Abstract
Objectives
People with intellectual and developmental disabilities (IDD) and autism are subject to restrictive practices like physical restraint and the overuse of psychotropic medications for challenging behavior. People with disabilities and their families are often not involved in shared decision-making for prescription and other care planning, which may violate the UN Human Rights Charter.
Methods
One way of reducing overmedication is by empowering adults with IDD and their family caregivers to collaborate in the decision to use medications. SPECTROM (https://spectrom.wixsite.com/project), a training program for direct care workers, was developed to help reduce the overmedication of these people. This article presents ideas on how SPECTROM resources could empower adults with IDD and their families to influence their care decisions, including psychotropic prescribing.
Results
Information provided in 32 easy-read leaflets in SPECTROM on psychotropic medications can be used to improve shared decision-making involving people with IDD and their families. Similarly, the Yellow Passport, an easy-read health record, could help information sharing among care service providers, thus improving their health care. SPECTROM has one module devoted to effectively engaging with people with IDD to improve their communication and help them with their skills building.
Conclusions
Currently, very limited evidence exists on the effects of SPECTROM to empower individuals with IDD and their families in reducing psychotropic medications for challenging behaviors. In addition to the two pilot studies on SPECTROM from UK and Australia, further research is needed to explore the evidence supporting the above suggestions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
People with disabilities are vulnerable to being affected by the violations of the United Nations Convention on the Rights of Persons with Disabilities (CRPD) (United Nations, 2008). This is evident from the fact that people with neurodevelopmental disorders (NDDs) such as intellectual and developmental disabilities (IDD) and autism spectrum disorder (ASD) are often subjected to restrictive practices such as physical restraint and inappropriate prescribing of psychotropic medications. Approximately half of the adults with IDD (Deb et al., 2023) and a similar proportion with ASD (Bertelli et al., 2022) are prescribed psychotropic medications such as antipsychotics, antidepressants, mood stabilizers, and anti-anxiety medications. These medications are indicated for the treatment of various psychiatric disorders. However, in people with IDD and ASD, these medications are often used outside their licensed indication to treat challenging behavior (Deb et al., 2023).
For example, antipsychotics are prescribed for 24–32% of adults with IDD compared with 1% in the general population who do not have IDD (Deb et al., 2023). However, only 2–4% of adults with IDD have a diagnosis of schizophrenia for which antipsychotics are primarily indicated (Deb et al., 2022a). Therefore, antipsychotics are used for psychosis among only 22% of adults with IDD, and in 72% of cases, no severe psychiatric illness is present. On the other hand, antipsychotics are used 58% of the time for challenging behavior (de Kuijper et al., 2010; Sheehan et al., 2015). Similarly, 45% of people with IDD with challenging behavior receive antipsychotics. Currently, the evidence for the efficacy of off-license psychotropic use for challenging behavior in people with IDD and autism is limited (Alfageh et al., 2019; Deb et al., 2023; Zhou et al., 2021). This inappropriate and excessive off-license use of antipsychotics and other psychotropics for challenging behavior in the absence of a psychiatric diagnosis may lead to a violation of human rights and is a major public health concern.
Challenging behavior (also known as problem behavior, behaviors that challenge, behaviors of concern, etc.) may be displayed by up to 60% of adults with IDD (Deb et al., 2022b). Challenging behavior includes aggression toward others and property, self-injurious behavior, and temper tantrum. The presence of challenging behavior causes distress to people with IDD and their caregivers, and hampers their community integration and, in some cases, exclusion from community activities and loss of community placement, sometimes leading to hospitalization. There are many causes of challenging behaviors, including physical (pain in the body such as headache or toothache, constipation, acid reflux, some genetic disorders, etc.), psychiatric (psychosis, depression, mania, etc.), psychological (stress, trauma, impaired coping strategy, etc.), and environmental (inappropriate environment, lack of support, etc.). Often, challenging behavior is a means of communication for adults with IDD. For example, if they are in pain or distressed and cannot communicate that through speech, they may scream and shout to convey their message (Deb et al., 2022b).
