Abstract
Objective
As a recognized therapy to improve airway clearance, high-frequency chest wall oscillation (HFCWO) is used to manage reduced vital capacity in patients with complex neuromuscular disorders (cNMD). This study aimed to investigate the budget impact of HFCWO versus chest wall physical therapy (CWPT) from a US-commercial payer perspective.
Methods
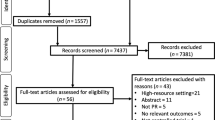
In combination with a previously developed cost-effectiveness model, a budget impact model was developed to evaluate the incremental budgetary impact associated with introducing a HFCWO device over a 5-year time horizon. The model compared the cost implications associated with the commonly used CWPT procedure, as the current scenario, with a new scenario consisting of 80% of market share for HFCWO. The resource use and costs included in the analyses were costs associated with the HFCWO device (Vest™ System) and its consumables, patient training, and medical services such as hospitalization, medications, emergency room, and outpatient visits. The primary outcome measures included total and incremental budgetary impact per member per year (PMPY).
Results
In a hypothetical plan of 1,000,000 members (men: 49.2%), 2099 patients with cNMD were estimated to be eligible to receive airway clearance services over 5 years. The new scenario (HFCWO and CWPT [US$24 PMPY]) was cost-saving compared with the current scenario (CWPT only [$34 PMPY]) with a cost reduction of US$9.46 PMPY. The model estimated a net cost-saving of US$1,594,131 and US$9,591,343 over 1 and 5 years, respectively.
Conclusion
This study suggests the HFCWO technique to manage the reduction in vital capacity in patients with cNMD would lead to favorable budget impact results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
High-frequency chest wall oscillation (HFCWO) is an efficient technology that reduces hospitalization costs by US$6845 per patient over 5 years due to decreased airway infections in patients with complex neuromuscular disorders (cNMD). |
This budget impact analysis shows HFCWO is a cost-saving strategy in managing cNMD. The reduction in hospitalization costs offset additional costs of the HFCWO device (Vest™ System). |
Prescribing HFCWO consistently for 80% of patients with cNMD could lead to cost savings of almost US$9.6 million over 5 years for a commercial healthcare payer with one million insurees in the USA. |
1 Introduction
Patients with complex neuromuscular disorders (cNMD) are at risk of reduced vital capacity due to weakness in inspiratory muscles and changes in the lungs and chest wall mechanical properties [1]. As a result, cNMD patients, including those with neuromuscular disease and cerebral palsy, have airway clearance difficulties, which may cause aspiration, respiratory infection, and death [2, 3].
High-frequency chest wall oscillation (HFCWO) is a procedure that facilitates airway clearance by providing positive and negative pressure shifts to increase the tracheal mucus movement for airway clearance [1, 4, 5]. Various available HFCWO devices are used for airway clearance in diseases such as neuromuscular disorders (NMD). Among others, the Vest™ System is used in many clinical studies focusing on the safety and efficacy of HFCWO interventions [6]. In most of these studies, HFCWO is compared with manual chest wall physiotherapy (CWPT). HFCWO has been shown to be a more efficient and cost-effective approach than CWPT for the management of reduced vital capacity in patients with cNMD [1, 7]. According to published articles, HFCWO has a significant impact in decreasing hospitalization rates and reducing length of stay [8], as well as increasing pulmonary function amongst affected pediatric patients with cNMD in two exploratory pilot studies [9, 10]. Additionally, patients typically show high adherence to therapy and satisfaction with treatment [10]. Javanbakht et al. (2019) showed that HFCWO was cost effective versus CWPT from a UK National Health Service (NHS) and personal social services (PSS) perspective [7].
Despite published evidence on clinical efficacy and value for money, the impact of HFCWO on payers’ budget has not been investigated. As mentioned earlier, HFCWO results in lower hospitalization rates and reduces inpatient costs associated with the management of NMD patients [8]. Lechtzin et al. (2016) investigated the impact of HFCWO on reducing healthcare resource use, specifically for inpatient services in the USA [8]. Despite the beneficial impact the intervention may have on healthcare service utilization, the device and consumable costs may result in increased budgetary pressure compared with existing approaches (CWPT). This study aimed to estimate the budget impact of introducing HFCWO for airway clearance in 80% of cNMD patients in the USA.
