Abstract
Objectives
Developmental Coordination Disorder (DCD) is a common condition with core difficulties in motor skills. Recent research has identified links between DCD symptoms and negative outcomes for mental and physical health. Despite this, DCD appears to still not be well known, even to many clinicians. To date, this has been documented among specific groups of clinicians (e.g., occupational therapists) in primarily English-speaking regions, but has not been compared across specific clinical professions or across countries. Therefore, we conducted a cross-national study to examine if clinicians in primarily English-speaking and German-speaking communities of various professions are sufficiently informed about characteristics of DCD in comparison with ADHD and other neurodevelopmental disorders.
Methods
N = 346 clinicians responded to questions in an online survey about general awareness and their experience in treating neurodevelopmental disorders, especially regarding specific characteristics of DCD and ADHD. Moreover, we asked them to classify a case vignette with DCD.
Results
Overall, 58% of participants had heard of DCD but only 42% had treated individuals with DCD. More specific knowledge about DCD and ADHD was low, varied by profession, and was generally reduced among clinicians working in primarily German-speaking communities. Participants often gave an incorrect diagnosis for the case vignette (35% correct responses) but still offered correct treatment recommendations (61% correct responses).
Conclusions
Awareness of the specific nature of DCD is still lacking for many clinicians. More training about DCD and other neurodevelopmental disorders should be disseminated in clinical training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Developmental Coordination Disorder (DCD) is a common condition involving delays in motor learning and coordinating fine and gross motor functions that begins in childhood and causes substantial impairment (American Psychiatric Association, 2013). Although DCD affects about 5% of the population (Blank et al., 2019), it receives much less attention in the scientific literature in publications and citations compared to other neurodevelopmental disorders with similar prevalence rates (e.g., ADHD; Bishop 2010; Meachon et al., 2022b). It is possible that this relative neglect in the literature is mirrored in low awareness of DCD among clinical professionals, which would be detrimental for adequate care.
Previous research has documented low awareness of DCD in well-established healthcare systems of primarily English-speaking countries (Australia: Hunt et al., 2020; Canada: Karkling et al., 2017; Canada, US, UK: Wilson et al., 2012) and identified numerous knowledge gaps about DCD in various groups of clinical professionals. More specifically, in an English-speaking sample, a minority of parents, teachers, and physicians reported familiarity with DCD (Wilson et al., 2012). A more recent study examined these stakeholders, as well as caretakers, in an Australian sample and found that knowledge about DCD is especially limited when compared to other disorders of childhood (Hunt et al., 2020). In addition, a group of Canadian occupational therapists reported familiarity with DCD by majority, but many were lacking up-to-date knowledge of procedures surrounding assessment and diagnosis of DCD (Karkling et al., 2017). Collectively, these studies demonstrate that DCD and its specific features are not well known, even among healthcare professionals.
It is important that more clinicians become aware of DCD in order to detect potential early motor signs (Anastasiadis, 2017) for more effective diagnosis and support. The previous research examining familiarity with DCD has indicated subtle differences in awareness may exist by role as a teacher, caretaker, general practitioner, or pediatrician (Hunt et al., 2020; Wilson et al., 2012). However, to our knowledge, no research has explicitly compared clinicians by profession who may be involved in the diagnostic and treatment process of DCD and other neurodevelopmental disorders (i.e., psychotherapists, occupational therapists, physical therapists, psychiatrists, general medicine practitioners). Identifying potential weak points in identification and diagnosis among professionals is important toward improving education in various forms of clinical training, especially as knowledge surrounding DCD is progressing (Meachon et al., 2022b). In addition, secondary symptoms involved in DCD are complex (Kirby et al., 2013; Tal Saban & Kirby, 2018; Zwicker et al., 2018) and have an impact on daily functioning (Delgado-Lobete et al., 2022; Tal Saban et al., 2016; Van der Linde et al., 2015). Potential psychosocial consequences (Caçola et al., 2016; Meachon et al., 2022b; Tamplain & Miller, 2020) require multidisciplinary care to adequately support individuals with DCD. Furthermore, existing studies considering awareness of DCD are limited to English-speaking populations (e.g., Hunt et al., 2020; Karkling et al., 2017; Wilson et al., 2012). Given that there are disparities in nomenclature, diagnostic tools, and treatment approaches between English-speaking regions and other countries (Meachon et al., 2022b), it is important to examine if this lack of research is reflected in a generally reduced awareness of DCD. Therefore, the present study aims to explore the current level of awareness among relevant clinical professions and their experience with the treatment of DCD. This enabled us to also compare the current state of awareness levels and treatment experience with DCD in groups of English- and German-speaking clinicians. We expected that participants would have less general and detailed awareness of DCD than ADHD. Regarding language group differences, we expected English-speaking clinicians would, on average, have more general and detailed knowledge about DCD than the German-speaking clinicians.
