Abstract
Workplace physical activity interventions in office-based settings are considered essential components of occupational health management, aimed at reducing sedentary behavior and its associated adverse effects, while also promoting employees’ health and wellbeing. This study investigates the effectiveness of office-yoga and walking on employees’ prevalence and intensity of musculoskeletal complaints (MSC), as well as on activation, which encompasses vitality and vigilance. Using a three-month longitudinal randomized controlled trial design, 459 office workers from five organizations were randomly assigned to either the office-yoga intervention group, the walking intervention group, or to a waitlist control group. Participants in the intervention groups were instructed to individually engage in brief daily sessions of the prescribed activity at the workplace. Those in the office-yoga group received video tutorials to perform the exercises. Self-reported MSC and activation were assessed weekly. Bayesian structural equation modeling revealed small effects of office-yoga (d = − 0.26) and walking (d = − 0.31) in reducing the prevalence of MSC as well as a program-based effectiveness of walking over office-yoga in reducing the intensity of MSC (d = 0.23). Concerning longitudinal trends, latent growth modeling revealed an intervention-based effectiveness for both office-yoga and walking on prevalence (doffice−yoga = − 0.32; dwalking = − 0.30) and intensity of MSC (doffice−yoga = − 0.42; dwalking = − 0.35). Neither intervention showed improvements in activation. We found no indication of adverse effects of either intervention. While both office-yoga and walking can effectively improve employees’ MSC, our findings suggest that walking is more effective in reducing intensity of MSC compared to office-yoga.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sedentary behavior is seen as a major risk factor for various physiological and psychological health complaints, including cardiovascular diseases (Owen et al., 2010), musculoskeletal complaints (MSC) in the neck, back, and shoulders (Côté et al., 2008b), and psychological distress (Hamer et al., 2014). Prolonged sitting has also emerged as an issue of particular interest in office-based contexts because office workers spend up to three-quarters of their workday engaged in sedentary, low-activity behavior (Parry & Straker, 2013; Prince et al., 2020), which, among other things, is considered to be responsible for poor health, absenteeism, and reduced productivity at work (Pieper et al., 2019). Hence, maintaining and promoting employees’ health is vital for organizations to ensure their performance and productivity. Considering this growing need to engage in occupational health management, it is crucial for organizations to invest in economically justifiable measures as they must use workplace interventions that are effective, economical, and easy to implement (Lutz et al., 2020).
Prolonged workplace sitting cannot be fully compensated by leisure time physical activity (Dunstan et al., 2012). Rather, addressing this issue, workplace physical activity interventions have been proposed as a promising approach within organizational health management since they incorporate physical activity as part of the daily work routine into the workday (e.g., Proper et al., 2003). Such interventions include for instance walking- or yoga-based interventions. Walking is considered an especially low-threshold health-promoting behavior and is among the most popular forms of physical activity (Lee & Buchner, 2008). Within organizational contexts, interventions promoting walking (e.g., through the implementation of pedometers; Aittasalo et al., 2012) have accordingly been implemented to counteract physical inactivity among employees and promote their health states (e.g., Gilson et al., 2009; Sitthipornvorakul et al., 2020). Yoga is a form of active exercise that involves physical posture exercises, controlled breathing techniques, relaxation, and meditation (Puerto-Valencia et al., 2019). Practicing yoga is considered a holistic “mind-body-intervention” (Chu et al., 2014, p. 235), as it incorporates physical as well as mental components. This approach to health promotion might offer benefits beyond those associated with interventions focusing solely on physical activity such as walking while still being low-threshold and easy to implement (Puerto-Valencia et al., 2019).
While meta-analytical evidence suggests that increasing physical activity at the workplace can increase employees’ health states (Moreira-Silva et al., 2016; Chu et al., 2014), two critical gaps remain within occupational health research that impede our understanding on intervention effectiveness. First, there is a lack of longitudinal high-quality trials regarding the number of measurement points (Bordado Sköld et al., 2019)—resulting in limited temporal resolution—and a lack of control groups not receiving any intervention (Abdin et al., 2018). The current study extends the previous lines of research by conducting a longitudinal RCT over the course of three months. This study design allows for examining temporal dynamics of health outcomes and differences in health trajectories across interventions. We aim to identify trends in the change of health outcomes to gain further insight into how change takes place over the course of workplace physical activity interventions.
Second, previous research has focused on single program studies with considerable heterogeneity in methodological approaches, workplaces, populations, and intervention components (e.g., Eisele-Metzger et al., 2023). Consequently, data do not allow to compare programs and research has failed to derive conclusive evidence (Proper et al., 2003) or clear recommendations what specific interventions are more beneficial (Pieper et al., 2019).
As part of this study, we intend to examine the effectiveness of office-yoga and walking in comparison to a waitlist control group, i.e., the intervention-based effectiveness. Furthermore, our design allows for an evaluation of the effectiveness of office-yoga in comparison with walking, i.e., the program-based effectiveness. Tackling the aforementioned research gap, the results of this research provide specific information to help select interventions that are most effective. This enables us to derive practical implications based on both the intervention-based and program-based effectiveness of office-yoga and walking.
Empirical Background and Hypotheses
Workplace physical activity interventions aim to reduce sedentary behavior and to increase employees’ physical activity and wellbeing within workplace settings. When implementing targeted interventions, there is usually a wide range of potential physical activities aimed at accomplishing the specific goal of decreasing sedentary behavior and promoting physical activity within occupational health management. For instance, one may integrate specific workstations, such as sit-stand workstations, treadmill workstations, or pedal machines, as examined in a systematic review by Commissaris and colleagues (2016). Another approach to enhance physical activity involves implementing exercise programs in the workplace, such as strength/endurance training, aerobic sessions, or group-based physiotherapy, as analyzed in a meta-analysis by Moreira-Silva and colleagues (2016). In this study, we examine and compare two particularly low-threshold and cost-efficient forms of workplace physical activity interventions, namely office-yoga and walking.
Walking is considered a dynamic physical activity (Morris & Hardman, 1997) of low to moderate intensity (i.e., between 2.3 metabolic equivalent units for very slow strolling and 4.8 metabolic equivalent units for walking for exercise; Herrmann et al., 2024). Walking has the advantage of being especially low-threshold in terms of accessibility (O’Connor et al., 2015) and requiring minimal effort from organizational perspectives (i.e., easy implementation, low costs; Brown et al., 2014). In comparison, yoga represents a holistic approach to health promotion, incorporating a mind-component going beyond exercise focusing solely on physical activity (Puerto-Valencia et al., 2019). Office-yoga in particular is a form of yoga practice based on classical hatha yoga, which is adapted to the conditions of the sedentary workplace environment. It represents a low-threshold workplace physical activity intervention of low to moderate intensity (i.e., between 2.3 metabolic equivalent units for yoga exercise videos and 2.5 metabolic equivalent units for Hatha yoga; Herrmann et al., 2024).
Empirical evidence derived from a systematic review conducted by Abdin and colleagues in 2018 indicates that workplace interventions utilizing yoga and walking may effectively enhance participants’ wellbeing. Additionally, wellbeing, as a multifaceted concept, encompasses various dimensions and can be defined as the equilibrium between an individual’s resources and the challenges they encounter (Dodge et al., 2012). Enhanced wellbeing could potentially provide individuals with the resources necessary to manage workplace and physical stressors, leading to reduced perception of MSC and increased activation. Nevertheless, the review highlights a lack of high-quality trials characterized by the absence of theoretical frameworks, placebo control conditions, evaluation of program-based effectiveness, and large sample sizes. Consequently, the authors could only conclude that engaging in some form of activity proves more beneficial than inactivity.
To address these issues, we aim to directly compare the effectiveness of an office-yoga and a walking intervention to derive conclusive results and evidence-based recommendations regarding the particular type of workplace physical activity interventions on MSC (i.e., prevalence and intensity) and activation (i.e., vitality and vigilance).
Musculoskeletal Complaints
Various characteristics of the modern workplace have been associated with adverse effects on the health of the musculoskeletal system and the occurrence of MSC in employees. MSC, which primarily include pain in the neck, shoulders, back, and upper extremities (for reference, see also Konradt et al., 2020) are a leading cause of work disability and absenteeism among the working population (Punnett & Wegman, 2004; Bevan, 2015) and are further associated with reduced work performance and productivity (Bevan, 2015).
Besides ergonomic factors like inadequate workstation design, frequent uninterrupted sitting at a desk with only occasional changes of posture has been found to burden musculoskeletal health and cause MSC (Côté et al., 2008a; Mayer et al., 2012). MSC stemming from sedentary behavior is vastly attributable to accumulating static load on the muscles during prolonged sitting (Bernard, 1997). Particularly computer work has been found to be associated with poor posture (i.e., neck flexion; Cagnie et al., 2007) that induces biomechanical strain. Breaking up prolonged periods of sitting by incorporating standing, walking, or any physical activity might help alleviate the static load and thereby perceived pain (Parry et al., 2019).
