Abstract
Objectives
This study, following Woodford et al. (2024), investigated the collateral child and parent effects of function-based behavioral sleep interventions for 21 children with rare genetic neurodevelopmental conditions (RGNC).
Methods
Measures completed by parents at pre- and post-intervention assessed change in children’s internalizing and externalizing symptoms, health-related quality of life, behavioral strengths and difficulties, as well as parental sleep, relationship quality, and mental health symptoms. Data were analysed using modified Brinley plots and effect size estimates.
Results
Results demonstrate modest collateral benefits across child emotional and behavioral difficulties and health-related quality of life, and maternal anxiety and stress symptoms and sleep quality. There was minimal improvement in parent ratings of child externalizing symptoms and physical health-related quality of life, parent relationship satisfaction and all paternal outcome measures. There was no statistically significant relationship between changes in collateral outcomes and sleep problem severity.
Conclusions
Findings underscore the diverse potential benefits of improved sleep and highlight the need for further prioritisation of sleep services and research in RGNC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rare genetic neurodevelopmental conditions (RGNC) are a group of syndromes resulting from genetic alterations that affect < 1:2,000 people (European Commission, 2021; e.g., Fragile X, Smith-Magenis, Prader-Willi, Angelman syndromes). The neurological and phenotypic characteristics of these conditions place children at increased risk of sleep disturbance (Chawner et al., 2023). Estimates suggest that up to 90% of children with RGNC experience sleep onset and/or maintenance difficulties, depending on the type of sleep difficulties and RGNC (Agar et al., 2021; Kronk et al., 2010).
Research into the cause(s) of sleep disturbance in children with RGNC has focused predominantly on neurological and medical factors. In turn, related intervention research has largely focused on the effectiveness of pharmacological approaches such as melatonin (Blackmer & Feinstein, 2016; Schwitchenberg & Malow, 2015). While melatonin may be effective (Schwitchenberg & Malow, 2015), it does not address the psychosocial and behavioral factors that can underpin sleep difficulties. Thus, pharmacological interventions may only offer a partial solution. Behavioral sleep interventions address the motivational and environmental antecedents (e.g., sleep pressure; sleep hygiene) and socially mediated contingencies (e.g., reinforcing parent–child interactions following sleep-interfering behavior) that precede and maintain sleep disturbance (McLay et al., 2022a). Evidence suggests that behavioral sleep interventions are generally effective in treating sleep difficulties in autistic children (McLay et al., 2020); with additional emerging evidence for those with RGNC (Allen et al., 2013; Bindels-de Heus et al., 2023; McLay et al., 2019; Woodford et al., 2022).
Without effective intervention, sleep difficulties are likely to persist, resulting in a range of adverse consequences for neurodivergent children and their families. These include children’s physical health, quality of life, cognitive functioning, psychological wellbeing, and communication (Astill et al., 2012; Chawner et al., 2023; Cohen et al., 2018; Kay et al., 2023; Kronk et al., 2010; Leader et al., 2020, 2021, 2022; Moulding et al., 2020; Quach et al., 2016; Stores, 2016; Vandeleur et al., 2018); and the sleep, mental and physical health, and relationship quality of their caregivers (Chu & Richdale, 2009; Goldman et al., 2012; McDougall et al., 2005; McLay et al., 2023; Mörelius & Hemmingsson, 2014; Peltz et al., 2016; Rhoades et al., 2012). These multifaceted effects may compound the many difficulties already experienced by neurodivergent children and their families.
Research suggests that the relationship between child sleep disturbance and parent and child wellbeing is multi-directional and transactional. Many of the variables that contribute to sleep disturbance, are also exacerbated by sleep disturbance, as well as readily influencing one another. For example, children’s daytime behavior difficulties can be both a precipitant and consequence of sleep disturbance (Cohen et al., 2018; Hollway & Aman, 2011; Konjarski et al., 2018; Leader et al., 2020, 2021, 2022; Peltz et al., 2016). Both child behavioral difficulties and sleep disturbance can also impact parent wellbeing and sleep, which may affect parenting practices associated with the maintenance of child sleep and behavioral difficulties (Martin et al., 2019; Rhoades et al., 2012). To explore this interplay further, research is needed that investigates how the treatment of sleep difficulties might have secondary benefits across other areas of functioning. Changes beyond the primary intervention target (in this case sleep) are commonly referred to as ‘secondary’ or ‘collateral’ effects (henceforth collateral effects; Ledbetter-Cho et al., 2017; McLay et al., 2022b).
Research investigating the collateral effects of behavioral sleep intervention for neurodivergent children has shown some evidence of collateral benefit for both the child and parents, including children’s internalizing and externalizing symptoms, autism symptoms (e.g., social interaction and restricted and repetitive behavior) and quality of life (Austin et al., 2013; Hiscock et al., 2015; Hunter et al., 2020; Malow et al., 2014; McLay et al., 2022b; Papadopoulos et al., 2019; Thackeray & Richdale, 2002; Wiggs & Stores, 1999). While family and/or parent factors are less well researched, McLay et al. (2022b) found reliable, moderate improvements in the externalizing and internalizing symptoms (dav = -0.37 to -0.63) of autistic children following behavioral sleep intervention, along with reduced maternal anxiety symptoms (dav = -0.49) and improved sleep quality (dav = -0.49). Conversely, effects were small and not statistically significant for paternal wellbeing, and paternal sleep quality was unable to be assessed due to missing data.
Few studies have explored the direct and collateral effects of behavioral sleep intervention for children with RGNC (Allen et al., 2013; Bindels-de Heus et al., 2023; Bramble, 1997; Woodford et al., 2022). These studies suggest that behavioral sleep interventions are generally effective (4/4 studies) and acceptable (2/2 studies; Allen et al., 2013; Woodford et al., 2022) to parents in the treatment of sleep disturbance. However, collateral effects have varied. Allen et al. (2013) noted a mean reduction in parent-reported daytime behavior difficulties following behavioral sleep intervention for five children with Angelman syndrome. Bramble (1997) also noted improvements in parent-reported daytime behavior difficulties, as well as maternal stress and sleep quality following behavioral sleep intervention for 15 children with developmental delays (including two with Angelman and Smith-Magenis syndromes). Conversely, using a randomized controlled single-blinded trial, Bindels-de Heus et al. (2023) found no statistically significant differences in daytime behavior and parent stress levels (whether maternal and/or paternal was not specified) following behavioral sleep intervention for nine children with Angelman syndrome. While a statistically significant improvement was reported for child psychosocial quality of life, this change was not statistically significantly different to that of the control group. Similarly, Woodford et al. (2022) reported minimal to no improvement across a range of child and parent collateral measures for five children with RGNC. Interestingly, this study also included five autistic children, who generally showed improvement, with a mean change in scores in the therapeutic direction across most measured areas including internalizing and externalizing symptoms, parent sleep quality and paternal relationship quality. Overall, research is limited by small sample sizes (N = 5 to 15) and a lack of reported effect size estimates, limiting the inferences that can be made. Given the range of co-occurring difficulties experienced by children with RGNC and the potential for collateral benefits of behavioral sleep intervention, research in this area is clinically important.
