Abstract
Background
Standard biopsy for prostate cancer diagnosis is an unpleasant and sometimes painful procedure with a detection rate as low as around 50%. Consequently, an accurate blood-based test would be highly desirable to improve the predictive accuracy. However, the clinical value of a new blood test for diagnosing prostate cancer depends on its sensitivity and specificity, in relation to the selected target population.
Objective
The aim of this analysis was to investigate the health-economic value of introducing a new and more accurate diagnostic blood-based test to identify men in need of a biopsy to diagnose prostate cancer.
Method
We developed a Discrete Event Simulation Model with outputs including number of biopsies, cancer diagnosis, treatments and prostate cancer deaths. The analysis was performed from a health care perspective. It used epidemiologic data, treatment patterns, and health care costs from the Swedish region Skåne (population of 1.3 million). A 90% sensitivity and specificity of the new test was assumed.
Results
Among 31,250 men, age 50–69 years, 16.4% had a PSA between 3.0 and 9.9 µg/L and 28.9% a PSA of 2.0–9.9 µg/L. Testing men with PSA 3.0–9.9 µg/L, as in current clinical practice, decreased the number of biopsies by 3595, detected 61 more cancers, resulting in and two more fatalities and subsequently a loss of 14 QALYs. Cost offsets could justify a test value of SEK 4996. Testing a larger population, PSA 2.0–9.9 µg/L prevented 6 deaths, added 50 QALYs, and could justify a value of the test of SEK 5165, given a value of health of SEK 500,000 per QALY.
Conclusion
A new blood-based test for prostate cancer has a significant potential to reduce the number of biopsies needed, resulting in reduced health care costs and improve patient care.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
A new blood-based test for prostate cancer has the potential to reduce the number of biopsies needed and decrease health-care costs. |
If the test is used in an extended population it could also reduce the number of deaths from prostate cancer. |
1 Introduction
Prostate cancer is one of the most common cancers and the third leading cause of cancer-related deaths among men in developed countries [1]. One factor behind this dismal development is the lack of symptoms at an early stage of the disease, resulting in late diagnosis since the diagnostic tools available today are insufficient and not applicable to a population-based screening. The introduction of measuring Prostate-Specific Antigen (PSA) in blood in the mid-1980s, provided an important tool for monitoring of prostate cancer, and did result in tumor detection at a much earlier phase of the disease [2].
However, while the PSA test has high sensitivity it suffers from low specificity, resulting in an immense over diagnosis, with studies showing that only 25% (PSA values ranging between 4 and 10) to 53% (majority of PSA values ranging between 3 and 10) of men who are biopsied due to an elevated PSA actually have prostate cancer [2, 3]. Another limitation is the sensitivity of the systemic prostate biopsy, which may be as low as 48% for clinically significant prostate cancer [4], meaning that more than half of these cases are not diagnosed correctly with the standard procedure. However, recent studies on targeted biopsies after multiparametric magnetic resonance imaging (mpMRI) have shown improved diagnostic accuracy and reduced number of biopsies needed [4, 5].
Despite such improved protocols to diagnose prostate cancer, there is a consistent problem with overdiagnosis and overtreatment, i.e. biopsies of men with slightly increased PSA values lead to detection of clinically insignificant tumors and side-effects after surgery or radiation therapy (RT). In addition, despite being an unpleasant and painful procedure the prostate biopsies are also accompanied with several adverse side-effects, such as infections and bleeding [6]. Furthermore, not all men can undergo MRI for different reasons and pre-biopsy MRI is not yet implemented in guidelines [7].
Due to these limitations, several diagnostic assays have been presented over the last years [8], such as, (1) STHLM3 [9] that has shown to reduce unnecessary biopsies in prostate cancer with Gleason ≥ 7; (2) Prostate health Index (PHI) [10] and (3) 4KScore [3, 11]. All three algorithms are based on proteins in the kallikrein family and have demonstrated an increased specificity reducing unnecessary biopsies but a limited sensitivity which results in failure to detect some cancers. Since many tests are being developed there is a need for an assessment to the potential value of these tests.
We have developed a solid technology platform for multiparametric protein expression profiling, using recombinant antibody fragments. This platform has successfully identified highly accurate diagnostic protein signatures in e.g. pancreatic cancer, as well as in other complex diseases [12]. In a pilot study, we also demonstrated that it could potentially be used to develop a blood-based test for stratifying prostate cancer risk groups [13]. However, further studies are needed to validate diagnostic tests for prostate cancer, where a sensitivity and specificity reaching over 90% would be desirable to further improve on current methods [14], which would significantly improve early diagnosis and reduce the number of prostate biopsies needed.