In a systematic review, Coury et al. (2009) found moderate to strong positive associations between physical activity and less MSC for employees in sedentary occupations. More precisely, O’Connor et al. (2015) provided meta-analytical evidence for the effectiveness of walking interventions in reducing MSC. Regarding neck pain specifically, Sitthipornvorakul and colleagues (2020) conducted an RCT demonstrating that a walking intervention could decrease the onset of neck pain among healthy office workers.
Yoga has been proposed as another effective means to reduce MSC including pain in the neck (Cramer et al., 2017) or lower back (Cramer et al., 2013). Its physiological benefits include the loosening of tight muscles and increased muscle strength, both of which have been associated with reduced muscle pain (Woodyard 2011). Beyond that, the meditative mind-components inherent to yoga practice might influence perceived pain by altered nociception (Villemure et al., 2014). Those meditative, relaxing components have been shown to down-regulate the sympathetic and to increase tonus in the parasympathetic nervous system, which is related to a reduced sensation of pain (La Forge, 1997). Accordingly, research indicates that meditation can effectively reduce MSC (Kabat-Zinn et al., 1985). Within occupational contexts, RCTs provided evidence that yoga-based interventions could improve flexibility in the back (Cheema et al., 2013) and reduce overall MSC (Telles et al., 2009). As yoga has been shown to be more effective in reducing neck pain than other physical activities like walking within a network meta-analysis on physical activity in general (Zoete et al., 2020), we also expect office-yoga to be more effective than walking as workplace physical activity interventions. Therefore, we hypothesize:
Hypothesis 1a
Employees assigned to a workplace physical activity intervention (i.e., office-yoga or walking) show a reduced prevalence and intensity of MSC after three months of intervention compared to employees not assigned to an intervention.
Hypothesis 1b
The office-yoga intervention is more effective in reducing prevalence and intensity of MSC after three months of intervention compared to the walking intervention.
Hypothesis 2a
Employees assigned to a workplace physical activity intervention (i.e., office-yoga or walking) show a negative trend in prevalence and intensity of MSC over the course of the intervention (i.e., decreasing prevalence and intensity of MSC over time) compared to employees not assigned to an intervention.
Hypothesis 2b
Employees assigned to the office-yoga intervention show a more pronounced negative trend in prevalence and intensity of MSC over the course of the intervention (i.e., more steeply decreasing prevalence and intensity of MSC over time) compared to employees assigned to the walking intervention.
Activation
While previous research on workplace health promotion has mainly focused on investigating its inhibiting effects on pathogenic physiological and mental outcomes such as MSC (Torp & Vinje, 2014), some have also examined potential salutogenic effects. Salutogenesis focuses on maintaining and promoting physiological and mental wellbeing, rather than solely preventing diseases (Mittelmark & Bauer, 2017).
Activation is a salutogenic outcome that is of particular interest within occupational health research (e.g., Konradt et al., 2022; Mailey et al., 2017). According to Hobi (1985), activation is a two-dimensional construct that comprises vitality and vigilance. Vitality refers to the physical and mental energy available to oneself and is characterized by a low level of fatigue and positive affective states (Ryan & Deci, 2008). Vigilance represents the state of one’s attentiveness and responsiveness (Oken et al., 2006). Accordingly, activation incorporates both physiological and mental components. Within occupational contexts, high levels of activation have been positively associated with work-related outcomes such as increased productivity and decreased absenteeism (e.g., Ryan & Deci, 2008; van Scheppingen et al., 2014).
Puetz and colleagues (2006) provided meta-analytical evidence that physical activity can increase feelings of energy and reduce perceived fatigue. The neurophysiological hypotheses can explain the connection between physical activity and states of activation. Through activation of the sympathetic nervous system, physical activity stimulates the release of monoamine neurotransmitters (especially serotonin, norepinephrine, and dopamine; Mikkelsen et al., 2017), which are linked to heightened levels of energy and lowered levels of fatigue (Stahl, 2002). In an RCT, Jakobsen et al. (2017) found that short workplace exercise sessions improved employees’ perceived vitality. Furthermore, evidence indicates that even low-intensity, short bouts of walking (10–15 min) can effectively increase perceived activation (Ekkekakis et al., 2000; Thøgersen-Ntoumani et al., 2014).
As theory suggests, the practice of yoga might be particularly effective in promoting activation, as the mental components of yoga specifically target the mental components of activation. For instance, yogic breathing and relaxation help to reduce specific aspects of general nervous system arousal (i.e., anxiety, restlessness; Brown & Gerbarg, 2009) associated with reduced overall vitality (Ryan & Frederick, 1997). Wood (1993) assumes that the combination of physical activity and conscious breathing inherent to yoga promotes activation.
According to this theoretical reasoning, a review by Ross and Thomas (2010) indicated that in pre-diseased populations yoga is as effective or even more effective than other forms of exercise like walking in terms of reducing fatigue. We therefore hypothesize:
Hypothesis 3a
Employees assigned to a workplace physical activity intervention (i.e., office-yoga or walking) show an improved vitality and vigilance after three months of intervention compared to employees not assigned to an intervention.
Hypothesis 3b
The office-yoga intervention is more effective in improving vitality and vigilance after three months of intervention compared to the walking intervention.
Hypothesis 4a
Employees assigned to a workplace physical activity intervention (i.e., office-yoga or walking) show a positive trend in vitality and vigilance over the course of the intervention (i.e., increasing vitality and vigilance over time) compared to employees not assigned to an intervention.
Hypothesis 4b
Employees assigned to the office-yoga intervention show a more pronounced positive trend in vitality and vigilance over the course of the intervention (i.e., more steeply increasing vitality and vigilance over time) compared to employees assigned to the walking intervention.
Method
Design
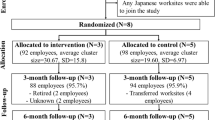
Within a multi-center, longitudinal randomized controlled trial over the course of three months, we compared two workplace physical activity intervention groups (i.e., office-yoga and walking) and a waitlist control group. We conducted 13 weekly self-assessment measures of physiological and psychological health parameters (T0 = baseline, preintervention; T1–T11 = during the intervention; T12 = at the end of the intervention). Because structural equation models involving all 13 time points (i.e., T0, T1,…, T12) exhibited convergence problems we used the data from all seven even timepoints including the baseline measurement (i.e., T0, T2,…, T12) for this study in order to reduce model complexity while preserving an equidistant measurement of variables.
Participants and Procedure
Participants in mostly sedentary occupations were recruited from five German white-collar organizations. Employees were informed about the study through their employer and could register via e-mail. Exclusion criteria included pregnancy or acute physiological or mental health complaints contradicting the practice of yoga or other physical activity (e.g., spinal diseases, psychotic disorder). Eligible participants were then randomly assigned to one of the three groups. All study questionnaires were administered online. To ensure anonymity, participants had to provide an individually generated code at each measurement point.
Prior to intervention onset (T0), baseline characteristics were assessed, including personal data and baseline measures of physiological and mental health parameters. Questionnaires were distributed weekly (T1–T12), assessing self-reported physiological and psychological health parameters as well as the adherence to the intervention (i.e., office-yoga or walking).
In total, 459 employees (18.8% male, Mage = 45.9, SDage =11.1) were subject to random allocation across three distinct study groups. This randomization process occurred within each organization, whereby upon conclusion of the registration phase within each organization, participants were randomly assigned to one of the three study groups. Consequently, individuals from all three study groups were represented within each of the five organizations, ensuring equitable distribution across organizational settings. Sample characteristics at T0 and T12 as well as an attrition analysis are presented in Table 1. The attrition analysis revealed no significant differences between participants who completed the measurements at T0 and T12. Furthermore, Table 2 shows the baseline sample characteristics of the five participating organizations respectively. Participants from two organizations (n = 246) completed the exercises during paid working hours, while the remaining (n = 213) completed the exercises during their break.
As compensation for participation participants could win one of twenty €50 vouchers. Furthermore, all study participants were given access to the office-yoga videos after the end of the study.
Intervention
Prior to intervention onset (T0), participants assigned to an intervention were given written information on the expected health benefits of practicing office-yoga or walking, respectively. To ensure comparability, participants not assigned to an intervention were given basic information on healthy sitting. With the beginning of the three-month study and intervention period, participants assigned to the office-yoga intervention were granted weekly access to 12 video tutorials instructing them on performing office-yoga exercises for 10 to 15 min. The video tutorials were produced in collaboration with a professional yoga teacher.
At the beginning of each week, participants were given access to an additional tutorial with the complexity of the exercises slightly increasing throughout the course of intervention. In addition to each video, they received a written video description. Participants were instructed to perform the yoga exercises around the middle of each workday. Participants assigned to the walking intervention were instructed to walk outside for about 10 to 15 min around the middle of each workday. Participants not assigned to an intervention were told to maintain their regular behavior at the workplace throughout the study period.
