Abstract
Objectives
Research suggests that the quality of life of professional caregivers of individuals with intellectual disabilities and autism spectrum disorder can be enhanced through mindfulness-based training. The effects of such training have been evidenced in terms of perceived psychological stress, compassion satisfaction, compassion fatigue (i.e., burnout, secondary traumatic stress), and symptoms of depression. In addition to changes in caregiver personal outcomes, mindfulness-based training may have effects on the quality assurance variables of the agency that employs these caregivers. The aim of the present study was to examine the changes from a systems perspective in terms of quality assurance variables related to caregivers and clients in community-based group homes.
Methods
Professional caregivers (n = 216) were randomized into three experimental conditions based on the training they received: mindfulness, psychoeducation, or inservice training-as-usual (control). The effects of the training were assessed in terms of quality assurance indices pertaining to caregivers (progressive discipline, call-ins, days absent, medical referrals, hospitalizations, and caregiver turnover) and clients (learning objectives, behavioral episodes, use of physical restraints, emergency medications [stat], medical emergencies, hospitalizations, aggression to staff, aggression to peers, and level of supervision).
Results
Overall, caregivers in the mindfulness group exhibited significantly fewer progressive discipline and call-ins when compared to the psychoeducation and control groups. Caregivers in both the mindfulness and psychoeducation groups exhibited significantly fewer days of absence from work, medical referrals, and caregiver turnover when compared to the control group. There was no difference across the three groups in terms of hospitalizations. Clients under the care of mindfulness-trained caregivers showed significantly greater improvement in completing learning objectives, fewer behavioral episodes, reduced need for physical restraints and stat medication for behavioral episodes, fewer episodes of aggression to peers, and lower levels of supervision when compared to those in the psychoeducation and control groups. Clients did equally well in terms of medical emergencies, hospitalizations, and aggression to staff in the mindfulness and psychoeducation groups when compared to those in the control group.
Conclusions
Differential effects of mindfulness training, psychoeducation, and inservice training-as-usual were evident in quality assurance variables related to caregivers and clients. The results suggest that training caregivers in different approaches to self-care may differentially affect not only their clinical status but also at a systems level in terms of quality assurance indices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Individuals with intellectual disability (ID) and autism spectrum disorder (ASD) often reside in community group homes and must rely on professionals employed specifically to support and take care of their needs. Although professional caregivers report much gratification in providing such services (Beighton & Wills, 2019; Hastings & Horne, 2004), long-term care of clients whose behaviors caregivers find challenging can be emotionally draining and may lead to stress, compassion fatigue, and decreased quality of life (Hensel et al., 2012; Mutkins et al., 2011; Panicker & Ramesh, 2019). Similar findings have also been reported for informal caregivers of individuals with intellectual or mental impairments (Sit et al., 2020). The consensus in the research literature is that regardless of the pathways that affect caregivers (e.g., personal attributes of the caregivers, clients’ behavioral repertoire, heavy workload), caregivers need organizational support and training to address the issues that affect their quality of life.
A variety of interventions have been developed and evaluated for their effects on enhancing the quality of life of caregivers of individuals with ID and ASD, but a majority of these interventions have been with parents and family caregivers (Iadarola et al., 2018; Wang et al., 2022; Yu et al., 2019). The research on interventions designed specifically for professional caregivers is meager and has focused on variations of two intervention strategies. First, the early studies used psychoeducation and cognitive behavioral interventions. These studies focused on reducing work-related stress to enhance the quality of life of professional caregivers (e.g., Gardner et al., 2005; Innstrand et al., 2004; Rose et al., 1998). Second, other studies used Acceptance and Commitment Therapy alone or in combination with other therapies, such as aspects of mindfulness (e.g., McConachie et al., 2014; Noone & Hastings, 2009, 2010) or applied behavior analysis (e.g., Bethay et al., 2013). These studies showed the enhanced quality of life of professional caregivers due to decreased psychological distress following the intervention. All of these studies focused on work-related stress or psychological distress as indicators of enhanced quality of life. Other approaches for enhancing caregivers’ quality of life, such as techniques for avoiding burnout, accessing employee assistance programs, engaging in basic stress management practices, having healthy nutrition, engaging in physical exercise, and utilizing wellness-based practices, have been explored minimally in extant research studies.