This study further analyses data gathered by Woodford et al. (2024), which evaluated the direct effects of behavioral interventions on sleep for 26 children with RGNC. Children received individualized function-based behavioral sleep interventions in which varying combinations of circadian (e.g., sleep/wake rescheduling), antecedent (e.g., stimulus control techniques, visual supports such as Social Stories™) and consequence (e.g., positive reinforcement of sleep-conducive behavior and modified extinction) variables were modified (see Woodford et al., 2024 for a summary of interventions). Intervention resulted in reduced sleep problem severity (SPS; a composite score of sleep difficulty taken from sleep diary data; Woodford et al., 2024) for 24/26 children. Improvements maintained at follow-up for 13/16 children. The present study includes data from 21 of the 26 participants for whom both pre- and post-intervention measure data were available and aimed to investigate whether a reduction in SPS following behavioral sleep intervention resulted in collateral improvement in (a) children’s internalizing and externalizing symptoms; (b) children’s health-related quality of life; (c) parents’ sleep quality; (d) parents’ relationship satisfaction; and (e) parents’ symptoms of depression, anxiety and stress.
Method
Participants
As described in Woodford et al. (2024), this research was approved by the relevant University Human Ethics Committee, and parent/caregiver consent and child assent was obtained (for participants with adequate developmental capacity). Children and their families were recruited from varying service providers for children with RGNC and their families across New Zealand.
According to the inclusion criteria reported in Woodford et al. (2024), child participants had a confirmed or likely diagnosis of a RGNC as verified by the child’s primary physician (e.g., neurologist or pediatrician; 18/21 children), or a neurogenetic condition with similar phenotypic characteristics to RGNC (e.g., developmental delay, confirmed neurological alterations; 3/21 children); were aged between 18 months to 19 years of age (M = 7 years); and had at least seven consecutive nights of sleep diary and/or video data from the intervention phase of the programme (consistent with SPS requirements). See Table 1 for participant characteristics, including age, gender, ethnicity, primary diagnosis and co-occurring conditions (also published in Woodford et al., 2024).
Study Design
This study follows on from Woodford et al. (2024), and retrospectively analyses the collateral effects of behavioral sleep interventions for 21 of 26 cases for whom sufficient data were available.
Procedures
Measures of collateral effects (i.e., questionnaires) were posted to and completed by parents during the programs assessment (pre-intervention) and maintenance (post-intervention; within 4 weeks of intervention ending) phases. In households with two parents (19 of participants), one parent completed all child collateral effect measures, and both parents completed all parent collateral effect measures independently (see measure details below). The procedures of the sleep program (i.e., assessment, baseline, intervention, and maintenance phases) are detailed in Woodford et al. (2024).
Measures
Primary Outcome Measure
As a composite measure of sleep problem severity, SPS was the primary outcome measure used in this study to assess sleep across baseline, intervention and follow-up phases. An SPS mean score was calculated for baseline and intervention using sleep diary data (or video in cases which had missing diary data) from the final seven nights of the respective phase. Criteria as outlined in previous studies (Clarke et al., 2024; McLay et al., 2020) were established for preschool (2 – 4 years 11 months), childhood (5 – 12 years 11 months) and teen participants (13 – 18 years). A mean SPS score of > 2 (range = 0–22) is suggestive of clinically significant sleep disturbance (i.e., that the child had a moderate difficulty with at least two sleep parameters, or a larger difficulty in one sleep parameter such as prolonged sleep onset latency, night wakings and unwanted bed-sharing). Refer to Woodford et al. (2024) for further information.
Measures of Collateral Effects
Collateral effect measures included the Pediatric Quality of Life Inventory (PedsQL; Varni et al., 2001), Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) and Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001) as measures of child collateral effects; and the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989), Depression, Anxiety and Stress Scale (DASS-21; Lovibond & Lovibond, 1995) and Relationship Quality Index (RQI; Norton, 1983) as measures of parent collateral effects.
Pediatric Quality of Life Inventory Generic Core Scales
The PedsQL is a 23-item measure of health-related quality of life in young people 2–18 years of age (Varni et al., 1999, 2001). Parents rate how much of a problem each item was for their child over the past month using a 5-point Likert scale. Item ratings are reversed and linearly transformed to a 0–100 scale, then averaged to obtain subscale scores (higher scores indicate better health-related quality of life). The PedsQL has four subscales: Emotional, Social, Physical and School-Related Functioning. Item ratings from the Emotional, Social, and School-Related Functioning subscales are averaged to obtain a psychosocial functioning score, and all item ratings are averaged to obtain a total score. The PedsQL has been validated for use with children with neurodevelopmental conditions, with good–excellent internal consistency for both the overall measure (α = 0.90) and subscales (α = 0.78–0.91), in addition to good convergent (with the SDQ; Goodman, 2001) and criterion referenced validity (Varni et al., 2001; Viecili & Weiss, 2015).
Child Behavior Checklist
The CBCL (1.5–5 years and 6–18 years; Achenbach & Rescorla, 2001) is a measure of behavioral, social, and emotional symptoms in young people where parents rate how often their child’s behavior occurred over the past six months using a 3-point Likert scale. Scores are summed to provide Internalizing and Externalizing problem scale scores, and a Total score (higher scores indicate greater symptom severity). These are converted to t-scores to determine whether the child meets criteria for classifying symptom severity as normal (non-clinical; t-score < 65), borderline (at-risk: t-score 65–69) or clinical (t-score > 70). The CBCL (1.5–5 years) has acceptable model fit indices, and acceptable-excellent internal consistency for the overall measure (α = 0.94), scales (α = 0.82–0.90) and subscales (α = 0.67–0.88) in pre-school aged children with RGNC (Neo et al., 2021). Although not validated in older children with RGNC, a systematic review and meta-analysis (Glasson et al., 2020) found it was the most used measure of psychiatric symptoms in this population, and it has been widely used in sleep research with children with neurodevelopmental conditions (Delahaye et al., 2014; Goldman et al., 2012).
Strengths and Difficulties Questionnaire
The SDQ is a 25-item parent-report measure of behavioral strengths and difficulties in young people 4–17 years of age (Goodman, 2001). Parents rate how much each item applied to their child over the past six months using a 3-point Likert scale. It has five subscales: Emotional Symptoms, Conduct Problems, Hyperactivity-Inattention, Peer Problems, and Prosocial Behavior; the sum of these, excluding Prosocial Behavior, gives a total difficulties score. Higher scores indicate greater difficulty, with score ranges classified as normal (0–13), borderline (14–16) and abnormal (i.e., clinical; 17–40) levels of difficulty. The SDQ has been validated for use with children with neurodevelopmental conditions, with acceptable internal consistency (α = 0.71) and convergent validity (with the Developmental Behavior Checklist; Einfeld & Tonge, 1995), although internal consistency across subscales varies (α = 0.31–0.87; Emerson, 2005).