Estimating the health economic value of introducing a new test in prostate cancer diagnosis before being fully developed, would generate important incentive to facilitate further development of new tests for prostate cancer diagnosis. The current study is based on the clinical guideline used in Sweden today were MRI guided biopsy and/or active surveillance are still not a general recommendation. There are several tests proposed along the PC care pathway (e.g. to stratify for biopsy, to determine aggressiveness of the tumor and tests to monitor progression). While it would be interesting to analyze the difference a new test could make in all these pathways, in this study we focus on the effect a new test would have if introduced as a screening tool at diagnosis, after a PSA test, which is why the patient groups in this study are divided based on their PSA value.
Health economic early-decision modeling [15, 16] is a well-established method to quantitatively estimate the likely health and cost consequences of a new test in the diagnostic pathway for prostate cancer, i.e. to screens for persons in need of a biopsy and previous health economic studies have shown a possibility to reduce unnecessary biopsies [17]. Consequently, the objective of this study was to estimate the potential value of a new diagnostic blood-based test in prostate cancer in a cohort representing PSA tested men 50–69 years old.
2 Methods
This study was conducted in accordance with Swedish and international guidelines for economic evaluation [18, 19]. [18, 19]. The analysis has a health-care sector perspective, including only health-care costs.
We constructed a Discrete Event Simulation (DES) model for evaluation of prostate cancer diagnostics and treatment. It uses micro-simulation techniques to simulate individual diagnostic pathways and capture competing event risks. We included 31,250 men, representing PSA-tested men aged 50–69 years in Region Skåne, Sweden. Each man was assigned, (1) a starting age between 50 and 69 years, (2) an age-related PSA-value, based on aggregated registry data from PSA-testing in Region Skåne (Table 1, Dr. Anna Jöud, Lund University), and (3) a prostate cancer status, i.e. (a) no cancer, (b) Gleason 6 (GS6) cancer or (c) Gleason ≥ 7 (GS ≥ 7) cancer [20]. All men were PSA-tested and diagnostic pathways were simulated based on PSA-test results, based on the standardized prostate cancer care pathway in Sweden.
In current clinical practice, men with PSA ≥ 3 µg/L or abnormal digital rectal examination (DRE) undergo prostate biopsy [7]. In this study, three hypothetical testing strategies were evaluated and compared with current clinical practice. The first strategy tested the same men as in current clinical practice, with a PSA value between 3.0 and 9.9 µg/L, aiming to reduce the need for biopsies (Fig. 1). The second strategy tested an extended population with a PSA value between 2.0 and 9.9 µg/L. The third strategy, only tested men with a PSA value between 2.0 and 2.9 µg/L. The tests were evaluated using assumed values of 90% sensitivity, for both GS6 and GS ≥ 7 cancer, and 90% specificity.
Flow charts for diagnosis of prostate cancer, for a current clinical practice, b testing strategy prostate-specific antigen (PSA) 3.0–9.9 µg/L, C) testing strategy PSA 2.0–9.9 µg/L and D) testing strategy PSA 2.0–2.9 µg/L. For simplicity of illustration digital rectal examination is not included in the flow chart
Prostate biopsy was modeled at 48% sensitivity [4], 100% specificity and 4.2% risk of hospitalization [21] based on a US Medicare population (Table 2). Any undetected cancer was incidentally detected after 7 years based on lead time in the European Randomized Study of Screening for Prostate Cancer (ERSPC) [22]. Men with GS6 cancer were assigned active surveillance (75%) or radical treatment (25%), while men diagnosed with GS ≥ 7 cancer were assigned radical treatment (80%) or watchful waiting (20%), based on Swedish treatment pattern of today [23]. Active surveillance was modeled according to the PRIAS-protocol [24] and men with a GS ≥ 7 cancer at biopsy were changed to radical treatment. Men on watchful waiting receive no further treatment, unless occurrence of metastasis.
In the model, we assume that prostate cancer advanced progressively from GS6 cancer to GS ≥ 7 cancer to metastatic cancer (Fig. 3 in Appendix). The risks of progression for GS6 cancers on active surveillance and radical treatment were calibrated by using the event rates for metastasis and all cause death in the Prostate Testing for Cancer and Treatment (ProtecT) [25]. The risk of metastasis for GS ≥ 7 cancer on radical treatment and watchful waiting were calibrated by using the corresponding event rates in the Prostate Cancer Intervention versus Observation Trial (PIVOT) [26]. The model has a lifelong time horizon and it was assumed that only men with metastatic cancer could die from prostate cancer [27], while all men also had Swedish age-related other-cause mortality [28].
