Abstract
Objective
We calculated the short- and long-term care resource use and costs in adults with high-risk conditions for cardiovascular disease (HRCVD) as defined by the Canadian Cardiovascular Society dyslipidemia guidelines.
Methods
We linked Alberta health databases to identify patients aged ≥ 18 years with HRCVD between fiscal year (FY) 2012 and FY2016. The first HRCVD event was the index event. Patients were categorized into (1) primary prevention patients and (2) secondary prevention patients at the index event and were followed until death, they moved out of the province, or they were censored at March 2018. We calculated the resource use and costs for each of the 5 years after the index event.
Results
The study included 459,739 HRCVD patients (13,947 [3%] were secondary prevention patients). The secondary prevention patients were older (median age 61 years vs. 55 years; p < 0.001), and there were fewer females in this group (30.4% vs. 51.3%; p < 0.001). The total healthcare costs in the first year decreased over time (FY2012: 1.16 billion Canadian dollars (CA$); FY2016: CA$1.05 billion; p < 0.001). An HRCVD patient incurred CA$12,068, CA$5626, and CA$4655 during the first, second, and fifth year, respectively (p for trend < 0.001). During the first year, healthcare costs per secondary prevention patient (CA$36,641) were triple that for a primary prevention patient (CA$11,299; p < 0.001), primarily due to higher hospitalization costs in secondary prevention patients (CA$26,896 vs. CA$6051; p < 0.001).
Conclusions
The healthcare costs for HRCVD patients were substantial but decreased over time. The costs were highest in the year following the index event and decreased thereafter. Secondary prevention patients incurred higher costs than the primary prevention patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Healthcare resource use and cost burden associated with high-risk conditions for cardiovascular disease are high, but decreased during the study period. |
Resource use and costs are highest during the first year after the diagnosis. |
Secondary prevention patients use more resources and incur higher costs than primary prevention patients. |
1 Introduction
Cardiovascular disease (CVD) is a public health issue in many countries. Heidenreich et al. estimated that approximately 40% of the United States (US) population would have CVD in 2030, which would result in a triple increase in the total costs of CVD from US$445 billion to US$1094 billion between 2010 and 2030 in the USA [1]. Similarly, CVD could cost Europeans €170 billion each year [2]. In Canada, it is estimated that CVD costs about 22 billion Canadian dollars (CA$) a year and is considered the second leading contributor to the national healthcare costs [3].
Dyslipidemia is an important risk factor for CVD. Patients with an elevated level of low-density lipoprotein cholesterol (LDL-C) have a higher risk for cardiac death [4]. Several clinical guidelines have recommended a lipid-lowering drug (LLD), for example, a statin, to lower the risk of atherosclerotic CVD in patients with high-risk conditions for CVD (HRCVD) [5, 6]. In the 2016 Canadian Cardiovascular Society (CCS) Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult, there are five groups of patients who are acknowledged as having HRCVD and are recommended to start statin treatment to prevent CVD events. They include patients who have LDL-C levels ≥ 5 mmol/L, clinical atherosclerosis, abdominal aortic aneurysm, diabetes mellitus, and chronic kidney disease [6, 7].
We have previously reported that patients with HRCVD who optimally controlled dyslipidemia had a lower mortality, but incurred higher healthcare costs, than those who did not. However, secondary prevention patients with optimal control of dyslipidemia had a lower mortality without additional healthcare costs [8]. Currently, little is known about the overall health service utilization and cost burden in patients with HRCVD who are recommended to start a statin to control dyslipidemia to prevent CVD events and mortality in short- and long-term care. Accordingly, we assessed the resource use and healthcare cost burden in this HRCVD patient population in Alberta, Canada, to address this knowledge gap and to provide data for decision making in cardiovascular care.