2 Method
A budget impact model was developed alongside the previously developed cost-effectiveness model in the UK by Javanbakht et al. [7]. In addition to the cost-effectiveness model adaptation to the US setting, the budget impact model was developed to adhere to the Principles of Good Practice For Budget Impact Analysis II Task Force [11]. We estimated an incremental budget impact over a 5-year timeframe from the perspective of commercial healthcare payers in the USA. Effectiveness and costs associated with HFCWO were obtained from a database analysis of two broad claims databases in the USA, including the Truven Health MarketScan databases (Truven Health Analytics, Ann Arbor, MI, USA) and Milliman’s Consolidated Health Cost Guidelines Source Database (Milliman, Seattle, WA, USA) [8].
2.1 Eligible Population
National-level population data in 2018 (men: 161,128,679, women: 166,038,755) and 2019 were obtained from the United States census bureau [12]. At the time of the study, the total population data in 2019 (328,239,523) were available until July 1, 2019. Therefore, we applied an identical population growth rate (1.003) in the second 6 months (July–December) equal to the first 6 months in 2019 (men: 162,021,313, women: 167,290,299) to estimate the population size. In the next step, the sex-specific population size between 2021 and 2025 was estimated assuming a constant sex-specific population growth rate, based on the growth rate and sex split present between 2018 and 2019 (men: 0.55%, women: 0.75%).
To estimate the prevalence rate of cNMD patients over the model time horizon, in the absence of data in the USA, we used a study by Rose et al. (2019) in which they reported trends in incidence and prevalence of NMD through emergency room (ER) presentation or hospital admission averaged over the 12-year period (Fiscal years 2003–2014) in Ontario [13]. Table 1 shows the prevalence rates of cNMDs and their annual growth rates used in this analysis.
aAverage change in prevalence per year
According to Rose et al., the prevalence rates of cNMD among children and adults were 56.0 and 74.5/100,000 population in 2014, respectively [13]. Additionally, the average changes in annual prevalence rates of the condition amongst children and adults were 0.09 and 0.07/100,000 population, respectively. Using the proportion of children (43.9%) in Lechtzin et al. [8], we estimated the average annual change in the prevalence rate (0.09/100,000) for children and adults. Subsequently, the sex-specific prevalence rate of cNMD (men: 98.61, women: 61.21/100,000 population) in 2021 was estimated using the proportion of men (61.7%) obtained from Lechtzin et al. [8]. For the subsequent years, the number of new cNMD cases was estimated by comparing the estimated population against the previous year. Finally, the eligible population to receive HFCWO was estimated according to the results of Fiorenza et al. [14]. The eligible population was equal to the proportion of those patients who require home mechanical ventilation on assessment at first presentation to a respiratory clinic (67%). This approach was chosen because of the assumption that patients requiring home mechanical ventilation due to significantly deranged respiratory function would also be eligible for at-home airway clearance therapy.
Following estimation of the eligible patient population at the national level, we ran the model for a hypothetical healthcare payer with 1,000,000 beneficiaries in the year 2021 (first year in time horizon). The proportion of men (49.2%) and beneficiaries’ annual growth for subsequent years were assumed to be identical to the national-level data. The size of the eligible population was estimated for the hypothetical healthcare payer, accordingly.
2.2 Clinical Inputs
Clinical inputs are explained in detail in Table 1 in Javanbakht et al. [7]. In summary, the budget impact model sourced clinical inputs from the UK-based cost-effectiveness model, which derived inputs from Yuan et al. [10] and Lechtzin et al. [8]. We also sourced and adjusted the cost-effectiveness model’s background mortality rates to reflect the USA’s age- and sex-specific mortality rates in 2017 [15]. Moreover, results from Blair et al. [16] were used to estimate the standardized mortality ratio (SMR) according to a disability score among patients with cerebral palsy. A weighted average of SMR for individuals with a high disability score (≥ 9) was estimated (51.03) to reflect a disease-specific mortality rate. A list of clinical inputs used in this study is presented in Table 2.
2.3 Cost Inputs
Model costs included the costs associated with the HFCWO device (the Vest™ System and its consumables), patient training, and medical services. According to Medtech innovation briefings 159, published by the National Institute for Health and Care Excellence (NICE), in a conservative approach, a lifespan of 5 years was assumed for the Vest™ System device to annualize the associated costs over the model time horizon [18]. Costs associated with garment replacement (every 18 months) and the Vest™ System device warranty costs were included in the initial device costs. For training costs, we used the mean hourly wage of registered nurses in 2019 [19]. Two 3-h home visits (including travel time for each visit) and two phone follow-up sessions (1 h for each call) were assumed for each patient who used HFCWO, while for CWPT, only one home visit and no phone follow-ups were assumed in the model.
