Abstract
Background
Health anxiety is a prevalent and debilitating disorder associated with extensive use of healthcare services and reduced quality of life (QoL). Regional variability in specialised clinics or specialist healthcare providers limits access to evidence-based treatment, which may be overcome by internet-delivered Acceptance and Commitment Therapy (iACT).
Objective
This study investigated the cost effectiveness of iACT for severe health anxiety in adults.
Methods
Based on a Danish randomised controlled trial (March 2016–March 2017), the economic evaluation compared costs and effects between iACT and an active control condition (iFORUM). Effectiveness was measured using self-report questionnaires. The cost analysis applied a societal perspective. Resource use and healthcare costs were extracted from the Danish National Registries. Linear regression analysis was applied using change in costs/effectiveness outcomes as the dependant variable. Time, group, and interaction between time and group were independent variables. The primary outcome was the proportion of clinically significant improvements, defined as a ≥ 25% reduction in two measures of health anxiety. The probability of cost effectiveness was presented in a cost-effectiveness acceptability curve for a range of threshold values for willingness to pay.
Results
No significant differences were detected in healthcare costs between groups; however, the iACT group significantly improved in all effectiveness outcomes. The economic analysis showed that, from the healthcare perspective, iACT was associated with an incremental cost-effectiveness ratio of €33 per additional case of clinically significant improvement compared with iFORUM and that, from the societal perspective, iACT dominated iFORUM because it was more effective and less expensive.
Conclusions
We found no statistically significant differences in costs between groups; however, iACT for severe health anxiety may be cost effective, as evidenced by significant differences in effect.
Trial Registry Number
Clinicaltrials.gov, no. NCT02735434.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study found that internet-delivered Acceptance and Commitment Therapy (iACT) for severe health anxiety may be cost effective. |
iACT is easily accessible and scalable, allowing for evidence-based treatment for many patients. |
Provision of internet-delivered treatment can help overcome barriers such as geographical distance and interference with patients' daily activities as the access to treatment is flexible. |
1 Introduction
Severe health anxiety, or hypochondriasis, is a prevalent and debilitating disorder associated with extensive use of healthcare services [1, 2], occupational disability, and reduced quality of life (QoL) [3, 4]. It is characterised by excessive ruminations about health and fear of suffering from a serious illness [5] and is often seen in patients seeking medical services [6]. Health anxiety affects 1–5% of the adult population [7, 8] and tends to persist if left untreated [1, 9], making it a costly disorder, not only for patients but also for healthcare providers and society as a whole.
There are several specialised treatments for health anxiety [10]. Systematic reviews and meta-analyses have established the effectiveness of different psychological interventions [6, 11,12,13,14,15,16,17], with cognitive behavioural therapy (CBT) being the oldest and therefore most widely investigated. Acceptance and Commitment Therapy (ACT), a new acceptance-based CBT approach [18, 19], has also demonstrated promising results for the treatment of health anxiety [14, 20, 21]. Although similarities exist between ACT and CBT, the therapeutic aim and techniques differ. Where CBT aims to change maladaptive thoughts about illness, ACT assumes that thoughts or inner states are not directly under our control. Instead, ACT focuses on changing maladaptive behaviour patterns such as control and avoidance, which are often triggered by unpleasant inner experiences such as illness-related thoughts, feelings, or bodily sensations. Therefore, ACT aims to increase the acceptance of inner experiences since futile attempts to change thought patterns can create an inner battle and interfere with living a healthy life in the long run. Despite the different effective treatments, there is a general problem of geographic or financial constraints, and regional variability in specialised clinics or specialist healthcare providers restrict patients’ access to appropriate and effective psychological treatment.
Using the internet to deliver psychotherapy can greatly increase the accessibility of evidence-based treatments [22]. This approach has several advantages, including being independent of geographic distance to a clinic, fewer or no scheduled appointments, less interference with patients’ daily life, and possibly less perceived stigma [23]. Results from a recent randomised controlled trial (RCT) [24] and a systematic review and meta-analysis suggested that the effectiveness of internet-delivered CBT (iCBT) for health anxiety is comparable to that of face-to-face CBT [10, 24].
Economic evaluations are useful because they provide a means of comparing the costs of and consequences for patient outcomes of different treatment approaches, which is important for evidence-based policy and decision making [25]. A few studies have investigated the cost-effectiveness and efficacy outcomes of CBT delivered in different formats (face-to-face, remote using telephone or videoconferencing, internet delivered with or without clinical guidance) for the treatment of health anxiety [16, 26,27,28,29,30]. Using the Health Anxiety Inventory (HAI) as the outcome measure, CBT was found to be cost effective regardless of the form of delivery. In contrast, cost-utility analyses using quality-adjusted life-years (QALYs) as the primary outcome measure were less conclusive, with CBT showing limited benefit for health-related QoL [26,27,28,29]. Previous cost-effectiveness studies have so far only investigated CBT treatments, and the studies were performed either in the UK or in Sweden. There is a need to replicate findings in other countries but more importantly to evaluate the cost effectiveness of other treatment models such as ACT. When it comes to psychological treatment models, there is no ‘one size fits all’, and previous studies found that only 30–50% of patients with health anxiety recover with CBT [9]. Hence, there is a continued need to investigate what treatments work for whom to increase the overall effectiveness of psychological interventions.
