Abstract
Background and Objective
Significant clinical burden is associated with higher-risk myelodysplastic syndromes (HR-MDS); however, the economic burden has not been fully examined. We examined cost of care and healthcare utilization (HCU) in HR-MDS patients engaged in routine care in the United States (US).
Methods
Adult US patients diagnosed with HR-MDS from 1/1/2008 to 10/31/2015 were identified from the Optum database. Patients were followed until death, progression to acute myeloid leukemia (AML), end of enrollment, or end of study (12/31/2015). Myelodysplastic syndrome (MDS)-related costs/HCU (including medical/pharmacy claims with a primary diagnosis of MDS, MDS-related treatment, or supportive care) and non-MDS-related costs/HCU were evaluated. Costs were calculated as per-patient per-month (PPPM) costs adjusted to 2015 US dollars.
Results
Of the 209 HR-MDS patients included, median follow-up was 9.9 months (interquartile range 4.6–17.9), and 69.4% had at least one inpatient admission, 56.9% had at least one emergency department visit, and nearly all patients had at least one outpatient visit. Average PPPM costs over follow-up were $17,361; year 1 versus year 2 costs were higher ($17,337 vs $12,976) following HR-MDS diagnosis. The majority of costs were for MDS-related medical services ($10,327 PPPM). MDS-related medical PPPM costs decreased from $10,557 (year 1) to $6530 (year 2). The main drivers of MDS-related medical costs and the decrease in year 2 were chemotherapy and supportive care costs.
Conclusions
The economic burden of HR-MDS is considerable, particularly within the first year of diagnosis. Treatment/supportive care costs accounted for a significant portion of MDS-related costs. As HR-MDS treatment evolves, the economic impact and HCU need to be further investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The cost of care for higher-risk myelodysplastic syndrome (MDS) patients is high, and MDS-related chemotherapy and supportive care are the main drivers for this cost. |
Higher costs are incurred in the first year following diagnosis, mainly due to a decrease in MDS-related medical costs in the second year. However, costs in the second year of diagnosis are still high. |
1 Introduction
Myelodysplastic syndromes (MDS) are a group of heterogeneous, malignant bone marrow disorders characterized by ineffective hematopoiesis leading to disease-related complications and death [1]. Data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database (2007–2011) estimated the age-adjusted incidence to be 4.9 per 100,000 per year, and rates increase with increasing age, indicating that MDS is a disease of the elderly [2]. The incidence is 13.5 per 100,000 in those aged 65–69 years and 63.6 per 100,000 in those aged ≥ 85 years [2]. However, it has been documented that registries have underestimated the incidence of MDS due to underreporting and underdiagnosis; the estimated prevalence of MDS in the United States (US) is between 60,000 and 170,000 and is projected to grow [2].
The Revised International Prognostic Scoring System (IPSS-R) for MDS is used to determine the prognosis of patients diagnosed with MDS. IPSS-R classifies patients into five distinct risk categories (very low, low, intermediate, high, and very high) based on cytogenetics, bone marrow blast percentage, and depth of cytopenias at the time of diagnosis, with the median survival decreasing with increasing IPSS-R risk score [3]. Moreover, IPSS-R risk classification is used to largely guide treatment decisions; for patients with higher-risk MDS (HR-MDS, defined as an IPSS-R risk classification of intermediate risk or higher), the National Comprehensive Cancer Network (NCCN) recommends hypomethylating agents (HMAs) (e.g., azacitidine or decitabine) or a clinical trial for patients unable to undergo allogenic stem cell transplantation (alloSCT) [4]. For transplant-eligible HR-MDS patients, alloSCT alone or after either high-intensity chemotherapy (most commonly with an antimetabolite with or without an anthracycline) or chemotherapy with an HMA is recommended [4].