Costs of medical services, including hospital admission and ER visits (facility and physician), were estimated according to the data obtained from Lechtzin et al. [8] for both treatment strategies. We firstly estimated ‘Number of members’ in pre-and post-intervention by dividing medical member months by duration per member. Secondly, ‘Total number of service over the period’ was estimated by multiplying total member year and service per person per year. In the next step, ‘total service costs’ were estimated by multiplying ‘number of members’, ‘duration/member’, and total service cost per member per month (PMPM). Lastly, the average service costs were estimated by dividing ‘total service costs’ by ‘total number of services over the period’. Monthly general practitioner (GP) visits and monthly medication costs were assumed to equal reported allowed PMPM costs by Lechtzin et al. [8]. Costs from Lechtzin et al. were based on data from 2007 to 2011, where all costs were inflated to the end of 2011. Therefore, in our study, costs obtained from Lechtzin et al. were inflated to 2019 using a consumer price index of 119.17 in 2019 versus 2011 (103.16) [20]. Table 3 shows the different cost components used in this study.
2.4 Analysis
Two arms consisting of five annual patient cohorts with cNMD, beginning each year until the end of the time horizon, were compared over 5 years (2021–2025). In the first patient cohort, the estimated eligible population for the year 2021 was followed until 2025. In subsequent patient cohorts, new cNMD cases in each year (2022, 2023, 2024, and 2025) were considered as new entries into the model and were followed until 2025.
We examined budget impact in the first arm, assuming 100% of patients use CWPT (current scenario), that is, HFCWO is not used. In the second arm, 80 and 20% distributions were assumed for HFCWO and CWPT, respectively (new scenario). Annual costs associated with each arm for each year and cumulative costs over the 5-year time horizon were estimated. The model estimated the new scenario’s total and incremental budget impact compared with the current scenario per member per year (PMPY).
The impact of all input parameters on incremental budget impact PMPY was examined using deterministic sensitivity analysis (DSA). All key input parameters were varied by ± 25% to determine the extent to which the change impacted the results of the analysis.
3 Results
At a national level population of 333,643,203 people (in 2021), 126,768 patients were estimated to have cNMD and to be eligible to use HFCWO. The number of eligible patients increased to 153,920 by 2025. In the analysis focusing on the hypothetical healthcare payer with 1,000,000 beneficiaries in 2021, 380 patients were estimated to be eligible. Table 4 shows the estimated total and eligible population at national- and hypothetical healthcare payer-levels in the USA between 2021 and 2025.
Over a 5-year time horizon and assuming 80% of patients are treated with HFCWO, the new scenario led to a −US$9.46 PMPY budget impact compared with the current scenario. Therefore, the new scenario could save US$9,591,343 for a hypothetical healthcare payer over the time horizon (Table 5). In 1 year, the new scenario showed a budget saving of US$1.59 PMPY, leading to a total budget impact of − US$1,594,131. The budget impact analysis results for other HFCWO likely market shares (30–100%) are shown in Appendix 1 (see electronic supplementary material). The result of the scenario analyses with the lower market shares also shows the new scenario remains cost saving compared with the current scenario.
Table 6 represents the costs breakdown by scenario over 5 years (2021–2025). In the new scenario, treatment costs were raised by about US$4.6 million, while the hospitalization costs associated with respiratory infections were reduced by US$14.4 million (US$6845 per patient) over 5 years. Moreover, the analysis results showed a 15% increase and 28% decrease in costs of medications and GP visits in the new scenario, respectively.
The results of the DSA are shown in Fig. 1. The key drivers of the model results were the hospitalization costs for HFCWO and CWPT. Moreover, the proportion of the eligible cNMD population to receive HFCWO, prevalence rates, and equipment costs were major drivers with a greater impact than the other input parameters. The results of the DSA showed that none of the ± 25% parameter variations resulted in a scenario where HFCWO would be more costly than current practice.