A recent RCT conducted in Denmark investigated the efficacy of internet-delivered ACT (iACT) for the treatment of severe health anxiety [21]. The study found that 12 weeks of clinician-guided iACT significantly reduced health anxiety as measured by the Whiteley Index-7 (WI-7) compared with the active control condition in which patients received an internet-delivered discussion forum (iFORUM). The between-group difference resulted in a large effect size at 6-month follow-up, measured by Cohen’s d (d = 0.80, 95% confidence interval [CI] 0.38–1.23). So far, there is no standardised, nationally available treatment for health anxiety in Denmark, and an internet-delivered treatment could permit broad access for many patients. Knowledge about the cost effectiveness of iACT is lacking but will be important for policy makers. The aim of the present study was to prospectively analyse the cost effectiveness of iACT for patients with severe health anxiety as a potential first-line treatment in a Danish healthcare setting.
2 Methods
2.1 Study Population
Patients were recruited through self-referral to the Research Clinic for Functional Disorders and Psychosomatics at Aarhus University Hospital in Denmark. Eligible patients had severe health anxiety determined by established diagnostic criteria [7] and a self-reported WI-7 score > 21.4 (scale range 0–100), which has been validated as a clinically relevant cut-off score [8]. Exclusion criteria included former treatment for health anxiety at the clinic and current psychological treatment for health anxiety elsewhere. The full eligibility criteria and study procedure are described elsewhere [21].
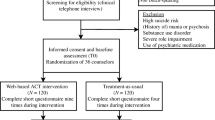
Between 18 March 2016 and 29 March 2017, a total of 151 adult patients self-referred and 132 (87%) were screened for eligibility using video-diagnostic assessment. In total, 101 patients were randomly assigned in a 1:1 computer-generated allocation process, with no restrictions or matching, to receive either iACT (n = 53) or iFORUM (n = 48). Characteristics of included patients are shown in Table 1.
2.2 Interventions
iACT was delivered as a clinician-guided self-help programme based on a modified version of an existing empirically supported manual for group-based ACT for health anxiety [14, 31]. The treatment programme consisted of seven online modules comprising written psychoeducation, videos, audio exercises (e.g., mindfulness), and homework assignments. The modules were consecutively opened to the participants over the 12 weeks of treatment. Four psychologists and one psychology student provided written guidance through an embedded message system. The written guidance was asynchronous and could be initiated by both the patient and the clinician. The aim was to motivate the patient, answer questions, and help tailor the generic homework assignments to the individual patient. The treatment platform was designed as a web-based application accessible through mobile devices and tablets.
There was no standardised treatment for health anxiety, and usual treatment may vary considerably from patient to patient, being dependant on the general practitioners' knowledge about the condition, local non-specialised services, and individual patient preferences. Hence, the intervention was compared with an active control programme, iFORUM, which was an add-on to usual treatment and consisted of an online discussion forum with seven modules that were consecutively opened over 12 weeks. The modules included different topics for discussion related to health anxiety (e.g., coping strategies, healthcare use, and impact on family or work) and were monitored for ethical reasons but were otherwise free of clinician interference. Thus, the iFORUM controlled for the effects of sharing one’s distress and having contact with others and the healthcare system. At the 6-month follow-up (6-MFU), patients from iFORUM were offered iACT. Detailed information on the trial and the components of iACT and iFORUM were previously published and are available in the electronic supplementary material (ESM)-1 [31].
2.3 Study Design
This economic evaluation was a secondary analysis of the RCT of iACT for health anxiety [21]. Data from patient-completed questionnaires administered during the study period—i.e., at baseline prior to clinical assessment, randomisation, 4 and 8 weeks into treatment, post-treatment, and 6-MFU (which was 10 months after baseline)—were analysed.
The economic evaluation applied a societal perspective incorporating intervention costs, follow-up healthcare costs (primary and secondary care), and broader societal costs related to the loss of productivity due to sick leave. To investigate the potential effect on resource use and costs after treatment completion, resource use and cost data were included for two time periods: 6 months before baseline to baseline (period 1), and from baseline to the last follow-up (i.e., 6-MFU). The time horizon for the economic evaluation was 6 months, reflecting the period over which incremental differences in resource use, costs, and outcomes were analysed. The study outline is presented in Fig 1.