Pittsburgh Sleep Quality Index
The PSQI is a 19-item self-report measure of adult sleep quality (Buysse et al., 1989), with seven subscales: Sleep Quality, Sleep Latency, Sleep Duration, Sleep Efficiency, Sleep Disturbances, Use of Sleep Medication and Daytime Dysfunction. Respondents rate how often each item occurred over the past month on a 4-point Likert scale. Specific items are summed to obtain subscale scores, and a global sleep quality score (18 items; score range = 0–21). Higher scores indicate poorer sleep quality, with scores > 5 reliably differentiating poor from good sleep quality. The PSQI has been found to have good internal consistency, test–retest reliability (α = 0.83 and r = 0.85 respectively) and criterion reference validity, although convergent validity is limited (Buysse et al., 1989).
Depression, Anxiety and Stress Scale
The DASS-21 (the abbreviated version of the 42-item DASS; Lovibond & Lovibond, 1995) is a 21-item self-report measure of depression, anxiety, and stress symptoms (Henry & Crawford, 2005). Respondents rate the extent to which each item applied to them over the past week on a 4-point Likert scale. Specific item ratings are summed to provide depression, anxiety and stress subscale scores, and a total score. Higher scores indicate greater psychological distress, with score ranges provided to reflect normal, mild, severe, or extremely severe symptom severity. The DASS-21 has good–excellent internal consistency (α = 0.82–0.93), and convergent and divergent validity (Henry & Crawford, 2005).
Relationship Quality Index
The RQI (Norton, 1983) is a six-item, self-report measure of adults’ perceptions of the quality of their relationship with their partner. All item ratings are summed to provide a total score. A higher score indicates better perceived relationship quality, with a score > 29/45 reliably differentiating good from poor relationship quality. The RQI has acceptable-good internal consistency (α = 0.68–0.85) and strong convergent and divergent validity (Norton, 1983).
Data Analysis
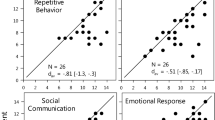
Modified Brinley plots (Blampied, 2017) were used to analyse change, pre- and post-intervention. In these scatterplots, each individual’s pre- and post-intervention scores are presented as a coordinate pair on the X and Y axis respectively. The 45˚ diagonal line (i.e., where X = Y) represents no change pre- to post- intervention. Data points above or below this line indicate a decrease or increase in scores respectively. The cross on the graph depicts the coordinates of the pre- (X) and post-intervention (Y) means and the length of each arm represents the standard deviation of the respective mean (Blampied, 2017). Additional dashed lines representing clinical cut-off scores are provided for the SDQ, PSQI, and RQI. For the CBCL and DASS-21, cut-off scores are not displayed due to multiple categorisations (e.g., normal, mild, severe) and/or they made visual presentation unclear.
Modified Brinley plots are accompanied by effect size estimates. The within-subjects standardized mean difference, Cohen’s dav (Cohen, 1988; calculated using Cumming, 2012 Exploratory Software for Confidence Intervals [ESCI]), and the Percent Superiority Effect Size (PSES; McGraw & Wong, 1992; calculated using Lakens, 2013 calculator) are reported. For Cohen’s dav, Cohen’s (1988) criteria (small dav ≤ 0.2, moderate dav = ~ 0.5, and large effect dav ≥ 0.8) guided tentative interpretation of results. Also calculated using ESCI (Cumming, 2012) were 95% Confidence Intervals (95% CI) about dav to assess whether dav was reliably different from zero. Where the 95% CI does not cross zero (i.e., the upper and lower limits are either both + or -) this indicates that the true value of d is unlikely to be zero (i.e., there is a treatment effect), and that a t-test on the corresponding means would be statistically significant (p < 0.05). Where the 95% CI crosses zero, a zero treatment effect cannot be ruled out. Across all measures except the PedsQL and RQI, a reduction in scores is clinically desirable, represented as points below the 45˚ line and a negative dav value. The PSES represents the probability, expressed as a percentage, that a randomly selected case will have a clinically better score post-intervention than at pre-intervention/baseline (McGraw & Wong, 1992).
Consistency Analysis
This analysis (such as that completed by McLay et al., 2022b) assesses how consistently improvements in child sleep are associated with concurrent changes in other (collateral) variables. First, change scores (pre-intervention minus post-intervention scores) were calculated for the primary sleep outcome measure (SPS; Woodford et al., 2024) and for each of the measures where there was evidence of some collateral benefit (i.e., dav > 0.45, and/or dav was reliably non-zero), computed such that the larger the change score, the larger the improvement. Second, these selected collateral change scores were then correlated with SPS change scores. Moderate to large positive correlations (r ≥ 0.5) were interpreted as representing high levels of consistency between improved sleep and collateral benefits.
Results
Descriptive data and effect size estimates for child and parent collateral effect measures are displayed in Tables 2 and 3, respectively. For the PedsQL, CBCL and SDQ, pre- and post-intervention data were available for 13, 19 and 14 participants, respectively. For the PSQI, DASS-21 and RQI, pre- and post-intervention data were available for 19, 21 and 17 mothers, and 18, 19 and 16 fathers, respectively. Reasons for missing data included non-completion by parent(s), participant withdrawal in the intervention phase, and single parent households (N = 2/21). In addition, the PedsQL was introduced part way through the wider research programme, and thus was not given to seven parents.
Child Collateral Effects
Pediatric Quality of Life
The modified Brinley plots showing individual change for PedsQL total, psychosocial and physical scores from pre- to post-intervention are displayed in Fig. 1. Mean pre-intervention PedsQL total, psychosocial, and physical scores were 49.12 (range = 33–75), 50.36 and 47.60, respectively. Total scores improved for 11, remained the same for two and deteriorated for one of 13 participants (PSES = 85%), indicating a moderate, reliably non-zero effect (dav = 0.42; 95% CI = 0.14, 0.69). There was greater improvement in the psychosocial scale than the physical scale with a small-moderate, reliably non-zero effect (dav = 0.44; 95% CI = 0.01, 0.85) versus a small and potentially zero effect (dav = 0.26; 95% CI = -0.20, 0.71), respectively.
Modified Brinley plots showing participants’ (N = 13) score changes from pre- to post-intervention for Paediatric Quality of Life Inventory (PedsQL) total (a) and psychosocial and physical subscales (b and c). Two data points lie on the pre- and post-intervention coordinates 53.1–62.5 for the physical subscale (c)
Child Behavior Checklist
The modified Brinley plots showing individual change for CBCL scale t-scores from pre- to post-intervention are displayed in Fig. 2. Mean pre-intervention, CBCL total, internalizing and externalizing t-scores fell within the clinical, borderline, and normal range, respectively. These scores reduced with intervention, with the mean total and internalizing scores crossing cut-offs (i.e., clinical to borderline for total, and borderline to normal for internalizing). For internalizing scores, 11 participants improved, seven worsened and one remained the same, with a moderate and reliably non-zero effect (dav = -0.56; 95% CI = -1.10, -0.01). For externalizing scores, 11 improved, six worsened and two remained the same, with a small and potentially zero effect (dav = 0.15; 95% CI = -0.48, 0.18). For total scores, 12 improved, six worsened and one remained the same, with a small-moderate but potentially zero effect (dav = -0.46; 95% CI = -0.95, 0.05). The probability of improvement post-intervention was never more than modest across subscales (PSES = 58–69%).