2 Methods
2.1 Data Source and Study Population
We used a cohort of 459,739 patients with HRCVD in the province of Alberta which has been described previously [8]. In brief, we linked seven administrative health databases in Alberta (National Ambulatory Care Reporting System, Discharge Abstract Database, Practitioner Claims, Pharmaceutical Information Network, Laboratory, Population Registry, and Vital Statistics [9]) to include patients who were 18 years or older and had HRCVD between April 2012 and March 2017 (fiscal years [FY] 2012–2016). Consistent with the CCS dyslipidemia guidelines, a patient was considered HRCVD if s/he had (1) an LDL-C test result ≥ 5 mmol/L (hypercholesterolemia) or (2) a hospitalization, ambulatory care visit, or practitioner claim where clinical atherosclerosis, abdominal aortic aneurysm, diabetes mellitus, or chronic kidney disease were coded as either the primary or secondary diagnoses during the study period [6]. Criteria for patient inclusion are presented in detail in Supplementary Table S1 (see the electronic supplementary material). The first occurrence of these events was selected as the index event. We excluded patients who died during the index event and who had any of the above conditions during the past year to create a cohort of newly diagnosed patients with HRCVD. Patients were followed from the index event until death, they moved out of the province, or they were censored at March 2018, and they were categorized into two mutually exclusive groups based on the index event: primary and secondary prevention patients. A patient was categorized as secondary prevention if s/he had a CVD event (nonfatal myocardial infarction, ischemic stroke, revascularization, or other acute coronary syndrome hospitalization) at the index event [6].
2.2 Main Outcomes
The main outcomes were healthcare resource utilization and costs in patients with HRCVD in short- and long-term care after the index event. Other outcomes included distribution of healthcare resource utilization and costs by sex, age, prevention purposes, and qualifying high-risk conditions.
2.3 Costing Methods
Costing methods have been described in detail previously [8]. Briefly, we multiplied the Alberta cost of a standard hospital stay (CSHS) [10] by the resource intensity weight (RIW) value of a hospitalization or ambulatory care visit to have the costs of the respective event. RIW is a measure to estimate resource consumption of each hospitalization or care visit contingent on a patient’s case mix group. The CSHS represents average direct care costs of a standard hospital stay or ambulatory care visit (RIW = 1.00) (e.g., nursing, diagnostic, and therapeutic costs) [11]. The Alberta CSHS values by year are provided in Supplementary Table S2 (see the electronic supplementary material). The costs for fee-for-service practitioner claims were based on the paid amount recorded in the practitioner claims database. The paid amount was not available in 10% of total claims; for these, we used the system-assessed amount instead. We multiplied the number of drug units dispensed by the price of an unit dispensed provided by the Alberta Drug Benefit List [12] to obtain the drug costs. Finally, we summed hospitalization, ambulatory, practitioner claims, and drug costs for each patient to obtain total healthcare costs for each patient each year after the index event. All costs were inflated to 2019 Canadian dollar values using the Canadian Consumer Price Index [13].
2.4 Sensitivity Analysis
A primary prevention patient could have a CVD event during follow-up and became a secondary prevention patient. Therefore, we conducted a sensitivity analysis where we excluded primary prevention patients who had a CVD event during follow-up from the per-patient cost calculation in the year they had a CVD event and subsequent years to examine resource use and costs associated with solely primary prevention.
2.5 Statistical Analysis
We reported patient characteristics using means (± standard deviation), medians (interquartile ranges), counts, and percentages where appropriate. Primary and secondary prevention patients were compared using the Student t test or Kruskal–Wallis and χ2 tests for continuous and categorical variables, respectively. Patient comorbidities were calculated using validated International Statistical Classification of Diseases and Related Health Problems (ICD) codes [14]. Comorbidities were counted if they were recorded in any secondary diagnosis of a hospitalization or ambulatory care visit at the index event, or in any diagnosis of hospitalizations or ambulatory care visits during the year before the index event. Poisson regression was used for incidence rate. Negative binomial regression (zero-inflated model where necessary) was used for count data (i.e., number of ambulatory care visits or number of hospital days), and a generalized linear model (GLM) with gamma distribution and log link was used for cost data.
All analyses were performed using Stata version 14 (Stata Corporation, College Station, Texas) and R version 3.5.2 (R Foundation for Statistical Computing, Vienna). Two-sided p values < 0.05 were considered statistically significant. This study was approved by the Health Research Ethics Board at the University of Alberta (IRB number: Pro00082020).
3 Results
3.1 Baseline Patient Characteristics
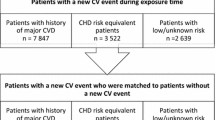
There were 480,473 HRCVD patients in Alberta between FY2012 and FY2016. Of them, 4712 patients died during the index event and 16,562 patients had an HRCVD event during the year prior to the index event. After excluding these patients, the final study cohort consisted of 459,739 patients. The flowchart in Fig. 1 depicts patient selection.