Healthcare utilization among patients with MDS is high. Patients often experience frequent and prolonged hospitalizations, frequent outpatient visits, and high costs [5]. The cost of treatment of MDS has been shown to be significantly higher in those patients receiving HMAs compared to patients who did not [6]. However, HMAs have demonstrated the ability to significantly reduce the transfusion burden in this patient population, which is also a substantial medical cost for patients with MDS [2, 7]. In fact, another retrospective claims analysis demonstrated that patients with MDS have a higher risk of emergency department (ED) visits and inpatient admissions during periods of follow-up when transfusions are administered versus during transfusion-free periods [8]. Both of the HMAs (i.e., azacitidine and decitabine) have been shown to be cost-effective options for the treatment of patients with HR-MDS, but azacitidine has been shown to be more cost-effective than decitabine in a recent analysis [9, 10]. This realization of cost effectiveness is likely due to both decreased transfusion dependence and fewer patients progressing to acute myeloid leukemia (AML) [10]. Overall, however, there are little data on current healthcare utilization and costs associated with treating HR-MDS in routine clinical practice. This study assessed the total healthcare costs and utilization of newly diagnosed HR-MDS patients.
2 Methods
2.1 Study Design and Data Source
This retrospective cohort study evaluated healthcare utilization and costs among treated HR-MDS patients using the Optum database. Optum is a large national administrative claims database in the US containing health plan data for more than 111 million patients with both commercial and Medicare enrollment information.
The study period spanned from January 1, 2008 to December 31, 2015, with enrollment occurring between January 1, 2008 and October 31, 2015. The index diagnosis date was the date of the first record of an MDS diagnosis, and the baseline period was defined as the 12-month period prior to the index diagnosis date. The follow-up period was at least 60 days from the index diagnosis date; however, patients who died within this 60-day period were followed for less than 60 days. Patients were followed until death, progression to AML (defined as at least one inpatient or outpatient International Classification of Diseases [ICD]-9 or ICD-10 diagnosis code occurring after initiation of first-line therapy for HR-MDS), end of continuous enrollment, or end of the study.
2.2 Selection of Participants
Newly diagnosed adult (≥ 18 years of age) patients who had at least one inpatient claim with a HR-MDS ICD-9 or ICD-10 diagnosis code (ICD-9 code 238.73; ICD-10 codes D46.20, D46.21, D46.22) or two or more outpatient claims with an MDS ICD-9 or ICD-10 diagnosis code with at least one of these coded as HR-MDS (the HR-MDS code had to either be the first code or within 14 days of the first code) were included in the study. Patients were also required to have continuous enrollment in medical and pharmacy benefits for 12 months in the baseline period and for at least 60 days in the follow-up period and evidence of MDS-related treatment with or without MDS-directed supportive care in the follow-up period. MDS-related treatment included stem cell transplant (SCT), azacitidine, decitabine, lenalidomide, cyclosporine, thalidomide, anti-thymocyte globulin, clofarabine, daunorubicin, idarubicin, cytarabine, fludarabine, and topotecan. MDS-directed supportive care included erythrocyte or platelet transfusions; thrombopoietin-, erythropoietin-, or granulocyte-stimulating agents; and hydroxyurea. Patients who had evidence of any chemotherapy or SCT in the baseline period or evidence of other primary cancers, metastatic disease, AML, or myelofibrosis in the baseline period were excluded.
2.3 Baseline Characteristics
Baseline demographic characteristics captured on the index diagnosis date included age, gender, geographic region, payer type, and index year. Baseline clinical characteristics, which included Charlson Comorbidity Index (CCI) score, presence of individual comorbidities comprising the CCI score (captured via ICD-9/ICD-10 coding), and use of MDS-directed supportive care at baseline, were recorded.
