Abstract
Ischemic stroke is one of the leading causes of death worldwide, and effective treatment strategies in the chronic phase of this disease remain insufficient. Homeostasis of metals in the brain plays an important role in maintaining normal brain function. However, the dynamic spatial distributions of iron, zinc, calcium, potassium, and copper in a rat brain following ischemic stroke and the association between structural distribution and function remain to be elucidated. In this study, we used a synchrotron radiation-based micro-X-ray fluorescence technique to image element mapping changes in special rat brain regions after ischemic stroke, showing the distribution characteristics of iron, zinc, calcium, potassium, and copper. We demonstrated, for the first time, the consistent dynamic spatial distributions of metal elements at a series of time points (3 h, 4.5 h, 6 h, 12 h, 1 d, 3 d, 5 d, 7 d, 10 d, 14 d, 28 d) after brain ischemia, which revealed that the homeostasis of iron, zinc, calcium, potassium, and copper in the brain was disturbed with distinctive change trends, providing clear insights in understanding the underlying pathogenesis of stroke from a novel perspective, thus laying the foundation of further developing new drug targets for stroke treatment.






Similar content being viewed by others
References
J.F. Collingwood, F. Adams, Chemical imaging analysis of the brain with X-ray methods. Spectrochim. Acta. B 130, 101–118 (2017). https://doi.org/10.1016/j.sab.2017.02.013
E.L. Que, D.W. Domaille, C.J. Chang, Metals in neurobiology: probing their chemistry and biology with molecular imaging (vol 108, pg 1517, 2008). Chem. Rev. 108(10), 4328 (2008). https://doi.org/10.1021/cr800447y
H. Wang, M. Wang, B. Wang et al., Immunogold labeling and X-ray fluorescence microscopy reveal enrichment ratios of Cu and Zn, metabolism of APP and amyloid-beta plaque formation in a mouse model of Alzheimer’s disease. Metallomics 4(10), 1113–1118 (2012). https://doi.org/10.1039/c2mt20056b
H. Wang, M. Wang, B. Wang et al., The distribution profile and oxidation states of biometals in APP transgenic mouse brain: dyshomeostasis with age and as a function of the development of Alzheimer’s disease. Metallomics 4(3), 289–296 (2012). https://doi.org/10.1039/c2mt00104g
H.-J. Wang, M. Wang, B. Wang et al., Quantitative imaging of element spatial distribution in the brain section of a mouse model of Alzheimer’s disease using synchrotron radiation X-ray fluorescence analysis. J. Anal. Atom. Spectrom. 25(3), 328–333 (2010). https://doi.org/10.1039/b921201a
P. Zatta, D. Drago, P. Zambenedetti et al., Accumulation of copper and other metal ions, and metallothionein I/II expression in the bovine brain as a function of aging. J. Chem. Neuroanat. 36(1), 1–5 (2008). https://doi.org/10.1016/j.jchemneu.2008.02.008
G. Robison, T. Zakharova, S. Fu et al., X-ray fluorescence imaging of the hippocampal formation after manganese exposure. Metallomics 5(11), 1554–1565 (2013). https://doi.org/10.1039/c3mt00133d
V.L. Dressler, E.I. Müller, D. Pozebon, Bioimaging Metallomics Adv. Exp. Med. Biol. 1055, 139–181 (2018). https://doi.org/10.1007/978-3-319-90143-5_7
C. Bich, D. Touboul, A. Brunelle, Biomedical studies by TOF-SIMS imaging. Biointerphases 10(1), 018901 (2014). https://doi.org/10.1116/1.4901511
A. Sussulini, J.S. Becker, J.S. Becker, Laser ablation ICP-MS: application in biomedical research. Mass Spectrom. Rev. 36(1), 47–57 (2017). https://doi.org/10.1002/mas.21481
J. Nuñez, R. Renslow, J.B. Cliff et al., NanoSIMS for biological applications: current practices and analyses. Biointerphases 13(3), 03B301 (2017). https://doi.org/10.1116/1.4993628
J. Decelle, G. Veronesi, B. Gallet et al., Subcellular chemical imaging: new avenues in cell biology. Trends Cell Biol. 30(3), 173–188 (2020). https://doi.org/10.1016/j.tcb.2019.12.007