Strengths and Difficulties Questionnaire (SDQ)
The modified Brinley plot showing individual change for SDQ total scores from pre- to post-intervention is displayed in Fig. 3. The mean pre-intervention SDQtotal score = 16.79 (range = 14–25), indicating a high (i.e., abnormal) level of emotional and behavioral difficulty. Scores improved for 9/14 participants (3 worsened and 2 remained the same; PSES = 71%). The mean total score moved from the abnormal to borderline range, showing a moderate but potentially zero effect (dav = -0.45; CI = -0.91, 0.02).
Parent Collateral Effects
Pittsburgh Sleep Quality Index (PSQI)
The modified Brinley plots showing mothers’ and fathers’ change in PSQI total scores from pre- to post-intervention are displayed in Fig. 4. Pre-intervention PSQI total scores were above the clinical cut-off for most parents (28/37 parent scores > 5), indicating poor sleep quality. Fourteen of the 19 mothers showed improvement from pre- to post-intervention, while three worsened and two remained the same (PSES = 76%). Effect size estimates indicated a strong and reliably non-zero effect (dav = -0.90; CI = -1.53, -0.24), however, the mean score remained above the clinical cut-off. For fathers, scores improved for ten, worsened for seven and remained the same for one, reflecting a small (likely zero) effect (dav = -0.19; CI = -0.58, 0.20; PSES = 59%).
Modified Brinley plots showing mothers’ (N = 19) (a) and fathers’ (N = 18) (b) score changes from pre- to post-intervention for the Pittsburgh Sleep Quality Index (PSQI). For mothers, two data points lie on the pre- and post-intervention coordinates 10–4, 7–5 and 9–6. For fathers, two data points lie on the pre- and post-intervention coordinates 4–5 and 4–6
Depression, Anxiety and Stress Scale (DASS-21)
A modified Brinley plot showing mothers’ and fathers’ change for DASS-21 total scores from pre- to post-intervention is displayed in Fig. 5. Depression, anxiety and stress subscale scores are not plotted, due to overlap in several pre- to post-intervention coordinate pairs. Most parent ratings yielded scores in the normal-mild range across subscales, pre- and post-intervention. Scores were slightly higher for the stress subscale. Four parents (2 mothers, 2 fathers) had scores in the extremely severe range for at least one subscale at pre-intervention, with all but one (which remained the same) showing a clinically meaningful reduction with intervention. The degree of change varied for these four participants, with post-intervention scores falling across all symptom severity ranges. Mean change scores were generally greater for mothers than fathers. Cohens dav for mothers’ anxiety (dav = -0.56; CI = -1.09, -0.02), stress (dav = -0.55; CI = -0.92, -0.18), and total (dav = -0.51; CI = -0.94, -0.07) scores showed a moderate and reliably non-zero reduction compared to fathers whose changes were small (dav = -0.15 – 0.19; all 95% CI crossed zero). Parent depressive symptoms changed little following intervention (dav = -0.13 and -0.15 for mothers and fathers), likely due to a floor effect.
Relationship Quality Index (RQI)
The modified Brinley plots showing mothers and fathers change in RQI scores from pre- to post-intervention are displayed in Fig. 6. There was a ceiling effect on the RQI, with most parents rating their relationship quality highly pre-intervention (i.e., only 3/33 scores fell below the cut-off). RQI scores remained largely unchanged, although there was a slight trend for fathers to report improvement (dav = 0.13) and mothers to report minor deterioration (dav = -0.15). Cohen’s dav values for mothers and fathers indicate a small (likely zero) effect. One mother’s rating reduced considerably following intervention (12 points), falling below the cut-off.
Modified Brinley plots showing mothers’ (N = 17) (a) and fathers’ (N = 16) (b) total score change from pre- to post-intervention for the Relationship Quality Index (RQI). For mothers, two data points lie on the pre- and post-intervention coordinates 44–44. For fathers, two data points lie on the pre- and post-intervention coordinates 45–45, 45–44 and 39–39
Consistency Analysis
Measures where there was evidence of collateral benefit were the PedsQL total and psychosocial scores, SDQ total scores, CBCL total and internalizing t-scores, mothers’ anxiety, stress and total scores (DASS), and mothers’ PSQI total scores. All correlations between SPS change scores and these collateral change scores were small and non-significant (r = 0.017–0.24; all p > 0.05). Interestingly, 3/7 correlations were negative, namely, mothers DASS-21 scores (total, anxiety, and stress), suggesting a possible inconsistency between changes in children’s sleep and maternal wellbeing. The correlations are provided in Online Resource 1.
Discussion
This is one of few studies to have investigated child and parent collateral effects of function-based behavioral sleep intervention in children with RGNC. Several child and parent variables known to be associated with sleep disturbance were assessed at pre- and post-intervention, including children’s health-related quality of life (Quach et al., 2016; Stores, 2016; Vandeleur et al., 2018), internalizing and externalizing symptoms and daytime behavior (Astill et al., 2012; Bindels-de Heus et al., 2023; Hiscock et al., 2015; Kay et al., 2023), and parent sleep quality, depression, anxiety and stress symptoms and relationship satisfaction (Chu & Richdale, 2009; Goldman et al., 2012; Peltz et al., 2016; Rhoades et al., 2012). Pre- and post-intervention data were available and analysed for 21 children and their parents who had implemented a behavioral sleep intervention with some effectiveness, reported in Woodford et al. (2024). We hypothesized that improvements in sleep may have collateral benefits and improve the collateral domains assessed.
The results of the present study showed improvements extended beyond sleep to several areas including child behavior, internalizing symptoms and health-related quality of life, and maternal anxiety and stress symptoms and sleep quality. Child outcomes are consistent with previous research that has included neurodivergent children (Austin et al., 2013; Hiscock et al., 2015; Hunter et al., 2020; Malow et al., 2014; McLay et al., 2022b; Papadopoulos et al., 2019; Wiggs & Stores, 1999). Children generally had clinical level emotional and behavioral difficulties pre-intervention which showed moderate improvements following behavioral sleep intervention. Although resolution (i.e., change from clinical to normal) of such difficulties was not generally achieved, several participant’s SDQ and CBCL scores crossed symptom severity ranges. This suggests potential for clinically meaningful change to occur across untargeted areas. By contrast, the effect for externalizing symptoms, was small and non-significant. The reason for this is unclear but could be due to a floor effect (mean score in normal range). It is also possible externalizing presentations are more resistant to change in children with RGNC, due to phenotypic neurobehavioral differences (Sloneem et al., 2011).
