study is to estimate the unit cost of individual healthcare services and the HBPs covered under the AB PM-JAY scheme [15, 16]. It is a four-phased study which includes a sample of the public tertiary hospitals (phase I), public district hospitals (phase II), private hospitals (phase III) and phase IV of the study covers remaining specialities in the tertiary public hospitals. The CHSI phase I results were used as cost evidence for price setting under the AB PM-JAY in 2019 [17].
In this paper, we present the findings of phase II of the CHSI study covering 27 public district hospitals from nine states of India. The district hospitals provide secondary care services for surgical and medical care. As per the Indian Public Health Standards (IPHS), general surgery, obstetrics and gynaecology (OBG), ophthalmology, otolaryngology (ENT) and orthopaedics are the essential/minimum assured services at the level of district hospitals [18]. Therefore, the cost data was collected for the above-mentioned surgical specialities at the level of district hospitals. This paper will provide cost information for five surgical specialities—general surgery, OBG, ophthalmology, ENT and orthopaedics for individual services (outpatient, inpatient, intensive care, operative care) and the cost of AB PM-JAY HBPs provided at the level of district hospitals. Our paper presents the first nationally representative evidence on the cost of surgical care at public secondary care hospitals, which will be crucial for subsequent revision of reimbursement prices for HBPs.
2 Methods
2.1 Study Overview and Sampling
The CHSI study includes public sector hospitals (i.e. tertiary and district hospitals) as well as private hospitals. For sampling of the hospitals, a multi-stage stratified sampling was undertaken. The study methodology and sampling strategy are explained in detail in the CHSI protocol, process evaluation and the results paper describing findings from phase I of the data collection in public sector tertiary care hospitals [15,16,17]. Further details of the sampling methodology are provided in the electronic supplementary material (ESM) S1.
To represent the heterogeneity based on the geography, human development index (HDI), gross state domestic product (GSDP) and health workforce density, 11 states of India were sampled. The states included in the study were Jammu and Kashmir, New Delhi, Rajasthan, Uttar Pradesh, Bihar, West Bengal, Gujarat, Odisha, Maharashtra, Andhra Pradesh and Tamil Nadu. However, for secondary-care-level costing at the public district hospitals, New Delhi was excluded due to administrative reasons and data collection could not be completed in Jammu and Kashmir. For the purpose of costing surgical care at district hospitals, data were collected from 27 district hospitals in nine states (ESM, S1). The district hospitals within a given state were selected using stratified sampling. One district hospital was randomly selected from each of the three tertiles, stratified based on a composite index drawn from socioeconomic, demographic and healthcare utilization indicators [19]. Therefore, a representative sample from nine states captures the heterogeneity in cost based on geography, volume of services and bed size [20].
2.2 Data Collection
2.2.1 Study Perspective and Costing Approach
The standard principles of health system costing were used for the CHSI study [15, 21, 22], which was further guided by the previous studies in similar settings [15, 17, 23,24,25]. The cost of healthcare services was calculated following the concept of economic costing and a mixed (top-down and bottom-up) micro-costing methodology. The detailed information on costing of different services is provided in ESM, S2.
The study estimated the unit cost of individual services (outpatient, inpatient, operation theatre) and AB PM-JAY HBPs for the five surgical specialities (i.e. general surgery, OBG, ophthalmology, ENT and orthopaedics). A few of the AB PM-JAY HBPs which are linked to be performed by specialists in the urology department were being performed at the sampled district hospitals by the general surgeons. The cost of such HBPs was also calculated. At the level of each district hospital, the cost of all the speciality-specific HBPs was calculated.
2.2.2 Measurement and Valuation of Resources
The first step was the identification of centres, and a list of cost centres was prepared for each hospital. The next step was to measure and value the input resources required for the service delivery. Lastly, for each cost centre, the annual quantity of outputs produced and inputs used for this were identified and their quantity was measured. The data were collected from routine physical or electronic records at the cost centre and hospital levels. A detailed description of sources of data, prices of input resources, apportioning of shared costs, assumptions and the data analysis were published in the protocol, process evaluation and CHSI phase I results paper [15,16,17]. The data in district hospitals for phase II of the CHSI study were collected from April 2019 to March 2021. Challenges due to the COVID-19 pandemic delayed the process of data collection. However, it did not affect the quality of data as the cost data was collected retrospectively for the financial year 2017-18.