Method
Participants
Participants were recruited online through posts on social media, and primarily via emails to clinics in Germany and the UK (see Supplementary Materials). N = 450 participants completed the first section of the study (see Supplementary Materials). As we cannot guarantee these participants actively completed this section, we excluded those who dropped out and were left with N = 346 clinicians who completed the entire survey. The final sample size exceeds the minimum requirement for power in all relevant analyses conducted in the study (see Data Analysis; G*Power 3.1: Faul et al., 2009). The sample specifically included n = 127 psychologists, n = 102 occupational therapists, n = 55 physical therapists, n = 43 general medicine practitioners including pediatricians, n = 18 psychiatrists, and n = 1 unspecified clinical occupation. At the time of completing the study, participants were an average of 42.4 years old (SD = 11.9, Range: 22–79), and practicing post-qualification for an average of 14.3 years (SD = 10.3). Notably, there was a significant effect of occupation on years of post-qualification clinical experience [F(4, 325) = 5.64, p < .001], where physical therapists in our sample had the longest average years of experience in the present study (M = 19.26, SD = 1.33), while occupational therapists (M = 13.17, SD = 0.97) and psychotherapists (M = 12.27, SD = 0.97) had the least. Participants were based in primarily German-speaking (Germany, Austria, Switzerland; n = 261) and primarily English-speaking (UK, Ireland, USA, Canada, Australia, n = 85) communities (see Table 1).
Procedure
Health practitioners and clinicians could participate in the online study if they were at least 18 years old, currently practicing, and working in a field of interest (e.g., general practitioner, pediatrician, psychotherapist etc.). Participants were primarily recruited through extensive online searches of clinics and practices across Germany and the UK. For each country, the principal towns were selected (e.g., Germany: Berlin, Hamburg, etc.; UK: London, Liverpool, etc.) and we searched online for clinics in each of these cities. The participants were contacted via their official practice email addresses over a time-span of three months. We did not contact individuals from our own clinic who may have been aware of our research.
As the response rate from this procedure alone was low, we also advertised our study on social media and contacted larger organizations, associations, and societies. For the latter, requested organizations share a personalized recruitment message with their members. Overall, more than 4,000 emails were sent out in the recruitment effort. It was not possible to determine a participation rate because we could not track to whom our messages were forwarded. Furthermore, emails were often sent to societies of offices with an unspecified amount of practitioners. The study took about 15–20 minutes to complete and was conducted via SoSciSurvey (soscisurbey.de). It included several sections to measure awareness and treatment experience with various neurodevelopmental disorders, a case study regarding DCD, and specific questions about symptoms of DCD and ADHD, in order of appearance.
Measures
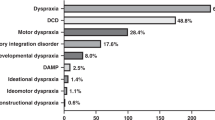
A comprehensive list of neurodevelopmental disorders as per the DSM-5 and ICD-11 (American Psychiatric Association, 2013; World Health Organization, 2022; see Table 2) was included in the initial part of the study, for which participants responded in a binary (yes/no) format. The first list was about awareness of each condition and the second about experience treating patients with each of these conditions (see Table 2 and Supplementary Materials). The order of disorders was randomized per participant within both lists and included regional terms, e.g., “Dyspraxia”, used in parallel with the internationally recognized name of “DCD” (Blank et al., 2019) in order to most accurately interpret awareness across many regions and professions. Later in the study, a 5-point Likert-scale format was used to probe the frequency at which the clinicians worked with neurodiverse patients (never – very often) and the ease of diagnosis and treatment for DCD and ADHD (very difficult – very easy).