2.4 MDS-Related Treatment Characteristics
MDS-related treatment following MDS diagnosis was captured in the follow-up period. First-line therapy was defined as any MDS-related treatment initiated on or after the index diagnosis date. An addition or substitution of an MDS-related treatment 28 days after the start of the first-line therapy triggered a subsequent line of therapy. SCT received at any time during the follow-up period was also captured. Time to treatment initiation was defined as the time from index diagnosis date to the first evidence of chemotherapy, and duration of treatment was defined as the time from the start of the line of therapy to the end date for the line of therapy.
2.5 Study Outcomes
2.5.1 Healthcare Utilization and Healthcare Costs
MDS-related and non-MDS-related healthcare utilization, including erythrocyte or platelet transfusion episodes, and costs incurred from the index diagnosis date through to the end of follow-up and yearly following the index diagnosis date were evaluated. Healthcare utilization and costs were derived from medical and pharmacy claims in the Optum data. Medical services included inpatient admissions, ED visits, outpatient office visits, other outpatient visits, chemotherapy visits, supportive care visits, and transfusion episodes. Outpatient pharmacy services included outpatient prescription fills for medications. MDS-related healthcare utilization and costs included medical claims with a primary diagnosis of MDS or MDS-related treatment (i.e., MDS chemotherapy or MDS-directed supportive care) and pharmacy claims for MDS-related treatment. Transfusion episodes were defined as claims for transfusions with unique dates of service. Non-MDS-related healthcare utilization and costs included all other medical and pharmacy claims not categorized as MDS-related. Costs among those patients who progressed to AML or died post-first-line therapy for HR-MDS were also evaluated versus those who did not have evidence of progression to AML or death. Per-patient per-month (PPPM) costs were calculated and adjusted to 2015 US dollars [11], which was the last year of data capture. Patients with a capitated payment plan were excluded from this cost analysis.
2.6 Statistical Analysis
Descriptive statistics were used to describe demographics, baseline clinical characteristics, MDS-related treatment characteristics, healthcare utilization, and costs. Healthcare costs and the number of healthcare services in each setting of care were calculated as PPPM for the duration of the follow-up and each year of follow-up. PPPM costs or utilization were calculated as costs incurred or total number of services during the follow-up period divided by the duration of follow-up (in months) for each patient. Univariate analyses of frequencies and percentages were reported for categorical measures, while means, standard deviations (SDs), medians, and interquartile ranges (IQRs) were presented for continuous measures. Analyses were conducted using SAS® version 9.2 (SAS Institute; Cary, NC, USA).
3 Results
3.1 Demographics and Clinical Characteristics
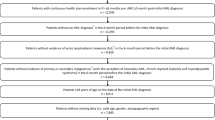
A total of 335 newly diagnosed patients with HR-MDS were identified; of these, 209 patients (62.4%) received MDS-related treatment following the index diagnosis date and were included in the analysis (Fig. 1). Of the 209 patients who received MDS-related treatment, as shown in Table 1, 61.2% were male and the mean age was 73 years (SD 10.1 years). The largest proportion of patients had a CCI score of ≥ 2 (42.1%), followed by a CCI score of 0 (29.7%) and of 1 (28.2%). The most common CCI comorbidities were diabetes (23.4%), moderate to severe renal disease (16.3%), congestive heart failure (16.3%), and diabetes with end-organ damage (8.1%). In the baseline period, 27.3% of patients received MDS-related supportive care and 24.9% of patients received transfusions.
Sample attrition. aDue to exclusion of patients with capitated claims for the cost analysis, 149 patients of the 209 treated HR-MDS patients were available for cost of care analyses. 1LT first-line therapy, AML acute myeloid leukemia, HR-MDS higher-risk myelodysplastic syndrome, MDS myelodysplastic syndrome, SCT stem cell transplant
3.2 MDS-related Treatment Characteristics
The median follow-up time for all treated patients was 9.9 months (IQR 4.6, 17.5). The median time to initiation of treatment following a diagnosis of MDS was 17 days (IQR 9, 35) (Table 2). The majority of patients received only one line of therapy over the duration of the follow-up period [first-line, 209 patients (100%); second-line, 30 patients (14.4%); third-line, six patients (2.9%)]. The median duration of therapy ranged from 4.4 months (IQR 2.2, 10.3) for the first-line to 2.2 months (IQR 1.3, 16.2) for the third-line. MDS-related treatment consisted mostly of HMAs (89.5% in the first-line; 63.3% in the second-line), and nearly all patients (90.5%) received MDS-directed supportive care during the follow-up period. Over the follow-up period, 38.8% (n = 81) of patients progressed to AML.