Patient selection flowchart. *(1) A patient identified in the laboratory database was reallocated to the hospital cohort if the test was conducted during hospitalization. (2) A patient identified in the ambulatory care database was reallocated to the hospital cohort if that patient was hospitalized within 1 day. (3) A patient identified in the physician database was reallocated to the hospital cohort if the claim originated from a hospitalization. FY fiscal year, HRCVD high-risk conditions for cardiovascular disease, pt patient
Secondary prevention patients (13,947 patients) accounted for 3% of the study cohort. The secondary prevention patients were older (median age 61 years vs. 56 years; p < 0.001), less likely to be females (30.4% vs. 51.3%; p < 0.001), and less likely to live in an urban area (80.7% vs. 86.1%; p < 0.001) than their primary prevention counterparts.
Patients with clinical atherosclerosis accounted for more than half of the study cohort (57.4%) and the majority of the secondary prevention patients (98%), while patients with abdominal aortic aneurysm contributed the least (1.4%). There were few patients with chronic kidney disease (0.1%) in the secondary prevention group at baseline (Table 1).
Hypertension (9.3%) was the most common non-HRCVD comorbidity and was present in 54.1% of the secondary prevention patients. Charlson comorbidity score in secondary prevention patients (mean = 1.6) was higher than that in primary prevention counterparts (mean = 0.5; p < 0.001). Secondary prevention patients had a shorter follow-up time (median 40.2 months vs. 41 months; p < 0.001) and higher mortality (9.4% vs. 5.2%; p < 0.001) during the study period (Table 1).
3.2 Population Incidence Rate
Both the absolute number (FY2012: 97,281; FY2016: 87,520 patients; p < 0.001) and incidence rate (FY2012: 3225; FY2016: 2687 patients per 100,000 population; p < 0.001) of new patients with HRCVD decreased during the study period (Fig. 2). The incidence rate was higher in females (2984 patients per 100,000 population) than it was in males (2853 patients per 100,000 population; p < 0.001).
3.3 Resource Use and Healthcare Costs
In total, there were 2,277,597 ambulatory care visits, 2,268,600 hospital days, 11,652,714 practitioner claims, and 10,684,899 drug dispensations for the study cohort in the first year after the index event, corresponding to an average of 4.95 ambulatory care visits, 4.93 hospital days, 25.35 practitioner claims, and 23.24 drug dispensations per patient during the first year. After that, health resource utilization decreased during subsequent years in all areas. The number of hospital days dropped the most (4.93 days in the first year to 1.18 days in the fifth year, equal to a 76% drop; p < 0.001) (Table 2).
Compared to primary prevention patients, secondary prevention patients had a higher number of ambulatory care visits (13.66 vs. 4.68 visits; p < 0.001), longer hospital stay (18.32 vs. 4.52 days; p < 0.001), higher number of practitioner claims (37.72 vs. 24.96 claims; p < 0.001), and higher number of drug dispensations (45.59 vs. 22.54 dispensations; p < 0.001) during the first year.
LLD accounted for 7.3% of all drug dispensations during the first year and increased to 8.3% during the fifth year after the index event (p < 0.001). The proportion of LLD was higher in secondary prevention patients (15.4% during the first year) compared to that in primary prevention patients (7% during the first year; p < 0.001). Statins were the most frequent LLD prescription (92.4%). On a per patient basis, only 28.7% of patients used LLD during the first year after the index event. This proportion was lower in the primary prevention patients (26.4%) than it was in the secondary prevention patients (85.3%; p < 0.001). However, while the proportion of patients with LLD remained relatively stable over time after the index event in the primary prevention patients, it decreased gradually in the secondary prevention group (71.7% and 65.6% in the third and fifth year, respectively, both p < 0.001).
Overall, the total healthcare cost for patients with HRCVD during the first year following the index event was CA$5548.1 million during the study period, and the cost decreased over time (FY2012: CA$1161.1; FY2016: CA$1053.5 million; p < 0.001). Hospitalization (55.4%) accounted for most of the cost (Fig. 3).
Patients with HRCVD incurred highest care costs during the first year following the index event (CA$12,068), more than double the care costs during the year prior to the index event (CA$5036) and subsequent years (CA$5626 during the second year and CA$4655 during the fifth year; p < 0.001). Care costs during the first year were higher in males (CA$12,730) than in females (CA$11,422; p < 0.001) and were highest in the most senior group (CA$19,130 in patients aged ≥ 70 years) compared to the costs in younger patients (CA$10,389 in patients aged < 70 years; p < 0.001) (Table 3 and Supplementary Table S4, see the electronic supplementary material).