A variety of non-pharmacological interventions have been used to manage challenging behaviors in people with IDD and autism, including behavior analytic treatments (e.g., Luiselli, 2021; Virues-Ortega et al., 2022), positive behavior support interventions (Gore et al., 2022), and more recently mindfulness-based programs (Singh et al., 2021, 2022). Both paid caregivers and family members play a pivotal role in influencing psychotropic prescribing for challenging behavior. Previous studies highlighted the lack of caregivers’ knowledge about the role of psychotropics such as when they could or should not be used, their side effects, monitoring requirements, evidence or lack of it in their support, and the effect of withdrawing these medications (Deb et al., 2022c). Often, individuals with IDD and their families are not involved in decision-making, such as psychotropic prescriptions or withdrawal (Deb & Limbu, 2022).
In the UK, a training resource, Short-term PsychoEducation for Carers To Reduce Over Medication of people with intellectual disabilities (SPECTROM) (https://spectrom.wixsite.com/project), was developed to address the issues mentioned earlier in relation to caregiver influence on prescribing (Deb et al., 2020, 2021). SPECTROM has 14 online modules that are introduced through two core modules during two face-to-face training workshops. The “Medication” core module provides caregivers detail knowledge of psychotropics, including their indications and side effects, monitoring requirements, and effects on withdrawal. SPECTROM encourages direct care staff team members to run their in-house information gathering/reviews on the effect and side effects of the interventions for challenging behavior regularly. The “Alternatives to Medication” core module teaches staff alternative ways to address challenging behavior without using medication. This article discusses how training direct care staff in the use of SPECTROM may be effective in empowering adults with IDD and their families to gradually reduce the prescription of off-label psychotropic medications for challenging behaviors.
SPECTROM Pilot Studies
Twenty staff received SPECTROM training in a pilot study in the UK (Deb et al., 2021). The Management of Aggression and Violence Attitudes Scale-Revised-Intellectual Disabilities (MAVAS-R-ID) (Duxbury, 2003) was used to assess trainees’ attitude toward challenging behavior, and a revised version of the psychotropic knowledge questionnaire (PKQ-R) (de Kuijper & Putten, 2017) to assess trainees’ knowledge of psychotropics. A semi-structured interview and a trainee feedback questionnaire (TFQ) were used for process evaluation. After training, MAVAS-R-ID scores showed a statistically significant (p < 0.05) improvement in staff attitude to “medication management” domain. PKQ-R scores showed post-training improvement in all domains, 50% of which were statistically significant (p < 0.05). TFQ and the process evaluation data showed that SPECTROM was acceptable, applicable, practical, and relevant to staff practice, and helped to improve self-reflection, knowledge, and confidence in supporting people with IDD.
Forty-two participants received SPECTROM training in a recent Australian pre-post pilot study (Wilson et al., 2023). PKQ-R scores showed statistically significant post-training improvement at all post-training time points (p < 0.05). MAVAS-R-ID scores were high at pre-training and did not change significantly at any of the post-training survey time points. A 2-week post-training TFQ reported 80% agreement that the training program was appropriate, useful, and valid. Process evaluation involving interviews revealed four main themes: (a) broad satisfaction with the SPECTROM training program, (b) empowering staff through reflective practice, (c) the limitations of their scope of practice, and (d) the need for multi-disciplinary team (MDT) involvement (Barratt et al., 2023).