2.3 Data Analysis
2.3.1 Estimation of the Unit Cost of Individual Services
For each cost centre, the total cost was valued by summing up capital and recurrent resources. The capital cost was annualized to calculate the equivalent annualized uniform cost using a discount rate of 3% [21,22,23,24,25,26]. The annual cost of each recurrent resource was calculated by multiplying the unit procurement price by the annual number of inputs consumed. The unit cost for the cost centre was calculated by the ratio of total annual cost and number of services delivered. The unit costs of surgical services were estimated cost per outpatient (OP) visit, inpatient (IP) bed-day and intensive care unit (ICU) bed-day. To derive an average cost estimate, the mean and median unit cost along with the range and interquartile range across the district hospitals were computed.
2.3.2 Estimation of the Unit Cost of AB PM-JAY Health Benefit Packages (HBPs)
The cost of an AB PM-JAY HBP was estimated by adding up the values obtained by multiplying the unit cost data for all the individual services within an HBP (i.e. outpatient consultation, inpatient care, intensive care, surgery, etc.) and multiplied it by the number of times (i.e. number of visits, procedure or bed-days of inpatient stay) an individual service was utilized for HBP (Fig. 1).
The provisioning of surgical care varies across different district hospitals. For each surgical speciality, there were two types of procedures, surgeries performed in the district hospital during the reference year and surgeries not performed. For some of the surgical HBPs, although the resources were available, no surgery was undertaken due to low incidence or disease burden. The unit cost of such surgical HBPs was calculated by multiplying cost per hour for the functional operation theatre with the average time taken to perform the surgery. The data on average time per surgery was calculated based on the expert opinion of the surgeons of the respective departments.
In Indian public sector hospitals, data on the use of individual services for AB PM-JAY HBPs were not maintained due to a lack of electronic health records. Therefore, HBP data on the number of outpatient visits, diagnostics, surgery time in the operation theatre and average length of stay in the ICU and inpatient department was collected based on expert opinion. The experts were surgical specialists (1–8) working in the district hospitals in different specialities. For each speciality, data on clinical inputs was collected based on an expert group meeting involving at least 25% of the specialists. Consensus was achieved based on existing clinical practices followed by expert opinion. In case a difference in opinion persisted, the arbitration was done by two experts who were purposively chosen from a teaching hospital. However, the latter was undertaken in only two instances. The unit cost of individual services such as OP visits, IP or ICU bed-days and surgery cost was based on the primary data collection. There is a lack of published data on the unit cost of diagnostic tests required during hospitalization from the health system perspective. Therefore, the present study used reimbursement rates from a national health insurance scheme, CGHS (Central Government Health Scheme), which provides comprehensive medical care to central government employees and pensioners. All costs represent prices for the 2017–18 financial year and are reported in US dollars ($) and Indian rupees (₹) (US$1 = ₹66.20).
Each district hospital functions at a different level of capacity utilization. To adjust for the variation in capacity utilization, unit costs were standardized to 80% and 100% of full capacity. Based on discussions with the payer (National Health Authority [NHA]), it was decided that the cost estimates for pricing decisions should be adjusted for the level of capacity utilization. Herein, a consensus was to present the estimates at 100% of capacity utilization. Since it is difficult to achieve 100% capacity utilization, we chose to present the findings for estimates of unit costs at both 80% and 100% capacity utilization. Further, similar presentation of unit cost data at 80% and 100% capacity utilization is available in published literature [17, 24]. Bed occupancy rate was used as a standard indicator to adjust for capacity utilization [20].
The input resources were divided into fixed and variable costs. Fixed costs included human resources, building, furniture and equipment. Unlike other classifications, we considered human resources as a fixed cost since norms for human resources at the facility level are set independent of the level of utilization and is rather constant for each district hospital. Variable costs included drugs, consumables, diagnostics, utilities (dietetics and laundry) and overheads (electricity, water, etc). The unit costs of AB PM-JAY HBPs were calculated in two scenarios: (i) full variable and full fixed costs and (ii) full variable cost but 50% fixed cost. As one of the objectives of the CHSI study was to inform pricing decisions under the PM-JAY, extensive discussions were held with the payer organization, NHA, on how the cost results would be used for price setting. The EHCPs under the PM-JAY comprise both public and private hospitals. Public hospitals are funded through general taxation via supply-side funding to create infrastructure, pay salaries and provide supplies. Hence, it may not be appropriate to pay the full cost of providing service to public hospitals. Similarly, it was felt that most private hospitals operate at below their full capacity utilization. The PM-JAY scheme will create demand for health care, which will fill this idle capacity in the private sector. Hence, in order to be a strategic purchaser, the NHA decided to use the latter of the two scenarios (i.e. partial cost) as a base cost scenario for price consultations. For the purpose of the unit cost of HBPs, standardized 100% capacity utilization was used in consultation with the NHA [17].