Care costs for secondary prevention patients (CA$36,641) were triple those for primary prevention patients (CA$11,299; p < 0.001) during the first year, primarily due to higher hospitalization costs in secondary prevention patients (CA$26,896; 73.4% of total care costs), compared to primary prevention patients (CA$6051; 53.6% of total care costs; p < 0.001). The care costs for secondary prevention patients in subsequent years were still higher than those for primary prevention patients, but the extra costs narrowed gradually to CA$395 in the fifth year (CA$5038 vs. CA$4643; p = 0.194) (Table 3 and Fig. 4).
Care costs during the first year were higher in patients with abdominal aortic aneurysm (CA$27,861; p < 0.001) and chronic kidney disease (CA$21,466; p < 0.001) and were lowest in patients with hypercholesterolemia (CA$4232; p < 0.001). From the second year, patients with chronic kidney disease had the highest care costs compared to the other four HRCVD conditions (Supplementary Table S5, see the electronic supplementary material).
3.4 Sensitivity Analysis
After excluding 7421 primary prevention patients who had a CVD event during the first year following the index event, 438,371 primary prevention patients remained for year 1 analysis. Number of ambulatory care visits and hospital days per primary prevention patient during the first year following the index event decreased from 4.68 visits and 4.52 days, respectively, to 4.51 visits and 4.29 days, respectively (both p < 0.001). As a result, the total care costs per primary prevention patient during the first year following the index event decreased from CA$11,299 to CA$10,661 (p < 0.001) (Tables 2, 3, and Supplementary Table S3 [see the electronic supplementary material]). However, the distribution of costs by type of services remained relatively the same (Supplementary Figure S1).
4 Discussion
Our population-based study of HRCVD patients in Alberta during FY2012–2016 found that despite the decrease in the incidence of HRCVD and associated healthcare costs over the study period, healthcare resource utilization and costs for this population were still substantial. During the first year following the index event, the study cohort attended more than 2 million ambulatory care visits, spent more than 2 million days in hospital, accounted for more than 10 million practitioner claims, and had more than 10 million drug dispensations. This level of resource utilization translated into a total 1-year healthcare cost of CA$5.5 billion over a period of 5 years for the provincial healthcare system. On a per patient basis, a patient with HRCVD incurred CA$12,068 in healthcare costs during the first year and CA$4655 during the fifth year after the index event. On a per-patient basis, secondary prevention patients used more resources and incurred higher healthcare costs than primary prevention patients during each of the 5 years followed up. However, it should be noted that in the setting of primary prevention, yearly event rates are lower and duration of treatment is typically longer, so the overall costs for it might be higher. Resource use and healthcare costs were higher in males and the elderly population compared to that in females and the younger population, respectively.
While dyslipidemia is a known and established risk factor for CVD, most studies focus on cost-effectiveness analysis of LLD, not the overall cost burden of the condition. Other studies estimate the cost burden of CVD [1, 3] or specific conditions such as myocardial infarction [15, 16] or heart failure [17, 18]. In the context of prevalent dyslipidemia, population aging in Canada, and the known relationship between dyslipidemia and CVD risk, the present study provides policy makers with additional insights on the overall cost burden on healthcare in patients with HRCVD who are recommended to start a statin to control dyslipidemia to prevent CVD events and mortality [6, 19, 20]. We found that the healthcare costs associated with HRCVD were substantial but decreased during the study period. These findings are in line with a recent study on the costs of myocardial infarction in Alberta between 2004 and 2013 that reported a decreasing trend in both the total healthcare costs and the costs per hospitalization. The decrease in healthcare costs and HRCVD incidence could be an indication of success in primary prevention efforts, a result of advancement in disease management (such as myocardial infarction), as well as decreased hospital length of stay over time [16, 21].
Despite CCS recommendation of statins for patients with HRCVD [6], we found a low proportion of LLD use, which was even suboptimal in secondary prevention patients. This result corresponds with other reports of low LLD use in the literature [22, 23]. The low LLD uptake, in combination with decreased LLD use over time in secondary prevention patients who need LLD the most to prevent a CVD recurrence, highlights the need to improve care practice for patients with HRCVD to better control dyslipidemia in this high-risk population. We have reported previously that patients with HRCVD who optimally control dyslipidemia gain additional health benefits compared to those who do not [8]. Hence, a multi-pronged approach for both physicians and patients could be considered to improve LLD uptake and adherence, and subsequently improve prevention efforts in the high-risk populations for CVD. First, guideline adherence among prescribers may be the most important opportunity. Bradley et al. reported that 59% of statin-eligible patients had never been offered a statin [23]. Even though the differences in the US and Canadian healthcare systems may limit generalization to the Canadian context, this finding does suggest physician perception of patients’ risk and of guideline adherence plays a critical role in the prevention of CVD. In addition, drug packaging and funding could also be an important factor for LLD adherence. Fixed-dose combination LLD has been reported to result in higher adherence than multi-pill therapies [24] and subsequently result in cost savings [25], and an increased out-of-pocket payment has been shown to have a negative effect on statin adherence [26]. Education on perceived side effects of LLD could also help improve LLD uptake and adherence [23]. Further, in the era of rapid development in digital health, use of a wearable device such as a reminder assistant could improve LLD adherence as seen in other chronic diseases like chronic obstructive pulmonary disease [27, 28].