Empowering People with IDD and Their Families
Training direct care staff to empower people with IDD and their families via SPECTROM may reduce overprescription of off-label psychotropic medication for challenging behaviors. In doing so, it may impact a number of articles in the UN convention on CRPD (United Nations, 2008). These include articles 15 (degrading treatment or punishment), 16 (abuse), 17 (the integrity of the person), and 25 (health). The other articles that may be indirectly affected include 5 (equality and non-discrimination), 9 (accessibility), 19 (independent living and community inclusion), 21 (access to information), 24 (education), 26 (rehabilitation), 27 (work and employment), 28 (adequate living standard), and 30 (participation in recreation and leisure). Given the rather limited evidence base for the utility of SPECTROM in this context, the discussion centers around what is possible rather than what can be definitely achieved.
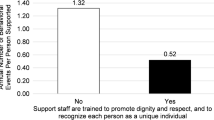
The SPECTROM module, “Effective engagement with people with IDD,” encourages direct care staff to understand better the person with disabilities they support by knowing their strengths and weaknesses, and likes and dislikes, which is crucial to build a rapport with the person and engage with them effectively. Effective engagement is important to improve a person’s quality of life. The module also encourages caregivers to know the communication needs of the person with disabilities to communicate using the most appropriate means. Another important element of the module is encouraging caregivers to support and help the person with disabilities to develop skills by drawing the right balance between allowing independence and managing risks.
The module suggests that the direct care staff should create opportunities for engagement and interaction to enhance effective engagement with people with disabilities. Other suggested ways to increase engagement are to spend time together in activities that the person with disabilities enjoys, use opportunities to interact during these activities, approve and encourage their activities (where appropriate), try to complete one enjoyable shared activity every day, use intensive interaction where appropriate, and allow consistency in approach. It is envisaged that these actions should make the person with disabilities engage more with the direct care staff, and any positive interaction will improve their relationship with the person they support.
A separate module in SPECTROM is devoted to the “Communication needs.” This module teaches caregivers different types of communication needs in people with IDD, ways to help the person communicate effectively, how to adjust the caregiver’s communication style to match the person’s needs and to recognize that some behavior could be a means of communication, and how to address these behaviors.
SPECTROM has developed accessible information leaflets on 32 commonly prescribed psychotropic medications for people with IDD that are available for downloading from the internet free of charge. The caregivers are encouraged to take the person with IDD through these leaflets explaining these medications’ indications, side effects, etc. Often, no one asks the person with IDD about their medication, and these leaflets are designed to involve people with IDD from the outset in their prescribing and other care plans. We envisage that this should improve shared decision-making and empower people with IDD, helping to reduce human rights violations through inappropriate psychotropic prescribing for people with IDD without their consent.
Within SPECTROM, we have developed a new resource, Yellow Passport, a handheld document kept by the person with disabilities containing all their health-related information in an accessible format in one place. As several agencies and professionals are often involved in the care of a person with disabilities, the right information is often not shared among these organizations and professionals at the right time appropriately. This hampers the quality of care. It is envisaged that the Yellow Passport should overcome this problem as the document will be updated regularly by direct care staff and families and carried by the person with disabilities to all places, they visit to receive care.
Although SPECTROM resources were primarily designed for direct care staff training, it is envisaged that they should be equally helpful for family caregivers. SPECTROM has one module on the “Effective engagement with families,” which advises staff on improving their relationships and engagements with family caregivers. Whereas direct care staff and other professionals come and go, the families are the constant presence in the lives of people with disability who know the person with disability best. Yet, the families often feel left out (Deb & Limbu, 2022) and uninvolved in the shared decision-making process for prescribing and other care planning, including restrictive practices for their loved ones. It is envisaged that this module should empower family caregivers by improving shared decision-making and allowing them to have a say in the treatment and care planning of their loved ones. This, in turn, is likely to reduce human rights violations.
The module emphasizes the need for appropriate information sharing in a timely manner using a language understandable to family caregivers so that they should receive both good and bad news. Keeping a written record of what has been discussed in the family caregiver’s presence is desirable. SPECTROM recommends that the family caregivers be given appropriate information on managing challenging behavior in their loved ones, including pharmacological and non-pharmacological interventions. These should include information sharing on psychotropic treatment, their side effects, and the potential effect on withdrawal. It is envisaged that the use of accessible medication leaflets by family caregivers should enhance shared decision-making.