2.4 Data Collection
2.4.1 Measure of Clinical Effectiveness
A detailed overview of the data points is available in ESM-2. Health anxiety symptoms were measured with the WI-7, a seven-item self-report questionnaire, on a five-point rating scale from 1 to 5 (aggregate scale range 7–35) [1]. The WI-7 is a frequently used outcome measure that has shown good sensitivity and specificity in screening for health anxiety [32]. The Short Health Anxiety inventory (SHAI) was used as a secondary measure of health anxiety to enable a more detailed analysis of clinically significant improvement. The SHAI is composed of 18 items on a categorical four-point scale from 1 to 4 (scale range 18–72) [33] and has shown high reliability, criterion validity, and sensitivity to treatment [34]. Mental well-being was measured with the five-item World Health Organization Well-being Index (WHO-5) [35] on a six-point scale ranging from 0 to 5 (scale range 0–25). All scales were transformed to a score between 0 and 100 using the equation ([score−min]/[max−min]) × 100. This was done to facilitate comparison of the effectiveness measures with previous studies, including the main efficacy study [14, 21].
The primary outcome for the analysis was clinically significant improvements calculated as the proportion of patients with a double improvement of ≥ 25% over baseline scores on two measures of health anxiety, i.e., the WI-7 and the SHAI, which has been proposed as a reliable measure of a clinically significant improvement [12].
2.4.2 Costs
2.4.2.1 Intervention Costs
A micro-costing approach was used to determine the cost of the treatment programme (iACT), which was calculated as time spent for a psychologist to develop each programme multiplied by the salary. The cost of consultations was calculated based on mean consultation time logged during the 12 weeks of treatment. Consultations consisted of the time spent reading patients' homework assignments and messages to the therapist as well as writing messages with clinical guidance to the patient. The valuation of consultation time was based on the average gross salary of psychologists involved in the programme. Running costs such as service fees (SMS), hosting, domain fee, hardware, and technical service were obtained from the local financial systems, and the total running costs were divided by the estimated total number of users of the internet platform to assign a cost per user.
2.4.2.2 Primary Healthcare Costs
Resource use in primary healthcare was obtained individually for each participant from the Danish National Health Service Register and included the number of visits and related activity-based tariffs [36]. The use of primary care services was categorised by healthcare providers (general practitioners, medical specialists, psychologists, therapists, and others).
2.4.2.3 Secondary Healthcare Costs
Information on the use of both somatic and psychiatric secondary healthcare resources was extracted from the Danish National Patient Registry [37] and valued using tariffs of diagnostic-related groupings for inpatient admissions and the Danish Ambulatory Grouping System for outpatient admissions.
2.4.2.4 Costs Due to Loss of Productivity
The National Labor Market Authority database (DREAM) [38], which contains information on all social benefits, was searched for events with employer reimbursement due to sickness absence. Productivity loss was calculated using the human capital approach based on weeks of absence from work for participants who were not retired at baseline and was valued using national age- and sex-matched gross wages [39].
All cost estimates were inflated to €, year 2018 values, using Statistics Denmark's consumer price index and a currency conversion rate of €1 = 7.45 Danish kroner. As the study time horizon was less than 1 year, costs were not discounted.
2.5 Evaluation
2.5.1 Effectiveness
To examine the incremental effectiveness of iACT, we used a linear regression model with a two-group two-period difference-in-difference (DID) approach. The DID approach relies on the assumption that confounders varying across the groups are time invariant and time-varying confounders are group invariant (the parallel trend assumption) [40]. The WI-7 and the SHAI scores informed the regression model, where the change in outcome from baseline to 6-MFU was the dependent variable, and time, group, and the interaction between time and group were the independent variables. Estimates for the change in score and 95% CI for the interaction term (the DID estimate) were considered as the primary result for the treatment effect under the parallel trend assumption.
The relative difference in number of clinically significant improvements between groups was estimated as a risk ratio. The analysis of clinically significant improvement explored the effectiveness using (1) complete cases, (2) missing follow-up data assigned the baseline value, and (3) missing values at 6-MFU being imputed using last observation carried forward (LOCF). There were no missing baseline values.
2.5.2 Costs
Mean resource use and costs during the 6-month pre-baseline and follow-up periods were calculated for each patient. Resource use, costs, and outcomes were tested for normality and distribution. Because the data were skewed, we followed International Society for Pharmacoeconomics and Outcomes Research (ISPOR) guidelines by statistically comparing group cost means using bootstrapping procedures [41, 42]. We applied nonparametric bootstrapping with 5000 replications. Further, and in accordance with ISPOR guidelines, the statistical comparison of mean group cost differences was assessed using the DID approach, as for outcomes, considering the interaction between group and time (the DID estimate) as the primary result for change in costs. The characteristics of the included patients showed baseline differences in age between groups. To assess the potential impact of this difference on results, the analyses were additionally performed adjusting for age.
To test the robustness of the cost analysis, we performed a one-way sensitivity analysis with different assumptions of the intervention costs. In the base case, the full programme development cost was distributed over the study participants, and running costs per user were calculated based on 2000 users of the internet platform. In the sensitivity analysis, we estimated the intervention cost assuming a 10-year depreciation time and the running costs per user assuming a total of 10,000 users of the platform. Estimates of different numbers of users were informed by IT specialists, and the estimated lifetime of the treatment programme was informed by clinical experts.