3.3 Healthcare Utilization
The number of patients evaluable for healthcare utilization decreased from 209 in year 1 to 92 in year 2. Over the entire follow-up period, the majority of patients had at least one outpatient physician office visit (MDS-related 82.3%; non-MDS-related 89.0%) and at least one other outpatient visit (MDS-related 96.2%; non-MDS-related 99.0%) (Table 3). On average, patients had 4.34 (SD 4.79) PPPM MDS-related outpatient physician visits and 3.24 (SD 3.53) PPPM other outpatient visits. There was also a mean of 2.47 (SD 3.00) non-MDS-related physician visits PPPM and 4.43 (SD 4.39) other outpatient visits PPPM.
Following diagnosis of MDS, the proportion of patients with at least one MDS-related physician and other outpatient visit decreased from year 1 (81.3% and 93.3%, respectively) to year 2 (72.8% and 73.9%, respectively). The proportion of patients with non-MDS-related physician office and other outpatient visits also decreased from year 1 (87.6% and 97.6%, respectively) to year 2 (75.0% and 90.2%, respectively). Further, the proportion of patients having a visit for MDS-related chemotherapy and MDS-directed supportive care treatment decreased from year 1 (87.1% and 78.5%, respectively) to year 2 (50.0% and 51.1%, respectively).
During the entire follow-up period, 69.4% of patients had at least one inpatient admission; 57.9% of patients had an MDS-related admission and 41.6% of patients had a non-MDS-related admission. The mean number of inpatient admission PPPM was 0.25 (SD 0.46), of which, 0.15 (SD 0.35) were MDS-related and 0.10 (SD 0.26) were non-MDS-related. The overall mean length of inpatient hospital stay was 1.97 days (SD 4.48) PPPM; 1.31 days (SD 2.91) were MDS-related and 0.66 days (SD 3.37) were non-MDS-related. The proportion of patients with both MDS- and non-MDS-related admissions also decreased by approximately 50% from year 1 (48.3% and 33.5%, respectively) to year 2 (23.9% and 18.5%, respectively).
MDS-related ED visits over the entire follow-up occurred in 56.9% of patients and were MDS-related in only 12% of the patients. Mean ED visits over the entire follow-up were 0.37 (SD 0.76) PPPM and were predominately non-MDS-related visits (0.33 [SD 0.69]) versus MDS-related visits (0.04 [SD 0.19]). From year 1 to year 2, the proportion of patients with MDS-related ED visits and non-MDS-related ED visits and the number of visits decreased.
Of the treated HR-MDS patients, 140 (67.0%) received at least one transfusion during the follow-up period. The mean number of transfusions was 3.38 (SD 5.07) PPPM. Of the 230 claims for transfusions recorded during the follow-up period, 46.5% were given in an outpatient setting, 33.5% were given in an inpatient setting, and 20.0% were given in the ED.
3.4 Healthcare Costs
Due to exclusion of patients with capitated claims, 149 patients were evaluable for cost analysis in year 1 and 62 patients in year 2. Over the entire follow-up period, the mean overall PPPM costs were $17,361 (SD $19,747), of which $10,839 (SD $11,101) were MDS-related and $6522 (SD $15,181) were non-MDS-related. Total costs were higher in year 1 [$17,337 (SD $19,696)] than in year 2 [$12,976 (SD $14,135)] following MDS diagnosis.