3 Results
The distribution of functional speciality-wise services (i.e. outpatient, inpatient, intensive care and operative care) is presented in Table 1. The specialities of general surgery and OBG have outpatient care, inpatient care and operative surgical care being delivered in all the sampled hospitals. Outpatient, inpatient and surgical care for ophthalmology were being provided in 26, 23 and 22 district hospitals, respectively. Similarly, for orthopaedics and ENT, outpatient, inpatient and surgical care were being provided in 26, 23 and 17, and 26, 23 and 22 district hospitals, respectively. A mixed ICU facility catering to multiple specialities was present in 18 hospitals.
The sampled district hospitals provided healthcare services to 125,252 outpatient care visits, 15,032 inpatient admissions and 6894 operative services per district hospital in the reference year. The speciality of OBG has the maximum number of average patient footfalls per district hospital in OP (36,006), IP (8796) and operation theatre (OT) (4724) settings.
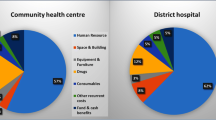
For surgical care at the level of public sector district hospitals, the share of fixed and variable resources were valued at 64% and 36%, respectively. At the speciality level, the share of fixed resources was 74% in ENT, 71% in ophthalmology, 67% in general surgery, 66% in orthopaedics, and 57% in OBG. The detailed distribution of input resources in each speciality is provided in Fig. 2.
3.1 Unit Costs of Specific Services
The mean unit costs with range (minimum–maximum) and corresponding median costs along with interquartile ranges per OP consultation and bed-day hospitalization in US dollars are presented in Table 2. The corresponding unit cost estimates in Indian rupees (₹) are provided in Table S1 (see ESM). The mean unit cost per OP consultation varied from US$4.10 (₹271) for ophthalmology to US$2.60 (₹172) for ENT. At 100% capacity utilization, the highest cost per OP consultation was observed for OBG at US$4.30 (₹285) and the lowest for ophthalmology and ENT at US$2.00 (₹132) (Table 2).
In the IP department, the bed occupancy rate was highest for the OBG at 168% and lowest for the ophthalmology at 53%. The highest mean unit cost per bed-day in IP was US$35.60 (₹2357) for ophthalmology and the lowest was US$13.40 (₹887) for the orthopaedics department at the current level of utilization (Table 2).
For the mixed speciality ICU, the average bed occupancy rate was 88%. The mean and median unit cost per bed-day along with range and interquartile range was US$74 (8–421) (₹4903 [552–27,842]) and US$37 (58) (₹2473 [3807]) at current bed occupancy. At 80% bed occupancy, the mean and median unit cost was US$44 (11–154) (₹2918 [707–10,224]) and US$33 (31) (₹2150 [2048]), respectively. The mean and median unit cost at 100% bed occupancy was US$38 (10–133) (₹2544 [645–8832]) and US$29 (24) (₹1904 [1585]), respectively.
The cost of human resources constituted the highest proportion of the unit cost for an OP consultation (60%), IP care (49%) and ICU admission (65%). This share of the cost of human resources varied from 41% (OBG) to 72% (general surgery & ophthalmology) in case of OP visit, and 40% (OBG) to 68% (ENT) in IP care. Drugs constituted the second-highest share of the cost for both OP and IP care.
3.2 Unit Cost of AB PM-JAY Surgical HBPs
The unit cost for the top five AB PM-JAY HBPs as per the number of claims (highest to lowest) in US dollars is provided in Table 3. Similarly, the heterogeneity in the unit cost evidence is presented in Fig. 3. The detailed unit cost information for all 250 of the AB PM-JAY HBPs available at the public district hospital level in US dollars and Indian rupees is given in Table S2 and S3, respectively (see ESM). Out of 250 HBPs, 43 HBPs required an implant during the surgical procedure. A comparison of unit cost information for these 43 HBPs with and without implant cost in US dollars and Indian rupees is given in Tables S4 and S5, respectively (see ESM).