There has been some interest in using mindfulness-based programs for enhancing the well-being of professional caregivers of individuals with intellectual and developmental impairments (Hwang & Singh, 2016; Myers et al., 2014). Other than for an early study by Brooker et al. (2013) that reported mixed results with a customized occupational mindfulness program, the best evidence for the utility of mindfulness-based programs comes from a series of studies that evaluated the effects of Mindfulness-Based Positive Behavior Support (MBPBS) on caregiver and client outcomes. Generally, caregivers trained in providing behavioral mindfulness services have reported significant reductions in their levels of perceived stress, secondary traumatic stress, and burnout and an increase in compassion satisfaction (Singh et al., 2015; Singh et al., 2016a, 2016b). Furthermore, in a comparative study, the MBPBS program was reported to be significantly more effective on caregiver outcomes than PBS alone in a randomized controlled trial (RCT; Singh et al., 2020a).
MBPBS is a behavioral mindfulness program consisting of two evidence-based components—mindfulness and positive behavior support (Singh et al., 2020b). Singh et al. (2020c) examined whether the mindfulness component of MBPBS by itself could enhance the quality of life of professional caregivers without using the PBS component to increase their expertise in managing the behavior of their clients. In a three-arm RCT, the effects of the mindfulness component of the MBPBS program were assessed against an active treatment condition (i.e., psychoeducation) and a control condition (i.e., inservice training-as-usual). Results showed that mindfulness practice was generally superior to psychoeducation in enhancing the quality of life of the caregivers, and no appreciable change was evidenced in the control condition. Quality of life outcomes were assessed in terms of the caregivers’ self-reported perceived psychological stress, compassion satisfaction, burnout, secondary traumatic stress, and symptoms of depression.
The outcome measures used in studies on the quality of life of caregivers have included clinical indices that are of some importance to the target participants. But there remains the question of whether enhancing the quality of life of caregivers may have spillover or cascading effects on standard quality assurance indicators used by agencies that employ them. These indicators may show benefits from a systems perspective due to the caregivers’ enhanced quality of life. Essentially what is needed are data attesting to changes in the behavior of both caregivers and clients that may result from mindfulness training of caregivers. The present study provides such data from a system’s perspective based on caregiver training reported in the Singh et al. (2020c) RCT. The aim is to provide a secondary analysis of agency data related to the Singh et al. (2020c) study on caregiver quality of life variables obtained from the Human Resources Department and client variables obtained from the Quality Assurance Department.
Method
Participants
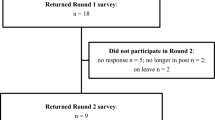
Detailed information on participants and procedures reported in the original study by Singh et al. (2020c) are briefly summarized here to provide the context for this study. A total of 216 caregivers were randomized into a mindfulness program, a psychoeducation program, or a control group program (i.e., inservice training-as-usual). Seventy-two participants were assigned to each experimental condition, clustered by group homes to avoid contamination of training across the three experimental conditions. Each group home had 6 caregivers, and thus, 12 clusters were assigned to each experimental condition. Those who participated in the mindfulness condition had an average age of 40.68 years (range = 19 to 61), had an average service of 15.11 years (range = 1 to 37), and included 42 females. Those in the psychoeducational condition had an average age of 37.89 years (range = 19 to 61), had an average service of 13.76 years (range = 1 to 35), and included 38 females. The participants in the control condition had an average age of 39.61 years (range = 19 to 61), had an average service of 15.17 years (range = 1 to 39), and included 39 females. There were no statistically significant differences in age, years of service, or sex distribution across the three groups (p > 0.05). Some participants in each experimental condition were lost during implementation, i.e., 3, 5, and 9 in the mindfulness, psychoeducation, and inservice training-as-usual conditions, respectively. Figure 1 presents a CONSORT participant flow diagram.
Procedure
Experimental Design
A three-arm cluster RCT design was used, with two active experimental conditions and a control condition: a mindfulness program, a psychoeducation program, and an inservice training-as-usual program. Training in each of the three programs was for 3 days, followed by implementation of the programs for 32 weeks.