J.K. Jeon, J.K. Kim, Track analysis of a synchrotron X-ray photoelectric nanoradiator by in situ fluorescence imaging of reactive oxygen species: comparative study of gold and iron oxide nanoparticles. J. Synchrotron Radiat. 25(Pt 6), 1768–1773 (2018). https://doi.org/10.1107/S1600577518011396
G. Van der Snickt, K. Janssens, J. Dik et al., Combined use of synchrotron radiation based micro-X-ray fluorescence, micro-X-ray diffraction, micro-X-ray absorption near-edge, and micro-fourier transform infrared spectroscopies for revealing an alternative degradation pathway of the pigment cadmium yellow in a painting by Van Gogh. Anal. Chem. 84(23), 10221–10228 (2012). https://doi.org/10.1021/ac3015627
U.E.A. Fittschen, G. Falkenberg, Trends in environmental science using microscopic X-ray fluorescence. Spectrochim. Acta. B 66(8), 567–580 (2011). https://doi.org/10.1016/j.sab.2011.06.006
R. Pérez-López, F. Macías, M.A. Caraballo et al., Mineralogy and geochemistry of Zn-rich mine-drainage precipitates from an MgO passive treatment system by synchrotron-based X-ray analysis. Environ. Sci. Technol. 45(18), 7826–7833 (2011). https://doi.org/10.1021/es201667n
R.V. Krishnamurthi, V.L. Feigin, M.H. Forouzanfar et al., Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob. Health. 1(5), e259–e281 (2013). https://doi.org/10.1016/S2214-109X(13)70089-5
F. Ma, A. Morancho, J. Montaner et al., Endothelial progenitor cells and revascularization following stroke. Brain Res. 1623, 150–159 (2015). https://doi.org/10.1016/j.brainres.2015.02.010
G. Esquiva, A. Grayston, A. Rosell, Revascularization and endothelial progenitor cells in stroke. Am. J. Physiol. Cell Physiol. 315(5), C664–C674 (2018). https://doi.org/10.1152/ajpcell.00200.2018
L. Finney, S. Mandava, L. Ursos et al., X-ray fluorescence microscopy reveals large-scale relocalization and extracellular translocation of cellular copper during angiogenesis. Proc. Natl. Acad. Sci. U. S. A. 104(7), 2247–2252 (2007). https://doi.org/10.1152/pnas.0607238104
E.Z. Longa, P.R. Weinstein, S. Carlson et al., Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20(1), 84–91 (1989). https://doi.org/10.1161/01.str.20.1.84
J. Chwiej, A. Patulska, A. Skoczen et al., Various ketogenic diets can differently support brain resistance against experimentally evoked seizures and seizure-induced elemental anomalies of hippocampal formation. J. Trace Elem. Med. Biol. 42, 50–58 (2017). https://doi.org/10.1016/j.jtemb.2017.04.002
S. Takahashi, S. Hatashita, Y. Taba et al., Determination of the spatial distribution of major elements in the rat brain with X-ray fluorescence analysis. J. Neurosci. Methods 100(1–2), 53–62 (2000). https://doi.org/10.1016/s0165-0270(00)00231-4
J.-L. Liu, Y.-G. Fan, Z.-S. Yang et al., Iron and Alzheimer’s disease: from pathogenesis to therapeutic implications. Front. Neurosci. 12, 632 (2018). https://doi.org/10.3389/fnins.2018.00632
R. Ingrassia, A. Lanzillotta, I. Sarnico et al., 1B/(-)IRE DMT1 expression during brain ischemia contributes to cell death mediated by NF-κB/RelA acetylation at Lys310. PLoS ONE 7(5), e38019 (2012). https://doi.org/10.1371/journal.pone.0038019
L. Goldstein, Z.-P. Teng, E. Zeserson et al., Hemin induces an iron-dependent, oxidative injury to human neuron-like cells. J. Neurosci. Res. 73(1), 113–121 (2003). https://doi.org/10.1002/jnr.10633
Y. Liu, J. Liu, H. Liu et al., Investigation of cerebral iron deposition in aged patients with ischemic cerebrovascular disease using susceptibility-weighted imaging. Ther. Clin. Risk Manag. 12, 1239–1247 (2016). https://doi.org/10.2147/tcrm.S107783
A. Saleh, M. Schroeter, A. Ringelstein et al., Iron oxide particle-enhanced MRI suggests variability of brain inflammation at early stages after ischemic stroke. Stroke 38(10), 2733–2737 (2007). https://doi.org/10.1161/strokeaha.107.481788