Diagnostic expertise can be assessed with case vignettes (e.g., Bruchmüller et al., 2012) which are commonly used to assess the quality of decision-making among clinical professionals (Evans et al., 2015). To our knowledge, this has not been examined to indicate awareness of DCD on a broad scale. Therefore, we included a case study of a child with DCD based on the work of Geuze (2007). The case study was available online in English and translated into German by the second author of this paper (see Supplementary Materials for German translation). Participants were then asked to (1) provide the most likely diagnosis of the patient according to the information, (2) list any potential co-occurrences they would screen for, and (3) suggest a course of treatment. The case study was a classic example of DCD, and therefore, to earn a correct response on the first question, participants had to list DCD, or an equivalent term (e.g., Dyspraxia). Given that the case vignette described the person as “slightly hyperactive and distractable”, correct responses for co-occurring conditions had to include ADHD, or ADHD and other co-occurring conditions. Finally, the correct course of treatment involved a suggestion of a specific or generic treatment path to focus on motor or coordination training, as well as support known to be effective for DCD, such as Cognitive Orientation to daily Occupational Performance (CO-OP; Thornton et al., 2016). All responses were based on the current consensus of DCD, it’s co-occurrences, and treatment course (Blank et al., 2019). Case study responses were checked and scored by two independent coders, and any discrepancies between them were discussed to arrive at final scoring.
The case study was followed by 5-point Likert-scale questions about the relevance of various symptomatic aspects of each condition (never - always). More specifically, this included ratings of relevance for persistence into adulthood and five major symptom domains (behavioral; emotional; social; physical; executive functions) for DCD and ADHD in particular. These novel measures had fair reliability via Cronbach’s alpha (α = 0.67).
Data Analyses
To compare factors by clinical occupation, one-way ANOVAs were conducted. A power analysis with G*Power revealed a one-way ANOVA with 5 groups required a minimum of N = 125 participants for an effect size of 0.4 with 0.95 power, α = 0.05 (Faul et al., 2009). For comparisons between language groups, independent samples t-tests were used, requiring a minimum sample size of N = 270 participants for an effect size of 0.4 with 0.95 power, α = 0.05 (G*Power 3.1: Faul et al., 2009). Corrected values for unequal group sizes are reported where Levene’s test was significant. In addition to the main analyses, we conducted exploratory analyses to investigate (1) prevalence ratings for DCD and ADHD predicted by the study participants, (2) self-reported levels of difficulty in treatment of DCD and ADHD, and (3) the influence of participants who listed diagnosing or treating a non-existent disorder. Descriptive analyses are also reported (see Supplementary Materials). All statistical analyses were executed with IBM SPSS Version 26.
Results
General Awareness
Overall, 58% of participants reported awareness of DCD and 42% of participants noted they had diagnosed or treated patients with DCD (see Table 2). Notably, more clinicians were familiar with the term “Dyspraxia” (84%). With respect to treatment, more clinicians reported experience with Dyspraxia (45%) than the equivalent term of DCD on a descriptive level. These proportions were all descriptively lower than reported awareness of ADHD (96%) and treatment experience with ADHD (75%).
There were significant effects of clinical profession on reported expertise about DCD [F(4, 326) = 42.90, p < .001, η = 0.59] and reported expertise about ADHD [F(4, 338) = 19.49, p < .001, η = 0.43]. Bonferroni’s post hoc test revealed the differences in reported expertise of ADHD were driven by significantly less expertise among physical therapists (M = 2.49, SD = 0.74, 95% CI [2.29, 2.69]) compared to all other groups of practitioners. For DCD expertise, post hoc tests showed that psychotherapists (M = 1.82, SD = 1.04, 95% CI [1.63, 2.00]) and psychiatrists (M = 1.88, SD = 1.26, 95% CI [1.20, 2.55]) self-reported significantly lower expertise than all other groups.
