Abstract
Purpose
Evaluate the “in vitro” effect of the 660-nm laser on the inactivation of planktonic cells of Candida albicans, by the application of 660-nm diode laser light (1) on its own and (2) together with photodynamic therapy using methylene blue. We will also compare the ability of microbial inactivation of the laser over octenidine dihydrochloride disinfectant.
Methods
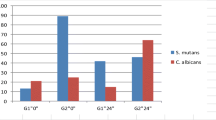
This study was conducted in a laminar flow cabinet with 4 groups, divided into two: no laser groups—C. albicans suspension in saline solution (Group 1) and C. albicans suspension, with octenidine dihydrochloride antimicrobial solution (Group 2); laser groups—C. albicans suspension, using a 660-nm diode laser with photodynamic therapy and methylene blue (Group 3), and C. albicans suspension, using a 660-nm diode laser without the presence of methylene blue as photosensitizer (PS) (Group 4). They were seeded in 96 wells where we applied laser light in different light conditions in order to get reliable results.
Results
The results of this study demonstrate that the application of a 660-nm laser, with and without the presence of a photosensitizer, showed microbial inhibition ability against Candida albicans. Photodynamic therapy using the methylene blue photosensitizer presented an antifungal effect against Candida albicans of 100% efficacy, similar to the results obtained with octenidine dihydrochloride.
Conclusions
The application of photodynamic therapy has demonstrated to be a good alternative, with an effective antifungal effect against Candida albicans, avoiding the side effects on patients, like those from octenidine dihydrochloride.


Similar content being viewed by others
References
Valentijn-Benz M, Nazmi K, Brand HS, van't Hof W, Veerman EC (2015) Growth of Candida albicans in human saliva is supported by low-molecular-mass compounds. FEMS Yeast Res 15(8):fov088. https://doi.org/10.1093/femsyr/fov088
Siqueira JF, Sen BH (2004) Fungi in endodontic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:632–641
Kumar J, Sharma R, Sharma M et al (2015) Presence of Candida albicans in root canals of teeth with apical periodontitis and evaluation of their possible role in failure of endodontic treatment. J Int Oral Health 7(2):42–45
Al-Ahmad A, Auschill TM, Dakhel R, Wittmer A, Pelz K, Heumann C, Hellwig E, Arweiler NB (2016) Prevalence of Candida albicans and Candida dubliniensis in caries-free and caries-active children in relation to the oral microbiota-a clinical study. Clin Oral Investig 20(8):1963–1971
Fouad AF (2009). Endodontic microbiology. Wiley. 368 p. ISBN 081380728X, 9780813807287
Waltimo S et al (2003) Yeasts in apical periodontitis. Crit Rev Oral Biol Med 14(2):128–137
Pappas PG, Rex JH, Lee J, Hamill RJ, Larsen RA, Powderly W, Kauffman CA, Hyslop N, Mangino JE, Chapman S, Horowitz HW, Edwards JE, Dismukes WE, NIAID Mycoses Study Group (2003) A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis 37:634–643
Koh AY, Kohler JR, Coggshall KT, Van Rooijen N, Pier GB (2008) Mucosal damage and neutropenia are required for Candida albicans dissemination. PLoS Pathog 4(2):35. https://doi.org/10.1371/journal.ppat.0040035
Al-Ahmad A, Auschill TM, Dakhel R, Wittmer A, Pelz K, Heumann C, Hellwig E, Arweiler NB (2016) Prevalence of Candida albicans and Candida dubliniensis in caries-free and caries-active children in relation to the oral microbiota-a clinical study. Clin Oral Investig 2016 20(8):1963–1971
Naglik JR, Fidel PL Jr, Odds FC (2008) Animal models of mucosal Candida infection. FEMS Microbiol Lett 283(2):129–139