This module suggests that where there is a conflict of opinion between families and staff and/or other professionals about the care of a person with disabilities, an attempt should be made in the first instance to resolve this through an open and honest discussion. It is worth remembering that all stakeholders involved have the person’s best interests in mind. If all efforts fail, an independent professional advocate may be appointed to safeguard the interest of the person with disabilities. In extreme cases, the legal system may have to be involved, which should be avoided if possible.
The module recommends that the families, where possible, should be involved in decision-making about their loved ones’ care planning, including prescribing medications from the outset. They should be appropriately supported so that their voice is heard if and when they feel intimidated by professionals, particularly in large care planning meetings. Families should be involved in any medication review and informed of all changes in the prescription. It is advised that families should appoint a spokesperson who could communicate on behalf of all family members who should have up-to-date information on the person with disabilities. Similarly, it has been suggested that direct care staff and the multidisciplinary team should have a key person respectively with whom the families could liaise for up-to-date information.
It was highlighted that because of staff turnover and possible changes in the person’s accommodation, families may have to deal with new people all the time, which may be stressful. This should be acknowledged by all staff and professionals involved in caring for the person with disabilities. The module recommends training families on medication-related issues, medication reviews, and the management of challenging behavior. Similarly, it is suggested that families themselves may contribute greatly if they are involved in training staff and other professionals working with people with disabilities.
This module recommends that interpreters should be found when families have language problems, and their cultural needs should be respected. If the family caregiver has any speech problem, an appropriate method of communication, such as the use of accessible information, is required. Family caregivers should be given information or signposted for financial and other service needs, such as respite care, where possible. If possible and desired, connecting families in similar situations will help to improve their confidence in dealing with the care of their loved ones.
Empowering Direct Care Staff
The medication core module provides information on different types of psychotropics, their indications, side effects, monitoring requirements, and the effect of withdrawal of these medications. Knowledge is power. So, we believe that this information should increase staff confidence in dealing with psychotropics and empower them to challenge inappropriate and unnecessary psychotropic prescribing. They should realize they know the person with disabilities best, much better than the professionals caring for them.
The “Medication review” module provides a checklist for the direct care staff to go through when they run their own staff-led in-house medication review, which is not a formal medical review but is arranged in preparation for a formal review by the prescribers. The same module provides a list of information that staff are encouraged to take with them to the clinic, where the prescribers formally review medications. This module also provides a list of questions that staff should and could ask the prescribers. The staff team are advised to run their own review every 6 months unless necessary more frequently, and definitely before a formal medical review in the clinic.
Examples of questions staff could and should ask the prescribers include (a) is the medication making a positive difference? (b) Why was the medication initially prescribed (for challenging behavior or a psychiatric disorder)? (c) Are there any other non-pharmacological management options available? (d) What are the side effects they should look out for? (e) What actions should they take if they see any side effects? (f) What are the monitoring requirements of these medications, such as blood tests? (g) What if the person finds it difficult to swallow the medication? (h) Have there been any changes in the person’s physical or mental health? (i) Is the medication still needed? (j) What is the plan for the eventual reduction or withdrawal of medication?
Both direct care staff and family caregivers are apprehensive about withdrawing psychotropic medications if they have been used for many years because of the fear of potential deterioration of challenging behavior (Deb et al., 2023). SPECTROM has a separate module on “Medication withdrawal review.” This module discusses why it is necessary to consider medication withdrawal or dose reduction, possible reasons for the deterioration in behavior upon withdrawal of medication or dose reduction, issues to consider before starting gradual dose reduction, consideration of factors that may affect withdrawal, evidence from recent withdrawal studies, what to include in a withdrawal plan, and main recommendations for the contingency plan along with a flow chart for a relapse prevention strategy.