Measures
We conducted weekly assessments of self-reported physiological and psychological health parameters. Although self-reported data are potentially prone to recall and social desirability bias and their interpretation is hindered by the lack of normative data (Nicholas et al., 2008), we chose to record participants’ health status through self-report scales rather than objective scales for several reasons: Self-reported health is a subjective indicator that encompasses biological, psychological, social, and functional aspects of an individual’s health status (Wuorela et al., 2020). Hence, for instance, self-reports of pain provide the most accurate indicator of an individual’s subjective experience (Katz & Melzack, 1999). Second, self-reported health status has proven to be a valid predictor of objective all-cause mortality (Schnittker & Bacak, 2014). Within organizational contexts, self-reported health further serves as a more valid proxy for work-related outcomes such as work-absenteeism (Eriksen et al., 1999). Finally, the use of self-report measures is common in both pain research (Labus et al., 2003) and research focusing on wellbeing (Linton et al., 2016).
Musculoskeletal Complaints
We measured prevalence and intensity of MSC using six self-report items adapted from Stress Report Germany (Lohmann-Haislah, 2013). We asked participants how intensely and how often they had perceived pain in any of the following body regions on a working day over the past week: lower back, neck or shoulder area, arms or hands, hips, knees, and legs or feet. The intensity of MSC was assessed on a 5-point scale, ranging from 1 (no impairment) to 5 (very severe impairment). The prevalence of MSC was operationalized as the frequency of MSC in certain parts of the body and was assessed on a 5-point scale, ranging from 1 (never) to 5 (very often). In accordance with Lohmann-Haislah (2013), prevalence and intensity ratings for the individual body regions were aggregated to a mean score for both prevalence and intensity of MSC. We opted to assess the prevalence of MSC instead of its incidence because the interventions aim not only to prevent the onset of MSC but also to reduce existing or chronic MSC, i.e., reduce the number of occurrences of complaints throughout the intervention period. Since we used a formative scale to measure prevalence and intensity of MSC common measures of internal consistency such as Cronbach’s α are not applicable (Gruijters et al., 2021).
Activation
We assessed activation by vitality and vigilance each with four self-report items from the Basler Mental State Scale (Hobi, 1985). The 5-point semantic differential scale consisted of polar-opposite pairs of adjectives describing the experience of different levels of activation. Example items are “This week at work I felt (1) weakened vs. (5) strengthened” for vitality and “… (1) inattentive vs. (5) attentive” for vigilance, where higher values represent higher levels of activation. Cronbach’s α was 0.90 for vitality (averaged across all even time points T0, T2,…, T12; ranging between 0.84 and 0.93) and 0.94 for vigilance (averaged across all even time points T0, T2,…, T12; ranging between 0.91 and 0.96). Confirmatory factor analyses revealed a good fit of the dual factor model (i.e., one factor for vitality and one factor for vigilance) for all measurement points used within further analyses (i.e., all even measurement points).
Adherence
We assessed the weekly intervention adherence in the office-yoga and the walking group. We divided the self-reported number of days on which the participant executed the intervention activity by the number of days in the respective week on which the participant was working (i.e., the weekly working days minus vacation and sick days). Accordingly, the values range between 0 (representing no adherence in the respective week) and 1 (representing full adherence in the respective week). For participants participating in the office-yoga intervention, the mean intervention adherence was M = 0.57 (SD = 0.25) while for participants participating in the walking intervention the mean intervention adherence was M = 0.71 (SD = 0.22).
Data Analysis
The subset of collected data used in this study consisted of 120,717 data points, that is 459 participants times 263 observations (observations on outcome measures from all even time points including T0, baseline characteristics, and all variables used within sensitivity and supplementary analyses). In total, 30.57% of data points were missing values. To answer the hypotheses, we used Bayesian structural equational modeling (BSEM) technique within the software package Mplus (Version 8.10, Muthén & Muthén, 1998–2018).
Bayesian estimation offers advantages over frequentist methods like Maximum Likelihood Estimation (MLE). First, it does not depend heavily on large sample sizes for consistent estimates, unlike MLE (Asparouhov & Muthén, 2021b). Second, it enables the use of Credibility Intervals (CI), suitable for skewed and non-normal distributions, unlike MLE’s confidence intervals, which assume normality and symmetric distributions (Muthén, 2010). Therefore, Bayesian estimation avoids assumptions about data normality. Additionally, CIs are more straightforward to interpret, representing an interval with 90% probability of containing the population value (van de Schoot et al., 2014). Lastly, Bayesian Structural Equation Modeling (BSEM) prevents implausible estimates like negative variances or correlations outside − 1 and 1 bounds (van de Schoot et al., 2014), common in MLE when covariance matrix estimates become non-positive-semi-definite.
To estimate the BSEMs, we used the Markov Chain Monte Carlo (MCMC) algorithm with two chains with a minimum of 20,000 and a maximum of 100,000 iterations. The algorithm iteratively computes the posterior distributions of the parameters obtaining point estimates (Muthén, 2010). We opted for PX1 (simple parameter extended algorithm) settings for the MCMC algorithm, known for their superior mixing and fast convergence compared to alternative methods (Asparouhov, & Muthén, 2010). We did not thin the estimation since we did not require a large number of iterations for successful convergence (Muthén, 2010). Furthermore, we used default non-informative prior settings in Mplus (Asparouhov & Muthén, 2021b).
To assess model convergence, we checked the convergence criterion (see for reference Asparouhov & Muthén, 2010). Furthermore, we checked that the Potential Scale Reduction value does not bounce after further iterations of the algorithm which is recommended by Wang and Wang (2012).
Since our sample was large and contained a substantial amount of missing data, we followed suggestions by Asparouhov and Muthén (2021a) to assess model fit via approximate fit indices RMSEA, CFI, TLI. According to Hu and Bentler (1999) a good approximate fit is indicated by RMSEA < 0.06, CFI > 0.95, and TLI > 0.95.
To test Hypotheses 1 and 3, we utilized residualized change score models (RCS) as outlined by Castro-Schilo and Grimm (2018). Specifically, we simultaneously modeled the dichotomized group variable and outcome values measured at baseline (T0) as predictors for respective post-intervention outcome values (T12). By (auto-)regressing the outcome (T12) on its respective baseline value (T0) we were able to adjust for potential baseline differences in outcome values among groups while estimating the effect of the dichotomized group variable on post-intervention values of the outcome. Regressing the outcome on the dichotomized group variable represents a comparison of the effectiveness of the intervention regarding the specific outcome between two groups. We repeated this analysis three times, utilizing the dichotomized group variable to compare the control group with each intervention group separately (0 = control, 1 = walking/office-yoga, representing intervention-based effectiveness for Hypothesis a), and both intervention groups (0 = walking, 1 = office-yoga, representing program-based effectiveness for Hypothesis b). All outcome variables were assessed using latent single indicators of mean scores to reduce model complexity and to ensure model convergence.
For Hypotheses 2 and 4, we used latent growth curve models (LGMs). The statistical examination was twofold. First, we determined the functional form of the trajectory by testing for linear, quadratic, cubic, logistic, and gompertz trajectories (Cameron et al., 2015) to choose the best-fit model to perform subsequent analyses. We used the Bayesian Information Criterion (BIC) to compare model fits since it is a consistent criterion and applicable within a BSEM context (Neath & Cavanaugh, 2012). A smaller BIC indicates a better comparative fit, hence we chose the LGMs with the smallest BIC to model the trend for Hypotheses 2 and 4. To test the models we used the baseline score at T0 and all even time points (i.e., T2, T4,…, T12) to reduce model complexity. When running the models with all 13 time points some of the model-combinations did not achieve adequate fit or failed to converge within the limit of iterations set. We chose to use all even timepoints as this provides an equidistant (in terms of time) partition of the timepoints yielding evenly spaced indicators for the latent intercept and latent slope. We tested for every combination of walking/office-yoga with MSC (i.e., prevalence and intensity) and activation (i.e., vitality and vigilance), respectively. In all cases the linear trajectory turned out to be the one with the smallest BIC, hence we chose a linear LGM for further inference.
Second, we conducted three linear LGMs each to examine if the trend of improvements is dependent on the group (Hesser, 2015). We used data from two groups at once with the same dichotomous predictor variables for the latent slope of dependent variables as mentioned above.
For effect sizes, we calculated Cohen’s d and its 90% credibility intervals for Hypotheses 1 and 3 within the RCS models. For Hypotheses 2 and 4 we used the approach proposed by Feingold (2019) to estimate the effectsize GMA d (Growth Model Analysis d) and its 90% credibility interval within Mplus (see Appendix C3 in Feingold, 2019) to evaluate intervention effectiveness. We interpreted the effect sizes as small (> 0.2), medium (> 0.5), and large (> 0.8) according to Cohen (1977).
Results
Means, standard deviations, and bivariate correlations are presented in Table 3.