Treatment Experience
Regarding treatment, there were significant effects of clinical profession on treatment frequency with DCD [F(4, 325) = 52.22, p < .001, η = 0.63] and ADHD [F(4, 338) = 20.52, p < .001, η = 0.44] patients. Furthermore, there were differences in the estimated persistence of DCD into adulthood by occupation [F(4, 305) = 4.14, p = .003, η = 0.05], but not for ADHD (p > .05). Bonferroni comparisons revealed the difference in reported relevance of DCD in adulthood was driven by a significant difference between psychotherapists (M = 3.06, SD = 0.89, 95% CI [2.89, 3.23]) and physical therapists (M = 3.57, SD = 0.84, 95% CI [3.33, 3.80]). The relevance of several symptom domains also differed by occupational group, including the social domain [F(4, 294) = 2.08, p = .026, η = 0.04] for DCD driven by higher ratings from psychiatrists (M = 3.82, SD = 0.60, 95% CI [3.41, 4.22]) versus all groups aside from general practitioners. For ADHD, differences by occupation were present for the social symptom domain [F(4, 333) = 4.89, p = .001, η = 0.06] driven by a significant difference between occupational therapists (M = 4.05, SD = 0.59, 95% CI [3.93, 4.17]) versus psychotherapists (M = 3.79, SD = 0.53, 95% CI [3.69, 3.88]) and physical therapists (M = 3.75, SD = 0.69, 95% CI [3.55, 3.94]), and behavioral domains [F(4, 329) = 6.95, p < .001, η = 0.08] where significant differences were present for most groups aside from psychiatrists.
Community Comparisons
Familiarity significantly differed by community for ADHD [t(342) = 4.47, p < .001, 95% CI (0.36, 0.79)], such that German-speaking professionals reported more expertise (M = 3.47, SD = 0.78) about ADHD than English-speaking professionals (M = 2.89, SD = 1.09). However, there were no significant differences between communities for self-reported experience treating ADHD.
There were significant differences by community for reported relevance of specific features of DCD and ADHD. Regarding DCD, the English-speaking professionals estimated a higher persistence into adulthood (M = 3.59, SD = 0.92; German-speaking clinicians: M = 3.09, SD = 0.79; t(309) = 4.19, p < .001; 95% CI [0.26, 0.73], corrected values), social relevance (M = 3.38, SD = 0.84; German-speaking clinicians: M = 2.97, SD = 0.77; t(301) = 3.70, p < .001; 95% CI [0.19, 0.63], corrected values), emotional relevance (M = 3.37, SD = 0.86; German-speaking clinicians: M = 3.00, SD = 0.77; t(301) = 3.32, p = .001, 95% CI [0.15, 0.60], corrected values), and physical relevance (M = 4.57, SD = 0.58; German-speaking clinicians: M = 3.84, SD = 0.89; t(304) = 8.23, p < .001, 95% CI [0.56, 0.91], corrected values).
Case Vignette
In the case vignette, 123 out of 346 participants, or 35.5% of the entire sample correctly identified a potential diagnosis of DCD or used a diagnostic label such as “Dyspraxia” or ICD-10 terminology, such as “Specific Disorder of Motor Function.” Among these participants, n = 10 (8.1%) proposed a diagnosis of “Clumsy Child Syndrome” for the case vignette, which, while not a current term, was coded as correct due to it being used for DCD prior to international consensus in 1994 (Polatajko et al., 1995). An additional n = 98 or 28.3% of participants indicated a response that was not specific enough, but on the right track toward DCD, such as “specific learning difficulties,” “fine motor skill delay,” “coordination problem,” and/or included a main diagnosis of ADHD/ADD alongside DCD, instead of the differential diagnosis. Furthermore, 28% correctly reported the need to screen for ADHD/ADD as the main differential diagnosis, and 61% provided treatment recommendations in line with guidelines from Blank et al. (2019), such as task-oriented or process-oriented approaches, specific motor skill training, and/or CO-OP. Correct treatment recommendations could also include referral to, or collaboration with, a physical or occupational therapist, additional psychomotor screening, and/or further assessment or specific motor skills.