The HBPs that were found to have the highest cost in general surgery, OBG, ophthalmology, orthopaedics and ENT were resection anastomosis–open US$719 (₹47,598), high-risk delivery–mothers with eclampsia / imminent eclampsia / severe pre-eclampsia US$365 (₹24,163), capsulotomy (YAG) US$256 (₹16,947), bone tumour (benign) curettage/excision and bone grafting US$564 (₹37,337) and open sinus surgery US$430 (₹28,466), respectively. Similarly, the HBPs that had the lowest cost in general surgery, OBG, ophthalmology, orthopaedics and ENT were biopsy–lymph node US$83 (₹5495), cervix cancer screening (PAP + colposcopy) US$36 (₹2383), lid tear repair US$49 (₹3244), excision arthroplasty of femur head US$63 (₹4171) and deep neck abscess drainage/post-trauma neck exploration US$86 (₹5693), respectively.
4 Discussion
The district hospitals are secondary referral centres providing comprehensive secondary health care. This becomes especially important since there is a shortfall of surgeons (78.9%) and obstetricians (69.7%) at the level of community health centres, which are the first point of contact for surgical care [27]. Therefore, practically the provisioning of surgical care starts at the level of the district hospital in India. Evidence on the cost of surgical care at public secondary care hospitals is crucial for the implementation of AB PM-JAY and subsequent revision of reimbursement prices, planning augmentation of the capacity at district hospitals to provide comprehensive surgical care and cost data that will be useful for HTA researchers and hospital planners. Further, the CHSI study’s design, methodology, data collection tools and linkage of cost evidence with research and policy making will guide the planning of similar costing studies in other LMICs.
However, there is a dearth of evidence on cost of surgical care in India. All the previously published studies report the cost of surgical care as unit cost for outpatient, inpatient and intensive care services, at the level of speciality, rather than individual disease management cost [24, 25, 28, 29]. Secondly, while the previous studies provide unit costs of specific services, these do not provide the full cost for a HBP comprising all services delivered while treating a given condition. Finally, most of these previous studies focused on a single or few specialities only. In contrast, we provide comprehensive estimates for 250 health benefit packages, for all major surgical procedures provided at secondary level hospitals, using standard costing methods. Further, we report disaggregated cost estimates in a variety of different scenarios, which is a useful tool for the NHA for price-setting and strategic purchasing. At present, the AB PM-JAY HBPs are paid, based on case-based bundled payments specific to a given procedure, to the EHCPs from both public and private sectors.
The unit cost of the outpatient and inpatient surgical care at district hospitals in our study, adjusted for capacity utilization, is very similar to that reported at tertiary hospital level. While the mean unit cost of OP and IP care at district hospitals varies from US$0.30 to US$14.10 (₹20–₹933) and US$1.40 to US$131.00 (₹93–₹8672), respectively, this is lower than the mean unit cost of OP and IP care for similar surgical specialities at tertiary public hospitals, that is, US$2.30–US$6.20 (₹153–₹410) and US$11–US$18 (₹725–₹1173), respectively [17]. However, when combined with the cost of surgical procedures, the average cost of common HBPs was on average 30% less in the district hospitals as compared with the tertiary hospitals. This is as a result of less specialized manpower and infrastructure, and lower salaries of staff. In addition, it could also be explained possibly on the basis of differences in severity-mix of patients. The cost information generated as part of the CHSI phase II will be subsequently fed into the national cost database of India [14].
Chatterjee et al. 2013 estimated the unit cost of caesarean delivery, hysterectomy and appendectomy at a single district hospital and reported it to be US$37 (₹2469), US$62 (₹4124) and US$37 (₹2421), respectively [28]. These are much lower than the cost of overall HBP that we have reported. The difference in cost findings can be explained as the former study only included the cost of operative care and not the full cost of an HBP. The cost of the surgical procedure alone in the Chatterjee study was also 67%, 63% and 62% less than our study, respectively. This could partly be explained based on the fact that the previous study took a health system perspective and did not account for what the patients spent. It is well recognized that the patients spend a significant amount as out-of-pocket expenditure [23, 30,31,32]. In our study, we also valued the resources for which the patients had paid for. Secondly, Chatterjee studied the costs in a single hospital, while we had a large sample of 27 hospitals chosen from several states. Thus, our study estimates are more comprehensive and represent heterogeneity in costs.