de Sousa L et al (2015) Photoinactivation of Candida albicans using methylene blue as photosensitizer. RGO, Rev Gaúch Odontol, Porto Alegre 63(4):411–417
Queiroga AS et al (2011) In vitro photodynamic inactivation of Candida spp. by different doses of low power laser light. Photodiagnosis Photodyn Ther, Amsterdam 8(4):332–336
Swanson KM, Petran LR & Hanlin, JH (2001). Culture methods for enumeration of microorganisms https://doi.org/10.2105/9780875531755ch06
Chan Y, Lai CH (2003) Bactericidal effects of different laser wavelengths on periodontopathic germs in photodynamic therapy. Lasers Med Sci 18(1):51–55
Lee MT, Bird PS, Walsh LJ (2004) Photo activated disinfection of the root canal: a new role for lasers in endodontics. Aust Endod J 30(3):93–98
Gutknecht N, Moritz A, Conrads G, Lampert F (1997) Der Dioden laser und seine bakterizide Wirkung im Wurzelkanal - eine In-vitro-Studie. Endodontie 3:217–222
Donnelly RF, McCarron PA, Tunney MM (2008) Antifungal photodynamic therapy. Res Microbiol, Paris 163(1):1–12
Polansky R, Haas M, Heschl A, Wimmer G (2009) Clinical effectiveness of photodynamic therapy in the treatment of periodontitis. J Clin Periodontol 36(7):575–580
De Oliveira BP et al (2014) In vitro antimicrobial photoinactivation with methylene blue in different microorganisms. Braz J Oral Sci 13(1):53–57
Maisch T (2012) Photodynamic inactivation for controlling Candida albicans infections. Fungal Biology 116:1–10. https://doi.org/10.1016/j.funbio.2011.10.001
Gutknecht N, Van Betteray C, Ozturan S, Vanweersch L, Franzen R (2015) Laser supported reduction of specific microorganisms in the periodontal pocket with the aid of an Er,Cr:YSGG laser: a pilot study. Sci World J 450258. https://doi.org/10.1155/2015/450258
Gutknech N, Al-Karadaghi TS, Al-Maliky MA, Conrads G, Franzen R (2016) The bactericidal effect of 2780 and 940 nm laser irradiation on enterococcus faecalis in bovine root dentin slices of different thicknesses. Photomed Laser Surg 34(1):11–16. https://doi.org/10.1089/pho.2015.3960
Gutknecht N, van Gogswaardt D, Conrads G, Apel C, Schubert C, Lampert F (2000) Diode laser radiation and its bactericidal effect in root canal wall dentin. J Clin Laser Med Surg 18:57–60
Gutknecht N, Schippers M, Franzen R, Lampert F (2002) The bactericidal effect of a 980-nm diode laser in root canal wall dentin of bovine teeth. Lasers Med Sci 17:137–144
Franzen R, Gutknecht N, Falken S, Heussen N, Meister J (2011) Bactericidal effect of a Nd:YAG laser on Enterococcus faecalis at pulse durations of 15 and 25 ms in dentine depths of 500 and 1,000 μm. Lasers Med Sci 26(1):95–101. https://doi.org/10.1007/s10103-010-0826-5
Gouw-Soares S, Gutknecht N, Conrads G, Lampert F, Matson E, Eduardo CP (2000) The bactericidal effect of Ho:YAG laser irradiation within contaminated root dentinal samples. J Clin Laser Med Surg 18(2):81–87
Sadık B, Arıkan S, Beldüz N, Yaşa Y, Karasoy D, Cehreli M (2013) Effects of laser treatment on endodontic pathogen Enterococcus faecalis: a systematic review. Photomed Laser Surg 31(5):192–200. https://doi.org/10.1089/pho.2013.3479
Asnaashari M, Safavi N (2013) Application of low level lasers in dentistry (endodontic). J Lasers Med Sci Spring 4(2):57–66
Chiniforush N, Pourhajibagher M, Shahabi S, Bahador A (2015) Clinical approach of high technology techniques for control and elimination of endodontic microbiota. J Lasers Med Sci Fall 6(4):139–150. https://doi.org/10.15171/jlms.2015.09
Saydjari Y, Kuypers T, Gutknecht N (2016) Laser application in dentistry: irradiation effects of Nd:YAG 1064 nm and diode 810 nm and 980 nm in infected root canals-a literature overview. Biomed Res Int:8421656. https://doi.org/10.1155/2016/8421656