In addition, evidence suggests sleep difficulties are associated with several adverse health-related sequelae (e.g., epilepsy, immune, and cardiovascular ailments; Delahaye et al., 2014; Quach et al., 2016; Vandeleur et al., 2018), and that sleep interventions could be beneficial for improving health-related quality of life (Hiscock et al., 2015; Quach et al., 2016; Vandeleur et al., 2018). This has rarely been considered for children with RGNC (Bindels-de Heus et al., 2023), despite high levels of health-related complexities (Joyce et al., 2018; Sinoo et al., 2019). In this study, the pre-intervention mean total PedsQL score (49.12) was lower than mean scores for a range of samples reported in previous studies (e.g., 22q deletion = 51, Dravet syndrome = 54.7, chronic health conditions = 73–77 and healthy children = 82–83; Joyce et al., 2018; Sinoo et al., 2019; Varni et al., 2001), suggesting this sample of children had generally poor health-related quality of life. A reliably moderate effect for both total and psychosocial quality of life was found, consistent with previous research with children with attention deficit hyperactivity disorder (ADHD) and Angelman syndrome (Bindels-de Heus et al., 2023; Hiscock et al., 2015). However, the mean total score remained relatively low (55.03), and the effect was small and non-significant for physical quality of life. It is possible this is because the conditions which affect the physical capacity of children with RGNC are not directly related to sleep disturbance. Further research is needed, however, as results related to physical quality of life in previous studies were either not statistically significant or not reported (Bindels-de Heus et al., 2023; Hiscock et al., 2015).
Mechanisms underpinning collateral child benefits are complex. Research suggests there is a direct link between better sleep quality and quantity and improved mood, daytime behavior, and quality of life (Bindels-de Heus et al., 2023; Hiscock et al., 2015; Hollway & Aman, 2011; Konjarski et al., 2018); however, improvements may not necessarily be linked directly to improved sleep. Behavioral sleep interventions often target a range of parent behaviors in order to change children’s night-time behavior. For example, teaching parents how to set limits around bedtime and altering operant contingencies related to parent–child interactions, such as the removal of reinforcement for sleep interfering behavior (e.g., parent attention, access to devices) and provision of reinforcement for sleep-conducive behavior (e.g., rewards for compliance with bedtime routines). Such strategies are generalisable to the management of day-time behavior difficulties. Therefore, with successful implementation in the sleep context, parents might gain new knowledge, confidence, and increased capacity to cope with and address other difficulties, potentially explaining changes in children’s daytime functioning concomitant with sleep (Bindels-de Heus et al., 2023; Goldman et al., 2012; McLay et al., 2022b). In addition, improvement in children’s sleep, may mean that children are better able to engage, tolerate and respond to instructions and requests (Chawner et al., 2023; Moulding et al., 2020). It is important to note that specific child characteristics (e.g., temperament, behavioural difficulties) and parental treatment fidelity may influence the extent to which improvements are made both in sleep and across collateral domains (Cohen et al., 2018; McLay et al., 2020). Further research is needed in these areas. Nonetheless, sleep interventions and collateral effect outcomes varied, and it is not clear how these variables are inter-related. Further research is needed which not only evaluates the effectiveness and acceptability associated with specific intervention strategies, but also the collateral effects thereof. This would ensure the strategies with the greatest collateral benefit(s) are prioritised for implementation.
Consistent with previous research (Hiscock et al., 2015; Hunter et al., 2020; McLay et al., 2022b; Wiggs & Stores, 2001), collateral benefits of behavioral sleep intervention were also evident among mothers. Results showed reliably moderate improvements in maternal sleep quality, and anxiety and stress symptoms. However, the magnitude of change varied, and the PSQI mean total score remained above the measure’s clinical cut-off, indicating sleep quality remained poor for many. Despite improvements in sleep for all 21 children, for some, sleep difficulties remained, which may mean maternal sleep might have continued to be disrupted (albeit to a lesser extent). Alternatively, it is possible parents continued to experience sleep difficulties due to external factors (e.g., mental health, stressors, sleep disorders). Although it is not clear what contributed to maternal sleep disturbance and levels of anxiety and stress, there is a wealth of research which suggests children’s sleep difficulties may disrupt parent sleep, resulting in fatigue and associated difficulties with mental health (e.g., low mood, irritability; Chu & Richdale, 2009; Goldman et al., 2012; McDougall et al., 2005; Peltz et al., 2016). Therefore, with child sleep improvements, mothers may have benefitted.
Interestingly, improvements in fathers’ wellbeing and sleep were small and non-significant. This may be related to the different roles mothers and fathers had in their child’s sleep and delivery of interventions (Mörelius & Hemmingsson, 2014). Within this sample, mothers primarily managed their child’s sleep pre-intervention and took on the role of the primary interventionist. Therefore, it is possible mothers attributed improvements to their efforts (i.e., as causal agent of change) which may have increased their self-efficacy and improved their wellbeing (McDougall et al., 2005). Conversely, it is also possible that because some fathers were less involved in the intervention, their ratings were less susceptible to bias (Hunter et al., 2020; McLay et al., 2022b). Further, fathers’ PSQI scores were slightly lower (indicative of better sleep quality) than that of mothers at pre-intervention, and so it is possible fathers were less sleep deprived or affected by their child’s sleep difficulties to begin with. Qualitative research which explores differences between mothers’ and fathers’ experiences would be beneficial.
Research on the impact of behavioral sleep intervention on parental relationship quality is limited. McLay et al. (2022b) is the only study identified to have measured parental relationship quality as a collateral measure. Consistent with the results of McLay et al. (2022b) no clear improvement in relationship quality was found. It is possible this is due to a ceiling effect and that a more detailed measure of relationship quality such as direct parent report, observation and/or other psychometric measures might have captured change more accurately.
Limitations and Areas for Future Research
There are several limitations to consider. First, all collateral measures were based on parent report and the perspectives of the children were not able to be captured due to the developmental and communicative level of all participants. Parents may have perceived and/or reported improvements in other areas as a reflection of improved sleep; a Halo effect (Hunter et al., 2020; McLay et al., 2022b). In addition, parents were aware of the rationale for administering the collateral effect measures and in turn may have responded in a socially desirable manner. To prevent potential biases influencing results, future research should obtain data from additional sources for triangulation. Second, while the psychometric properties of the selected measures were good, it is possible some were not sensitive enough to detect small changes (e.g., the RQI has only 5 broad items). In addition, although most have been used extensively with children with neurodevelopmental conditions (e.g., Glasson et al., 2020; McLay et al., 2022b), some (e.g., CBCL 5–18 years) have not been validated with this population, and thus may have compromised reliability and validity. Observational data would ensure small and specific changes were captured and validated (e.g., Cohen et al., 2018). Third, although this study administered a range of collateral effect measures, sleep difficulties can negatively impact a wide range of areas of functioning (e.g., childrens’ cognitive functioning, school attendance and communication, and parents’ child-related stress and perceived control) that were not measured. Fourth, although the inclusion of a range of RGNC provided an adequate sample size for formal quantitative evaluation (Lakens, 2022), RGNC are a heterogenous group of conditions with varying presentations. We know the etiology of sleep difficulties and the child and parent variables assessed are multifaceted, and the direction of the relationship varies. Therefore, the degree to which children and families studied here are representative of the range of children with RGNC is unknown, as is the generality of intervention effects. Finally, although these results are promising, it is not possible to determine whether changes in sleep and/or the strategies taught in behavioral sleep intervention directly resulted in all the collateral benefits reported. The intervention duration for some participants was prolonged (maximum = 210 nights), and thus so was the time between completion of pre- and post-intervention measures. It is possible change could have occurred without intervention, at least in some cases and particularly for young children in sensitive developmental periods. In future research, comparison to a waitlist control group would clarify if the magnitude of change was greater for those who received a behavioral sleep intervention. On the other hand, for those who had shorter intervention periods (minimum = 29 nights), collateral effects might not yet have had time to emerge. The duration of any collateral benefits is also important, and future research should consider administering collateral measures during follow-up periods, to determine the maintenance of collateral effects or whether collateral effects emerge later (McLay et al., 2022b).