Exploratory Analyses
Prevalence estimates for DCD and ADHD significantly differed by occupation. For DCD, psychiatrists (M = 4.93, SD = 5.63), psychotherapists (M = 6.83, SD = 8.51), and general practitioners (M = 8.34, SD = 7.71) reported the lowest prevalence rates, while physical therapists (M = 14.94, SD = 11.86) and occupational therapists (M = 18.70, SD = 16.70) reported the highest prevalence estimates [(F(4, 253) = 12.73, p < .001, η = 0.41],. Similarly, estimates of ADHD prevalence were highest among occupational therapists (M = 18.24, SD = 2.17) and lowest among psychiatrists (M = 5.80, SD = 1.37) [F(4, 273) = 10.70, p < .001, η = 0.37].
Exploratory analyses were conducted for reported difficulty of treatment, which differed by occupation for DCD [F(4, 305) = 4.25, p = .002, η = 0.23] but not for ADHD (p > .05). Bonferroni’s post hoc test revealed the effect of difficulty treating DCD was driven by contrasts between occupational therapists who reported more difficulties (M = 3.08; SD = 0.74) than psychotherapists (M = 2.76, SD = 0.75) and general practitioners (M = 2.67, SD = 0.74).
Finally, a total of n = 41 participants reported being familiar with a non-existent condition we called “Specific Motor Flexibility Disorder.” In addition, n = 37 reported treating this non-existent condition. Participants who reported familiarity with the non-existent condition also reported having greater expertise on DCD (M = 3.45, SD = 1.04) than respondents who did not report being familiar with the fake condition (M = 2.58, SD = 1.26; t(59.6) = 4.92, p < .001, CI[0.52, 1.22]). Furthermore, they reported treating DCD more frequently (M = 2.98, SD = 1.02) than participants who did not report knowing the non-existent disorder (M = 2.21, SD = 1.18; t(58) = 4.45, p < .001, CI[0.52, 1.22]). While there are small discrepancies in reports by the participants who indicated familiarity with a non-existent condition, we ultimately included them in the main analyses given their reported expertise and, primarily, that the sham condition may not have been discernable enough from other conditions (e.g., stereotypic movement disorder).
Discussion
This study highlights a number of concerning gaps in awareness of DCD and other neurodevelopmental disorders among clinical professionals. The low rate of reported general awareness of DCD compared to a much higher rate of awareness about ADHD is consistent with previous studies in other populations (Hunt et al., 2020; Kirby et al., 2007; Wilson et al., 2012). However, word choice may make a difference, as reported awareness of “Dyspraxia” was much higher than “DCD” showing more promising general awareness than past research (e.g., Wilson et al., 2012). Considering “DCD” was made the official international term over “Dyspraxia” in 1994 (Blank et al., 2019), these findings suggest a potential disconnect between practice and research, where the latter favors the term “DCD” (Meachon et al., 2022b). This is echoed in responses to the case study, for which many correct responses were various terms for DCD, such as “Dyspraxia,” “Specific disorder of motor functions,” and even the now outdated term “Clumsy Child Syndrome.” However, many practitioners were less accurate and varied substantially in knowledge of specific features of DCD, in line with more recent research of occupational therapists (Karkling et al., 2017). Collectively, these findings demonstrate a dissonance of knowledge about DCD among many clinicians.
Awareness Differs by Clinical Profession
Between clinical professions, a number of differences in awareness and treatment experience for both DCD and ADHD were found. For example, psychotherapists and psychiatrists reported less expertise about DCD which could be based on the assumption that motor deficits are not relevant to psychotherapy and psychiatry. Given that lower prevalence estimates of DCD were reported by psychotherapists and psychiatrists, this discrepancy might also be explained by an expectation that DCD is less common among these groups. Regardless, there is a psychological impact of DCD that is highly relevant for psychotherapy (Meachon et al., 2022b; Tamplain & Miller, 2020). In many cases, practitioners may underestimate the complexity of symptoms in cases of DCD and ADHD.
Clinical specialization might have further influenced differences in awareness of specific features of DCD. For example, occupational therapists and physical therapists who more accurately reported adulthood prevalence and social impacts may interact with individuals who have DCD more often, and may even be ahead of the research on interventions for DCD (O’Dea et al., 2021). Nonetheless, low awareness of DCD can be disastrous; in order to detect DCD in adulthood, or in general, one must be aware it exists.