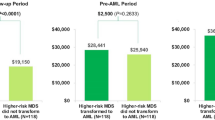
The majority of the overall costs of care was composed of medical costs as opposed to outpatient pharmacy costs. Average PPPM medical costs over the entire follow-up period were $16,451 (SD $19,203); between year 1 and year 2 following MDS diagnosis, PPPM medical costs decreased from $16,427 (SD $19,111) to $11,971 (SD $14,104). About 63% of the mean total PPPM costs over the follow-up period were for MDS-related medical services [$10,327 (SD $11,050)]. Between years 1 and 2 after MDS diagnosis, MDS-related medical PPPM costs decreased from $10,557 (SD $11,164) to $6530 (SD $7406) (Fig. 2). Costs associated with medical services for chemotherapy [$3161 PPPM (SD $2106)] and supportive care [$3700 PPPM (SD $9134)] were the main drivers of MDS-related medical costs, and these costs also decreased from year 1 [$3304 (SD $2157) and $3678 ($9174), respectively] to year 2 [$1880 (SD $2134) and $1652 ($2897)] following MDS diagnosis (Fig. 3a). The other main contributors of MDS-related costs were inpatient admissions [$1175 PPPM (SD $4670)] and other outpatient services [$1602 PPPM (SD $2281)] (Fig. 3a).
Non-MDS-related medical costs made up about 37% of overall medical costs ($6124 [SD $15,158]) and did not change significantly between year 1 and year 2 following MDS diagnosis. The primary contributors to non-MDS-related medical costs were inpatient admissions [$3729 (SD $14,003)] and outpatient services [$1817 PPPM (SD $2826)].
Of the 149 patients evaluable for cost analysis, 79 (53.0%) had evidence of progression to AML or death. The total cost over year 1 for those who progressed to AML or died was roughly twice that of those without evidence of progression or death (n = 70); mean PPPM total cost was $22,820 (SD $24,925) for those with progression to AML or death versus $11,148 (SD $7517) for those without progression or death in year 1. Both MDS-related and non-MDS-related medical costs within year 1 were higher for those who either progressed to AML or died [MDS-related $13,720 (SD $13,995) vs $6988 (SD $4779); non-MDS-related $8056 (SD $19,972) vs $3404 (SD $5102)] versus those who did not. Of the medical cost components, the most notable differences were in the cost of MDS-related supportive care [$5385 (SD $12,139) vs $1752 (SD $2618)], the cost of non-MDS-related inpatient visits [$5288 (SD $18,638) vs $1377 (SD $3910)], the cost of MDS-related inpatient visits [$1695 (SD $6219) vs $651 (SD $2392)], and the cost of MDS-related other outpatient visits [$2142 (SD $2895) vs $1082 (SD $1689)] for those who progressed or died versus those who did not.
4 Discussion
This study evaluated healthcare utilization and costs among treated HR-MDS patients in routine clinical practice and revealed that the healthcare burden associated with HR-MDS is considerable, particularly in the first year following diagnosis relative to the second year, across all settings of care. While overall costs PPPM were higher in the first year after diagnosis ($17,361 PPPM), costs PPPM remained high in the second year ($12,976 PPPM) following HR-MDS diagnosis. Over the entire follow-up period, 62% of the total costs were due to MDS-related care (64% in year 1 and 54% in year 2). Although MDS-related costs decreased from the first to the second year of diagnosis, non-MDS-related costs remained relatively similar. This same trend of decreasing cost of treated patients over time has been noted in multiple myeloma (MM) as well. In a retrospective study composed of 1181 patients with newly diagnosed MM, the total monthly cost for patients declined steadily, from $15,734 per month during the first quarter of therapy initiation to $5082 per month for the period starting 18 months after initiation of therapy [15]. In our patient population, the higher MDS-related costs in the first year following HR-MDS diagnosis were consistent with a larger proportion of patients receiving MDS-related chemotherapy and supportive care. The decrease in costs observed in the second year after diagnosis was mainly driven by the MDS diagnosis being captured in the first year’s costs and fewer patients receiving treatments. Further, it should be noted that the cost of progression to AML in this HR-MDS population was not evaluated, as follow-up ended upon transformation to AML. In our study, 38.8% of our population progressed to AML, and these patients, along with those who died, incurred higher costs in the first year after diagnosis relative to patients who did not have these events. For non-MDS-related medical costs, inpatient hospitalizations were the main cost driver, accounting for 60% of costs.