Costs for curative treatments and hospitalization were obtained from the hospital administration and costs for PSAtest, prostate biopsy and diagnosis from price lists from the regional healthcare provider, Region Skåne (Table 3) [29,30,31]. The yearly cost for treating metastatic cancer was based on a recent health-economic evaluation by the Swedish Dental and Pharmaceutical Benefits Agency [32]. All costs were calculated in Swedish currency (SEK) at 2017 price level. Health effects were quantified as Quality-adjusted life years (QALYs) and event-related QALY-losses were based on literature [33]. All health effects and cost were discounted at a yearly discount rate of 3% following Swedish recommendations [19].
Model outputs included number of biopsies, cancer diagnosis, treatments and death from prostate cancer. Total costs and QALYs were calculated based on modelled events. For each testing strategy, the test value was calculated at a cost-neutral level, resulting in no increase in health care costs, and at a value of health of SEK 500,000 per QALY, which is the threshold between a moderate and a high cost per QALY used by the Swedish National Board of Health and Welfare [34]. Potential value drivers were tested by deterministic and probabilistic sensitivity analysis across 1000 simulated cohorts. In the probabilistic sensitivity analysis, the risks of progression, metastasis, and prostate cancer death, as well as unit costs and utility values were randomized using normal distributions and a 10% standard error.
3 Results
3.1 Current Clinical Practice
Modeling current clinical practice, with men having PSA ≥ 3 µg/L or abnormal DRE being biopsied, resulted in 8706 biopsies. In total, 703 GS6, and 281 GS ≥ 7 cancers were initially detected at the start of simulation, while 3082 men received curative treatment during the course of the simulation and 901 died from prostate cancer. The total cost accumulated over the lifetime of the 31,250 men was 1.2 billion SEK. The majority of this was from the treatment of metastatic cancer (793 million SEK for 1111 treated men) and radical treatment (273 million SEK 3082 treated men). In total, the men generated 380,334 QALYs over their lifetimes (on average 12.2 discounted QALYs per man).
3.2 Introduction of a New Diagnostic Test
After the initial modeling, a hypothetic new test was added to the diagnostic scheme to screen for those in need of a biopsy. The test was evaluated using three different testing strategies. The results are presented at a 90% sensitivity and specificity of the new test.
3.2.1 PSA Value Between 3.0 and 9.9 µg/L
In the first testing strategy, 5126 men with PSA values between 3.0 and 9.9 µg/L and normal DRE were tested, which resulted in 3595 fewer biopsies (Table 4). However, 45 less GS6 cancers and 16 less GS ≥ 7 cancers were initially detected. Consequently, another five men did not receive curative treatment during the course of the simulation and two more men died from prostate cancer. While this testing strategy reduced health care costs by SEK 26 million it also led to a health loss of 14 QALYs. The cost-neutral value of the test was SEK 4996 and the value of the test, at a value of health of SEK 500,000 per QALY was SEK 3622.
3.2.2 PSA Value Between 2.0 and 9.9 µg/L
The second testing strategy of 9014 men with PSA between 2.0 and 9.9 µg/L reduced the number of biopsies by 2608. At the same time more cancer cases were initially detected, and six fewer men died from prostate cancer. The testing strategy lead to both a health gain and a cost reduction, with a test value of SEK 5165 at the same value of health as before.
3.2.3 PSA Value Between 2.0 and 2.9 µg/L
The third testing strategy, which only tested the 3888 men with PSA between 2.0 and 2.9 µ/L, lead to 987 more biopsies. However, 22 more patients received curative treatment and eight less died from prostate cancer. This strategy lead to a health gain but at a cost increase with a test value of SEK 7199 using the same value of health as before.
3.3 The Effect of a Changes in Sensitivity and Specificity
The impact of different assumptions of sensitivity and specificity on the value of the test is demonstrated in Table 5. For the first strategy the cost neutral value of the test varies from 2800 SEK for low specificity up to 5100 SEK for high specificity. For the second strategy the cost neutral value of the test varies from 100 SEK for low specificity up to 2500 SEK for high specificity. The third strategy does not generate a positive cost neutral value of the test for any of the sensitivity and specificity analyzed, since this strategy drives the health care costs upwards by diagnosing more prostate cancer patients.