2.5.3 Cost Effectiveness
The cost-effectiveness analysis was expressed as the incremental cost-effectiveness ratio (ICER), which was informed by the observed scores and registry data from the trial. The statistical uncertainty was assessed using nonparametric bootstrapping, and the ICERs for each iteration of the simulation were plotted in a scatterplot. We assumed that the costs and effects were independent, which was confirmed by tests for potential correlation between costs and effects in each arm of the study. In addition, we estimated net monetary benefit (NMB) using a range of hypothetical threshold values for decision makers’ willingness to pay for a clinically significant improvement (from €0 to 10,000). The probability that the treatment was cost effective for the range of willingness to pay for a clinically significant improvement was visually presented in a cost-effectiveness acceptability curve (CEAC) [43,44,45].
To assess the robustness of the study results, all analyses were performed using (1) complete cases, (2) missing follow-up data assigned the baseline value, and (3) imputation-based cases (LOCF) for the clinically significant improvement. The NMB was calculated both from a societal perspective and from a healthcare sector perspective to illustrate the influence of the costing perspective on results. One-way sensitivity analyses were performed using the estimated variation in the intervention costs.
Data were analysed at the secure research platform provided by The Danish Health Data Authority using STATA 15 (StataCorp; College Station, TX, USA) applying a statistical significance level of 0.05.
3 Results
Overall, patients in both the iACT and the iFORUM groups actively used the internet-delivered programmes. Additional details on the use of services can be found in ESM-3.
3.1 Effectiveness
The iACT group showed marked improvements in all included effectiveness outcomes compared with the iFORUM control group at 6-MFU (Table 2). Twice as many patients receiving iACT as receiving iFORUM showed a clinically significant improvement, defined as a ≥ 25% reduction in health anxiety symptoms scored using the WI-7 and the SHAI (risk ratio 2.09; 95% CI 1.3–3.3; p = 0.002).
3.2 Costs
Intervention costs are presented in ESM-4. Table 3 presents a summary of the base-case and sensitivity estimates of the intervention costs.
Healthcare resource use in primary and secondary sectors and number of sick leave weeks are shown in Table 4, and related costs including intervention costs are presented in Table 5. The use and costs of psychologists were significantly lower with iACT than with iFORUM. Interestingly, the iACT group showed a decrease in weeks of sick leave, whereas the iFORUM group showed an increase, but this change was not statistically significant. The use and costs of other healthcare services in primary and secondary sectors and sick leave did not differ significantly between groups. The age-adjusted analyses did not alter the results (see ESM-5).
3.3 Cost Effectiveness
As complete cases showed the least effectiveness, and imputation-based cases showed the best effectiveness, the presentation of cost-effectiveness results was limited to include these two effectiveness analyses only. The results are presented in Table 6.
From the healthcare perspective, the ICER comparing iACT and iFORUM was €33 per additional case of clinically significant improvement (for the complete case analysis); from the societal perspective, iACT dominated iFORUM as it was more effective and less expensive. The sensitivity analyses reduced the cost per additional clinically significant improvement to €6 from the healthcare perspective.
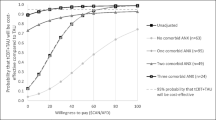
For societal costs, the results of bootstrapped replicates of differences in costs and effects were located primarily in the northeast and southeast quadrants of the scatter plot, which implies uncertainty about the cost effectiveness of the iACT programme as being either dominant (more effective and less costly) or more effective and costly than iFORUM. For healthcare costs, the data were more concentrated in the northeast quadrant than for societal costs, indicating that iACT was more effective and costly than iFORUM from a healthcare sector perspective (Fig. 2).
CEACs were generated to assess the probability of iACT being cost effective at different threshold values of willingness to pay for a clinically significant improvement in health anxiety, incorporating uncertainties associated with cost-effectiveness estimates. CEACs applying both societal and healthcare costing perspectives revealed that the probability of iACT being cost effective was close to 100% at a threshold willingness-to-pay value of €6000 for the base-case scenario using complete cases. Sensitivity analyses using the estimated sensitivity scenario for intervention costs showed a similar trend, except that the treatment was cost effective at a lower threshold value of €4000 (Fig. 3). CEACs using imputation-based cases showed that the probability of iACT being cost effective was close to 100% at a threshold willingness-to-pay value of €4000 in the base-case analysis applying the societal costing perspective and of €6000 applying the healthcare costing perspective. The sensitivity analyses showed that iACT had a probability of being cost effective at a reduced willingness-to-pay threshold compared with the base-case analyses. The CEACs using imputation-based cases are found in ESM-6.