Studies evaluating the economic burden of HR-MDS patients are limited. The cost of drugs alone for lower-risk MDS was estimated at an average of $63,577 per patient annually [16]. In our analysis, HMAs were the most frequently utilized first-line therapy, with approximately 90% of patients receiving an HMA; of these, most patients (69%) received azacitidine. This aligns with both the NCCN guidelines and the primary literature, which show that azacitidine improves overall survival in trial-selected HR-MDS patients, while decitabine has not demonstrated a survival benefit [4, 12,13,14]. Further, the majority of patients in our analysis did not receive MDS-directed therapy beyond the first line, as transformations to AML and/or death were the predominant events that occurred during the follow-up period. A longitudinal analysis of elderly MDS patients utilizing the SEER database found that the 2-year cost from MDS diagnosis was higher in patients treated with HMAs versus those who did not receive HMAs [$92,102 vs $40,111, respectively (2009 US dollars)] [6]. Additionally, a retrospective analysis reviewing the use of transfusions and/or active therapy in MDS patients showed that patients were at highest risk for hospitalization when receiving both transfusions and active therapy [8]. However, neither of these previous studies accounted for IPSS-R risk category. Therefore, the results of this analysis add needed data regarding cost and healthcare utilization in an HR-MDS population.
MDS-related supportive care visits and costs were also higher in the first year of diagnosis compared to the second year of diagnosis. This result is slightly unexpected, as the use of HMAs is commonly associated with a decreased need for transfusions and supportive care, thereby leading to decreased costs [7, 17, 18].
4.1 Limitations
The limitations of this study include those inherent of any retrospective study. Clinical information is based on only diagnosis codes and is limited by corresponding caveats. All relevant characteristics cannot be captured by diagnosis codes, including, but not limited to, the true measure of high- or low-risk MDS. It is possible that using ICD-9 codes to identify the HR-MDS population may have resulted in a heterogeneous group of patients encompassing those with both very good and with unfavorable prognostic factors that may affect the study outcomes. In addition, healthcare utilization and costs following disease progression to AML, which occurred in 38.8% of this patient population, were not captured in this analysis. Also, the incremental costs and utilization due to HR-MDS relative to a similar population without cancer was not assessed. Finally, as with all cost analyses, how the value of currency changes over time may affect the results; however, it would be expected to impact all results in the same manner without bias.
5 Conclusions
Healthcare utilization and the associated medical costs in HR-MDS patients receiving treatment are high, with a cost of almost $18,000 PPPM. The medical costs associated with HR-MDS decreased from the first to the second year following HR-MDS diagnosis, coinciding with a decrease in healthcare utilization, in particular the administration of chemotherapy and supportive care. However, costs continued to remain high in the second year. As treatment of HR-MDS evolves, the economic impact and healthcare utilization need to be further investigated in this patient population.
Data Availability Statement
The data that support the findings of this study are available from Optum®, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, the authors can confirm that all relevant data are included in the article and/or its supplementary information files.
References
Komrokji RS. Current state of the art: management of higher risk myelodysplastic syndromes. Clin Lymphoma Myeloma Leuk. 2016;16(S1):S39–43.
Cogle CR. Incidence and burden of the myelodysplastic syndromes. Curr Hematol Malig Rep. 2015;10(3):272–81.
Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65.