Hypothesis 1a which predicted a reduced prevalence and intensity of MSC for employees assigned to a workplace physical activity intervention after three months of intervention compared to those not assigned to an intervention was partially supported. Among employees assigned to an intervention, we observed reduced prevalence of MSC relative to non-recipients (doffice−yoga = − 0.26, PSD = 0.12, 90% CI [− 0.45, − 0.06]; dwalking = − 0.31, PSD = 0.12, 90% CI [− 0.51, − 0.13]). However, only employees assigned to the walking intervention showed beneficial effects on intensity of MSC (dwalking = − 0.36, PSD = 0.13, 90% CI [− 0.56, − 0.15]). We found no support for Hypothesis 1b which postulated that the office-yoga intervention is more effective in reducing prevalence and intensity of MSC than the walking intervention. On the contrary, the effect for intensity of MSC (d = 0.23, PSD = 0.14 90% CI [+ 0.00, 0.46]) indicates a superiority of walking over office-yoga. Estimates for MSC outcomes at T12 regressed on the group variable as well as estimates for autoregressive paths (outcome at T12 regressed on respective outcome T0), and model fit indices of respective models are presented in Table 4 for all group comparisons.
Hypothesis 2a which predicted a negative trend in prevalence and intensity of MSC over the course of the intervention for employees assigned to a workplace physical activity intervention compared to those not assigned to an intervention was supported. Both interventions exhibited a more pronounced negative trend in prevalence (GMA doffice−yoga = − 0.32, PSD = 0.19, 90% CI [− 0.63, − 0.01]; GMA dwalking = − 0.30, PSD = 0.17, 90% CI [− 0.58, − 0.04]) and intensity of MSC (GMA doffice−yoga = − 0.42, PSD = 0.22, 90% CI [− 0.79, − 0.07]; GMA dwalking = − 0.35, PSD = 0.17, 90% CI [− 0.63, − 0.08]) compared to employees not assigned to an intervention. However, we found no support for Hypothesis 2b which postulated a more pronounced negative trend in prevalence and intensity of MSC over the course of the intervention for employees assigned to the office-yoga intervention compared to those assigned to the walking intervention. Estimates and model fit indices are presented in Table 5.
Hypothesis 3a that predicted an improved vitality and vigilance for employees assigned to a workplace physical activity intervention after three months of intervention compared to those not assigned to an intervention was not supported. We found no beneficial effects for employees assigned to an intervention on vitality and vigilance after the intervention compared to employees not assigned to an intervention. Furthermore, there were no differences in the activation between employees who were assigned to the office-yoga intervention compared to those who were assigned to the walking intervention indicating no support for Hypothesis 3b. Table 6 presents estimates for vitality and vigilance outcomes at T12 regressed on the group variable as well as estimates for autoregressive paths (outcome at T12 regressed on the respective outcome T0) for all group comparisons, and model fit indices of respective models.
We did not find differences in trends in vitality or vigilance for either intervention, hence Hypotheses 4a and 4b were not supported (see Table 7 for estimates and model fit indices).
Sensitivity Analyses
We conducted several sensitivity analyses to gain insight into the robustness of our findings. We identified six factors that could potentially confound our results. First, our sample exhibited an imbalance in terms of gender, with the majority of participants being women. Research revealed differences between women and men regarding the prevalence and sensation of pain—both being elevated in women (Afridi et al., 2021)—as well as regarding adherence to worksite health promotion programs with women generally showing higher adherence to treatment (Robroek et al., 2009). Second, the effectiveness of our intervention could be confounded by concurrent physical activity, i.e., physical activity performed in addition to the intervention plan (for the intervention groups) or during the intervention period (for the waitlist control group). To address this potential bias, we collected data on concurrent sporting activity (in hours per week), concurrent walking activity not included in the intervention plan (in hours per week), as well as concurrent yoga activity not included in the intervention plan (in hours per week). Third, as we provided information on the anticipated health benefits of their respective activities to participants (i.e., office-yoga or walking), the expectation regarding intervention utility might act as a confounding variable when collecting self-report measures. We evaluated this expectation using four items on a 5-point Likert scale adapted from Christophersen and Konradt (2011). Finally, we assessed whether participants had prior experience with yoga practice (0 = no experience, 1 = prior experience).
After identifying those potential confounding variables, we included them as predictors of outcomes in RCS models and LGM models, respectively. The sole significant finding was that concurrent sporting activity negatively predicted the trend of MSC. However, when incorporating concurrent sporting activity into the respective models used for Hypotheses 3a and 3b, the initial significance pattern remained unchanged.
Supplementary Analyses
To deepen the understanding of our results, we conducted three supplementary analyses. First, results regarding the functional form of the trajectories revealed that for every LGM used in Hypotheses 2 and 4 a positive linear trend was present. This indicates that for employees assigned to any intervention (i.e., office-yoga and walking) prevalence and intensity of MSC and activation (i.e., vitality and vigilance) improved over the course of three months.
Second, we accounted for a potential dose-response effect. Our investigation centered on whether intervention adherence serves as a predicting factor in the trend of MSC and activation. Consequently, we integrated the latent intercept of adherence (computed at T2, T4,…, T12) as a predictor of the latent slopes utilized to examine Hypotheses 2 and 4 for the office-yoga and walking group, respectively. The pattern of results was inconsistent. Concerning MSC, we only observed a dose-response effect for walking and prevalence of MSC (β = −0.42, PSD = 0.23, p =.035). In terms of activation, we found a positive dose-response effect for office-yoga and the trend of both vitality and vigilance (βvitality = 0.55, PSD = 0.16, p =.001; βvigilance = 0.40, PSD = 0.20, p =.026). However, we did not find such a dose-response effect for walking and the trend of activation. All model fits were excellent.
Third, to test for potential adverse intervention effects, we conducted a mixture latent curve analysis that allows for differences in growth parameters across different unobserved subpopulations. The 1-class model showed the best fit to the data, which indicates no different groups within our sample. Thus, neither intervention had any adverse effects on employees’ health and wellbeing.
Discussion
The purpose of this study was to examine and compare the effectiveness of two low-threshold workplace physical activity interventions—specifically office-yoga and walking —on self-reported employees’ health outcomes (i.e., MSC and activation). We addressed this question using a longitudinal, three-armed, multicentric RCT over the course of three months with office-based workers. The key findings of this study were (1) employees assigned to an office-yoga or a walking intervention both showed reduced prevalence of MSC while those assigned to the walking intervention also showed a reduced intensity of MSC. Effect sizes were small indicating (limited) intervention-based effectiveness of the interventions; (2) employees assigned to the walking intervention showed a reduced intensity of MSC compared to those assigned to the office-yoga intervention indicating a program-based effectiveness of walking over office-yoga in reducing intensity of MSC; (3) the positive trend of both prevalence and intensity of MSC was more pronounced—with effect sizes being small—for employees assigned to the office-yoga or the walking intervention than for those not assigned to an intervention with no differences in trends when comparing office-yoga and walking directly, indicating (limited) intervention-based effectiveness of both interventions with neither being superior over the other; and (4) no intervention affected activation thus no effectiveness of office-yoga and walking to increase activation is indicated.
We provided evidence on the effectiveness of office-yoga and walking in reducing MSC (limited for intensity of MSC), demonstrating beneficial effects even for short bouts of light intensity activity integrated within the workday. To our knowledge this is the first study to directly compare the effectiveness of two low-threshold workplace physical activity interventions, namely office-yoga and walking, in promoting employees’ subjective health. In doing so, we did not find a program-based effectiveness of office-yoga when compared to walking. Indeed, walking showed a program-based superiority over office-yoga, indicating that the mind-component inherent to yoga practice did not provide an additional benefit regarding the reduction of perceived musculoskeletal pain. This unexpected finding may be attributed to the contextual factors, primarily the environmental settings of the interventions. While the walking intervention took place outside of the workplace environment, the office-yoga sessions were conducted within the direct environment of the workplace. This distinction may have inhibited the office-yoga participants’ ability to mentally disengage from work-related stressors during the intervention and enter a meditative state (Kabat-Zinn, 1982), potentially impacting the intervention’s effectiveness in altering nociception (Villemure et al., 2014). Furthermore, the environmental conditions inherent in outdoor walking, such as exposure to natural light and fresh air, could have played a significant role in modulating participants’ pain perception given the associations between exposure to greenspaces and physiological and mental wellbeing (Twohig-Bennett & Jones, 2018; Bowler et al., 2010). This difference in environmental conditions of the interventions might have contributed to a reduced perception of intensity of MSC for employees assigned to the walking intervention compared to those assigned to the office-yoga intervention.
Taken together, we cannot make any explicit recommendation for implementing holistic approaches like office-yoga in contrast to more reduced interventions involving physical activity components only. This finding is particularly important for organizations that have to implement workplace interventions that are as cost-effective as possible (Lutz et al., 2020). Despite the aforementioned, we do not advise against office-yoga at the workplace either, since we found no indication of adverse effects of office-yoga. Although the lack of comparative effectiveness over walking, office-yoga can be a useful means for organizations to promote employees’ health when other forms of physical activities such as walking are not applicable (i.e., due to missing infrastructure, time management, or other organizational reasons). We advocate future research to explore variations of yoga-based workplace physical activity interventions within diverse contextual settings to optimize intervention strategies for reducing musculoskeletal complaints in sedentary employees.