4 Discussion
In this study, we investigated the cost effectiveness of an iACT programme compared with an active control for the treatment of patients with severe health anxiety. We found no statistically significant differences in utilisation of healthcare services or healthcare costs between groups at 6-MFU, although the iACT group showed significant improvements in all measured effectiveness outcomes. The economic evaluation showed that, from the healthcare perspective, iACT was associated with an ICER of €33 per additional case of clinically significant improvement compared with iFORUM and that, from the societal perspective, iACT dominated iFORUM as it was more effective and less expensive. From both costing perspectives, iACT had an almost 100% probability of being cost effective at a willingness-to-pay threshold of €6000 for a clinically significant improvement.
4.1 Strengths and Limitations
The main strength of this study was the randomised design with an active comparator, which minimised the influence of confounders on the results. The choice of control group could be criticised for lacking ecological validity since treatment as usual rarely consists of discussion forums. However, there is currently no defined standardised treatment for health anxiety in the Danish healthcare system, and the commonly used waitlist control condition is criticised for interrupting patients’ spontaneous remission and thus resembling a nocebo treatment, which inflates the effectiveness of the intervention [46]. Patients in the iFORUM discussion group, a format that was used in a previous study of iCBT [47] for health anxiety, did report minor improvements in health anxiety, which might largely be explained by the effect of the diagnostic interview. In terms of cost effectiveness, we expected only a minor impact from the active control on healthcare resource use. By not including the intervention costs related to iFORUM, we chose a conservative approach, where the cost-effectiveness results might, in the worst case, underestimate the true differences between iACT and treatment as usual.
Another strength was the use of validated questionnaires with high completion rates at follow-up. Resource use and costs were obtained from various national registries and included complete information with no missing data. Altogether, this contributed to the internal validity of the study. A potential limitation to consider was that the data on prescribed medication outside of hospitals were unavailable. However, it is unlikely that these data would significantly affect the results, as the use of other healthcare resources did not differ significantly between the treatment and control groups.
Productivity loss was calculated as the amount of time by which working life was reduced due to illness multiplied by salary. Data regarding the inability to work was obtained from the DREAM database (a national register) and was based on weekly information and therefore not sensitive to shorter time periods or changes in absence. This is another potential study limitation, given that health anxiety is a condition known to fluctuate [1] and therefore result in brief, recurrent rather than long-term sick leave. However, this shortcoming was equally applicable to both groups. On the other hand, the data were suitable for longitudinal analyses focusing on the duration of periods of sickness absence. Additionally, cost-effectiveness analyses were performed from a healthcare sector perspective and excluded productivity loss so that the influence of these costs on the final results could be transparently assessed.
The included intervention costs were based on different registrations but were also calculated using several assumptions, such as the number of users and lifetime of equipment. We have listed these assumptions in ESM-4 to allow assessment of their transferability to other settings. The base-case analyses were performed from a conservative perspective, with the full programme costs assigned to the study participants, whereas the sensitivity scenario used a more optimistic assignment of the intervention costs as an annual cost for an estimated maximum number of platform users, thereby limiting the risk of over- or underestimating potential cost differences.
Patients’ personal or travel time was not included in the intervention costs, which is a potential shortcoming. However, as the programme was delivered via the internet with no constraints on participants’ log-in time, we assumed that most participants accessed the programme outside of work hours. Thus, the results of our analyses may underestimate the cost difference between iACT and usual care because of potential differences in costs associated with travel and hospital appointments during the day.
We used the DID method to analyse differences in outcomes and costs between the two groups over time. This is a well-established approach that is based on the assumption of parallel trends over time between treatment and control groups. Pre-baseline measurements are required to test the validity of this assumption; the fact that these were not available is a study limitation.
The study did not include measurements of health-related QoL, which precluded a cost-utility evaluation. Health-related QoL questionnaires assess both mental and physical functioning, and—although health anxiety is regarded as a severe health condition—physical functioning may not be substantially affected in anxiety disorders [48]. This was underscored in our previous work in which our cohort showed poor mental functioning but average physical functioning at baseline [49]. This might explain the limited treatment effect of CBT for health anxiety on health-related QoL [10].
The lack of an explicit threshold value for improvement in health anxiety in the cost-effectiveness analysis makes it harder to determine whether the iACT programme should be considered good value for money. This is a general concern when applying clinical outcomes in cost-effectiveness studies, as threshold values rarely explicitly exist. Another concern is that the use of a clinical outcome measure as opposed to application of the QALY makes it impossible to compare the incremental cost effectiveness across different disease areas and thus consider the opportunity costs of adopting the intervention. In this study, iACT was found to be dominant from the societal perspective, which implies that the intervention represents good value to society. However, the scatterplots incorporating uncertainties surrounding the ICER estimates (Fig. 2) showed that a proportion of ICERs was located in the northeast quadrant of the cost-effectiveness plane, with iACT being more effective but also costlier. Following, the CEAC showed that, given no willingness to pay, the decision about adopting iACT was associated with considerable uncertainty and a 45% risk of iACT not being cost effective (Fig. 3). Increased willingness to pay would reduce the decision uncertainty; at a willingness to pay of €6000 for a clinically significant improvement, the analyses showed a 100% probability of iACT being cost effective.