Conclusion
Consistent with other research, improvements extended beyond sleep to several areas of child and parental behavior and wellbeing. These results highlight the importance of considering sleep difficulties in the context of other challenges children with RGNC and their families might experience (e.g., low mood, irritability), given effectively treating sleep disturbance might have flow on effects (Hiscock et al., 2015; Hunter et al., 2020; McLay et al., 2022b). The findings, however, suggest that not all children and families will experience collateral benefits from behavioral sleep intervention with variability in the magnitude of change, and some participant ratings deteriorating or remaining stable across measures. Further research is needed which explores a range of possible collateral effects beyond that measured in this study, the mechanisms underpinning collateral effects, and if and why differences might occur across varying presentations.
Data Availability
The data that support the findings of this study are available on request from the corresponding author (EW).
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6–18, teacher's report form, youth self-report: An integrated system of multi-informant assessment. University of Vermont, Research Center for Children Youth & Families.
Agar, G., Brown, C., Sutherland, D., Coulborn, S., Oliver, C., & Richards, C. (2021). Sleep disorders in rare genetic syndromes: a meta-analysis of prevalence and profile. Molecular Autism, 12(1), 1–18. https://doi.org/10.1186/s13229-021-00426-w
Allen, K. D., Kuhn, B. R., DeHaai, K. A., & Wallace, D. P. (2013). Evaluation of a behavioral treatment package to reduce sleep problems in children with angelman syndrome. Research in Developmental Disabilities, 34(1), 676–686.
Astill, R. G., Van der Heijden, K. B., Van IJzendoom, M. H., & Van Someren, E. J. W. (2012). Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychological Bulletin, 138(6), 1109–1138. https://doi.org/10.1037/a0028204
Austin, K. L., Gordon, J. E., & O’Connell, A. (2013). Preliminary evaluation of sleepwise program for children with sleep disturbance and developmental delay. Child and Family Behavior Therapy, 35(3), 195–211. https://doi.org/10.1080/07317107.2013.818886
Blackmer, A. B., & Feinstein, J. A. (2016). Management of sleep disorders in children with neurodevelopmental disorders: a review. Pharmacotherapy, 36(1), 84–98. https://doi.org/10.1002/phar.1686
Blampied, N. M. (2017). Analysing therapeutic change using modified Brinley plots: History, construction, and interpretation. Behaviour Therapy, 48(1), 115–127. https://doi.org/10.1016/j.beth.2016.09.002
Bramble, D. (1997). Rapid-acting treatment for a common sleep problem. Developmental Medicine and Child Neurology, 39(8), 543–547. https://doi.org/10.1111/j.1469-8749.1997.tb07483.x
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Chawner, S. J. R. A., Evans, A., Williams, N., Owen, M. J., Hall, J., van den Bree, M. B. M., IMAGINE-ID consortium. (2023). Sleep disturbance as a transdiagnostic marker of psychiatric risk in children with neurodevelopmental risk genetic conditions. Translational Psychiatry, 13(1), 7–7. https://doi.org/10.1038/s41398-022-02296-z
Chu, J., & Richdale, A. L. (2009). Sleep quality and psychological wellbeing in mothers of children with developmental disabilities. Research in Developmental Disabilities, 30(6), 1512–1522. https://doi.org/10.1016/j.ridd.2009.07.007
Clarke, M. A. C., McLay, L. K., France, K. G., & Blampied, N. M. (2024). An evaluation of a stepped-care telehealth program for improving the sleep of autistic children. Research in Autism Spectrum Disorders, 112. https://doi.org/10.1016/j.rasd.2024.102356
Cohen, S., Fulcher, B. D., Rajaratnam, S. M. W., Phillips, A. J. K., Cornish, K. M., Lockley, S. W., Sullivan, J. P., St Hilaire, M. A., Loddenkemper, T., Kothare, S. V., Conduit, R., McConnell, K., Braga-Kenyon, P., Ahearn, W., Shlesinger, A., Potter, J., & Bird, F. (2018). Sleep patterns predictive of daytime challenging behavior in individuals with low-functioning autism. Autism Research, 11(2), 391–403. https://doi.org/10.1002/aur.1899
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Earlbaum Associates. https://doi.org/10.4324/9780203771587
Cumming, G. (2012). Understanding the new statistics: effect sizes, confidence intervals, and meta-analysis. Routledge. https://doi.org/10.4324/9780203807002
de Heus, K. G. C. B. B., Hooven-Radstaake, M. T., Legerstee, J. S., Hoopen, L. W. T., Dieleman, G. C., Moll, H. A., Mous, S. E., & de Wit, M.-C.Y. (2023). Sleep problems in children with angelman syndrome: The effect of a behavioral intervention program. Research in Developmental Disabilities, 135, 104444–104444. https://doi.org/10.1016/j.ridd.2023.104444
Delahaye, J., Kovacs, E., Sikora, D., Hall, T. A., Orlich, F., Clemons, T. E., van der Weerd, E., Glick, L., & Kuhlthau, K. (2014). The relationship between health-related quality of life and sleep problems in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 8(3), 292–303. https://doi.org/10.1016/j.rasd.2013.12.015
Einfeld, S. L., & Tonge, B. J. (1995). The developmental behavior checklist: the development and validation of an instrument to assess behavioral and emotional disturbance in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders, 25(2), 81–104. https://doi.org/10.1007/BF02178498
Emerson, E. (2005). Use of the strengths and difficulties questionnaire to assess the mental health needs of children and adolescents with intellectual disabilities. Journal of Intellectual & Developmental Disability, 30(1), 14–23. https://doi.org/10.1080/13668250500033169
European Commission. (2021). Rare diseases: Commission activities in the area of rare diseases. Retrieved from https://ec.europa.eu/info/research-and-innovation_en?pg=area&areaname=rare. Accessed July 2023
Glasson, E. J., Buckley, N., Chen, W., Leonard, H., Epstein, A., Skoss, R., Jacoby, P., Blackmore, A. M., Bourke, J., & Downs, J. (2020). Systematic review and meta-analysis: mental health in children with neurogenetic disorders associated with intellectual disability. Journal of the American Academy of Child and Adolescent Psychiatry, 59(9), 1036–1048. https://doi.org/10.1016/j.jaac.2020.01.006
Goldman, S. E., Bichell, T. J., Surdyka, K., & Malow, B. A. (2012). Sleep in children and adolescents with angelman syndrome: association with parent sleep and stress. Journal of Intellectual Disability Research, 56(6), 600–608. https://doi.org/10.1111/j.1365-2788.2011.01499.x
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry, 40(11), 1337–1345.