We found no indication of beneficial effects for employees’ activation as a salutogenic health parameter incorporating physiological and mental components when assigned to the office-yoga or the walking intervention. Results indicate that neither the physical activity components in the walking intervention nor the additional mental components inherent to office-yoga were sufficient to effectively target employees’ vitality and vigilance states. Hence, we did not find evidence that previous results (Ross & Thomas, 2010) on pre-diseased populations can be generalized to a healthy population in a workplace setting. However, we cannot rule out that office-yoga is a useful addition to occupational health management when it comes to promoting activation in a subpopulation of employees who are predisposed to poor health. Furthermore, there was a positive trend for both interventions regarding activation indicating no harmful effects on activation.
Our findings remained robust even after controlling for various potentially confounding variables. There was no evidence suggesting that concurrent activities such as yoga, walking, or sports influenced the results regarding the interventions’ effectiveness. Nevertheless, participants engaging in higher levels of concurrent sporting activities exhibited a more pronounced negative trend in MSC. Despite encountering a skewed gender distribution in our sample and a generally heightened pain sensitivity among women (Afridi et al., 2021), we did not observe a gender bias in our results. This indicates similar effectiveness across genders. Additionally, our analyses demonstrate that office-yoga exhibits intervention-based effectiveness, irrespective of prior expectations regarding its utility and individuals’ prior familiarity with yoga. Consequently, it emerges as an easily accessible tool within occupational health management.
Contrary to our expectations, we did not observe a conclusive pattern when examining the relationship between average intervention adherence and the trends in MSC and activation over a three-month period. We identified a dose-response effect solely among participants in the office-yoga group, affecting their vitality and vigilance, and among those in the walking group, impacting their MSC prevalence. Given the dose-response principle of workplace interventions (Garber et al., 2011), an intervention must be carried out with sufficient frequency to achieve the intended effects. Research indicates that various intrapersonal, interpersonal, and institutional factors are involved in predicting adherence to workplace health interventions including for example active support of intervention participation in the team and by superiors (Linnan et al., 2001). Our findings suggest that increasing adherence through proactive support may contribute to fostering a positive activation trend. However, due to inconclusive results regarding MSC, advocating for active support alone to ensure or enhance intervention effectiveness is not warranted.
Finally, we identified the functional form of the trajectories of MSC and activation over the intervention period of three months. Our results indicate linear trends of both MSC and activation for both interventions suggesting consistent improvement over time without evidence of fade-out effects or deterioration within this timeframe. While accordingly the timeframe of three months seems to be a reliable benchmark for intervention implementation, this linear trajectory might not persist over longer durations, as demonstrated by previous research showing fade-out of positive intervention effects over extended intervention periods (Konradt et al., 2020, 2022). The examination of larger timeframes may unveil different functional forms of trajectories, such as quadratic or cubic, which were not discernible within our study. This methodological perspective should be taken into consideration when choosing a sampling frame (i.e., the sampling interval and rate) within longitudinal research. Although we initially aimed to enhance data resolution by including 13 measurement points, the decision to use only even measurement points in our analyses was primarily driven by challenges in achieving model convergence and adequate fit. While our decision to reduce the number of measurement points may limit the granularity of our analyses, it still allowed us to investigate different trajectories of health changes in extended timeframes compared to previous research on occupational health, that seldomly included two measurement points or was limited to relatively short timeframes (Bordado Sköld et al., 2019). Nevertheless, we propose future research to consider not only different time frames (i.e., longer sampling intervals, different sampling rates, follow-up measurements) but also different methodological approaches like person-specific techniques such as ambulatory assessment methodology (Hofmans et al., 2019) and time series analyses to enhance our understanding of temporal dynamics and individual variations in response to health interventions.
Limitations and Future Research
There are, admittedly, four main limitations to the current study. First, we performed randomization procedures on an individual-level rather than applying methods of cluster randomization based on organizations as units of randomization. Hence, we cannot rule out the risk of contamination between study groups within each organization. Even though contamination might diminish estimations of intervention effectiveness and might result in the failure to detect an existing effect (Howe et al., 2007), at the same sample size, cluster RCTs are less efficient and have less statistical power due to the lack of independence within clusters (Donner et al., 2000). As our outcomes at interest were measured at an individual-level (i.e., participants’ individual health status), we aimed to avoid bias by introducing intervention delivery at cluster-level (Donner & Klar, 2004) and to minimize the risk of baseline imbalances of potential confounders often occurring in cluster RCTs (Ivers et al., 2012). Finally, individual-based randomization was chosen due to the practical reason to heighten the organizational stakeholders’ willingness to participate in the study.
Second, our study is limited to subjective data regarding both the assessed health outcomes and intervention adherence. Regarding individuals’ health status, our findings still provide valuable information, since self-reported perceptions of health status can in fact capture the impact on individual functioning more effectively than objective measures (Punnett & Wegman, 2004). Further, there is a lack of explicitly objective and quantifiable measures for (musculoskeletal) pain (Shekhar et al., 2023) and activation due to the subjective nature of the constructs. The development of objective measurement methods as well as their application within occupational health research should be object to future research. Nevertheless, we still encourage future researchers to complement subjective self-report measures of health status with measures of objective outcomes that might serve as proxies for musculoskeletal health (e.g., muscle strength or flexibility, e.g., Moreira et al., 2021) or activation (e.g., reaction time or concentration, e.g., Schwartz et al., 2019; Laux & Corazza, 2019) to further support findings based on self-report measures. Moreover, our evaluation of MSC frequency was restricted to self-reported prevalence. Subsequent research should therefore include the incidence of MSC and explore whether interventions can effectively prevent the occurrence of complaints. Addressing the lack of objective data on intervention adherence, incorporating objective measures (e.g., using accelerometers; Dunstan et al., 2012) in future research would allow for a more fine-grained and reliable examination of the associations between adherence to workplace physical activity and health promotion.
Third, the participants demonstrated rather low levels of health complaints at baseline (i.e., low prevalence and intensity of MSC, high vitality and vigilance). While such population-based research heightens the external validity of our results, our interventions might have yielded more pronounced effects when delivered to at-risk populations. Meta-analytical evidence (Robroek et al., 2020) showed that workplace health promotion interventions differed in their effectiveness based on the target population with interventions delivered to at-risk populations being more effective. Accordingly, future research should investigate the comparative effectiveness of workplace physical activity interventions targeting different samples (i.e., particularly at-risk, predisposed to poor health) to determine whether to tailor interventions solely to specific subgroups of employees (Conn et al., 2009). In addition, we advocate future research to address potential confounding, person-related variables of pain medication. The intake of pain medication could influence participants’ perception of pain and thus MSC (for review see Afridi et al., 2021), potentially biasing results regarding the intervention effectiveness in reducing perceived prevalence and intensity of MSC.
Finally, future research should aim to identify (psychological) mechanisms that are predictive of intervention adherence as well as overall intervention effectiveness. While to date, most studies within organizational health research have not moved beyond evaluating the overall effectiveness of interventions (Nielsen & Miraglia 2017), future research should investigate factors that give rise to (positive) change in health parameters and serve as determinants of the adherence to and the effectiveness of workplace physical activity interventions, thereby contributing to the understanding of when and why workplace physical activity interventions are (most) effective. This would help to improve the timing and maintenance of interventions. As Konradt and colleagues (2022) found that the initial velocity (i.e., rate of change) and acceleration (i.e., rate of rate of change) of health changes in individuals had some predictive value regarding the effectiveness of a sit-stand desk intervention, it might be a promising approach to further investigate such temporal dynamics for yoga- and walking-based workplace physical activity interventions as well.
Conclusion
Workplace physical activity interventions play an integral role in improving employees’ health and wellbeing by aiming at reducing risk factors and adverse effects of prolonged times spent sitting or at low energy expenditure at the workplace. We have demonstrated that the low-threshold and easy to implement interventions of office-yoga and walking improve the MSC of employees over the course of three months of intervention. In comparing the effectiveness of both interventions, we further found a relative superiority of walking over office-yoga (i.e., program-based effectiveness of walking) on the intensity of MSC. While we found no improvements in activation over the course of the intervention there were no detrimental effects present. Thus, office-yoga and walking can be valuable and cost-efficient addendums to organizations’ occupational health management. In sum, we provided substantial field-experimental evidence incorporating the examination of program-based effectiveness of office-yoga and walking on employees’ health and wellbeing contributing to the literature on workplace physical activity interventions.
Data Availability
The data and codes are available on reasonable request from the corresponding author at nath(at)psychologie.uni-kiel.com.
References
Abdin, S., Welch, R. K., Byron-Daniel, J., & Meyrick, J. (2018). The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health, 160, 70–76. https://doi.org/10.1016/j.puhe.2018.03.029.
Afridi, B., Khan, H., Akkol, E. K., & Aschner, M. (2021). Pain perception and management: Where do we stand? Current Molecular Pharmacology, 14(5), 678–688. https://doi.org/10.2174/1874467213666200611142438.
Aittasalo, M., Rinne, M., Pasanen, M., Kukkonen-Harjula, K., & Vasankari, T. (2012). Promoting walking among office employees - evaluation of a randomized controlled intervention with pedometers and e-mail messages. Bmc Public Health, 12(1), 403. https://doi.org/10.1186/1471-2458-12-403.