4 Discussion
HFCWO devices facilitate airway clearance by providing appropriate secretion movement and reduce mucous viscosity [1, 4, 5] in diseases such as cNMD. To aid evidence generation in this area, this study aimed to explore the budgetary impact associated with the introduction of HFCWO (using the Vest™ System) compared with CWPT only for the management of airway clearance in patients with cNMD, from a healthcare payer perspective in the USA.
The model results showed the HFCWO technique could lead to financial savings for healthcare payers in the USA. With an 80% distribution of patients treated, the Vest™ System could save US$9.46 PMPY over 5 years from a healthcare payer perspective. This relative superiority of HFCWO compared with CWPT in terms of cost savings can potentially lead to savings of approximately US$4569 over 5 years for each eligible patient. The higher costs associated with the device (the Vest™ System) and its consumables were offset by the considerable impact of HFCWO in reducing hospitalization costs, which has also been shown in the study by Lechtzin et al. [8]. Although the results of this study are dependent on the proportion of patients on HFCWO (80%) in the new scenario, the result of scenario analyses with lower shares of HFCWO in the new scenario led to cost-saving results compared with the current scenario (only CWPT).
This budget impact model was built according to the Principles of Good Practice For Budget Impact Analysis II Task Force [11]. One of its strengths is it uses real-world data on clinical effectiveness, with cost data obtained from Lechtzin et al. [8]. Using real-world data in this analysis can provide more reliable results for healthcare payers. Not surprisingly, our model results are consistent with the findings of Lechtzin et al. [8], which reflects the internal validity of the model. Additionally, this model was developed alongside a cost-effectiveness model, which will help for the purposes of decision making [21].
Our study has some limitations worth noting. First, we used epidemiological data from a Canadian study to estimate the prevalence and annual incidence of more severe cNMD cases, in the absence of comparable information in the USA [13]. Rose et al. estimated the population-based prevalence rate of those presenting to the ER or requiring hospital admission. However, as shown in Fig. 1, we explored the uncertainty present in these estimates during the sensitivity analysis outlined. Despite the relatively wide range of variation presented, the model results remained stable. Secondly, to the best of our knowledge, there are other available HFCWO devices on the market. No study to date has compared the efficacy and cost effectiveness of the Vest™ System with other HFCWO devices. Therefore, this study does not involve a comparison between alternative HFCWO devices, but rather focuses on the medical device technology. Future studies should investigate the potential budget impact of alternative HFCWO devices now that sufficient evidence has been presented on the clinical and economic benefits of HFCWO compared with CWPT. Moreover, other peripheral airway clearance techniques for cNMD, including intrapulmonary percussive ventilation (IPV) and chest wall strapping (CWS) [22] were not included in the cost-effectiveness model (used for this budget impact analysis). Hence, our study is solely focused on the comparison of HFCWO against CWPT, as IPV and CWS are not widely used due to their limitations, such as device expense (IPV) and diminishing pulmonary system compliance (CWS) [22]. Thirdly, we used cost data from a relatively dated study. Lechtzin et al. indicated consistency in the respiratory care of cNMD between 2007 and 2015, and due to lack of published information regarding any major change in the routine practice between 2016 and 2019, we assumed data from Lechtzin et al. are still relevant [8]. Moreover, there is a chance all airway clearance services before HFCWO were not CWPT solely and we assumed other services may not impact on overall costs and effectiveness of total airway clearance services. This assumption was made due to chest physical therapy being the gold standard of airway clearance for cNMD in the first decade of 2000 according to the Cystic Fibrosis Foundation Guidelines [23].
5 Conclusion
Airway clearance is a vital need in the management of cNMD patients. The Vest™ System uses the HFCWO method to loosen secretions in the chest by reducing their viscosity. Following previously published studies regarding the clinical and economic benefits of HFCWO compared with CWPT, our study has shown HFCWO would result in net cost savings of US$9.46 PMPY, which hypothetically translates to US$9.6 million over 5 years from a US commercial healthcare payer perspective. Further studies are necessary to compare the budget impact of alternative HFCWO devices.
References
Chatwin M, Toussaint M, Gonçalves MR, Sheers N, Mellies U, Gonzales-Bermejo J, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med. 2018;136(February):98–110. https://doi.org/10.1016/j.rmed.2018.01.012.
Emery AE. The muscular dystrophies. BMJ. 1998;317(7164):991–5.
Gozal D. Pulmonary manifestations of neuromuscular disease with special reference to Duchenne muscular dystrophy and spinal muscular atrophy. Pediatr Pulmonol. 2000;29(2):141–50.