In addition to control of blood lipids, which has the highest population attributable risk for myocardial infarction [29], innovative prevention measures targeting other modifiable risk factors for CVD in general should be enhanced to improve prevention efforts and reduce healthcare cost burden in this high-risk population. Kahn et al. estimated that implementing all recommended CVD prevention activities (i.e., providing aspirin and LLD, lowering blood pressure, reducing weight, and smoking cessation) would result in an additional 244 million quality-adjusted life-years over a period of 30 years for the US adult population, and most of the prevention activities are cost-effective from a societal perspective and are cost saving from a healthcare system perspective [30]. Similarly, Yang et al. reported that a supplement of plant sterol-enriched foods for a high-risk population could be cost-effective in preventing CVD events from a societal perspective and could result in cost savings for healthcare systems if consumers bear the costs of the food supplements [31]. Therefore, better involvement and participation from other sectors and patients in CVD prevention could help relieve the healthcare cost burden in an era of ever-increasing healthcare costs in developed countries, including Canada [32].
Our study provides novel data on the resource use and healthcare cost burden in the short- and long-term care of patients with HRCVD. However, it has limitations. First, resource use and costs incurred in privately funded healthcare facilities (i.e., privately funded practitioners or rehabilitation facilities) were not included. In a publicly funded healthcare system in Alberta, these costs should be very small and should not affect the study results. Secondly, the drug costs did not include dispensing fee, so the healthcare cost burden could even be higher than the present estimates. Lastly, we focused solely on the healthcare costs and did not include indirect costs in the estimates. Heidenreich et al. estimated that productivity losses could be as high as 55% of the direct medical costs for CVD in 2015 in the USA [1]. Therefore, the real economic burden associated with HRCVD in Alberta could be substantially higher.
5 Conclusion
This population-based study of patients who are at high risk for cardiovascular disease shows that the burden of healthcare costs associated with the conditions is substantial but decreases over time. The long-term care costs are much less than the costs incurred during the first year after diagnosis.
References
Heidenreich PA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44.
Leal J, et al. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J. 2006;27:1610–9.
Public Health Agency of Canada. Tracking heart disease and stroke in Canada, 2009, viii. Ottawa: Public Health Agency of Canada; 2009.
Collaboration CTT. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Grundy SM, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–143.
Anderson TJ, et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can J Cardiol. 2016;32(11):1263–82.
Brunham LR, et al. Canadian Cardiovascular Society Position Statement on Familial Hypercholesterolemia: Update 2018. Can J Cardiol. 2018;34(12):1553–63.
Tran DT, et al. Outcome and Cost of Optimal Control of Dyslipidemia in Adults with High Risk for Cardiovascular Disease. Can J Cardiol. 2021;37(1):66–76.
Alberta Health. Overview of Administrative Health Datasets. 2017 April 28, 2017. https://open.alberta.ca/dataset/657ed26d-eb2c-4432-b9cb-0ca2158f165d/resource/38f47433-b33d-4d1e-b959-df312e9d9855/download/Research-Health-Datasets.pdf. Accessed 3 Octo 2020.
Canadian Institute for Health Information. Cost of a Standard Hospital Stay 2019. http://yourhealthsystem.cihi.ca/inbrief/?lang=en&_ga=2.233170907.456686591.1556912958-199991464.1544733065#!/indicators/015/cost-of-a-standard-hospital-stay/;mapC1;mapLevel2;trend(C1,C20018). Accessed 3 May 2019.
Canadian Institute for Health Information. Cost of a standard hospital stay: appendices to indicator library—methodology notes. Canadian Ottawa: Institute for Health Information; 2017.