Asparouhov, T., & Muthén, B. (2010). Bayesian analysis using Mplus: Technical implementation. Technical Report, Version 3. http://statmodel.com/download/Bayes3.pdf.
Asparouhov, T., & Muthén, B. (2021a). Advances in bayesian model fit evaluation for structural equation models. Structural Equation Modeling, 28(1), 1–14. https://doi.org/10.1080/10705511.2020.1764360.
Asparouhov, T., & Muthén, B. (2021b). Bayesian analysis of latent variable models using Mplus. Version 5. https://www.statmodel.com/download/BayesAdvantages18.pdf.
Bernard, B. P. (Ed.). (1997). Musculoskeletal disorders and workplace factors: A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. U.S. Department of Health and Human Services NIOSH. https://doi.org/10.26616/nioshpub97141.
Bevan, S. (2015). Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Practice & Research Clinical Rheumatology, 29(3), 356–373. https://doi.org/10.1016/j.berh.2015.08.002.
Bordado Sköld, M., Bayattork, M., Andersen, L. L., & Schlünssen, V. (2019). Psychosocial effects of workplace exercise–A systematic review. Scandinavian Journal of Work Environment & Health, 45(6), 533–545. https://doi.org/10.5271/sjweh.3832.
Bowler, D. E., Buyung-Ali, L. M., Knight, T. M., & Pullin, A. S. (2010). A systematic review of evidence for the added benefits to health of exposure to natural environments. Bmc Public Health, 10, 1–10. https://doi.org/10.1186/1471-2458-10-456.
Brown, R. P., & Gerbarg, P. L. (2009). Yoga breathing, meditation, and longevity. Annals of the New York Academy of Sciences, 1172(1), 54–62. https://doi.org/10.1111/j.1749-6632.2009.04394.x.
Brown, D. K., Barton, J. L., Pretty, J., & Gladwell, V. F. (2014). Walks4Work: Assessing the role of the natural environment in a workplace physical activity intervention. Scandinavian Journal of Work Environment & Health, 40(4), 390–399. https://doi.org/10.5271/sjweh.3421.
Cagnie, B., Danneels, L., van Tiggelen, D., de Loose, V., & Cambier, D. (2007). Individual and work related risk factors for neck pain among office workers: A cross sectional study. European Spine Journal, 16(5), 679–686. https://doi.org/10.1007/s00586-006-0269-7.
Cameron, C. E., Grimm, K. J., Steele, J. S., Castro-Schilo, L., & Grissmer, D. W. (2015). Nonlinear Gompertz curve models of achievement gaps in mathematics and reading. Journal of Educational Psychology, 107(3), 789–804. https://doi.org/10.1037/edu0000009.
Castro-Schilo, L., & Grimm, K. J. (2018). Using residualized change versus difference scores for longitudinal research. Journal of Social and Personal Relationships, 35(1), 32–58. https://doi.org/10.1177/0265407517718387.
Cheema, B. S., Houridis, A., Busch, L., Raschke-Cheema, V., Melville, G. W., Marshall, P. W., Chang, D., Machliss, B., Lonsdale, C., Bowman, J., & Colagiuri, B. (2013). Effect of an office worksite-based yoga program on heart rate variability: Outcomes of a randomized controlled trial. BMC Complementary and Alternative Medicine, 13(1), 1–10. https://doi.org/10.1186/1472-6882-13-82.
Christophersen, T., & Konradt, U. (2011). Development and validation of a formative and a reflective measure for the assessment of online store usability. Behaviour & Information Technology,31(9), 839–857. https://doi.org/10.1080/0144929X.2010.529165
Chu, A. H. Y., Koh, D., Moy, F. M., & Müller-Riemenschneider, F. (2014). Do workplace physical activity interventions improve mental health outcomes? Occupational Medicine, 64(4), 235–245. https://doi.org/10.1093/occmed/kqu045.
Cohen, J. (1977). Statistical power analysis for the behavioral sciences (Revised edition). Academic Press.
Commissaris, D. A. C. M., Huysmans, M. A., Mathiassen, S. E., Srinivasan, D., Koppes, L. L. J., & Hendriksen, I. J. M. (2016). Interventions to reduce sedentary behavior and increase physical activity during productive work: A systematic review. Scandinavian Journal of Work Environment & Health, 42(3), 181–191. https://doi.org/10.5271/sjweh.3544.
Conn, V. S., Hafdahl, A. R., Cooper, P. S., Brown, L. M., & Lusk, S. L. (2009). Meta-analysis of workplace physical activity interventions. American Journal of Preventive Medicine, 37(4), 330–339. https://doi.org/10.1016/j.amepre.2009.06.008.
Côté, P., Kristman, V., Vidmar, M., van Eerd, D., Hogg-Johnson, S., Beaton, D., & Smith, P. M. (2008a). The prevalence and incidence of work absenteeism involving neck pain. European Spine Journal, 17(S1), 192–198. https://doi.org/10.1007/s00586-008-0636-7.
Côté, P., van der Velde, G., Cassidy, J. D., Carroll, L. J., Hogg-Johnson, S., Holm, L. W., Guzman, J., Haldemann, S., Carragee, E. J., Hurwitz, E., Nordin, L., M., & Peloso, P. M. (2008b). The burden and determinants of neck pain in workers: Results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Journal of Manipulative and Physiological Therapeutics, 32(2), 70–86. https://doi.org/10.1007/s00586-008-0626-9.
Coury, H. J. C. G., Moreira, R. F. C., & Dias, N. B. (2009). Evaluation of the effectiveness of workplace exercise in controlling neck, shoulder and low back pain: A systematic review. Brazilian Journal of Physical Therapy, 13(6), 461–479. https://doi.org/10.1590/S1413-35552009000600002.
Cramer, H., Lauche, R., Haller, H., & Dobos, G. (2013). A systematic review and meta-analysis of yoga for low back pain. The Clinical Journal of Pain, 29(5), 450–460. https://doi.org/10.1097/AJP.0b013e31825e1492.
Cramer, H., Klose, P., Brinkhaus, B., Michalsen, A., & Dobos, G. (2017). Effects of yoga on chronic neck pain: A systematic review and meta-analysis. Clinical Rehabilitation, 31(11), 1457–1465. https://doi.org/10.1177/0269215517698735.
de Zoete, R. M., Armfield, N. R., McAuley, J. H., Chen, K., & Sterling, M. (2020). Comparative effectiveness of physical exercise interventions for chronic non-specific neck pain: A systematic review with network meta-analysis of 40 randomised controlled trials. British Journal of Sports Medicine, 55(13), 730–742. https://doi.org/10.1136/bjsports-2020-102664.
Dodge, R., Daly, A., Huyton, J., & Sanders, L. (2012). The challenge of defining wellbeing. International Journal of Wellbeing, 2(3), 222–235. https://doi.org/10.5502/ijw.v2i3.4.
Donner, A., & Klar, N. (2004). Pitfalls of and controversies in cluster randomization trials. American Journal of Public Health, 94(3), 416–422. https://doi.org/10.2105/ajph.94.3.416.
Donner, A., Klar, N., & Klar, N. S. (2000). Design and analysis of cluster randomization trials in health research, 27. Arnold.
Dunstan, D. W., Howard, B., Healy, G. N., & Owen, N. (2012). Too much sitting– a health hazard. Diabetes Research and Clinical Practice, 97(3), 368–376. https://doi.org/10.1016/j.diabres.2012.05.020.
Eisele-Metzger, A., Schoser, D. S., Klein, M. D., Grummich, K., Schwarzer, G., Schwingshackl, L., Hermann, R., Biallas, B., Wilke, C., Meerpohl, J. J., & Braun, C. (2023). Interventions for preventing back pain among office workers–A systematic review and network meta-analysis. Scandinavian Journal of Work Environment & Health, 49(1), 5–22. https://doi.org/10.5271/sjweh.4070.
Ekkekakis, P., Hall, E. E., VanLanduyt, L. M., & Petruzzello, S. J. (2000). Walking in (affective) circles: Can short walks enhance affect? Journal of Behavioral Medicine, 23(3), 245–275. https://doi.org/10.1023/A:1005558025163.
Eriksen, H. R., Ihlebæk, C., & Ursin, H. (1999). A scoring system for subjective health complaints (SHC). Scandinavian Journal of Public Health, 27(1), 63–72. https://doi.org/10.1177/14034948990270010401.
Feingold, A. (2019). New approaches for estimation of effect sizes and their confidence intervals for treatment effects from randomized controlled trials. The Quantitative Methods for Psychology, 15(2), 96–111. https://doi.org/10.20982/tqmp.15.2.p096.
Garber, C. E., Blissmer, B., Deschenes, M. R., Franklin, B. A., Lamonte, M. J., Lee, I. M., Nieman, D. C., & Swain, D. P. (2011). Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Medicine and Science in Sports and Exercise, 43(7), 1334–1359. https://doi.org/10.1249/MSS.0b013e318213fefb.