King M, Phillips DM, Zidulka A, Chang HK. Tracheal mucus clearance in high-frequency oscillation. II: chest wall versus mouth oscillation. Am Rev Respir Dis. 1984;130(5):703–6.
Freitag L, Long WM, Kim CS, Wanner A. Removal of excessive bronchial secretions by asymmetric high-frequency oscillations. J Appl Physiol. 1989;67(2):614–9.
HFCWO clinical studies [Internet]. ClinicalTrials.gov. Available from: https://clinicaltrials.gov/ct2/results?term=HFCWO&Search=Search.
Javanbakht M, Mashayekhi A, Montazeri M, Rezai Hemami M, Branagan-Harris M. The VestTM high-frequency chest wall oscillation system compared with manual chest wall physiotherapy for managing airway clearance in patients with complex neurological disorders: a UK-based cost-effectiveness analysis. Open Pharmacoecon Heal Econ J. 2019;7(1):1–8.
Lechtzin N, Wolfe LF, Frick KD. The impact of high-frequency chest wall oscillation on healthcare use in patients with neuromuscular diseases. Ann Am Thorac Soc. 2016;13(6):904–9.
Fitzgerald K, Dugre JL, Pagala S, Marcus M, Kazachkov M. Use of aggressive lower respiratory secretion clearance in children with muscle weakness and tracheostomy: a pilot study. Chest. 2010;138(4):323A. https://doi.org/10.1378/chest.10486.
Yuan N, Kane P, Shelton K, Matel J, Becker BC, Moss RB. Safety, tolerability, and efficacy of high-frequency chest wall oscillation in pediatric patients with cerebral palsy and neuromuscular diseases: an exploratory randomized controlled trial. J Child Neurol. 2010;25(7):815–21.
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Heal J Int Soc Pharmacoecon Outcomes Res. 2014;17(1):5–14.
Population [Internet]. The US Census Bureauthe. US Census Bureau. Available from: https://www.census.gov/topics/population.html.
Rose L, McKim D, Leasa D, Nonoyama M, Tandon A, Bai YQ, et al. Trends in incidence, prevalence, and mortality of neuromuscular disease in Ontario, Canada: a population-based retrospective cohort study (2003–2014). PLoS ONE. 2019;14(3):1–12.
Fiorenza D, Vitacca M, Bianchi L, Gabbrielli L, Ambrosino N. Lung function and disability in neuromuscular patients at first admission to a respiratory clinic. Respir Med. 2011;105(1):151–8.
Life Table, 2017 [Internet]. Social security. Available from: https://www.ssa.gov/oact/STATS/table4c6.html.
Blair E, Langdon K, McIntyre S, Lawrence D, Watson L. Survival and mortality in cerebral palsy: observations to the sixth decade from a data linkage study of a total population register and National Death Index. BMC Neurol. 2019;19(1):1–11.
Myles PR, Hubbard RB, Gibson JE, Pogson Z, Smith CJP, McKeever TM. Pneumonia mortality in a UK general practice population cohort. Eur J Public Health. 2009;19(5):521–6. https://doi.org/10.1093/eurpub/ckp081.
The Vest for delivering highfrequency chest wall oscillation in people with complex neurological needs [Internet]. NICE—Medtech innovation briefing 159. 2018. p. 3. Available from: https://www.nice.org.uk/advice/mib159/resources/the-vest-for-delivering-highfrequency-chest-wall-oscillation-in-people-with-complex-neurological-needs-pdf-2285963525028805.
Occupational Employment and Wages, May 2019 [Internet]. US Bureau of Labor Statistics. 2019. Available from: https://www.bls.gov/oes/current/oes291141.htm.
Consumer Price Index—United States [Internet]. The World Bank. 2020. Available from: https://data.worldbank.org/indicator/FP.CPI.TOTL?locations=US.
Yagudina RI, Kulikov AU, Serpik VG, Ugrekhelidze DT. Concept of combining cost-effectiveness analysis and budget impact analysis in health care decision-making. Value Health Reg Issues. 2017;13:61–6.
Chatwin M, Toussaint M, Gonçalves MR, Sheers N, Mellies U, Gonzales-Bermejo J, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med. 2018;136(January):98–110. https://doi.org/10.1016/j.rmed.2018.01.012.