Experimental Conditions
Mindfulness Program. The mindfulness experimental condition used the 3-day stepped-care mindfulness component from the full MBPBS program to teach basic meditations and related contemplative practices (Singh et al., 2020b). The mindfulness program included the following standard Buddhist meditation practices: (1) Samatha, walking, and insight meditations; (2) five hindrances (i.e., sensory desire, ill will, sloth and torpor, restlessness and remorse, and doubt); (3) the four immeasurables (i.e., lovingkindness, compassion, empathetic joy, and equanimity [equipoise]); (4) the three poisons (i.e., attachment, anger, and ignorance [doubt]); (5) beginner’s mind; (6) informal mindfulness practices; and (7) practicing ethical precepts (e.g., refrain from harming anyone, taking that which is not given, and incorrect or false speech). Following instructions in the meditation practices, the caregivers were encouraged to develop a daily formal meditation practice for about 20 min that involved focused meditation and different combinations of the other meditations.
Psychoeducational Program. A psychoeducational program was developed specifically for this condition. The program had two key functions. First, it was designed to teach caregivers key aspects of workplace stress, how to recognize it, and how to reduce it. Second, it was designed to educate caregivers on how to meet the needs of individuals with ID and ASD. This included information on positive methods of responding to the behavioral excesses and deficits of the individuals and their social and instructional relationships with the individuals. The program emphasized the following: (1) how to relate skillfully with the individuals (i.e., effective communication that is positive, attentive, and nonjudgmental); (2) how to be accepting of the individual, especially when they are engaged in behaviors that the caregivers found challenging to manage (i.e., reducing automatic negative responses, no use of aversive or punishing consequences, responding in a calm manner that showed the caregiver understood the behavioral functions of the challenging behaviors, as well as the role of emotion dysregulation in their behavior); and (3) how to use evidence-based and practice-based evidence for the treatment of individuals with ID and ASD.
Inservice Training-as-Usual Program. The agency responsible for the group homes provided their standard inservice training on the care and management of individuals with ID and ASD, as well as booster sessions to supplement the new employee training. The yearly updated training curriculum included (1) behavior management; (2) crisis intervention plans; (3) 1-on-1 staffing interventions; (4) emergency medications for severe aggressive behavior to self, peers, and staff; (5) physical restraints; (6) aversive contingencies and punishment strategies; and (7) skills training. All newly employed caregivers receive the basic and supplemental new employee training regardless of additional program-specific training that they may later receive as employees of the agency. Thus, the caregivers in all three arms of the study had received the standard inservice training as part of their new employee training. The caregivers in the control condition received an additional three days of Inservice Training-as-Usual program to equalize the training conditions across the three arms of the study.
Measures
Data on caregiver quality of life variables were obtained from the agency’s Human Resources Department personnel file. These data were recorded by each caregiver’s supervisor and verified by staff from the Human Resources Department. Data on client quality of life variables were obtained from the agency’s Quality Assurance Department. The data were verified by the group home supervisor or discipline-specific supervisors for occurrence and accuracy of reporting.
Caregiver Variables
Progressive Discipline. This was used as a risk management system by the agency. It allowed and supported a caregiver disciplinary system that provided a graduated range of agency responses to unsatisfactory employee performance or behavioral issues. By policy, progressive discipline consisted of a 5-step process that included a verbal warning, a written warning, a poor performance evaluation, a performance improvement plan, and separation (i.e., termination).
Call-In. This was defined as an unplanned absence on a specific day when a caregiver calls in as soon as possible but no less than 2 h before the start of the shift to notify their immediate supervisor of an absence from work. It also included unscheduled leave requests.
Days Absent. This was defined as unauthorized absence from work beyond legitimate requests for unplanned leave (e.g., family and/or medical issues) or unexpected events (e.g., car problems).
Medical Referral. This was defined as a written order from the caregiver’s primary care doctor or specialist clinical professional (e.g., psychiatrist) to obtain specified medical services due to work-related issues.
Hospitalization. This was defined as the level of care in a hospital as an inpatient requiring at least an overnight stay due to work-related issues.
Caregiver Turnover. This was defined as caregiver separation from the agency due to work-related issues. Separation due to regular life events, such as family relocation, were not counted as caregiver turnover.
Client Variables
Learning Objectives. These were defined as the learning objectives specified in the client’s Individualized Support Plan (ISP), which was developed by the treatment team to reflect the clinical and support needs of the client. Caregivers provided instructions as specified in the client’s ISP and recorded each learning objective that was mastered to competency by the client. Identified skills for the client were task analyzed, and each component was defined as a learning objective. Mastery criterion was provided by discipline staff (e.g., psychology, physical therapy, occupational therapy, etc.) responsible for developing the learning objective.