Gilson, N. D., Puig-Ribera, A., McKenna, J., Brown, W. J., Burton, N. W., & Cooke, C. B. (2009). Do walking strategies to increase physical activity reduce reported sitting in workplaces: A randomized control trial. International Journal of Behavioral Nutrition and Physical Activity, 6(1), 43. https://doi.org/10.1186/1479-5868-6-43.
Gruijters, S. L. K., Fleuren, B. P. I., & Peters, G. J. Y. (2021). Crossing the seven cs of internal consistency: Assessing the reliability of formative instruments. PsyArXiv. https://doi.org/10.31234/osf.io/qar39.
Hamer, M., Coombs, N., & Stamatakis, E. (2014). Associations between objectively assessed and self-reported sedentary time with mental health in adults: An analysis of data from the Health Survey for England. BMJ open, 4(3), 004580. https://doi.org/10.1136/bmjopen-2013-004580. Article e.
Herrmann, S. D., Willis, E. A., & Ainsworth, B. E. (2024). The 2024 Compendium of Physical activities and its expansion. Journal of Sport and Health Science, 13(1), 1–2. https://doi.org/10.1016/j.jshs.2023.09.008.
Hesser, H. (2015). Modeling individual differences in randomized experiments using growth models: Recommendations for design, statistical analysis and reporting of results of internet interventions. Internet Interventions, 2(2), 110–120. https://doi.org/10.1016/j.invent.2015.02.003.
Hobi, V. (1985). Basler Befindlichkeits-Skala [Basel Mental State Scale]. Beltz.
Hofmans, J., De Clercq, B., Kuppens, P., Verbeke, L., & Widiger, T. A. (2019). Testing the structure and process of personality using ambulatory assessment data: An overview of within-person and person-specific techniques. Psychological Assessment, 31(4), 432–443. https://doi.org/10.1037/pas0000562.
Howe, A., Keogh-Brown, M., Miles, S., & Bachmann, M. (2007). Expert consensus on contamination in educational trials elicited by a Delphi exercise. Medical Education, 41(2), 196–204. https://doi.org/10.1111/j.1365-2929.2006.02674.x.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Ivers, N. M., Halperin, I. J., Barnsley, J., Grimshaw, J. M., Shah, B. R., Tu, K., Upshur, R., & Zwarenstein, M. (2012). Allocation techniques for balance at baseline in cluster randomized trials: A methodological review. Trials, 13, 1–9. https://doi.org/10.1186/1745-6215-13-120.
Jakobsen, M. D., Sundstrup, E., Brandt, M., & Andersen, L. L. (2017). Psychosocial benefits of workplace physical exercise: Cluster randomized controlled trial. Bmc Public Health, 17(798). https://doi.org/10.1186/s12889-017-4728-3.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. https://doi.org/10.1016/0163-8343(82)90026-3.
Kabat-Zinn, J., Lipworth, L., & Burney, R. (1985). The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8(2), 163–190. https://doi.org/10.1007/BF00845519.
Katz, J., & Melzack, R. (1999). Measurement of pain. Surgical Clinics of North America, 79(2), 231–252. https://doi.org/10.1016/S0039-6109(05)70381-9.
Konradt, U., Heblich, F., Krys, S., Garbers, Y., & Otte, K. P. (2020). Beneficial, adverse, and spiraling health-promotion effects: Evidence from a longitudinal randomized controlled trial of working at sit–stand desks. Journal of Occupational Health Psychology, 25(1), 68–81. https://doi.org/10.1037/ocp0000161.
Konradt, U., Nath, A., Krys, S., & Heblich, F. (2022). Longitudinal effects of a sit-stand desk intervention-persistence, fade-out, and psychological momentum: A randomized controlled trial. BMC Psychology, 10(1), 1–13. https://doi.org/10.1186/s40359-022-00948-9.
La Forge, R. (1997). Mind-body fitness: Encouraging prospects for primary and secondary prevention. Journal of Cardiovascular Nursing, 11(3), 53–65. https://doi.org/10.1097/00005082-199704000-00006.
Labus, J. S., Keefe, F. J., & Jensen, M. P. (2003). Self-reports of pain intensity and direct observations of pain behavior: When are they correlated? Pain, 102(1–2), 109–124. https://doi.org/10.1016/s0304-3959(02)00354-8.
Laux, R. C., & Corazza, S. T. (2019). Improvement of reaction time after a workplace physical activity intervention. Revista Brasileira De Medicina do Esporte, 25, 515–519. https://doi.org/10.1590/1517-869220192506191493.
Lee, I. M., & Buchner, D. M. (2008). The importance of walking to public health. Medicine & Science in Sports & Exercise, 40(7), 512–518. https://doi.org/10.1249/mss.0b013e31817c65d0.
Linnan, L. A., Sorensen, G., Colditz, G., Klar, D. N., & Emmons, K. M. (2001). Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 28(5), 591–607. https://doi.org/10.1177/109019810102800506.
Linton, M. J., Dieppe, P., & Medina-Lara, A. (2016). Review of 99 self-report measures for assessing well-being in adults: Exploring dimensions of well-being and developments over time. BMJ open, 6(7), e010641. https://doi.org/10.1136/bmjopen-2015-010641.
Lohmann-Haislah, A. (2013). Stressreport Deutschland 2012. Psychische Anforderungen, Ressourcen und Befinden. Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. https://www.baua.de/DE/Angebote/Publikationen/Berichte/Gd68.pdf.
Lutz, N., Clarys, P., Koenig, I., Deliens, T., Taeymans, J., & Verhaeghe, N. (2020). Health economic evaluations of interventions to increase physical activity and decrease sedentary behavior at the workplace: A systematic review. Scandinavian Journal of Work Environment & Health, 46(2), 127–142. https://doi.org/10.5271/sjweh.3871.
Mailey, E. L., Rosenkranz, S. K., Ablah, E., Swank, A., & Casey, K. (2017). Effects of an intervention to reduce sitting at work on arousal, fatigue, and mood among sedentary female employees. Journal of Occupational and Environmental Medicine, 59(12), 1166–1171. https://doi.org/10.1097/JOM.0000000000001131.
Mayer, J., Kraus, T., & Ochsmann, E. (2012). Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: A systematic review. International Archives of Occupational and Environmental Health, 85(6), 587–603. https://doi.org/10.1007/s00420-011-0701-0.
Mikkelsen, K., Stojanovska, L., Polenakovic, M., Bosevski, M., & Apostolopoulos, V. (2017). Exercise and mental health. Maturitas, 106, 48–56. https://doi.org/10.1016/j.maturitas.2017.09.003.
Mittelmark, M. B., & Bauer, G. F. (2017). The Meanings of Salutogenesis. In M. Mittelmark, S. Sagy, M. Eriksson, G. F. Bauer, J. M. Pelikan, B. Lindström, & G. A. Espnes (Eds.), The Handbook of Salutogenesis (pp. 7–13). Springer. https://doi.org/10.1007/978-3-319-04600-6_2.
Moreira, R. F. C., Moriguchi, C. S., Carnaz, L., Foltran, F. A., Silva, L. C. C. B., & Coury, H. J. C. G. (2021). Effects of a workplace exercise program on physical capacity and lower back symptoms in hospital nursing assistants: A randomized controlled trial. International Archives of Occupational and Environmental Health, 94(2), 275–284. https://doi.org/10.1007/s00420-020-01572-z.
Moreira-Silva, I., Teixeira, P. M., Santos, R., Abreu, S., Moreira, C., & Mota, J. (2016). The effects of workplace physical activity programs on musculoskeletal pain: A systematic review and meta-analysis. Workplace Health & Safety, 64(5), 210–222. https://doi.org/10.1177/2165079916629688.
Morris, J. N., & Hardman, A. E. (1997). Walking to health. Sports Medicine, 23(5), 306–332. https://doi.org/10.2165/00007256-199723050-00004.
Muthén, B. O. (2010). Bayesian analysis in Mplus: A brief introduction. Incomplete Draft, Version 2https://www.statmodel.com/download/IntroBayesVersion%202.pdf.
Muthén, L. K., & Muthén, B. O. (1998–2018). Mplus User´s Guide. Eighth Edition. Muthén & Muthén.
Neath, A. A., & Cavanaugh, J. E. (2012). The bayesian information criterion: Background, derivation, and applications. Wiley Interdisciplinary Reviews: Computational Statistics, 4(2), 199–203. https://doi.org/10.1002/wics.199
Nicholas, M. K., Asghari, A., & Blyth, F. M. (2008). What do the numbers mean? Normative data in chronic pain measures. Pain, 134(1–2), 158–173. https://doi.org/10.1016/j.pain.2007.04.007.
Nielsen, K., & Miraglia, M. (2017). What works for whom in which circumstances? On the need to move beyond the ‘what works?’ Question in organizational intervention research. Human Relations, 70(1), 40–62. https://doi.org/10.1177/0018726716670226.
O’Connor, S. R., Tully, M. A., Ryan, B., Bleakley, C. M., Baxter, G. D., Bradley, J. M., & McDonough, S. M. (2015). Walking exercise for chronic musculoskeletal pain: Systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation, 96(4), 724–734e3. https://doi.org/10.1016/j.apmr.2014.12.003.