Cystic Fibrosis Foundation guidelines for patient services, evaluation, and monitoring in cystic fibrosis centers. The Cystic Fibrosis Foundation Center Committee and Guidelines Subcommittee. Am J Dis Child. 1990;144(12):1311–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Hillrom, USA. The funder had no influence on the design, interpretation of data, and the decision to submit the article for publication.
Conflict of interest
A. Ansaripour, A. Mashayekhi, and M. Javanbakht are employed by OPTiMAX Access or/and Device Access, which has received research grants from Hillrom. K. Roehrich, M. Wanjala, S. Noel, and A. Murray are employed by Hillrom, which has funded this study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
AA designed the study, programmed the model, performed statistical analyses, conducted the data collection, interpreted results, and provided a draft of the manuscript. AM and MRH designed the study and conducted data collection. MJ designed the study, interpreted the results, and critically reviewed the manuscript, while KR, MW, SN, and AM critically reviewed the manuscript. All authors reviewed the manuscript and approved the final version of the manuscript.
Availability of data and material
The model used in this study was provided to the journal’s peer reviewers for their reference when reviewing the manuscript. The information reported in this manuscript is sufficient to replicate the results of the study.
Appendix 1 The budget impact of HFCWO for various market shares in the new scenario
Appendix 1 The budget impact of HFCWO for various market shares in the new scenario
% CWPT | % HFCWO | Results | 2021 | 2022 | 2023 | 2024 | 2025 | Total |
|---|---|---|---|---|---|---|---|---|
70% | 30% | Total incremental costs | − $597,799 | − $742,626 | − $746,920 | − $751,865 | − $757,543 | − $3,596,754 |
Total incremental costs (PMPY) | − $0.60 | − $0.74 | − $0.74 | − $0.74 | − $0.74 | − $3.55 | ||
60% | 40% | Total incremental costs | − $797,065 | − $990,168 | − $995,893 | − $1,002,487 | − $1,010,058 | − $4,795,672 |
Total incremental costs (PMPY) | − $0.80 | − $0.98 | − $0.98 | − $0.98 | − $0.98 | − $4.73 | ||
50% | 50% | Total incremental costs | − $996,332 | − $1,237,710 | − $1,244,866 | − $1,253,109 | − $1,262,572 | − $5,994,590 |
Total incremental costs (PMPY) | − $1.00 | − $1.23 | − $1.23 | − $1.23 | − $1.23 | − $5.91 | ||
40% | 60% | Total incremental costs | − $1,195,598 | − $1,485,252 | − $1,493,840 | − $1,503,731 | − $1,515,087 | − $7,193,507 |
Total incremental costs (PMPY) | − $1.20 | − $1.48 | − $1.47 | − $1.47 | − $1.48 | − $7.10 | ||
30% | 70% | Total incremental costs | − $1,394,865 | − $1,732,794 | − $1,742,813 | − $1,754,352 | − $1,767,601 | − $8,392,425 |
Total incremental costs (PMPY) | − $1.39 | − $1.72 | − $1.72 | − $1.72 | − $1.72 | − $8.28 | ||
20% | 80% | Total incremental costs | − $1,594,131 | − $1,980,336 | − $1,991,786 | − $2,004,974 | − $2,020,116 | − $9,591,343 |
Total incremental costs (PMPY) | − $1.59 | − $1.97 | − $1.97 | − $1.97 | − $1.97 | − $9.46 | ||
10% | 90% | Total incremental costs | − $1,793,397 | − $2,227,878 | − $2,240,760 | − $2,255,596 | − $2,272,630 | − $10,790,261 |
Total incremental costs (PMPY) | − $1.79 | − $2.21 | − $2.21 | − $2.21 | − $2.21 | − $10.64 | ||
0% | 100% | Total incremental costs | − $1,992,664 | − $2,475,420 | − $2,489,733 | − $2,506,218 | − $2,525,145 | − $11,989,179 |
Total incremental costs (PMPY) | − $1.99 | − $2.46 | − $2.46 | − $2.46 | − $2.46 | − $11.83 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ansaripour, A., Roehrich, K., Mashayekhi, A. et al. Budget Impact of the Vest™ High Frequency Chest Wall Oscillation System for Managing Airway Clearance in Patients with Complex Neurological Disorders: A US Healthcare Payers’ Perspective Analysis. PharmacoEconomics Open 6, 169–178 (2022). https://doi.org/10.1007/s41669-021-00299-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-021-00299-y