However, by attaching a monetary value to the health gains, corresponding to SEK 500,000 per QALY gained, the third strategy gives the highest value of the test, of about SEK 7200. The better sensitivity and the specificity the more value will be attached to the test. Both the first and second strategy will generate positive values of the test, but only when sensitivity and specificity reached certain thresholds. For example, for strategy one sensitivity must reach 70% in combination with a specificity of at least 80% to generate a positive value.
3.4 Value Drivers
The value of the test depends on how the health care and treatment strategies are organized. In this analysis the differences in test values are demonstrated by three different testing strategies. The first strategy corresponds to current approach of testing men at PSA 3.0 and above. The second strategy assumes an extended testing of men with PSA 2.0 and above, and the third strategy is implementing the new test only for men with PSA values between 2.0 and 2.9.
The cost-neutral value of the first testing strategy (PSA 3.0–9.9 µg/L) was mainly driven by the price of biopsies, while the cost-neutral values for the second (2.0–9.9 µg/L) and the third (2.0–9.9 µg/L) testing strategies were affected by both the biopsy cost and the treatment cost of metastatic disease (Appendix Table 6). Biopsy cost remained an important value driver even when health effects were included at a value of health of SEK 500,000 per QALY. The value of all treatment strategies at this value of health was also affected by the biopsy sensitivity, time to incidental detection and risk of metastatic disease.
3.5 Probabilistic Sensitivity Analysis
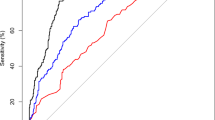
The probabilistic sensitivity analysis indicated that the results are robust. The results for each of the three strategies are shown in the cost-effectiveness planes in Fig. 2. The first testing strategy reduced health care costs in all simulations, with cost savings between SEK 19 million and SEK 31 million (95% confidence interval). The corresponding cost-neutral value of the test was SEK 3798 to SEK 6124 and the value of the test, at a value of health of SEK 500,000 per QALY was SEK 2727 to SEK 4029.
The second strategy was dominant in 98% of the simulations, with cost savings between SEK 13 million and SEK 31million and health gains between 2 and 111 QALYs (95% confidence interval). The related cost-neutral value of the test was SEK 1440 to SEK 3433 and the test value at the same value of health as before was SEK 3529 to SEK 7606.
The third strategy lead to health gains in more than 99% of the simulations but at a cost-increase in 82% of the simulations. The health gains ranged between 12 and 127 QALYs and the cost changes ranged from cost savings of SEK 6 million to a cost increase of SEK 12 million (95% confidence interval). The corresponding test value, at a value of health of SEK 500,000 per QALY was SEK 3068 to SEK 13,217.
4 Discussion
The adoption of a new test for prostate cancer for persons in need of a biopsy (PSA value in the range of 3.0–9.9 µg/L), with 90% sensitivity and specificity, has a potential to reduce health care costs due to a decrease in clinical resources used. However, at a sensitivity of 90% for the new test will result in fewer diagnosed patients with cancer compared to the current Swedish strategy with biopsies of all men with PSA value ≥ 3. If the new test would be implemented in a region such as Region Skåne in Sweden with a population of 1.3 million people, about 60 patients less would be diagnosed with prostate cancer, resulting in 2 additional deaths. However, in the same region we can expect reduced costs of about 26 million SEK.
The value of a test is generally determined based on two types of value propositions. The first one is related to the reduction of resources used as consequence of implementing the new test. The second value is the health gains due to the use of the new test. With a target population of men with PSA 3.0–9.9 µg/L cost offsets have a potential too justify a value per test of SEK 5000. However, with an assumed sensitivity of the new test of 90% it will not identify as many prostate cancers as the current management, thus, the new test will result in loss of QALYs, which will reduce the value of the new test to a total value of SEK 3600 when both types of value drivers are considered.
However, if a new test will be used to test an extended population, including men with PSA values between 2 and 2.9 in addition to men with PSA ≥ 3, we will identify more patients with prostate cancer. This has the potential to reduce the number of deaths with prostate cancer and increase the number of QALYs. At the same time, we will expect cost offsets due to reduced number of biopsies and surgical procedures. The value of improved detection of prostate cancer and the subsequent treatment of cancer could justify a value of this new test in the magnitude of SEK 5200 per test if the society is willing to pay SEK 500,000 per QALY gained. From a health care perspective, assuming no value of health, the cost offsets generated by introducing the new test can justify a value for the test in the magnitude of SEK 2400.