Behavioral Episodes. These were defined as a client hitting, biting, scratching, punching, kicking, slapping, or destroying property. Caregivers recorded each instance of a behavioral event on an incident reporting form at the point of occurrence and entered it in the agency’s incident management database.
Use of Physical Restraints. This was defined as a brief physical hold of an aggressive client by a caregiver when there was imminent danger of physical harm to the client, peers, or staff and when the behavior could not be controlled with verbal redirection. Caregivers recorded each instance of the use of physical restraint at the point of occurrence and entered it in the agency’s incident management database.
Emergency (Stat) Medication. Emergency medication was prescribed by a physician and administered by a registered nurse for behavioral or psychiatric emergencies. These medications were not prescribed for medical or other conditions. Emergency medication was prescribed for the calming of a client who was aggressive and could not be managed by other means, including physical restraints. Each administration was counted as one event as recorded by a registered nurse in the client’s Medication Administration Record.
Medical Emergencies. This was defined as a medical event that required medical examination by a physician or a nurse practitioner, as needed. It excluded those events that required only first aid treatment or resulted in hospitalization. Each medical emergency was recorded by a physician or a nurse practitioner in the client’s medical records.
Hospitalizations. This was defined as a level of care in a hospital as an inpatient requiring at least an overnight stay due to behavioral or psychiatric issues and excluded those for medical or other conditions. Each hospitalization was recorded by a registered nurse in the client’s medical records.
Aggression to Staff. This was defined as any aggressive act by a client directed at a caregiver, with physical contact, requiring medical examination, first aid, or medical care. Each instance of staff injury was recorded on an incident reporting form at the point of occurrence and entered in the agency’s incident management database.
Aggression to Peers. This was defined as any aggressive act by a client directed at a peer, with physical contact, requiring medical examination, first aid, or medical care. Each instance of peer injury was recorded on an incident reporting form at the point of occurrence and entered into the agency’s incident management database.
Level of Supervision. This was defined as the level of supervision when a client’s aggressive or destructive behavior could not be managed through clinical interventions, and the safety of the client, staff, and peers was in question. It included enhanced level of supervision (i.e., 1-to-1 or 2-to-1 staffing) required that was ordered by a physician or clinical psychologist as determined by the client’s treatment team and documented in the client’s treatment plan.
Data Analyses
The main goal of the data analyses was to evaluate the differences across three experimental conditions in terms of caregiver and client outcome variables. Considering that the caregiver and client outcome variables represent ratio-level data, a group count for an entire condition was used instead of a count for individuals within a condition because traditional analyses for RCTs were deemed unsuitable for this study (Singh et al., 2020c). The primary reason for this is that the variables are not at the individual level, which would be required for standard RCT analyses.
To address this challenge, change across time within each condition was examined by treating each group as an n of 1. This approach enabled the computation of the count of each variable for each condition including means and SD across the 32 weeks of the study, thereby ensuring a robust analysis of the differences between conditions. Analysis of variance (ANOVA) was employed to compare the three groups. This method was chosen due to its ability to handle ratio-level data and its suitability for comparing multiple groups simultaneously. Additionally, ANOVA accounts for variance within and between groups, making it a highly reliable statistical tool for analyzing the data in this study.
Following the ANOVA, post-hoc tests were conducted to further explore the differences between the three experimental conditions. We used Welch’s ANOVA to address unequal variances across groups and Bonferroni adjustment for the number of post-hoc tests. These tests helped to identify the specific pairs of conditions that were significantly different from one another, thus providing a more detailed understanding of the results. Statistical significance was determined using a p-value threshold of <0.05. This criterion is widely accepted within the scientific community and ensures that any observed differences between groups are unlikely to have occurred by chance alone. The effect sizes were estimated using partial eta squared (η2), a measure indicating the proportion of total variance in the dependent variable attributable to each independent variable while controlling for others. Following Cohen (1988), an effect size of 0.01 was considered small, 0.06 medium, and 0.14 large. These thresholds provided an assessment of the practical significance of our findings beyond mere statistical significance.