4.2 Comparison with Other Studies
This was the first study to investigate the cost effectiveness of iACT for health anxiety. Only a few studies have examined the costs and cost effectiveness of iCBT programmes for health anxiety [16, 27, 30], and their control groups, follow-up periods, outcome measures, and methods for economic evaluation differed from those in our study. We found that the iACT programme was not associated with significantly lower costs compared with iFORUM, irrespective of costing perspective (societal or healthcare). We did observe a tendency for lower healthcare service utilisation, but this was similar for both groups, with the iACT group demonstrating a slightly higher relative reduction for most of the included resource categories. These results are similar to those from the previous iCBT studies [16, 26, 27, 30] that reported the same tendency but found no statistically significant differences in costs between groups at follow-up, although the included costs and follow-up periods differed from those examined here. One possible reason for the non-significant difference in costs is the relatively small sample size. This is a well-known weakness of economic evaluations performed alongside clinical studies, which are usually powered to reach statistical significance for effectiveness outcomes [50]. Recent larger clinical trials have found significant cost reductions associated with CBT interventions [28, 29].
The ICER expressed as cost per additional case of clinically significant improvement comparing the investigated alternatives was found to be €33 from the healthcare perspective. The intervention was dominant from the societal perspective. Although not directly comparable because of the different effectiveness measures, our results were in line with those of Axelsson et al. [26], who used cases in remission as an effectiveness measurement and found a slightly higher ICER for therapist-guided iCBT from the healthcare perspective, whereas the intervention, similar to our findings, was found to be dominant from the societal perspective. The findings that the internet-delivered treatment was dominant from the societal perspective underlines the potential societal benefits resulting from these types of interventions.
The cost-effectiveness plane of the 5000 bootstrap-replicated ICERs revealed uncertainties around the estimates. For the societal costing perspective, replicates were concentrated in the southeast quadrant when the iACT treatment was dominant and in the northeast quadrant when the treatment was more effective and costlier. These findings, as well as the probability of iACT being cost effective interpreted through CEACs, are supported by previous studies reporting similar results using reduction of health anxiety as the cost-effectiveness outcome [27, 28]. The difference in cost-effectiveness results according to costing perspective in our study was driven by the impact of productivity loss, which was a substantial cost relative to the other included cost categories and was reduced with iACT but increased with iFORUM at the follow-up. Overall, our results indicate that iACT for health anxiety is effective and may be cost effective depending on the willingness-to-pay threshold, which is in line with the conclusions of a review and meta-analysis of the cost effectiveness of iCBT for health anxiety [10].
4.3 Clinical Implications
There is a well-known treatment gap in mental health care [51] that is attributable to limited accessibility to and regional variability in specialised treatment. The effectiveness results presented here support the use of internet-delivered treatment (i.e., iACT) as a means of increasing treatment access regardless of geographic location. The fact that the large reduction in health anxiety symptoms was sustained at 6-MFU and that this effect is similar to that demonstrated in an earlier trial of face-to-face ACT for health anxiety [14] suggests that iACT is a valid alternative to clinic-based treatment. Furthermore, we found that iACT dominated iFORUM by being more effective and less expensive when applying the societal costing perspective and that iACT was associated with an ICER of €33 per additional case of clinically significant improvement from the healthcare perspective. In terms of economic considerations for healthcare policy, our findings support the implementation of iACT, not only as a way to reduce the net costs of treatment delivery (e.g., less travel time for patients and absence from work, and reduced rent for outpatient offices in hospitals) but also to offer a treatment option that is accessible and may appeal to a broader patient population [49], thus minimizing the treatment gap. Future research should investigate health economic outcomes with iACT in a larger cohort with a longer follow-up period, e.g., 5 years, to further validate the feasibility of incorporating this treatment approach into the existing healthcare system in Denmark. To our knowledge, no long-term cost-effectiveness studies exist. As health anxiety symptoms are found to persist if left untreated [1], and symptom reduction is found to be stable at 6-MFU, it is possible that symptom improvement and even small changes in illness behaviour and use of healthcare services would potentially have a significant impact in the long run.
5 Conclusion
We found no statistically significant differences in healthcare utilisation or costs between groups; however, iACT for health anxiety may be a cost-effective treatment as evidenced by the observed differences in effect. Despite the limitations of this study, the results are important because they provide the first economic evaluation of iACT as a treatment option that can not only benefit but is broadly accessible to patients with health anxiety.
References
Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PLoS ONE. 2010;5(3): e9873.
Barsky AJ, Ettner SL, Horsky J, Bates DW. Resource utilization of patients with hypochondriacal health anxiety and somatization. Med Care. 2001;39(7):705–15.
Creed F, Barsky A. A systematic review of the epidemiology of somatisation disorder and hypochondriasis. J Psychosom Res. 2004;56(4):391–408.
Mykletun A, Heradstveit O, Eriksen K, Glozier N, Øverland S, Mæland JG, et al. Health anxiety and disability pension award: the HUSK study. Psychosom Med. 2009;71(3):353–60.