National Comprehensive Cancer Network. Myelodysplastic syndromes. V.1.2018. Fort Washington. https://www.nccn.org/professionals/physician_gls/pdf/mds.pdf. Accessed 4 October 2017.
Powers A, Faria C, Broder MS, et al. Hematologic complications, healthcare utilization, and costs in commercially insured patients with myelodysplastic syndrome receiving supportive care. Am Health Drug Benefits. 2012;5(7):455–65.
Wang R, Gross CP, Frick K, et al. The impact of hypomethylating agents on the cost of care and survival of elderly patients with myelodysplastic syndromes. Leuk Res. 2012;36(11):1370–5.
Goldberg SL, Chen E, Sasane M, et al. Economic impact on US Medicare of a new diagnosis of myelodysplastic syndromes and the incremental costs associated with blood transfusion need. Transfusion. 2012;52(10):2131–8.
Smith BD, Mahmoud D, Dacosta-Byfield S, Rosen VM. Health care utilization and risk of infection and bleeding among patients with myelodysplastic syndromes with/without transfusions, and with/without active therapy. Leuk Lymphoma. 2014;55(5):1119–25.
Pan F, Peng S, Fleurence R, et al. Economic analysis of decitabine versus best supportive care in the treatment of intermediate- and high-risk myelodysplastic syndromes from a US payer perspective. Clin Ther. 2010;32(14):2444–56.
Gidwani R, Khan ZM, Fenaux P, et al. A cost-effectiveness analysis of using azacitidine vs. decitabine in treating patients with myelodysplastic syndromes. J Med Econ. 2012;15(1):145–54.
Bureau of Labor Statistics. CPI Inflation Calculator. 2018. https://www.bls.gov/data/inflation_calculator.htm. Accessed 9 Jul 2018.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32.
Kantarjian H, Issa JP, Rosenfeld CS, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794–803.
Lübbert M, Suciu S, Baila L, et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29(15):1987–96.
Arikian SR, Milentijevic D, Binder G, et al. Patterns of total cost and economic consequences of progression for patients with newly diagnosed multiple myeloma. Curr Med Res Opin. 2015;31(6):1105–15.
Greenberg PL, Cosler LE, Ferro SA, Lyman GH. The costs of drugs used to treat myelodysplastic syndromes following National Comprehensive Cancer Network Guidelines. J Natl Compr Canc Netw. 2008;6:942–53.
Harnan S, Ren S, Gomersall T, et al. Association between transfusion status and overall survival in patients with myelodysplastic syndromes: a systematic literature review and meta-analysis. Acta Haematol. 2016;136(1):23–42.
Frytak JR, Henk HJ, De Castro CM, et al. Estimation of economic costs associated with transfusion dependence in adults with MDS. Curr Med Res Opin. 2009;25(8):1941–51.
Acknowledgements
The authors would like to thank Dr. Megan Pollack for assistance in manuscript writing/development.
Author information
Authors and Affiliations
Contributions
All authors confirm that they have made substantial contributions to the intellectual content of the paper as described: concept and design of the study, analysis and interpretation of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. In addition, EF, HS, and AO conducted the statistical analysis.
Corresponding author
Ethics declarations
Funding
Funding for the research study and resultant publication was provided by Takeda.
Conflict of Interest
AG, JB, DF, and RF are employees of Takeda. HS, EF, MB, AO, and ME are employees of Xcenda, which has received research funding from Takeda for the conduct of this study and for the preparation of this manuscript.
Additional information
Millennium Pharmaceuticals, Inc., Cambridge, MA, USA: A wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bell, J.A., Galaznik, A., Blazer, M. et al. Economic Burden of Patients Treated for Higher-Risk Myelodysplastic Syndromes (HR-MDS) in Routine Clinical Care in the United States. PharmacoEconomics Open 3, 237–245 (2019). https://doi.org/10.1007/s41669-018-0100-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-018-0100-5