Results
Figure 2 displays the average scores of adverse caregiver outcomes during 32 weeks following training in the mindfulness, psychoeducation, and control groups. Overall, the mindfulness group experienced notably lower levels of adverse caregiver outcomes compared to the psychoeducation and control groups. The control group, on the other hand, had higher adverse outcome levels than the psychoeducation group. Table 1 presents Welch’s ANOVA results, which support the outcomes shown in Fig. 2. As illustrated in Fig. 2A,B, significant differences were found in the average incidence of progressive discipline and call-ins among the three experimental conditions, with a large effect size. Post-hoc tests revealed that the mindfulness group had a significantly lower incidence of progressive discipline and call-ins compared to both the psychoeducation and control groups. Moreover, the control group had a significantly higher number of incidences compared to the psychoeducation group. As shown in Fig. 2C,D, group effects were also significant for the number of days absent from work (large effect size) and the number of medical referrals (large effect size). However, no significant differences were found between the mindfulness and psychoeducation groups for these variables. The control group, in contrast, had a significantly higher number of absent days and medical referrals compared to both the psychoeducation and mindfulness groups. There was no significant group effect for hospitalizations (Fig. 2E), but a significantly medium group effect was observed for caregiver turnover (Fig. 2F). Post-hoc tests indicated that the mindfulness group had significantly lower caregiver turnover compared to the control group, with no significant differences between the mindfulness and psychoeducation groups or the psychoeducation and control groups.
Figure 3 shows the average scores of client outcomes for the three experimental conditions, with supporting statistical tests presented in Table 1. Figure 3A demonstrates that the mindfulness group had a higher rate of achieving learning objectives compared to the psychoeducation and control groups. These group differences were significant with a large effect size, while no significant difference was found between the psychoeducation and control groups, both of which had significantly lower rates compared to the mindfulness group. In contrast, the mindfulness group experienced significantly fewer behavioral episodes than both the psychoeducation and control groups, which showed no significant difference from each other (Fig. 3B).
The group effect was significant and large for the use of physical restraints (Fig. 3C) and the administration of Stat medication (Fig. 3D). The mindfulness group exhibited significantly lower occurrences compared to the psychoeducation and control groups, while the control group had a significantly higher occurrence compared to the psychoeducation group. Medical emergencies were more frequent in the control group compared to both the mindfulness and psychoeducation groups, which showed no significant difference, as indicated by ANOVA and post-hoc tests and illustrated in Fig. 3E.
Hospitalizations, aggression toward peers, and the required level of supervision were significantly different across groups, with the control group being significantly higher compared to both the psychoeducation and mindfulness groups, as indicated in Table 1 and illustrated in Fig. 3F,H,I. However, no statistical differences were found between the mindfulness and psychoeducation groups for hospitalizations. In contrast, the mindfulness group exhibited less aggression toward peers and required significantly less supervision compared to the psychoeducation group. There was no significant group effect for aggression toward staff (Fig. 3G) between the mindfulness and psychoeducation groups, but it was significantly lower in the mindfulness group when compared to the control group.
Discussion
The results of Singh et al. (2020c) showed that the mindfulness component of the MBPBS program was significantly better at enhancing caregiver compassion satisfaction and in reducing caregiver-perceived psychological stress, burnout, secondary traumatic stress, and symptoms of depression when compared to psychoeducation and inservice training-as-usual. These findings were aligned with those in another component analysis study with caregivers (Singh et al., 2020a), which showed that the full MBPBS program was more effective than the PBS component alone in enhancing caregiver compassion satisfaction and in decreasing caregiver perceived psychological stress, burnout, and secondary traumatic stress. These studies showed that mindfulness-based training resulted in clinical benefits for caregivers.
The present study provides secondary data from a system’s perspective. Agency-wide data are typically collected by Human Resource Department and Quality Assurance personnel related to the behavioral health workforce as part of their standard operating procedures. The data are used to assess how well the caregiving staff are keeping pace with changing clinical practices, the need for continued inservice training in new and innovative treatment strategies, and the effectiveness of administrative practices designed to prevent caregivers from experiencing adverse clinical outcomes and burnout. The data collected varies across agencies that provide similar services but generally includes both caregiver and client outcome variables. Thus, the present study can be easily replicated with different interventions or across different agencies because caregiver and client data are usually collected agency-wide in community and other residential settings for individuals with ID and ASD.