In addition, reported difficulty in the treatment process for DCD differed across clinical professions, with a seemingly inverse result with regard to prevalence estimates. More specifically, occupational therapists in the sample reported substantially more difficulties treating DCD and also indicated a much higher prevalence estimate for DCD. The opposite was true for psychotherapists and general practitioners, who reported DCD was less difficult to treat compared to other occupation-based groups, but also indicated a lower prevalence estimate of DCD compared to other groups. It is possible these results are linked such that practitioners who work with DCD more often have a greater understanding of its complexity and expect DCD to occur more often because they more regularly treat individuals with DCD. The opposite could be true for general practitioners and psychotherapists, who treat DCD less often, and thereby may understand less about its complexity and expect DCD to occur less often. Future research should investigate this theory on a causal basis.
Awareness Differs by Region of Practice
German-speaking clinicians were an ideal comparison group for an initial cross-cultural comparisons because of similar standardized clinical training, comparably large populations, highly functional healthcare systems, and potential for regional diagnostic differences (Bruchmüller et al., 2012) in primarily German-speaking communities (i.e., Germany, Austria, Switzerland) compared to primarily English-speaking communities in the USA, UK, Canada, and Australia (i.e., Hunt et al., 2020; Karkling et al., 2017; Wilson et al., 2012). There were differences between the English- and German-speaking clinicians in expertise, but not treatment of ADHD. Future studies should examine if this difference reflects more confidence in knowledge or more detailed education surrounding ADHD for clinical professionals in Germany.
Due to the historically increased access of assessment and screening tools available in the English language compared to the German language (Meachon et al., 2022b), we expected that German-speaking clinicians would be less accurate than English-speaking clinicians in general and specific knowledge of DCD. We could only confirm specific knowledge differed for: reported persistence into adulthood, and importance of emotional, physical, and social domains of DCD symptoms. General knowledge was high overall, but the simplicity of the answer formats for these binary questions (yes/no) may have led to overinflation of reported knowledge. Taken together, these findings indicate the German-speaking clinicians may have underestimated the complexity of DCD. It is possible this disparity sources from differences in training materials (i.e., required course textbooks), tools, and scientific journals available in German and English languages. For example, the first screening tool in German for adults with DCD was released in 2022 but could be used in English since 2010 (Meachon et al., 2022a).
Mixed Results for Case Vignette
Curiously, a majority of the participants were often correct in treatment recommendations for motor skill intervention although a majority could not correctly diagnose a case vignette of DCD. This could be from educated guessing, or because of the limited nature of existing treatment options for motor deficits (Blank et al., 2019). Considering treatment recommendations were often correct even when the case vignette diagnosis was incorrect, it could be debated whether the specific diagnostic label for DCD is necessary. Especially because co-occurrence is more common among the neurodevelopmental disorders than having just one condition (Cleaton & Kirby, 2018). At present, the value of a specific diagnosis and advancements in current research of DCD should be considered. More accurate diagnosis can support estimating a more accurate prevalence of DCD, proper support for the patient, improved policy, access to accommodations in school and work, and avoiding consequences of misdiagnosis (e.g., medication for incorrectly diagnosed ADHD; Meachon et al., 2022a). Given the multidimensional impacts of DCD, diagnosis may be more accurate when considering spectrums of symptoms (e.g., RDoC criteria; Harrison et al., 2021; Mittal & Wakschlag, 2017) rather than via discrete and non-exhaustive lists of symptoms from the existing diagnostic manuals (Purcell et al., 2015).
Knowledge of a non-existent Disorder
Curiously, there were few differences in responses from participants who reported knowing a non-existent disorder we called “Specific Motor Flexibility Disorder.” The responses about specific features of DCD and ADHD were more accurate in the participants reporting they knew a fake condition than all other participants. It is possible this result is coincidental, or that their inclination to respond based on social desirability meant that they always indicated a high relevance for features of DCD and ADHD.