Salkovskis PM, Warwick HM. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behav Res Ther. 1986;24(5):597–602.
Weck F, Richtberg S, Neng JMB. Epidemiology of hypochondriasis and health anxiety: comparison of different diagnostic criteria. Curr Psychiatry Rev. 2014;10(1):14–23.
Fink P, Ørnbøl E, Toft T, Sparle KC, Frostholm L, Olesen F. A new, empirically established hypochondriasis diagnosis. Am J Psychiatry. 2004;161(9):1680–91.
Sunderland M, Newby JM, Andrews G. Health anxiety in Australia: prevalence, comorbidity, disability and service use. Br J Psychiatry. 2013;202(1):56.
Hartman TCO, Borghuis MS, Lucassen PLBJ, van de Laar FA, Speckens AE, van Weel C. Medically unexplained symptoms, somatisation disorder and hypochondriasis: course and prognosis. A systematic review. J Psychosom Res. 2009;66(5):363–77.
Axelsson E, Hedman-Lagerlof E. Cognitive behavior therapy for health anxiety: systematic review and meta-analysis of clinical efficacy and health economic outcomes. Expert Rev Pharmacoecon Outcomes Res. 2019;19(6):663–76.
Thomson AB, Page LA. Psychotherapies for hypochondriasis. Cochrane Database Syst Rev. 2007;17(4): Cd006520.
Fallon BA, Ahern DK, Pavlicova M, Slavov I, Skritskya N, Barsky AJ. A randomized controlled trial of medication and cognitive-behavioral therapy for hypochondriasis. Am J Psychiatry. 2017;174(8):756–64.
Hedman E, Axelsson E, Andersson E, Lekander M, Ljotsson B. Exposure-based cognitive-behavioural therapy via the internet and as bibliotherapy for somatic symptom disorder and illness anxiety disorder: randomised controlled trial. Br J Psychiatry. 2016;209(5):407–13.
Eilenberg T, Fink P, Jensen JS, Rief W, Frostholm L. Acceptance and commitment group therapy (ACT-G) for health anxiety: a randomized controlled trial. Psychol Med. 2016;46(1):103–15.
McManus F, Surawy C, Muse K, Vazquez-Montes M, Williams JMG. A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis). J Consult Clin Psychol. 2012;80(5):817–28.
Tyrer P, Cooper S, Salkovskis P, Tyrer H, Crawford M, Byford S, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial. Lancet. 2014;383(9913):219–25.
Tyrer P, Cooper S, Tyrer H, Salkovskis P, Crawford M, Green J, et al. CHAMP: cognitive behaviour therapy for health anxiety in medical patients, a randomised controlled trial. BMC Psychiatry. 2011;14(11):99.
Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioural and cognitive therapies. Behav Ther. 2004;35(4):639–65.
Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies—republished article. Behav Ther. 2016;47(6):869–85.
Eilenberg T, Hoffmann D, Jensen JS, Frostholm L. Intervening variables in group-based acceptance and commitment therapy for severe health anxiety. Behav Res Ther. 2017;92:24–31.
Hoffmann D, Rask CU, Hedman-Lagerlof E, Jensen JS, Frostholm L. Efficacy of internet-delivered acceptance and commitment therapy for severe health anxiety: results from a randomized, controlled trial. Psychol Med. 2020;14:1–11.
Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, et al. The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry. 2018;5(3):237–86.
Andersson G, Titov N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11.
Axelsson E, Andersson E, Ljotsson B, Bjorkander D, Hedman-Lagerlof M, Hedman-Lagerlof E. Effect of internet vs face-to-face cognitive behavior therapy for health anxiety: a randomized noninferiority clinical trial. JAMA Psychiat. 2020;77:915–24.
Rabarison KM, Bish CL, Massoudi MS, Giles WH. Economic evaluation enhances public health decision making. Front Public Health. 2015;3:164.
Axelsson E, Andersson E, Ljotsson B, Hedman-Lagerlof E. Cost-effectiveness and long-term follow-up of three forms of minimal-contact cognitive behaviour therapy for severe health anxiety: results from a randomised controlled trial. Behav Res Ther. 2018;107:95–105.
Hedman E, Andersson E, Lindefors N, Andersson G, Ruck C, Ljotsson B. Cost-effectiveness and long-term effectiveness of internet-based cognitive behaviour therapy for severe health anxiety. Psychol Med. 2013;43(2):363–74.
Hedman E, Andersson E, Ljotsson B, Axelsson E, Lekander M. Cost effectiveness of internet-based cognitive behaviour therapy and behavioural stress management for severe health anxiety. BMJ Open. 2016;6(4): e009327.
Morriss R, Patel S, Malins S, Guo B, Higton F, James M, et al. Clinical and economic outcomes of remotely delivered cognitive behaviour therapy versus treatment as usual for repeat unscheduled care users with severe health anxiety: a multicentre randomised controlled trial. BMC Med. 2019;17(1):16.