The human resource and quality assurance data collected by the agency during caregiver training in mindfulness, psychoeducation, and inservice training-as-usual included six caregiver and nine client variables. Overall, when compared to the standard inservice training, the outcomes for both caregivers and clients were significantly better in mindfulness and psychoeducation training conditions. When compared to psychoeducation training, caregiver outcomes during the mindfulness training were significantly better for progressive discipline and call-ins and equivalent for days absent from work, referrals for medical care, and caregiver turnover. In addition, no significant difference was found for caregiver hospitalizations across the three conditions, probably because the number of caregiver hospitalizations agency-wide was very low to begin with. When compared to psychoeducation training, client outcomes during the mindfulness condition were significantly better for mastery of learning objectives, number of behavioral episodes, use of physical restraints and Stat medication for aggressive behavior, aggression to peers, and level of supervision. These outcomes were equivalent for medical emergencies, hospitalizations, and aggression to staff, which were all low-frequency behaviors at baseline.
These findings hold substantial significance for caregivers and clients alike, as they suggest that incorporating mindfulness-based practices into the caregiving environment not only enhances the well-being of caregivers but also improves the quality of care provided to individuals with ID and ASD. By adopting mindfulness-based strategies, caregivers may be better equipped to handle the challenges associated with their roles, ultimately fostering a more supportive and nurturing atmosphere for the clients they serve.
We suspect that mindfulness-based interventions produce cascading effects that may work at two levels. First, when caregivers are trained in mindfulness, their clients are able to detect the positive behavioral changes in their caregivers and are responsive to the new contingencies. This is an example of external cascading of the behavior of caregivers to their clients without any specific training being provided to the clients. Second, the positive behavioral changes that clients observe in their caregivers could have occurred as a result of the wisdom that arises due to the daily meditation practice of the caregivers. This wisdom enhances the awareness of the caregivers of their own behaviors and enables them to be responsive to the clients in a kind, compassionate, loving, and generally positive manner. The nature of these behavioral changes in the caregivers can be analyzed on a moment-by-moment basis through behavior analytic methodologies (Singh et al., 2023). This is an example of the internal cascading of the effects that mindfulness training produces in caregivers, which is strengthened and grows with continued meditation practice. Neither external nor internal cascading of training effects appear to have been reported for psychoeducation or other interventions generally used with caregivers.
Limitations and Future Research
The key limitation of this study is that the data were collected by, and supervision of the data collection was undertaken by, multiple management staff, as would be expected in an agency quality assurance system. This means that data reliability may be a limiting factor when interpreting the results. Primary supervisors in each group home were responsible for checking the occurrence of events and the accuracy of reporting the data, but the use of substitute supervisors in the absence of the primary supervisor may have occasioned discrepancies in the data collection system. However, data from previous studies using the full MBPBS program which utilized trained experimenters to collect the data have shown similar findings for some of the variables included in the present study. For example, similar findings were reported for staff turnover, staff injuries, peer injuries, use of physical restraints, and Stat medication (Singh et al., 2015, 2016a, 2016b, 2020a). There are two caveats that should be noted. First, there is no way of knowing if the frequency and number of events for specific variables were commensurate across the current and previous studies. Future studies could examine this issue by comparing experimenter vs. agency-collected data for the same caregiver and client variables. Second, the current study examined agency data when the caregivers in the mindfulness group were trained in only the mindfulness component of MBPBS as opposed to the full MBPBS program in previous studies.
A possible confounding factor in the present study could have been the caregivers’ previous training and experience in terms of the use of certain interventions (e.g., physical restraints, stat medication). By policy, all caregiving staff in agencies are provided inservice training at intake and then yearly on all quality assurance variables, including treatment modalities. Future research could investigate how previous training and experience may impact the quality of care provided by each caregiver as measured in the quality assurance process. Finally, the present findings cannot be generalized across healthcare agencies except in terms of the general trends in the data because of the heterogeneity of policies, procedures, and the breadth and definitions of the variables for which data are collected. At best, future studies could examine variability in quality assurance data across settings within an agency.
The use of psychoeducation as an active control condition and inservice training as the control condition is a methodological strength (Davidson & Kaszniak, 2015), but it is likely that the psychoeducation group was not a true active control or comparison condition. Theoretically, the active control condition should match the experimental condition on all non-specific factors without including any specific components of the active condition. Psychoeducation in this study matched non-specific factors but also included some specific aspects of the mindfulness program, such as being nonjudgmental and accepting of the clients even when they exhibited challenging behaviors. The overlap in specific components in the two programs may have contributed to the finding that the mindfulness program showed significant improvement in some variables but was equivalent in others when compared to psychoeducation. Future research should focus on using comparison conditions that match the experimental condition on all essential variables that impact outcomes. This study is informative in terms of global changes that may occur at the agency level as a consequence of training caregivers in different self-care models, but further investigation is needed to truly understand the nature and extent of these changes.