The withdrawal process is based on the following principles: (a) empower the person with disabilities and their caregivers through shared decision-making, (b) medication withdrawal review should be part of a wider person-centered care plan, (c) stabilize the person’s behavior on a minimum number of medications prescribed at the lowest possible dose for the shortest period of time, or without medication (d) for a better quality of life of the person with disabilities. The main recommendations in this module are (a) assess factors affecting the withdrawal before starting withdrawal, (b) withdraw one medication at a time slowly and monitor efficacy and side effects, (c) develop and share on a need-to-know basis a relapse plan with consultation with the person with IDD, their families, the care team, and all other stakeholders, (d) if necessary, allow time (sometimes a few weeks) after withdrawing one medication and before starting to withdraw another, (e) consider non-medication-based interventions and re-assess the initial formulation and rationale for using the medication, (f) the prescriber should choose to withdraw the medication with the least benefit first, and (g) the prescriber must check the initial formulation and treatment plan to identify which medication is having a positive effect and which has no effect on the behavior or potentially harmful.
We developed the Comprehensive Assessment of Triggers for Behaviors of Concern Scale (CATS) within SPECTROM (Limbu et al., 2021). CATS has 333 examples of triggers for challenging behavior categorized under five primary contextual categories, (a) external environment, (b) internal environment, (c) expression of volition, (d) characteristics associated with IDD or ASD, and (e) specific activities/events. Each of the main categories is further subdivided into 17 subcategories. Caregivers are supposed to go through the examples of triggers for challenging behavior to detect which ones apply to the person they support. This, in turn, should help with the functional analysis of behavior (Matson et al., 2011).
Effective collaboration among the stakeholders is the key to successful care delivery. Therefore, SPECTROM has developed a module on “Effective engagement with professionals.” This module teaches the caregivers to (a) respect each other’s opinions, (b) treat every member of the multidisciplinary team equally, (c) have a clear understanding of each other’s roles, (d) understand each other’s perspective and point of view, (e) accept that different professionals have expertise in different areas, and they may not understand other’s areas of expertise, (f) understand and accept that everyone’s expertise is important and necessary to provide the person with disabilities with a good quality of life, (g) avoid the use of professional jargons, (h) effective and timely communication with the professionals, and (i) there may be differences in opinion, but true collaborative work is in the best interests of the person with disabilities that every professional is trying to achieve. Regular meetings of multi-professional team members with the direct care staff, the person with disabilities, and their family carer/advocate should help to achieve this goal. Service provider organizations should put in place the right structure and support to facilitate the process of effective liaison with professionals.
Alternatives to Medication (ATM) core module teaches caregivers (a) why some people with IDD display challenging behavior, (b) how understanding the person behind the behavior helps to improve caregivers’ relationship with the person they support, which in turn should help to improve the person’s quality of life, (c) how caregivers’ response to challenging behavior and attitude toward the person displaying the behavior can affect the person’s behavior, and how can caregivers address this issue, and (d) similarly, how can caregivers’ own stress affect the person they support, and how to handle the stress. SPECTROM provides action checklists for managers and organizations to support caregivers and prevent stress among them. SPECTROM provides a simple scale that caregivers can use to regularly assess their mental health status with support from their managers to detect and prevent burnout. This module also teaches caregivers how to effectively engage and communicate with the person with disabilities and help with their skills building, as discussed in the previous sections.