The CHSI phase II costs were also compared with the inflation-adjusted estimates from the previous studies. For instance, the median unit cost of overall OP and IP care reported by Prinja et al. (2017) was within a range of 10% at the current level of utilization [24]. There is wide heterogeneity in the cost because of the differences in infrastructure, non-uniform salaries across states, and different prices for drugs, consumables and equipment. There is a need for further research to explore the factors leading to heterogeneity in the cost data.
In 2019, the CHSI phase I cost evidence was used by the NHA as a base cost during the price consultations and revision of AB PM-JAY HBPs [17]. The current information on the cost of surgical care would be useful evidence for NHA for subsequent revision of AB PM-JAY HBPs prices pertaining to secondary level HBPs, especially if differential price is considered for secondary and tertiary care facilities. It will provide guidance for evidence-based scale-up of secondary care surgical services at district hospitals. Further, the data from the secondary care HBPs can be used along with tertiary care data (CHSI phase I) to develop a cost function which can be used for developing the price weights.
As the availability of surgical care is heterogenous in the district hospitals, the CHSI cost evidence will be helpful in scaling up of service delivery for AB PM-JAY HBPs. We found that there was heterogeneity in the extent of functionality of surgical care across the sampled district hospitals. While the specialities of general surgery and obstetrics & gynaecology (OBG) were available in all the sampled hospitals, this was not the case for ophthalmology, otolaryngology and orthopaedic care, where availability was not uniform. There is an urgent need to scale up the district hospitals to a level that all the AB PM-JAY HBPs for secondary level surgical care become available.
A possible strategy to strengthen the district hospitals is to reserve the secondary care HBPs for the district hospitals. Presently, in many states, some of the HBPs are reserved only for the public sector district hospitals [33]. This implies a gatekeeping strategy whereby certain HBPs needing secondary care are only implemented at the district hospital level. This has a significant cost-saving potential for the NHA and AB PM-JAY by reimbursing differential pricing for district hospitals. Should this be the case, the NHA could set differential prices of surgical HBPs delivered at the secondary level versus tertiary care level. The cost provisioning of similar HBPs was on an average 28% less in the district hospitals than the tertiary hospitals. Further, it reduces the burden on tertiary level hospitals, which are already overburdened. However, such a strategy implies enforcing the choice of health care providers, which requires a stronger regulatory role and political will.
An alternative approach is that the NHA continues to provide a common reimbursement price for services. In such cases, the district hospitals stand to gain for every service provided as the cost of healthcare delivery is lower than the price in the tertiary hospitals. This excess revenue should be used for the augmentation of infrastructure and quality of care. This would in turn make the AB PM-JAY a vehicle to strengthen the public health system at the district level. Experience from other countries also suggests that the creation of revenue generation at lower-level facilities as well as the policy of retaining the revenue to be utilized for quality improvement leads to an overall augmentation of service coverage and quality [34]. This will also increase the accessibility of surgical care at the population level as the district hospitals will cater to patients from relatively more rural and remote areas for whom tertiary care hospitals are more distant. In other words, strengthening the district hospitals for the provision of surgical care can also lead to equitable outcomes.
Our study has a few limitations, primarily attributed to the lack of disaggregated data on input resources [17]. Firstly, the data on utilization of certain resources such as overheads is pooled at the level of hospital or drugs and consumables and is aggregated at the cost centre. As a result, such resources had to be apportioned for each specific service. Secondly, we did not collect data on patient characteristics. As a result, we are limited to providing the heterogeneity in the cost of HBPs based on the severity of the disease condition. However, since we provide the cost of individual services which constitute a given HBP, these unit costs along with data on the quantity of individual services in conditions with varying severity can be used to update the estimates. We recommend that future studies should focus on collecting more granular data on patient characteristics which could help improve the use of cost data for price setting. Thirdly, the provider payment rates under the CGHS—a national social health insurance scheme were used as a proxy for the cost of diagnostic tests. However, since this is a large scheme, its prices are considered representative. Fourthly, there is significant heterogeneity in the cost of service delivery at the level of district hospitals. There are multiple supply-side and demand-side factors which influence the cost trends. Further, the share of input resources varies across different cost centres (OP, IP, OT) within the same speciality. It is an important area for future research to identify and explain the reasons for heterogeneity in the cost estimates in the district hospitals. Fifthly, the data collection in the state of Meghalaya was not initiated due to administrative reasons. As we could not include any district hospitals from north-east India, it may influence the generalizability of our estimates. Finally, the quality of services varies between hospitals and states as well. However, we did not collect data on the quality of healthcare services in the public district hospitals.