References
Beighton, C., & Wills, J. (2019). How parents describe the positive aspects of parenting their child who has intellectual disabilities: A systematic review and narrative synthesis. Journal of Applied Research in Intellectual Disabilities, 32, 1255–1279. https://doi.org/10.1111/jar.12617
Bethay, J. S., Wilson, K. G., Schnetzer, L. W., Nassar, S. L., & Bordieri, M. J. (2013). A controlled pilot evaluation of acceptance and commitment training for intellectual disability staff. Mindfulness, 4, 113–121. https://doi.org/10.1007/s12671-012-0103-8
Brooker, J., Julian, J., Webber, L., Chan, J., Shawyer, F., & Meadows, G. (2013). Evaluation of an occupational mindfulness program for staff employed in the disability sector in Australia. Mindfulness, 4, 122–136. https://doi.org/10.1007/s12671-012-0112-7
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Erlbaum.
Davidson, R. J., & Kaszniak, A. W. (2015). Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist, 70(7), 581–592. https://doi.org/10.1037/a0039512
Gardner, B., Rose, J., Mason, O., Tyler, P., & Cushway, D. (2005). Cognitive therapy and behavioural coping in the management of work-related stress: An intervention study. Work and Stress, 19, 137–152. https://doi.org/10.1080/02678370500157346
Hastings, R. P., & Horne, S. (2004). Positive perceptions held by support staff in community mental retardation services. American Journal of Mental Retardation, 109(1), 53–62. https://doi.org/10.1352/0895-8017(2004)109<53:PPHBSS>2.0.CO;2
Hensel, J. M., Lunsky, Y., & Dewa, C. S. (2012). Exposure to client aggression and burnout among community staff who support adults with intellectual disabilities in Ontario, Canada. Journal of Intellectual Disability Research, 56(9), 910–915. https://doi.org/10.1111/j.1365-2788.2011.01493.x
Hwang, Y-S., & Singh, N. N. (2016). Mindfulness. In N. N. Singh (Ed.), Handbook of evidence-based practices in intellectual and developmental disabilities (pp. 311-346). Springer.
Iadarola, S., Levato, L., Harrison, B., Smith, T., Lecavalier, L., Johnson, C., Swiezy, N., Bearss, K., & Scahill, L. (2018). Teaching parents behavioral strategies for autism spectrum disorder (ASD): Effects on stress, strain, and competence. Journal of Autism and Developmental Disorders, 48, 1031–1041. https://doi.org/10.1007/s10803-017-3339-2
Innstrand, S. T., Espnes, G. A., & Mykeltun, R. (2004). Job stress, burnout, and job satisfaction: An intervention study for staff working with people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 17, 119–126. https://doi.org/10.1111/j.1360-2322.2004.00189.x
McConachie, D. A. J., McKenzie, K., Morris, P. G., & Walley, R. M. (2014). Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Research in Developmental Disabilities, 35, 1216–1227. https://doi.org/10.1016/j.ridd.2014.03.005
Mutkins, E., Brown, R. F., & Thorsteinsson, E. B. (2011). Stress, depression, workplace supports and burnout in intellectual disability support staff. Journal of Intellectual Disability Research, 55(5), 500–510. https://doi.org/10.1111/j.1365-2788.2011.01406.x
Myers, R. E., Winton, A. S. W., Lancioni, G. E., & Singh, N. N. (2014). Mindfulness in developmental disabilities. In N. N. Singh (Ed.), Psychology of meditation (pp. 209–240). Nova Science.
Noone, S. J., & Hastings, R. P. (2009). Building psychological resilience in support staff: Pilot evaluation of an acceptance-based intervention. Journal of Intellectual Disabilities, 13(1), 43–53. https://doi.org/10.1177/1744629509103519
Noone, S. J., & Hastings, R. P. (2010). Using acceptance and mindfulness-based workshops with support staff caring for adults with intellectual disabilities. Mindfulness, 1, 67–73. https://doi.org/10.1007/s12671-010-0007-4
Panicker, A. S., & Ramesh, S. (2019). Psychological status and coping styles of caregivers of individuals with intellectual disability and psychiatric illness. Journal of Applied Research Intellectual Disabilities, 32(1), 1–14. https://doi.org/10.1111/jar.12496
Rose, J., Jones, F., & Fletcher, C. B. (1998). The impact of a stress management programme on staff well-being and performance at work. Work and Stress, 12, 112–124. https://doi.org/10.1080/02678379808256854
Singh, N. N., Lancioni, G. E., Chan, J., McPherson, C. L., & Jackman, M. M. (2020b). Mindfulness-based positive behavior support. In I. Ivtzan (Ed.), Handbook of mindfulness-based programs: Mindfulness interventions from education to health and therapy (pp. 42–52). Routledge.