Limitations and Future Directions
There are several limitations to the present study which should be discussed. For one, there are some small subgroups (e.g., psychiatrists and general practitioners) and differing group sizes by language, but the overall sample sizes are fairly powered and compare with other research in this field. Furthermore, physical therapists had significantly more average years of experience than psychotherapists and occupational therapists. This could have influenced some differences by occupation, for which physical therapists reported the least amount of expertise on ADHD while psychotherapists were among the groups with lower reported expertise on DCD. However, it is possible the expertise on each condition is more closely related to professional relevance than years of experience. The link between profession, years of experience, and expertise on DCD and ADHD should be examined in future research with causal designs.
Another major limitation is that the results cannot be broadly generalized to cultural groups. While we include novel comparisons between two major communities of English- and German-speaking clinicians, our results should be replicated and examined in more communities. Furthermore, awareness levels may even vary from region to region within one language group (e.g., awareness of ADHD across Germany; Grobe 2017). Future research should investigate awareness of DCD and other neurodevelopmental disorders in other communities and causal links for disparities in knowledge.
Another limitation is that the survey took a long time to complete, which may have contributed to the high drop-out rate. In addition, it is possible there was a self-selection bias and clinicians who completed the survey had greater expertise about neurodevelopmental disorders. The answer format of general knowledge questions (yes/no) was simple, and given that specific knowledge was less accurate, it is possible responses in general questions did not accurately reflect true awareness. Nonetheless, the results still show concerningly low rates of awareness of DCD. Future studies should consider the use of larger, representative samples (e.g., national survey designs).
Due to the preliminary nature of this study and its non-experimental design, we are not able to draw causal links between awareness, treatment experience, and other factors (e.g., years of experience, training programs). Future research should replicate our work in other contexts, as well as in other groups of non-medical professionals who may work with individuals with DCD (e.g., educators, Anastasiadis 2017; family awareness and relations, Weyers et al., 2019). Finally, we found that many practitioners did not correctly diagnose DCD, but frequently selected the correct type of treatment for the patient. Therefore, future research should continue efforts toward establishing causal links between awareness of DCD and outcomes in patient care.
In the present study, clinicians with relevant professional backgrounds and from unique communities completed an online survey about their awareness of various neurodevelopmental disorders with a focus on DCD. General awareness of DCD and related treatment experience was concerningly low compared to ADHD, and consistent with awareness levels observed in previous research. Furthermore, there were several noteworthy differences in the reported relevance of various features of DCD and ADHD (e.g., persistence into adulthood). Notably, a majority of the participants could not correctly identify a typical case of DCD. The findings highlight the need for increased clinical education surrounding DCD in German-speaking and English-speaking regions. Overall, this study contributes to a broader identification of aspects surrounding DCD which should be emphasized more in clinical training.
Data Availability
The data for this study are publicly available at and linked to this paper on the MADATA repository via the following link https://madata.bib.uni-mannheim.de/id/eprint/400.
References
American Psychiatric Association. (2013). Diagnostic and statistical Manual of Mental Disorders (5th ed.). American Psychiatric Publishing.