References
Alfageh, B. H., Wang, Z., Mongkhon, P., Besag, F. M., Alhawassi, T. M., Brauer, R., & Wong, I. C. K. (2019). Safety and tolerability of antipsychotic medication in individuals with autism spectrum disorder: A systematic review and meta-analysis. Pediatric Drugs, 21, 153–167. https://doi.org/10.1007/s40272-019-00333-x
Barratt, M., Jorgensen, M., Deb, S., Limbu, B., Donley, M., Buchholtz, M., Smith, V., & Wilson, N. (2023). Staff perceptions following a training program about reducing psychotropic medication use in adults with intellectual disability: The need for a realistic professional practice framework. Journal of Applied Research in Intellectual Disabilities, 36, 486–496. https://doi.org/10.1111/jar.13070
Bertelli, M. O., Azeem, M. W., Underwood, L., Scattoni, M. L., Persico, A. M., Ricciardello, A., Sappok, T., Bergmann, T., Keller, R., Bianco, A., Corti, S., Miselli, G., Lassi, S., Croce, L., Bradley, E., & Munir, K. (2022). Autism spectrum disorder. In M. O. Bertelli, S. Deb, K. Munir, A. Hassiotis, L. Salvador-Carulla (Eds.), Textbook of psychiatry for intellectual disability and autism spectrum disorder (pp. 369–455). Springer Nature. https://doi.org/10.1007/978-3-319-95720-3_16
de Kuijper, G., & van der Putten, A. A. (2017). Knowledge and expectations of direct support professionals towards effects of psychotropic drug use in people with intellectual disabilities. Journal of Applied Research in Intellectual Disability, 30, 1–9. https://doi.org/10.1111/jar.12357
de Kuijper, G., Hoekstra, P., Visser, F., Scholte, F. A., Penning, C., & Evenhuis, H. (2010). Use of antipsychotic drugs in individuals with intellectual disability (ID) in the Netherlands: Prevalence and reasons for prescription. Journal of Intellectual Disability Research, 54(7), 659–667. https://doi.org/10.1111/j.1365-2788.2010.01275.x
Deb, S., & Limbu, B. (2022). Direct care staff liaising effectively with family caregivers: Findings from a co-design event and recommendation for a staff training resource. Frontiers in Psychiatry, 13, 977442. https://doi.org/10.3389/fpsyt.2022.977442
Deb, S., Limbu, B., Crawford, M., & Weaver, T. (2020). Short-term PsychoEducation for Carers To Reduce Over Medication of people with intellectual disabilities (SPECTROM): study protocol. British Medical Journal Open, 10, e037912. https://doi.org/10.1136/bmjopen-2020-037912
Deb, S., Limbu, B., Unwin, G., Woodcock, L., Cooper, V., & Fullerton, M. (2021). Short-term Psycho-Education for Caregivers To Reduce OverMedication of people with intellectual disabilities (SPECTROM): Development and field testing. International Journal of Environmental Research and Public Health, 18, 13161. https://doi.org/10.3390/ijerph182413161
Deb, S., Limbu, B., Unwin, G. L., & Weaver, T. (2022c). Causes of and alternatives to medication for behaviors that challenge in people with intellectual disabilities: Direct care providers’ perspectives. International Journal of Environmental Research & Public Health, 19, 9988. https://doi.org/10.3390/ijerph19169988
Deb, S., Perera, B., Krysta, K., Ozer, M., Bertelli, M., Novell, R., Wieland, J., & Sappok, T. (2022a). The European guideline on the assessment and diagnosis of psychiatric disorders in adults with intellectual disabilities. European Journal of Psychiatry, 36, 11–25. https://doi.org/10.1016/j.ejpsy.2021.10.002
Deb, S., Unwin, G. L., Cooper, S-A., & Rojahn, J. (2022b). Problem behaviors. In M. O. Bertelli, S. Deb, K. Munir, A. Hassiotis, L. Salvador-Carulla (Eds.), Textbook of psychiatry for intellectual disability and autism spectrum disorder (pp. 145–186). Springer. https://doi.org/10.1007/978-3-319-95720-3_7
Deb, S., Roy, M., & Limbu, B. (2023). Psychopharmacological treatments for psychopathology in people with intellectual disabilities and/or autism spectrum disorder. British Journal of Psychiatry Advances, 1–12 (FirstView). https://doi.org/10.1192/bja.2022.61
Duxbury, J. (2003). Testing a new tool: The Management of Aggression and Violence Attitude Scale (MAVAS). Nurse Researcher, 10(4), 39–52. https://doi.org/10.7748/nr2003.07.10.4.39.c5906
Gore, N. J., Sapiets, S. J., Denne, L. D., Hastings, R. P., Toogood, S., MacDonald, A., Baker, P., Allen, D., Apanasionok, M. M., Austin, D., Bowring, D. L., Bradshaw, J., Corbett, A., Cooper, V., Deveau, R., Hughes, J. C., Jones, E., Lynch, M., McGill, P., … Williams, D. (2022). Positive behavioral support in the UK: A state of the nation report. International Journal of Positive Behavioral Support, 12(1), 4–39.