K.E. Sandoval, K.A. Witt, Blood-brain barrier tight junction permeability and ischemic stroke. Neurobiol. Dis. 32(2), 200–219 (2008). https://doi.org/10.1016/j.nbd.2008.08.005
C. Demougeot, M. Van Hoecke, N. Bertrand et al., Cytoprotective efficacy and mechanisms of the liposoluble iron chelator 2,2’-dipyridyl in the rat photothrombotic ischemic stroke model. J. Pharmacol. Exp. Ther. 311(3), 1080–1087 (2004). https://doi.org/10.1124/jpet.104.072744
Q.Z. Tuo, P. Lei, K.A. Jackman et al., Tau-mediated iron export prevents ferroptotic damage after ischemic stroke. Mol. Psychiatr. 22(11), 1520–1530 (2017). https://doi.org/10.1038/mp.2017.171
S.L. Galasso, R.H. Dyck, The role of zinc in cerebral ischemia. Mol. Med. 13(7–8), 380–387 (2007). https://doi.org/10.2119/2007-00044.Galasso
R.D. Palmiter, S.D. Findley, Cloning and functional characterization of a mammalian zinc transporter that confers resistance to zinc. EMBO J. 14(4), 639–649 (1995). https://doi.org/10.1002/j.1460-2075.1995.tb07042.x
C.T. Sheline, M.M. Behrens, D.W. Choi, Zinc-induced cortical neuronal death: contribution of energy failure attributable to loss of NAD(+) and inhibition of glycolysis. J. Neurosci. 20(9), 3139–3146 (2000). https://doi.org/10.1523/jneurosci.20-09-03139.2000
Y. Yamasaki, N. Matsuura, H. Shozuhara et al., Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke 26(4), 676–681 (1995). https://doi.org/10.1161/01.Str.26.4.676
K. Szydlowska, M. Tymianski, Calcium, ischemia and excitotoxicity. Cell Calcium 47(2), 122–129 (2010). https://doi.org/10.1016/j.ceca.2010.01.003
Z. Tang, S. Li, P. Han et al., Pertussis toxin reduces calcium influx to protect ischemic stroke in a middle cerebral artery occlusion model. J. Neurochem. 135(5), 998–1006 (2015). https://doi.org/10.1111/jnc.13359
G. Yu, F. Wu, E.-S. Wang, BQ-869, a novel NMDA receptor antagonist, protects against excitotoxicity and attenuates cerebral ischemic injury in stroke. Int. J. Clin. Exp. Pathol. 8(2), 1213–1225 (2015)
O. Gotoh, T. Asano, T. Koide et al., Ischemic brain edema following occlusion of the middle cerebral artery in the rat. I: The time courses of the brain water, sodium and potassium contents and blood-brain barrier permeability to 125I-albumin. Stroke 16(1), 101–109 (1985). https://doi.org/10.1161/01.Str.16.1.101
U. Ito, K. Ohno, R. Nakamura et al., Brain edema during ischemia and after restoration of blood flow. Measurement of water, sodium, potassium content and plasma protein permeability. Stroke 10(5), 542–547 (1979). https://doi.org/10.1161/01.str.10.5.542
K.A. Hossmann, S. Sakaki, V. Zimmerman, Cation activities in reversible ischemia of the cat brain. Stroke 8(1), 77–81 (1977). https://doi.org/10.1161/01.str.8.1.77
B.S. Jensen, BMS-204352: a potassium channel opener developed for the treatment of stroke. CNS Drug Rev. 8(4), 353–360 (2002). https://doi.org/10.1111/j.1527-3458.2002.tb00233.x
J.Z. Wang, M.V. Vyas, G. Saposnik et al., Incidence and management of seizures after ischemic stroke: systematic review and meta-analysis. Neurology 89(12), 1220–1228 (2017). https://doi.org/10.1212/WNL.0000000000004407
Z. Lei, H. Zhang, Y. Liang et al., Reduced expression of IA channels is associated with post-ischemic seizures. Epilepsy Res. 124, 40–48 (2016). https://doi.org/10.1016/j.eplepsyres.2016.05.008
D.R. Kramer, T. Fujii, I. Ohiorhenuan et al., Interplay between cortical spreading depolarization and seizures. Stereotact. Funct. Neurosurg. 95(1), 1–5 (2017). https://doi.org/10.1159/000452841
A. Zakharov, K. Chernova, G. Burkhanova et al., Segregation of seizures and spreading depolarization across cortical layers. Epilepsia 60(12), 2386–2397 (2019). https://doi.org/10.1111/epi.16390
L.S. Johnson, N. Mattsson, A. Sajadieh et al., Serum potassium is positively associated with stroke and mortality in the large. Population-based malmö preventive project cohort. Stroke 48(11), 2973–2978 (2017). https://doi.org/10.1161/STROKEAHA.117.018148