Alberta Health. Interactive Drug Benefit List. 2018. https://www.ab.bluecross.ca/dbl/publications.html. Accessed 10 May 2018
Statistics Canada. Table 326-0020: Consumer Price Index (CPI). June 6, 2018. http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=3260020&&pattern=&stByVal=1&p1=1&p2=37&tabMode=dataTable&csid=. Accessed 3 May 2019.
Quan H, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Tran DT, et al. Resource use and burden of hospitalization, outpatient, physician, and drug costs in short- and long-term care after acute myocardial infarction. Can J Cardiol. 2018;34(10):1298–306.
Tran DT, et al. The healthcare cost burden of acute myocardial infarction in Alberta, Canada. Pharmacoecon Open. 2017;2(4):433–42.
Tran DT, et al. The current and future financial burden of hospital admissions for heart failure in Canada: a cost analysis. CMAJ Open. 2016;4(3):E365–70.
Heidenreich PA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19.
Statistics Canada. Cholesterol levels of adults, 2012 to 2013. https://www150.statcan.gc.ca/n1/pub/82-625-x/2014001/article/14122-eng.htm. Accessed 9 July 2019.
Statistics Canada. Table: 17-10-0057-01 (formerly CANSIM 052-0005) - Projected population, by projection scenario, age and sex, as of July 1 (x 1,000). CANSIM (database). http://www5.statcan.gc.ca/cansim/pick-choisir?lang=eng&p2=33&id=0520005. Accessed 7 Feb 2018.
Reddy K, Khaliq A, Henning RJ. Recent advances in the diagnosis and treatment of acute myocardial infarction. World J Cardiol. 2015;7(5):243–76.
Chen G, et al. Treatment and low-density lipoprotein cholesterol management in patients diagnosed with clinical atherosclerotic cardiovascular disease in Alberta. Can J Cardiol. 2019;35(7):884–91.
Bradley CK, et al. Patient-reported reasons for declining or discontinuing statin therapy: insights from the PALM Registry. J Am Heart Assoc. 2019;8(7):e011765.
Balu S, et al. Impact of fixed-dose and multi-pill combination dyslipidemia therapies on medication adherence and the economic burden of sub-optimal adherence. Curr Med Res Opin. 2009;25(11):2765–75.
Gaziano TA, et al. Modeling the cost effectiveness and budgetary impact of Polypills for secondary prevention of cardiovascular disease in the United States. Am Heart J. 2019;214:77–87.
Gibson TB, et al. Impact of statin copayments on adherence and medical care utilization and expenditures. Am J Manag Care. 2006;12:11–9.
Wu R, et al. Feasibility of using a smartwatch to intensively monitor patients with chronic obstructive pulmonary disease: prospective cohort study. JMIR Mhealth Uhealth. 2018;6(6):e10046.
Tran DT, et al. Current and future direct healthcare cost burden of chronic obstructive pulmonary disease in Alberta, Canada. Can J Respir Crit Care Sleep Med. 2019;4(1):39–47.
Yusuf S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Kahn R, et al. The impact of prevention on reducing the burden of cardiovascular disease. Circulation. 2008;118(5):576–85.
Yang W, et al. The effectiveness and cost-effectiveness of plant sterol or stanol-enriched functional foods as a primary prevention strategy for people with cardiovascular disease risk in England: a modeling study. Eur J Health Econ. 2018;19(7):909–22.
Stabile M, et al. Health care cost containment strategies used in four other high-income countries hold lessons for the United States. Health Aff (Millwood). 2013;32(4):643–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was reviewed and approved by Health Research Ethics Board at the University of Alberta (IRB number: Pro00082020).
Consent to participate
Not applicable.
Consent for publication
The study was reviewed and approved for publication by our Institutional Reviewer.
Data availability statement
The data that support the findings of this study are available from Alberta Health. However, restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from Alberta Health.
Code availability
The Stata code is available upon reasonable request from the corresponding author.
Conflict of interest
Dat Tran, Dan Palfrey, and Robert Welsh have no conflicts of interest to disclose.
Funding
This research has been commissioned and funded by Alberta Innovates, through the Alberta/Sanofi Health Innovation Fund.
Author contributions
DTT and RW conceptualized the study. DTT carried out analyses and drafted the manuscript. DP secured funding support. All the authors contributed to the writing. All the authors critically reviewed the manuscript for intellectual content.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tran, D.T., Palfrey, D. & Welsh, R. The Healthcare Cost Burden in Adults with High Risk for Cardiovascular Disease. PharmacoEconomics Open 5, 425–435 (2021). https://doi.org/10.1007/s41669-021-00257-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-021-00257-8