Henry, J. D., & Crawford, J. R. (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44(2), 227–239. https://doi.org/10.1348/014466505X29657
Hiscock, H., Sciberras, E., Mensah, F., Gerner, B., Efron, D., Khano, S., & Oberklaid, F. (2015). Impact of a behavioral sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: Randomised controlled trial. BMJ (online), 350, h68. https://doi.org/10.1136/bmj.h68
Hollway, J. A., & Aman, M. G. (2011). Sleep correlates of pervasive developmental disorders: a review of the literature. Research in Developmental Disabilities, 32(5), 1399–1421. https://doi.org/10.1016/j.ridd.2011.04.001
Hunter, J. E., McLay, L. K., France, K. G., & Blampied, N. M. (2020). Systematic review of the collateral effects of behavioral sleep interventions in children and adolescents with autism spectrum disorder. Research in Autism Spectrum Disorders, 79, 101677. https://doi.org/10.1016/j.rasd.2020.101677
Joyce, P., O’Rourke, C., McDermott, B., & Heussler, H. (2018). Health-related quality of life in 22q11.2 deletion syndrome: the child’s perspective. Journal of Paediatrics and Child Health, 54(3), 311–315. https://doi.org/10.1111/jpc.13746
Kay, C., Leonard, H., Smith, J., Wong, K., & Downs, J. (2023). Genotype and sleep independently predict mental health in rett syndrome: an observational study. Journal of Medical Genetics. https://doi.org/10.1136/jmg-2022-108905
Konjarski, M., Murray, G., Lee, V. V., & Jackson, M. L. (2018). Reciprocal relationships between daily sleep and mood: a systematic review of naturalistic prospective studies. Sleep Medicine Reviews, 42, 47–58. https://doi.org/10.1016/j.smrv.2018.05.005
Kronk, R., Bishop, E. E., Raspa, M., Bickel, J. O., Mandel, D. A., & Bailey, D. B., Jr. (2010). Prevalence, nature, and correlates of sleep problems among children with fragile X syndrome based on a large scale parent survey. Sleep, 33(5), 679–687.
Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 1–12. https://doi.org/10.3389/fpsyg.2013.00863
Lakens, D. (2022). Sample Size Justification. Collabra: Psychology, 8(1). https://doi.org/10.1525/collabra.33267
Leader, G., Murray, M., O’Súilleabháin, P. S., Maher, L., Naughton, K., Arndt, S., White, K., Traina, I., & Mannion, A. (2020). Relationship between parent-reported gastrointestinal symptoms, sleep problems, autism spectrum disorder symptoms, and behavior problems in children and adolescents with 22q11.2 deletion syndrome. Research in Developmental Disabilities, 104, 103698–103698. https://doi.org/10.1016/j.ridd.2020.103698
Leader, G., Forde, J., Naughton, K., Maher, L., Arndt, S., & Mannion, A. (2021). Relationships among gastrointestinal symptoms, sleep problems, challenging behavior, comorbid psychopathology and autism spectrum disorder symptoms in children and adolescents with 15q duplication syndrome. Journal of Intellectual Disability Research, 65(1), 32–46. https://doi.org/10.1111/jir.12789
Leader, G., Gilligan, R., Whelan, S., Coyne, R., Caher, A., White, K., Traina, I., Muchenje, S., Machaka, R. L., & Mannion, A. (2022). Relationships between challenging behavior and gastrointestinal symptoms, sleep problems, and internalizing and externalizing symptoms in children and adolescents with angelman syndrome. Research in Developmental Disabilities, 128, 104293–104293. https://doi.org/10.1016/j.ridd.2022.104293
Ledbetter-Cho, K., Lang, R., Watkins, L., O’Reilly, M., & Zamora, C. (2017). Systematic review of collateral effects of focused interventions for children with autism spectrum disorder. Autism & Developmental Language Impairments, 2, 1–22. https://doi.org/10.1177/2396941517737536
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety Inventories. Behavior Research and Therapy, 33(3), 335–343.
Malow, B. A., Adkins, K. W., Reynolds, A., Weiss, S. K., Loh, A., Fawkes, D., Katz, T., Goldman, S. E., Madduri, N., Hundley, T., & Clemons, T. (2014). Parent- based sleep education for children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 216–228. https://doi.org/10.1007/s10803-013-1866-z
Martin, C. A., Papadopoulos, N., Chellew, T., Rinehart, N. J., & Sciberras, E. (2019). Associations between parenting stress, parent mental health and child sleep problems for children with ADHD and ASD: systematic review. Research in Developmental Disabilities, 93, 1–15. https://doi.org/10.1016/j.ridd.2019.103463
McDougall, A., Kerr, A. M., & Espie, C. A. (2005). Sleep disturbance in children with Rett syndrome: a qualitative investigation of the parental experience. Journal of Applied Research in Intellectual Disabilities, 18(3), 201–215. https://doi.org/10.1111/j.1468-3148.2005.00220.x
McGraw, K. O., & Wong, S. P. (1992). A common language effect size statistic. Psychological Bulletin, 111(2), 361–365. https://doi.org/10.1037/0033-2909.111.2.361
McLay, L., Roche, L., France, K. G., Blampied, N. M., Lang, R., France, M., & Busch, C. (2019). Systematic review of the effectiveness of behaviorally-based interventions for sleep problems in people with rare genetic neurodevelopmental disorders. Sleep Medicine Reviews, 46, 54–63. https://doi.org/10.1016/j.smrv.2019.04.004
McLay, L., France, K., Blampied, N., van Deurs, J., Hunter, J., Knight, J., Hastie, B., Carnett, A., Woodford, E., Gibbs, R., & Lang, R. (2020). Function-based behavioral interventions for sleep problems in children and adolescents with autism: summary of 41 clinical cases. Journal of Autism and Developmental Disorders, 51(2), 418–432. https://doi.org/10.1007/s10803-020-04548-7
McLay, K. L., Carnett, A., & Rispoli, M. (2022a). Function-based interventions for sleep problems in children on the autism spectrum. In McLay, L. K., France, K. G., & Blampied, N. M. (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 93 – 109). Springer. https://doi.org/10.1007/978-3-030-99134-0_5
McLay, K. L., France, K. G., Blampied, N. M., Hunter, J. E., van Deurs, J. R., Woodford, E. C., Gibbs, R., & Lang, R. (2022b). Collateral child and parent effects of function-based behavioral interventions for sleep problems in children and adolescents with autism. Journal of Autism and Developmental Disorders, 52(5), 2258–2273. https://doi.org/10.1007/s10803-021-05116-3
McLay, L. K., Hansen, S. G., Blampied, N. M., France, K. G., & Rispoli, M. (2023). The type, severity, and impact of sleep problems in children with Angelman syndrome and parental help-seeking patterns. Behavioral Sleep Medicine, 1–13. https://doi.org/10.1080/15402002.2023.2241943
Mörelius, E., & Hemmingsson, H. (2014). Parents of children with physical disabilities perceived health in parents related to the child’s sleep problems and need for attention at night. Child: Care, Health & Development, 40(3), 412–418. https://doi.org/10.1111/cch.12079
Moulding, H. A., Bartsch, U., Hall, J., Jones, M. W., Linden, D. E., Owen, M. J., & van den Bree, M. B. M. (2020). Sleep problems and associations with psychopathology and cognition in young people with 22q11.2 deletion syndrome (22q11.2DS). Psychological Medicine, 50(7), 1191–1202. https://doi.org/10.1017/S0033291719001119
Neo, W. S., Suzuki, T., & Kelleher, B. L. (2021). Structural validity of the child behavior checklist (CBCL) for preschoolers with neurogenetic syndromes. Research in Developmental Disabilities, 109, 103834–103834. https://doi.org/10.1016/j.ridd.2020.103834
Norton, R. (1983). Measuring marital quality: a critical look at the dependent variable. Journal of Marriage and Family, 45(1), 141–151. https://doi.org/10.2307/351302
Papadopoulos, N., Sciberras, E., Hiscock, H., Mulraney, M., McGillivray, J., & Rinehart, N. (2019). The efficacy of a brief behavioral sleep intervention in school-aged children with ADHD and comorbid autism spectrum disorder. Journal of Attention Disorders, 23(4), 341–350.