M. Lai, D. Wang, Z. Lin et al., Small molecule copper and its relative metabolites in serum of cerebral ischemic stroke patients. J. Stroke Cerebrovasc. Dis. 25(1), 214–219 (2016). https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.09.020
M.T. Huuskonen, Q.-Z. Tuo, S. Loppi et al., The copper bis(thiosemicarbazone) complex Cu-II(atsm) is protective against cerebral ischemia through modulation of the inflammatory milieu. Neurotherapeutics 14(2), 519–532 (2017). https://doi.org/10.1007/s13311-016-0504-9
X.Y. Choo, J.R. Liddell, M.T. Huuskonen et al., Cu(atsm) attenuates neuroinflammation. Front. Neurosci. 12, 668 (2018). https://doi.org/10.3389/fnins.2018.00668
J.R. Prohaska, A.A. Gybina, Rat brain iron concentration is lower following perinatal copper deficiency. J. Neurochem. 93(3), 698–705 (2005). https://doi.org/10.1111/j.1471-4159.2005.03091.x
X. Xu, S. Pin, M. Gathinji et al., Aceruloplasminemia: an inherited neurodegenerative disease with impairment of iron homeostasis. Ann. N. Y. Acad. Sci. 1012, 299–305 (2004). https://doi.org/10.1196/annals.1306.024
M.X. Yuan, X.W. Chen, B. Song et al., Characterization of dermal fiber architecture based on X-ray phase contrast micro-tomography. Nuclear Tech. 43, 70103 (2020). https://doi.org/10.11889/j.0253-3219.2020.hjs.43.070103
J. Hu, P. Li, X. Yin et al., Nondestructive imaging of the internal microstructure of vessels and nerve fibers in rat spinal cord using phase-contrast synchrotron radiation microtomography. J. Synchrotron Radiat. 24(Pt 2), 482–489 (2017). https://doi.org/10.1107/S1600577517000121
M. Zhang, G. Peng, D. Sun et al., Synchrotron radiation imaging is a powerful tool to image brain microvasculature. Med. Phys. 41, 3 (2014). https://doi.org/10.1118/1.4865784
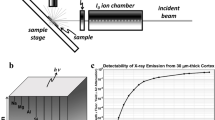
X.Y. Lan, A.G. Li, J. Wang, Bluesky-based fluorescence mapping technology. Nucl. Tech. 42, 040104 (2019). https://doi.org/10.11889/j.0253-3219.2019.hjs.42.040104. (in Chinese)
C. Epaule, A. Maksimenko, G. Bastian et al., X-ray microfluorescence for biodistribution studies of nanomedicines. Int. J. Pharm. 531(1), 343–349 (2017). https://doi.org/10.1016/j.ijpharm.2017.08.106
S.T. Kang, T. Wu, Z.H. Chen et al., 3D imaging of rat brain neural network using synchrotron radiation. Nucl. Tech. 43, 070101 (2020). https://doi.org/10.11889/j.0253-3219.2020.hjs.43.070101. (in Chinese)
Y. Cao, Y. Zhou, S. Ni et al., Three dimensional quantification of microarchitecture and vessel regeneration by synchrotron radiation microcomputed tomography in a rat model of spinal cord injury. J. Neurotrauma 34(6), 1187–1199 (2017). https://doi.org/10.1089/neu.2016.4697
M.Q. Zhang, D.N. Sun, Y.Y. Xie et al., Three-dimensional visualization of rat brain microvasculature following permanent focal ischaemia by synchrotron radiation. Br. J. Radiol. 87(1038), 20130670 (2014). https://doi.org/10.1259/bjr.20130670
Acknowledgements
The authors would like to thank the staff at the BL15U station of SSRF for their kind assistance during the experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All animal experiments were approved by the Experimental Zoology Department of Central South University and performed following Central South University experimental welfare ethics review standards on the use of animals in research.
Additional information
This work was supported by the National Natural Science Foundation of China (No. 81501025) and the Natural Science Foundation of Hunan Province (Nos. 2020JJ4134 and 2016JJ3174).
Rights and permissions
About this article
Cite this article
Shi, SP., Wang, H., Chen, ZH. et al. Characterization of metal element distributions in the rat brain following ischemic stroke by synchrotron radiation micro-fluorescence analysis. NUCL SCI TECH 31, 96 (2020). https://doi.org/10.1007/s41365-020-00807-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41365-020-00807-5