Seivewright H, Green J, Salkovskis P, Barrett B, Nur U, Tyrer P. Cognitive-behavioural therapy for health anxiety in a genitourinary medicine clinic: randomised controlled trial. Br J Psychiatry. 2008;193(4):332–7.
Hoffmann D, Rask CU, Hedman-Lagerlof E, Ljotsson B, Frostholm L. Development and feasibility testing of internet-delivered acceptance and commitment therapy for severe health anxiety: pilot study. JMIR Ment Health. 2018;5(2): e28.
Fink P, Ewald H, Jensen J, Sorensen L, Engberg M, Holm M, et al. Screening for somatization and hypochondriasis in primary care and neurological in-patients: a seven-item scale for hypochondriasis and somatization. J Psychosom Res. 1999;46(3):261–73.
Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002;32(5):843–53.
Alberts NM, Hadjistavropoulos HD, Jones SL, Sharpe D. The Short Health Anxiety Inventory: a systematic review and meta-analysis. J Anxiety Disord. 2013;27(1):68–78.
Topp CW, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–76.
Andersen JS, Olivarius NDF, Krasnik A. The Danish National Health Service Register. Scand J Public Health. 2011;39(7 Suppl):34–7.
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–3.
Ministry of Employment (Danish: Styrelsen for Arbejdsmarked og Rekruttering). The National Labor Market Authrority database guide version 44 v2 (Danish: DREAM vejledning version 44 v2). 2019. https://www.dst.dk/-/media/Kontorer/13-Forskning-og-Metode/DREAM-koder----version-44---E.pdf?la=da. Accessed 01 Sept 2019.
(Statistik) SDDD. Gross and disposable income by region, gender and age range. 2015. http://www.statistikbanken.dk/statbank5a/default.asp?w=1920. Accessed 01 Nov 2019.
Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39:453–69.
Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1(1):54–75.
Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA task force report. Value Health. 2005;8(5):521–33.
Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves-facts, fallacies and frequently asked questions. Health Econ. 2004;13(5):405–15.
Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Mak. 1998;18(2 Suppl):S68–80.
Hoch JS, Rockx MA, Krahn AD. Using the net benefit regression framework to construct cost-effectiveness acceptability curves: an example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of “community acquired” syncope. BMC Health Serv Res. 2006;6:68.
Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatr Scand. 2014;130(3):181–92.
Hedman E, Andersson G, Andersson E, Ljotsson B, Ruck C, Asmundson GJ, et al. Internet-based cognitive-behavioural therapy for severe health anxiety: randomised controlled trial. Br J Psychiatry. 2011;198(3):230–6.
Axelsson E, Lindsater E, Ljotsson B, Andersson E, Hedman-Lagerlof E. The 12-item Self-Report World Health Organization Disability Assessment Schedule (WHODAS) 2.0 administered via the internet to individuals with anxiety and stress disorders: a psychometric investigation based on data from two clinical trials. JMIR Ment Health. 2017;4(4): e58.
Hoffmann D, Rask CU, Hedman-Lagerlöf E, Eilenberg T, Frostholm L. Accuracy of self-referral in health anxiety: comparison of patients self-referring to internet-delivered treatment versus patients clinician-referred to face-to-face treatment. BJPsych Open. 2019;5(5): e80.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford University Press; 2015.
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
Acknowledgements
The authors thank Nicolaj Knudsen for programming the internet-based platform and ensuring continuous registration of the use of services during the study period. We also thank Erik Hedman-Lagerlöf for professional feedback on the study design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was financially supported by the Health Foundation (ID no. 17-B-0213) and TrygFonden Foundation (ID no. 102644).
Conflicts of Interest
Bettina Wulff Risør, Ditte Hoffmann Frydendal, Marie Konge Villemoes, Camilla Palmhøj Nielsen, Charlotte Ulrikka Rask, Lisbeth Frostholm have no conflicts of interest that are directly relevant to the content of this article.
Data availability statement
The raw data from this study represent confidential information and cannot be made publicly available according to the specific data licence agreement (granted solely for the purpose of project evaluation).
Code availability
The STATA software code is available upon request.
Contributors
BWR and DHF contributed equally to this paper. These authors designed the study, performed the data analyses, and drafted the manuscript. MKV, CPN, CUR, and LF contributed to study conception and design and critically commented on the data analyses and the manuscript. All authors approved the final manuscript.
Ethics approval
The study was approved by the Ethics Committee of the Central Region Denmark in January 2016 (ID no. 1-10-72-321-15) and the Danish Data Protection Agency in February 2016 (ID no. 1-16-02-51-16).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Informed consent was obtained from all individual participants included in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Risør, B.W., Frydendal, D.H., Villemoes, M.K. et al. Cost Effectiveness of Internet-Delivered Acceptance and Commitment Therapy for Patients with Severe Health Anxiety: A Randomised Controlled Trial. PharmacoEconomics Open 6, 179–192 (2022). https://doi.org/10.1007/s41669-021-00319-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-021-00319-x