5 Conclusions
Provisioning of surgical care is an important step to achieve universal health coverage and financial risk protection. Further, the AB PM-JAY through its cashless hospitalization care has attempted to improve access to surgical care. In this scenario, district hospitals should be strengthened to play an important role to achieve these goals. The data on costs of delivering surgical care at the level of district hospitals is a critical value addition for evidence-based policymaking, price setting for secondary-level surgical care and planning for strengthening district hospitals in terms of availability as well as the quality of surgical care.
References
Ologunde R, Maruthappu M, Shanmugarajah K, Shalhoub J. Surgical care in low and middle-income countries: burden and barriers. Int J Surg. 2014;12(8):858–63.
Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624.
Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN. Essential surgery: disease control priorities, third edition (volume 1). Washington (DC); 2015.
Lancet Commission on Global Surgery Consensus C. The Lancet Commission on Global Surgery—Association of rural surgeons of India Karad consensus statement on surgical system strengthening in Rural India. Healthcare. 2019;7(2):7–9.
Vora K, Saiyed S, Shah AR, Mavalankar D, Jindal RM. Surgical unmet need in a low-income area of a metropolitan city in India: a cross-sectional study. World J Surg. 2020;44(8):2511–7.
Okoroh JS, Chia V, Oliver EA, Dharmawardene M, Riviello R. Strengthening health systems of developing countries: inclusion of surgery in universal health coverage. World J Surg. 2015;39(8):1867–74.
Pradhan Mantri Jan Arogya Yojana (PM-JAY) New Delhi 2021. https://pmjay.gov.in/about/pmjay.
Journey from HBP 1.0 to HBP 2.0 New Delhi: National Health Authority; 2020. https://pmjay.gov.in/sites/default/files/2020-01/Journey-from-HBP-1.0-to-HBP-2.0.pdf.
NHA launches new version of Health Benefit Package under AB-PMJAY adding 365 new procedures. Thehindu.com. 2022. https://www.thehindu.com/news/national/nha-launches-new-version-of-health-benefit-package-under-ab-pmjay-adding-365-new-procedures/article65303372.ece. Accessed 20 Apr 2022.
Financing of The Scheme [Internet]. Pmjay.gov.in. 2022. https://pmjay.gov.in/about/pmjay. Accessed 20 Apr 2022.
Figueras J, Robinson REJ. Purchasing to improve health systems performance. Berkshire: University Open Press; 2005.
Bahuguna P, Guinness L, Sharma S, Chauhan AS, Downey L, Prinja S. Estimating the unit costs of healthcare service delivery in India: addressing information gaps for price setting and health technology assessment. Appl Health Econ Health Policy. 2020;18(5):699–711.
Prinja S, Chauhan AS, Rajsekhar K, Downey L, Bahuguna P, Sachin O, et al. Addressing the cost data gap for universal healthcare coverage in India: a call to action. Value Health Reg Issues. 2020;21:226–9.
National Health System Cost Database for India Chandigarh, India: Department of Community Medicine & School of Public Health, PGIMER. https://www.healtheconomics.pgisph.in/costing_web/.
Prinja S, Singh MP, Guinness L, Rajsekar K, Bhargava B. Establishing reference costs for the health benefit packages under universal health coverage in India: cost of health services in India (CHSI) protocol. BMJ Open. 2020;10(7): e035170.
Prinja S, Brar S, Singh MP, Rajsekhar K, Sachin O, Naik J, et al. Process evaluation of health system costing—experience from CHSI study in India. PLoS ONE. 2020;15(5): e0232873.
Prinja S, Singh MP, Rajsekar K, Sachin O, Gedam P, Nagar A, et al. Translating research to policy: setting provider payment rates for strategic purchasing under India's National Publicly Financed Health Insurance Scheme. Appl Health Econ Health Policy. 2021.
Indian Public Health Standards (IPHS) Guidelines for District Hospitals (101 to 500 Bedded). 2012. https://nhm.gov.in/images/pdf/guidelines/iphs/iphs-revised-guidlines-2012/district-hospital.pdf.
Ram F, Shekhar C. Ranking and mapping of districts. Mumbai: International Institute for Population Sciences; 2006.