Oken, B. S., Salinsky, M. C., & Elsas, S. M. (2006). Vigilance, alertness, or sustained attention: Physiological basis and measurement. Clinical Neurophysiology, 117(9), 1885–1901. https://doi.org/10.1016/j.clinph.2006.01.017.
Owen, N., Healy, G. N., Matthews, C. E., & Dunstan, D. W. (2010). Too much sitting: The population-health science of sedentary behavior. Exercise and Sport Sciences Reviews, 38(3), 105–113. https://doi.org/10.1097/JES.0b013e3181e373a2.
Parry, S. P., & Straker, L. M. (2013). The contribution of office work to sedentary behaviour associated risk. Bmc Public Health, 13(1), 1–10. https://doi.org/10.1186/1471-2458-13-296.
Parry, S. P., Coenen, P., Shrestha, N., O’Sullivan, P. B., Maher, C. G., & Straker, L. M. (2019). Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. The Cochrane Database of Systematic Reviews, 2019(11). https://doi.org/10.1002/14651858.CD012487.pub2.
Pieper, C., Schröer, S., & Eilerts, A. L. (2019). Evidence of workplace interventions - a systematic review of systematic reviews. International Journal of Environmental Research and Public Health, 16(19), 3553. https://doi.org/10.3390/ijerph16193553.
Prince, S. A., Roberts, K. C., Reed, J. L., Biswas, A., Colley, R. C., & Thompson, W. (2020). Daily physical activity and sedentary behaviour across occupational classifications in Canadian adults. Health Reports, 31(9), 11–26. https://doi.org/10.25318/82-003-x202000900002-eng.
Proper, K. I., Koning, M., van der Beek, A. J., Hildebrandt, V. H., Bosscher, R. J., & van Mechelen, W. (2003). The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clinical Journal of Sport Medicine, 13(2), 106–117. https://doi.org/10.1097/00042752-200303000-00008.
Puerto-Valencia, L. M., Weber, A., Spegel, H., Bögle, R., Selmani, A., Heinze, S., & Herr, C. (2019). Yoga in the workplace and health outcomes: A systematic review. Occupational Medicine, 69(3), 195–203. https://doi.org/10.1093/occmed/kqz033.
Puetz, T. W., O’Connor, P. J., & Dishman, R. K. (2006). Effects of chronic exercise on feelings of energy and fatigue: A quantitative synthesis. Psychological Bulletin, 132(6), 866–876. https://doi.org/10.1037/0033-2909.132.6.866.
Punnett, L., & Wegman, D. H. (2004). Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. Journal of Electromyography and Kinesiology, 14(1), 13–23. https://doi.org/10.1016/j.jelekin.2003.09.015.
Robroek, S. J., Van Lenthe, F. J., Van Empelen, P., & Burdorf, A. (2009). Determinants of participation in worksite health promotion programmes: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 6, 1–12. https://doi.org/10.1186/1479-5868-6-26.
Robroek, S. J., Oude Hengel, K. M., van der Beek, A. J., Boot, C. R., van Lenthe, F. J., Burdorf, A., & Coenen, P. (2020). Socio-economic inequalities in the effectiveness of workplace health promotion programmes on body mass index: An individual participant data meta‐analysis. Obesity Reviews, 21(11). https://doi.org/10.1111/obr.13101. Article e13101.
Ross, A., & Thomas, S. (2010). The health benefits of yoga and exercise: A review of comparison studies. The Journal of Alternative and Complementary Medicine, 16, 3–12. https://doi.org/10.1089/acm.2009.0044.
Ryan, R. M., & Deci, E. L. (2008). From ego depletion to vitality: Theory and findings concerning the facilitation of energy available to the self. Social and Personality Psychology Compass, 2(2), 702–717. https://doi.org/10.1111/j.1751-9004.2008.00098.x.
Ryan, R. M., & Frederick, C. (1997). On energy, personality, and health: Subjective vitality as a dynamic reflection of well-being. Journal of Personality, 65(3), 529–565. https://doi.org/10.1111/j.1467-6494.1997.tb00326.x.
Schnittker, J., & Bacak, V. (2014). The increasing predictive validity of self-rated health. Plos One, 9(1). https://doi.org/10.1371/journal.pone.0084933. Article e84933.
Schwartz, B., Kapellusch, J. M., Baca, A., & Wessner, B. (2019). Medium-term effects of a two-desk sit/stand workstation on cognitive performance and workload for healthy people performing sedentary work: A secondary analysis of a randomised controlled trial. Ergonomics, 62(6), 794–810. https://doi.org/10.1080/00140139.2019.1577497.
Shekhar, V., Choudhary, N., Rathore, P., Singh, S. P., & Bhatnagar, S. (2023). Non-invasive objective markers to measure pain: A direction to develop a pain device-a narrative review. Indian Journal of Palliative Care, 29(2), 217–222. https://doi.org/10.25259/IJPC_257_2022.
Sitthipornvorakul, E., Sihawong, R., Waongenngarm, P., & Janwantanakul, P. (2020). The effects of walking intervention on preventing neck pain in office workers: A randomized controlled trial. Journal of Occupational Health, 62(1), e12106. https://doi.org/10.1002/1348-9585.12106.
Stahl, S. M. (2002). The psychopharmacology of energy and fatigue. The Journal of Clinical Psychiatry, 63(1), 7–8. https://doi.org/10.4088/jcp.v63n0102.
Telles, S., Dash, M., & Naveen, K. V. (2009). Effect of yoga on musculoskeletal discomfort and motor functions in professional computer users. Work (Reading, Mass.), 33(3), 297–306. https://doi.org/10.3233/WOR-2009-0877.
Thøgersen-Ntoumani, C., Loughren, E. A., Taylor, I. M., Duda, J. L., & Fox, K. R. (2014). A step in the right direction? Change in mental well-being and self-reported work performance among physically inactive university employees during a walking intervention. Mental Health and Physical Activity, 7(2), 89–94. https://doi.org/10.1016/j.mhpa.2014.06.004.
Torp, S., & Vinje, H. F. (2014). Is workplace health promotion research in the nordic countries really on the right track? Scandinavian Journal of Public Health, 42(15_suppl), 74–81. https://doi.org/10.1177/1403494814545106.
Twohig-Bennett, C., & Jones, A. (2018). The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental Research, 166, 628–637. https://doi.org/10.1016/j.envres.2018.06.030.
van de Schoot, R., Kaplan, D., Denissen, J., Asendorpf, J. B., Neyer, F. J., & van Aken, M. A. G. (2014). A gentle introduction to bayesian analysis: Applications to developmental research. Child Development, 85(3), 842–860. https://doi.org/10.1111/cdev.12169.
van Scheppingen, A. R., de Vroome, E. M. M., Have, K. C. J. M., ten, Zwetsloot, G. I. J. M., Bos, E. H., & van Mechelen, W. (2014). Motivations for health and their associations with lifestyle, work style, health, vitality, and employee productivity. Journal of Occupational and Environmental Medicine, 56(5), 540–546. https://doi.org/10.1097/jom.0000000000000143.
Villemure, C., Ceko, M., Cotton, V. A., & Bushnell, M. C. (2014). Insular cortex mediates increased pain tolerance in yoga practitioners. Cerebral Cortex, 24(10), 2732–2740. https://doi.org/10.1093/cercor/bht124.
Wang, J., & Wang, X. (2012). Structural equation modeling: Applications using Mplus. Wiley. https://doi.org/10.1002/9781118356258.
Wood, C. (1993). Mood change and perceptions of vitality: A comparison of the effects of relaxation, visualization and yoga. Journal of the Royal Society of Medicine, 86, 254–258. https://doi.org/10.1177/014107689308600504.
Woodyard, C. (2011). Exploring the therapeutic effects of yoga and its ability to increase quality of life. International Journal of Yoga, 4(2), 49–54.
Wuorela, M., Lavonius, S., Salminen, M., Vahlberg, T., Viitanen, M., & Viikari, L. (2020). Self-rated health and objective health status as predictors of all-cause mortality among older people: A prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatrics, 20, 1–7. https://doi.org/10.1186/s12877-020-01516-9.
Acknowledgements
We thank Kristin Dahlhaus for providing help with the production of the office-yoga videos. We further thank Gesa Lücke for her help on data acquisition.
Funding
The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
A.N. is responsible for the study conception and design. A.N. and S.S. were responsible for acquisition of the data. A.N. analyzed the data and U.K. contributed to the supplementary analyses. S.S. provided the tables and figures. All authors were involved in the interpretation of the data. The first draft of the manuscript was written by A.N. and S.S. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Kiel University (Date 31.05.2022/No ZEK-13/22).
Consent to Participate
Informed consent was obtained from all individuals included in the study.
Consent for Publication
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nath, A., Schimmelpfennig, S. & Konradt, U. Effects of Office-Yoga and Walking at the Workplace to Improve Health and Wellbeing: A Longitudinal Randomized Controlled Trial. Occup Health Sci (2024). https://doi.org/10.1007/s41542-024-00194-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41542-024-00194-y