A strength of the cost-effectiveness model is that it can be used to estimate the outcomes of many additional potential strategies. For example, we modeled a subpopulation of men with PSA value between 2.0 and 2.9 µ/L. This gave 987 fewer biopsies, 322 more prostate cancers detected and 8 less deaths. This resulted in 64 QALYs, additional costs of 4 million SEK and a test value of SEK 7199, if value of health per QALY again is assumed to be 500,000 SEK. The use of decision-analytic modelling also enables the estimation of results for several combinations of sensitivity and specificity for the new test. Another strength of our analysis is that we have used real world data, from Swedish registries, regarding the actual prevalence of PSA-testing and the distribution of PSA-values among tested men.
A limitation with our study is that progression rates and metastasis risks were taken from international clinical studies and may differ from real-world data. Additionally, there was only one publicly available risk equation for prostate cancer, which limited our possibility of varying cancer prevalence in the sensitivity analysis. Another limitation was the lack of data on the size of the disutility associated with a prostate biopsy. While this does not affect the cost-neutral value of the test, it would have increased the value of test at a value of health of SEK 500,000 per QALY for the first and second testing strategies, while decreasing it for the third testing strategy.
Early health economic assessment of new health care technologies is often used to identify which criteria must be met, and under what conditions they are expected to be cost-effective, i.e. good value for money. Our study aimed at identifying and analyzing some of these criteria and conditions in order to specify which factors are driving the value of the new test. First the analyses provided are intended to identify information gaps and to guide further research in the development of a test for prostate cancer. Secondly, economic modeling in early stages can identify parameters to which the estimates of value drivers are particularly sensitive. It is important to identify these parameters early in the development process in order to plan and priorities for future data collection. Thirdly, pricing of a new product starts early in the development process and understanding and collecting data for demonstration of the value of a new technology is a key driver for pricing. Early cost-effectiveness modeling is important to take customers and their value of health into account, understanding the payers value perceptions and integrate them into the development process.
5 Conclusion
In brief, a blood-based test, displaying 90% sensitivity and specificity would be a significant improvement for early diagnosis of prostate cancer.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Barry MJ. Clinical practice. Prostate-specific-antigen testing for early diagnosis of prostate cancer. N Engl J Med. 2001;344:1373–7.
Vickers AJ, Gupta A, Savage CJ, Pettersson K, Dahlin A, Bjartell A, et al. A panel of kallikrein marker predicts prostate cancer in a large, population-based cohort followed for 15 years without screening. Cancer Epidemiol Biomark Prev. 2011;20:255–61.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Raaijmakers R, Kirkels WJ, Roobol MJ, Wildhagen MF, Schrder FH. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002;60:826–30.
Regionala Cancercentrum i Samverkan. Standardized Prostate Cancer Care [Standardiserat vårdförlopp för prostatacancer]. 2016.
Olleik G, Kassouf W, Aprikian A, Hu J, Vanhuyse M, Cury F, et al. Evaluation of new tests and interventions for prostate cancer management: a systematic review. J Natl Compr Canc Netw. 2018;16:1340–51.
Gronberg H, Adolfsson J, Aly M, Nordstrom T, Wiklund P, Brandberg Y, et al. Prostate cancer screening in men aged 50–69 years (STHLM3): a prospective population-based diagnostic study. Lancet Oncol. 2015;16:1667–76.
Loeb S, Shin SS, Broyles DL, Wei JT, Sanda M, Klee G, et al. Prostate Health Index improves multivariable risk prediction of aggressive prostate cancer. BJU Int. 2017;120:61–8.
Vedder MM, de Bekker-Grob EW, Lilja HG, Vickers AJ, van Leenders GJ, Steyerberg EW, et al. The added value of percentage of free to total prostate-specific antigen, PCA3, and a kallikrein panel to the ERSPC risk calculator for prostate cancer in prescreened men. Eur Urol. 2014;66:1109–15.
Mellby LD, Nyberg AP, Johansen JS, Wingren C, Nordestgaard BG, Bojesen SE, et al. Serum biomarker signature-based liquid biopsy for diagnosis of early-stage pancreatic cancer. J Clin Oncol. 2018;36:2887–94.
Nordstrom M, Wingren C, Rose C, Bjartell A, Becker C, Lilja H, et al. Identification of plasma protein profiles associated with risk groups of prostate cancer patients. Proteom Clin Appl. 2014;8:951–62.