Özaltın A, Cashin C (eds.) Costing of health services for provider payment: a practical manual based on country costing challenges, trade-offs, and solutions. 2014.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programme. 3rd ed. Oxford: Oxford University Press; 2005.
Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009;18(10):1188–201.
Singh MP, Chauhan AS, Rai B, Ghoshal S, Prinja S. Cost of treatment for cervical cancer in India. Asian Pac J Cancer Prev. 2020;21(9):2639–46.
Prinja S, Balasubramanian D, Jeet G, Verma R, Kumar D, Bahuguna P, et al. Cost of delivering secondary-level health care services through public sector district hospitals in India. Indian J Med Res. 2017;146(3):354–61.
Prinja S, Chauhan AS, Bahuguna P, Selvaraj S, Muraleedharan VR, Sundararaman T. Cost of delivering secondary healthcare through the public sector in India. Pharmacoecon Open. 2020;4(2):249–61.
Health Technology Assessment in India A Manual. New Delhi: Department of Health Research; 2018.
Rural Health Statistics 2019–20. New Delhi: Ministry of Health & Family Welfare, Division S.
Chatterjee S, Levin C, Laxminarayan R. Unit cost of medical services at different hospitals in India. PLoS ONE. 2013;8(7): e69728.
Bahuguna P, Khanduja P, Prinja S. Economic analysis of delivering postpartum intrauterine contraceptive device services in India. Indian J Commun Med. 2019;44(2):147–51.
Sharma D, Prinja S, Aggarwal A, Bahuguna P, Sharma A, Rana S. Out-of-pocket expenditure for hospitalization in Haryana State of India: extent, determinants & financial risk protection. Indian J Med Res. 2017;146(6):759–67.
Prinja S, Kaur G, Gupta R, Rana SK, Aggarwal AK. Out-of-pocket expenditure for health care: district level estimates for Haryana state in India. Int J Health Plann Manag. 2019;34(1):277–93.
Prinja S, Bahuguna P, Duseja A, Kaur M, Chawla YK. Cost of intensive care treatment for liver disorders at tertiary care level in India. Pharmacoecon Open. 2018;2(2):179–90.
Joseph J, Sankar DH, Nambiar D. Empanelment of health care facilities under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) in India. PLoS ONE. 2021;16(5): e0251814.
Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development, and The World Bank; 2018.
Acknowledgements
We gratefully acknowledge the efforts of state data collection teams and the central data analysis team (Rajan Jaswal, Sameer Sharma, Sachin Sharma, Kriti Sharma, Jebas Arun Singh, Jaswant Singh, Aseem Sidhu and Chirag Anand) of the Department of Community Medicine & School of Public Health, Postgraduate Institute of Medical Education & Research, Chandigarh, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study is funded by the Department of Health Research (F.NO.T.11011/02/2017-HR), Ministry of Health and Family Welfare, Government of India for research.
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
Approvals from the Institutional Ethics Committee (IEC) vide letter no. PGI/IEC/2018/00125A and Institutional Collaborative Committee (ICC) vide letter no. 79/30-Edu-13/111273 of Postgraduate Institute of Medical Education & Research, Chandigarh, India were obtained.
Informed consent
Informed consent was obtained from all the individual participants in the study including consent to publish study findings.
Author contributions
Conception and design: MPS, SP, KR, OS. Acquisition of data: SK, SS, VS, PP, ACP, RJ, AH, RM, DM, SBB, AP, KLG, JPP, DKS, KM, PM, KN, AC, GDV, ASB, RB, AS, SK. Analysis and interpretation of data: MPS, SP. Drafting of the manuscript: MPS, SP. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: MPS, SP. Obtaining funding: SP. Administrative, technical, or material support: MPS, SP, KR, PG, VA, OS, JN, AA, AN, BB. Supervision: MPS, SP, KR, PG, VA, OS, JN, AN, BB.
Data availability
The unit cost data generated and analysed during phase II of the CHSI study is provided with the manuscript as tables in the main text and ESM.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Singh, M.P., Prinja, S., Rajsekar, K. et al. Cost of Surgical Care at Public Sector District Hospitals in India: Implications for Universal Health Coverage and Publicly Financed Health Insurance Schemes. PharmacoEconomics Open 6, 745–756 (2022). https://doi.org/10.1007/s41669-022-00342-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-022-00342-6