Asnaashari M, Godiny M, Azari-Marhabi S, Tabatabaei FS, Barati M (2016) Comparison of the antibacterial effect of 810 nm diode laser and photodynamic therapy in reducing the microbial Flora of root canal in endodontic retreatment in patients with Periradicular lesions. J Lasers Med Sci Spring 7(2):99–104. https://doi.org/10.15171/jlms.2016.17
Teichert MC, Jones JW, Usacheya MN, Biel MA (2002) Treatment of oral candidiasis with methylene blue-mediated photodynamic therapy in an immunodeficient murine model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93(2):155–160. https://doi.org/10.1067/moe.2002.120051
Kopnopka K, Goslinski T (2007) Photodynamic therapy in dentistry. J Dent Res 86(8):694–707. https://doi.org/10.1177/154405910708600803
Ryscova L, Buchta V, Slezak R (2010) Photodynamic antimicrobial therapy. Cent Eur J Biol, New York 5(4):400–406
Dai T, Fuchs BB, Coleman JJ, Prates RA, Astrakas C, St Denis TG, Ribeiro MS, Mylonakis E, Hamblin MR, Tegos GP (2012) Concepts and principles of photodynamic therapy as an alternative antifungal discovery platform. Front Microbiol 3:120
Kato TI, Prates RA, Sabino CP, Fuchs BB, Tegos G, Mylonakis E et al (2013) Antimicrobial photodynamic inactivation inhibits Candida albicans virulence factors and reduces in vivo pathogenicity. Antimicrob Agents Chemother 57(1):445–451. https://doi.org/10.1128/AAC.01451-12
De Souza SC, Junqueira JC, Balducci I, Koga-Ito CY, Munin E, Jorge AO (2006) Photosensitization of different Candida species by low power laser light. J Photochem Photobiol B 83(1):34–38
Peloi LS et al (2008) Photodynamic effect of light-emitting diode light on cell growth inhibition induced by methylene blue. J Biosci, Bangalore 32(2):231–237
Silva MJ et al (2011) Antimicrobial photodynamic therapy in rat experimental candidiasis: evaluation of pathogenicity factors of candida albicans. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, St Louis 111(1):71–77
Khan S et al (2012) Gold nanoparticles enhance methylene blue-induced photodynamic therapy: a novel therapeutic approach to inhibit Candida albicans biofilm. Int J Nanomed, Auckland 7:3245–3257
Pereira Gonzales F, Maisch T (2012) Photodynamic inactivation for controlling Candida albicans infections. Fungal Biol 116(1):1–10. https://doi.org/10.1016/j.funbio.2011.10.001
Soria-Lozano Y, Gilaberte MP, Paz-Cristobal L, Pérez-Artiaga V, Lampaya-Pérez J, Aporta V, Pérez-Laguna I, García-Luque MJ, Revillo A (2015) In vitro effect photodynamic therapy with differents photosensitizers on cariogenic microorganisms. BMC Microbiol 15:187
Giroldo LM, Felipe MP, De Oliveira MA, Munin E, Alves LP, Costa MS (2009) Photodynamic antimicrobial chemotherapy (PACT) with methylene blue increases membrane permeability in Candida albicans. Lasers Med Sci 24:109–112. https://doi.org/10.1007/s10103-007-0530-2
Castaño AP, Demidova TN, Hamblin MR (2004) Mechanisms in photodynamic therapy: part one: photosensitizers, photochemistry and cellular localization. Photodiagnosis photodyn ther Amsterdam 1(4):279–293
Eldeniz AU, Guneser MB, Akbulut MB (2015) Comparative antifungal efficacy of light-activated disinfection and octenidine hydrochloride with contemporary endodontic irrigants. Lasers Med Sci 30(2):669–675
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors (in vitro study).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martín Santiago, M.P., Gutknecht, N., Martín-Carrillo, N. et al. In vitro study of photodynamic therapy with visible laser systems applied to fungal infections. Laser Dent Sci 4, 103–110 (2020). https://doi.org/10.1007/s41547-020-00096-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-020-00096-6