Peltz, J. S., Rogge, R. D., Sturge-Apple, M. L., O’Connor, T. G., & Pigeon, W. R. (2016). Reciprocal influences among family processes and toddlers’ sleep problems. Journal of Family Psychology, 30(6), 720–731. https://doi.org/10.1037/fam0000202
Quach, J., Mensah, F. K., & Hiscock, H. (2016). Differential outcomes of sleep problems in children with and without special health care needs: Australian population study. Journal of Developmental and Behavioral Pediatrics, 37(5), 415–423. https://doi.org/10.1097/DBP.0000000000000274
Rhoades, K. A., Leve, L. D., Harold, G. T., Mannering, A. M., Neiderhiser, J. M., Shaw, D. S., Natsuaki, M. N., & Reiss, D. (2012). Marital hostility and child sleep problems: direct and indirect associations via hostile parenting. Journal of Family Psychology, 26(4), 488–498. https://doi.org/10.1037/a0029164
Schwichtenberg, A. J., & Malow, B. A. (2015). Melatonin treatment in children with developmental disabilities. Sleep Medicine Clinics, 10(2), 181. https://doi.org/10.1016/j.jsmc.2015.02.008
Sinoo, C., de Lange, I. M., Westers, P., Gunning, W. B., Jongmans, M. J., & Brilstra, E. H. (2019). Behavior problems and health-related quality of life in dravet syndrome. Epilepsy & Behavior, 90, 217–227. https://doi.org/10.1016/j.yebeh.2018.11.029
Sloneem, J., Oliver, C., Udwin, O., & Woodcock, K. A. (2011). Prevalence, phenomenology, aetiology and predictors of challenging behavior in Smith-Magenis syndrome. Journal of Intellectual Disability Research, 55(2), 138–151. https://doi.org/10.1111/j.1365-2788.2010.01371.x
Stores, G. (2016). Multifactorial influences, including comorbidities, contributing to sleep disturbance in children with a neurodevelopmental disorder. CNS Neuroscience & Therapeutics, 22(11), 875–879. https://doi.org/10.1111/cns.12574
Thackeray, E. J., & Richdale, A. L. (2002). The behavioural treatment of sleep difficulties in children with an intellectual disability. Behavioral Interventions, 17(4), 211–231. https://doi.org/10.1002/bin.123
Vandeleur, M., Walter, L. M., Armstrong, D. S., Robinson, P., Nixon, G. M., & Horne, R. S. C. (2018). Quality of life and mood in children with cystic fibrosis: associations with sleep quality. Journal of Cystic Fibrosis, 17(6), 811–820. https://doi.org/10.1016/j.jcf.2017.11.021
Varni, J. W., Seid, M., & Rode, C. A. (1999). The PedsQL™: measurement model for the pediatric quality of life inventory. Medical Care, 126–139.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQL 4.0: reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Med Care, 39(8), 800–812.
Viecili, M. A., & Weiss, J. A. (2015). Reliability and validity of the pediatric quality of life inventory with individuals with intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 120(4), 289–301. https://doi.org/10.1352/1944-7558-120.4.289
Wiggs, L., & Stores, G. (1999). Behavioural treatment for sleep problems in children with severe learning disabilities and challenging daytime behaviour: effect on daytime behaviour. Journal of Child Psychology and Psychiatry, 40(4), 627–635. https://doi.org/10.1111/1469-7610.00479
Wiggs, L., & Stores, G. (2001). Behavioural treatment for sleep problems in children with severe intellectual disabilities and daytime challenging behaviour: effect on mothers and fathers. British Journal of Health Psychology, 6(3), 257. https://doi.org/10.1348/135910701169197
Woodford, E. C., McLay, L., Blampied, N. M., France, K. G., Gibbs, R., Whitaker, C., & McCaughan, E. (2022). Less restrictive behavioral interventions for sleep problems in children with neurodevelopmental disorders: a single case feasibility study. Journal of Developmental and Physical Disabilities. https://doi.org/10.1007/s10882-022-09872-7
Woodford, E. C., France, K. G., Blampied, N. M., Hanning, U., Swan, C., & McLay, L. (2024). Behavioral sleep interventions for children with rare genetic neurodevelopmental conditions: A retrospective analysis of overall outcomes for 26 cases. Advances in Neurodevelopmental Disorders. https://doi.org/10.1007/s41252-024-0040-3
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This research was supported by funding from the Royal Society of New Zealand Marsden Fund Fast-Start Grant (#M1211).
Author information
Authors and Affiliations
Contributions
EW: designed and executed the study, completed assessment and intervention with most participants, conducted the data analyses including figure construction, and wrote the paper. LM and KF: provided clinical supervision and collaborated with the design of the study and editing of the manuscript. NB: collaborated with the design of the study, data analyses and editing of the final manuscript. CS: collaborated with editing the final manuscript. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics Approval
This research was approved by the relevant university Human Ethics Committee (HEC 2018–48) and has been conducted in accordance with the tenets of the declaration of Helsinki and its later amendments.
Consent
Informed consent was obtained from all parent participants and, assent was provided by most children for both participation in the study and publishing of results.
Competing Interests
The authors have no competing interests to declare relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Woodford, E.C., McLay, L.K., France, K.G. et al. Collateral Child and Parent Effects of Behavioral Sleep Interventions for Children with Rare Genetic Neurodevelopmental Conditions. Adv Neurodev Disord (2024). https://doi.org/10.1007/s41252-024-00399-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s41252-024-00399-w