Singh, N. N., Lancioni, G. E., Felver, J. C., Myers, R. E., Hwang, Y.-S., Chan, J., & Medvedev, O. N. (2023). Effects of mindful engagement and attention on reciprocal caregiver and client interactions: A behavioral analysis of moment-to-moment changes during mindfulness practice. Mindfulness. Advance of Print.
Singh, N. N., Lancioni, G. E., Karazsia, B. T., Chan, J., & Winton, A. S. W. (2016b). Effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) vs. training-as-usual (TAU): A randomized controlled trial. Frontiers in Psychology, 7, 1549. https://doi.org/10.3389/fpsyg.2016.01549
Singh, N. N., Lancioni, G. E., Karazsia, B. T., & Myers, R. E. (2016a). Caregiver training in mindfulness-based positive behavior support (MBPBS): Effects on caregivers and adults with intellectual and developmental disabilities. Frontiers in Psychology, 7, 98. https://doi.org/10.3389/fpsyg.2016.00098
Singh, N. N., Lancioni, G. E., Karazsia, B. T., Myers, R. E., Winton, A. S. W., Latham, L. L., & Nugent, K. (2015). Effects of training staff in MBPBS on the use of physical restraints, staff stress and turnover, staff and peer injuries, and cost effectiveness in developmental disabilities. Mindfulness, 6, 926–937. https://doi.org/10.1007/s12671-014-0369-0
Singh, N. N., Lancioni, G. E., Medvedev, O. N., Hwang, Y.-S., Myers, R. E., & Townshend, K. (2020c). Using mindfulness to improve quality of life in caregivers of individuals with intellectual disabilities and autism spectrum disorder. International Journal of Developmental Disabilities, 66(5), 370–380. https://doi.org/10.1080/20473869.2020.1827211
Singh, N. N., Lancioni, G. E., Medvedev, O. N., Myers, R. E., Chan, J., McPherson, C. L., Jackman, M. M., & Kim, E. (2020a). Comparative effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) and positive behavior support (PBS) in a randomized controlled trial. Mindfulness, 11(1), 99–111. https://doi.org/10.1007/s12671-018-0895-2
Sit, H. F., Huang, L., Chang, K., Chau, W. I., & Hall, B. J. (2020). Caregiving burden among informal caregivers of people with disability. British Journal of Health Psychology, 25(3), 790–813. https://doi.org/10.1111/bjhp.12434
Wang, R., Liu, Q., & Zhang, W. (2022). Coping, social support, and family quality of life for caregivers of individuals with autism: Meta-analytic structural equation modeling. Personality and Individual Differences, 186, 111351. https://doi.org/10.1016/j.paid.2021.111351
Yu, Y., McGrew, J. H., & Boloor, J. (2019). Effects of caregiver-focused programs on psychosocial outcomes in caregivers of individuals with ASD: A meta-analysis. Journal of Autism and Developmental Disorders, 49, 4761–4779. https://doi.org/10.1007/s10803-019-04181-z
Acknowledgements
The authors acknowledge with much gratitude the support and assistance of the agency and staff for their participation.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
Nirbhay N. Singh: conceptualization, methodology, investigation, data collection and curation, writing, reviewing, editing, and revisions. Giulio E. Lancioni, Yoon-Suk Hwang, Rachel E. Myers, Kishani Townshend: writing, reviewing, and editing. Oleg N. Medvedev: data analyses, validation, writing, reviewing, and revisions.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all caregivers and either clients or their guardians.
Conflict of Interest
NNS is the developer of the Mindfulness-Based Positive Behavior Support (MBPBS) program.
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, N.N., Lancioni, G.E., Hwang, YS. et al. Using Mindfulness to Improve Quality of Life in Caregivers of Individuals with Intellectual Disabilities and Autism Spectrum Disorder: Agency Outcomes for Caregivers and Clients. Adv Neurodev Disord 7, 604–615 (2023). https://doi.org/10.1007/s41252-023-00353-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-023-00353-2