Zappala SM, Scardino PT, Okrongly D, Linder V, Dong Y. Clinical performance of the 4Kscore Test to predict high-grade prostate cancer at biopsy: a meta-analysis of us and European clinical validation study results. Rev Urol. 2017;19:149–55.
Hartz S, John J. Contribution of economic evaluation to decision making in early phases of product development: a methodological and empirical review. Int J Technol Assess Health Care. 2008;24:465–72.
MJ IJ, Koffijberg H, Fenwick E, Krahn M. Emerging use of early health technology assessment in medical product development: a scoping review of the literature. Pharmacoeconomics. 2017;35:727–40.
Nicholson A, Mahon J, Boland A, Beale S, Dwan K, Fleeman N, et al. The clinical effectiveness and cost-effectiveness of the PROGENSA(R) prostate cancer antigen 3 assay and the Prostate Health Index in the diagnosis of prostate cancer: a systematic review and economic evaluation. Health technology assessment. 2015;19:1–191.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
The Dental and Pharmaceutical Benefits Agency. The Dental and Pharmaceutical Benefits Agencys general guidelines (TLVAR 2017:1) [Tandvårdsoch läkemedelsförmånsverkets allmänna råd (TLVAR 2017:1)]. TLVAR 2017:12017.
Ankerst DP, Koniarski T, Liang Y, Leach RJ, Feng Z, Sanda MG, et al. Updating risk prediction tools: a case study in prostate cancer. Biometric J Biometrische Zeitschrift. 2012;54:127–42.
Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830–4.
Finne P, Fallah M, Hakama M, Ciatto S, Hugosson J, de Koning H, et al. Lead-time in the European randomised study of screening for prostate cancer. Eur J Cancer. 2010;46:3102–8.
The Swedish National Prostate Cancer Register. National Report for Prostate Cancer 2017 [Prostatacancer Nationell kvalitetsrapport för 2017]. Assessed http://www.npcr.se.
Bokhorst LP, Valdagni R, Rannikko A, Kakehi Y, Pickles T, Bangma CH, et al. A decade of active surveillance in the PRIAS study: an update and evaluation of the criteria used to recommend a switch to active treatment. Eur Urol. 2016;70:954–60.
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375:1415–24.
Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ, Fox S, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367:203–13.
National Cancer Institute. SEER cancer statistics review, cancer of the prostate (invasive), 5-year relative survival 2004–2010 by stage at diagnosis.
Statistics Sweden. Demographics, Life Table by sex and age, 2016 [Befolkningsstatistik, Livslängdstabell efter kön och ålder, 2016].
Region Skåne. Clinical chemistry price list [Klinisk kemi prislista]. 2017.
Region Skåne. Medical imaging price list [Bildoch funktionsmedicin prislista]. 2017.
Södra Regionvårdsnämnden. Regional prices and compensation for the southern health care region [Regionala priser och ersättningar för södra sjukvårdsregionen]. 2017.
The Dental and Pharmaceutical Benefits Agency. Zytiga (abirateron). 2015.
Heijnsdijk EA, Wever EM, Auvinen A, Hugosson J, Ciatto S, Nelen V, et al. Quality-of-life effects of prostate-specific antigen screening. N Engl J Med. 2012;367:595–605.
Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). Assessment of methods in health care and social services. 2018.
Acknowledgements
The support by Anna Jöud, PhD, Division of Occupational and Environmental Medicine, Lund University, for information on age-related PSA distributions is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
AF constructed the simulation model and conducted the analysis. AB provided clinical expert opinion on the disease area. The manuscript was drafted by AF and UA. All authors contributed to the planning of the study, interpretation of results and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by VINNOVA as a part of the UDI program—Advanced diagnostics in oncology a test bed for risk prediction in prostate cancer and by CREATE Health Translational Cancer Center.
Conflict of interest
Adam Fridhammar, Ulrika Axelsson, Ulf Persson, Anders Bjartell and Carl A.K. Borrebaeck have no conflict of interest.
Ethics approval
Not applicable
Consent to participate
Not applicable
Data availability atatement
All data generated or analyzed during this study are included in this published article and its supplementary files. The simulation model used to derive the analysis is the proprietary of IHE, and access to the model is at the discretion of IHE. The model was shared with the manuscript reviewers upon request.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fridhammar, A., Axelsson, U., Persson, U. et al. The Value of a New Diagnostic Test for Prostate Cancer: A Cost-Utility Analysis in Early Stage of Development. PharmacoEconomics Open 5, 77–88 (2021). https://doi.org/10.1007/s41669-020-00226-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-020-00226-7