Limbu, B., Unwin, G., & Deb, S. (2021). Comprehensive Assessment of Triggers for Behaviors of Concern Scale (CATS): Initial development. International Journal of Environmental Research and Public Health, 18(10674), 1–33. https://doi.org/10.3390/ijerph182010674
Luiselli, J. K. (2021). Applied behavior analysis treatment of violence and aggression in persons with neurodevelopmental disabilities. Springer.
Matson, J. L., Kozlowski, A. M., Worley, J. A., Shoemaker, M. E., Sipes, M., & Horovitz, M. (2011). What is the evidence for environmental causes of challenging behaviors in persons with intellectual disabilities and autism spectrum disorders? Research in Developmental Disabilities, 32, 693–698.
Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A., & Horsfall, L. (2015). Mental illness, challenging behavior, and psychotropic drug prescribing in people with intellectual disability: UK population-based cohort study. British Medical Journal, 351, h4326. https://doi.org/10.1136/bmj.h4326
Singh, N. N., Lancioni, G. E., & Hwang, Y.-S. (2021). Mindful caregiving and support for anger and aggression management. In J. K. Luiselli (Ed.), Applied behavior analysis treatment of violence and aggression in persons with neurodevelopmental disabilities (pp. 189–202). London: Springer.
Singh, N. N., Lancioni, G. E., Hwang, Y.-S., & Myers, R. E. (2022). Mindfulness: Therapeutic applications for individuals with autism spectrum disorder. In J. L. Matson & P. Sturmey (Eds.), Handbook of autism and pervasive developmental disorders (pp. 1283–1300). Springer.
United Nations. (2008). Convention on the Rights of Persons with Disabilities and Optional Protocol.
Virues-Ortega, J., Pérez-Bustamante, A., & Tarifa-Rodriguez, A. (2022). Evidence-based Applied Behavior Analysis (ABA) autism treatments: An overview of comprehensive and focused meta-analyses. In J. L. Matson & P. Sturmey (Eds.), Handbook of autism and pervasive developmental disorder, autism and child psychopathology series (pp. 631–660). Springer Nature: Switzerland AG. https://doi.org/10.1007/978-3-030-88538-0_27
Wilson, N., Barratt, M., Jorgensen, M., Limbu, B., Donley, M., Buchholtz, M., Smith, V., & Deb, S. (2023). Training support workers about the overmedication of people with intellectual disabilities: An Australian pre-post pilot study. Journal of Intellectual Disability Research, 67(6), 519–530. https://doi.org/10.1111/jir.13023
Zhou, M. S., Nasir, M., Farhat, L. C., Kook, M., Artukoglu, B. B., & Bloch, M. H. (2021). Meta-analysis: Pharmacologic treatment of restricted and repetitive behaviors in Autism Spectrum Disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 60(1), 35–45. https://doi.org/10.1016/j.jaac.2020.03.007
Author information
Authors and Affiliations
Contributions
Both authors conceptualized, drafted, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deb, S.(., Limbu, B. Training Direct Care Staff to Empower Adults with Intellectual Disabilities and Their Families to Reduce Overmedication. Adv Neurodev Disord 8, 192–197 (2024). https://doi.org/10.1007/s41252-023-00337-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-023-00337-2