Anastasiadis, M. (2017). Educator’s ability to identify students with coordination disorders: A review of literature. Arab Journal of Nutrition and Exercise (AJNE), 2(3), 139–151. https://doi.org/10.18502/ajne.v2i3.1218
Bishop, D. V. M. (2010). Which neurodevelopmental disorders get researched and why? PLoS One, 5(11), 1–9. https://doi.org/10.1371/journal.pone.0015112
Blank, R., Barnett, A. L., Cairney, J., Green, D., Kirby, A., Polatajko, H., Rosenblum, S., Smits-Engelsman, B., Sugden, D., Wilson, P., & Vinçon, S. (2019). International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Developmental Medicine and Child Neurology, 61(3), 242–285. https://doi.org/10.1111/dmcn.14132
Bruchmüller, K., Margraf, J., & Schneider, S. (2012). Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. Journal of Consulting and Clinical Psychology, 80(1), 128–138. https://doi.org/10.1037/a0026582
Caçola, P., Romero, M., Ibana, M., & Chuang, J. (2016). Effects of two distinct group motor skill interventions in psychological and motor skills of children with developmental coordination disorder: A pilot study. Disability and Health Journal, 9(1), 172–178. https://doi.org/10.1016/j.dhjo.2015.07.007
Cleaton, M. A. M., & Kirby, A. (2018). Why do we find it so hard to calculate the burden of neurodevelopmental disorders? Journal of Childhood & Developmental Disorders, 4(3:10), 1–20. https://doi.org/10.4172/2472-1786.100073
Delgado-Lobete, L., Montes-Montes, R., Pértega-Díaz, S., Santos-Del-Riego, S., Hartman, E., & Schoemaker, M. M. (2022). Motor performance and daily participation in children with and without probable developmental coordination disorder. Developmental Medicine and Child Neurology, 64(2), 220–227. https://doi.org/10.1111/dmcn.15036
Evans, S. C., Roberts, M. C., Keeley, J. W., Blossom, J. B., Amaro, C. M., Garcia, A. M., Stough, C. O., Canter, K. S., Robles, R., & Reed, G. M. (2015). Vignette methodologies for studying clinicians’ decision-making: Validity, utility, and application in ICD-11 field studies. International Journal of Clinical and Health Psychology, 15(2), 160–170. https://doi.org/10.1016/j.ijchp.2014.12.001
Faul, F., Erdfelder, E., Buchner, A., & Lang, A. G. (2009). Statistical power analyses using G* power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Geuze, R. H. (2007). Characteristics of DCD: On problems and diagnosis. In R. H. Geuze (Ed.), Developmental coordination disorder. A review of current approaches (pp. 9–25). Solal.
Grobe, T. G. (2017). Regionale Unterschiede von ADHS-Diagnoseraten in Krankenkassendaten 2005 bis 2015 [Regional differences of ADHD diagnosis rates in health insurance data from 2005 to 2015]. Bundesgesundheitsblatt Gesundheitsforschung – Gesundheitsschutz, 60, 1336–1345. https://doi.org/10.1007/s00103-017-2640-8
Harrison, L. A., Kats, A., Kilroy, E., Butera, C., Jayashankar, J., Keles, U., & Aziz-Zadeh, L. (2021). Motor and sensory features successfully decode autism spectrum disorder and combine with the original RDoC framework to boost diagnostic classification. Scientific Reports, 11. https://doi.org/10.1038/s41598-021-87455-w
Hunt, J., Zwicker, J. G., Godecke, E., & Raynor, A. (2020). Awareness and knowledge of developmental coordination disorder: A survey of caregivers, teachers, allied health professionals and medical professionals in Australia. Child: Care and Health Development, 47(2), 174–183. https://doi.org/10.1111/cch.12824
Karkling, M., Paul, A., & Zwicker, J. G. (2017). Occupational therapists’ awareness of guidelines for assessment and diagnosis of developmental coordination disorder. Canadian Journal of Occupational Therapy, 84(3), 148–157. https://doi.org/10.1177/0008417417700915
Kirby, A., Salmon, G., & Edwards, L. (2007). Attention-deficit hyperactivity and developmental coordination disorders: Knowledge and practice among child and adolescent psychiatrists and paeditricians. Psychiatric Bulletin, 31, 336–338. https://doi.org/10.1192/pb.bp.107.0153
Kirby, A., Williams, N., Thomas, M., & Hill, E. L. (2013). Self-reported mood, general health, wellbeing and employment status in adults with suspected DCD. Research in Developmental Disabilities, 34, 1357–1364. https://doi.org/10.1016/j.ridd.2013.01.003
Meachon, E. J., Beitz, C., Zemp, M., Wilmut, K., & Alpers, G. W. (2022a). The adult developmental coordination disorders/dyspraxia checklist - german: Adapted factor structure for the differentiation of DCD and ADHD. Research in Developmental Disabilities, 126. https://doi.org/10.1016/j.ridd.2022.104254
Meachon, E. J., Zemp, M., & Alpers, G. W. (2022b). Developmental coordination disorder (DCD): Relevance for clinical psychologists in Europe. Clinical Psychology in Europe, 4(2), 1–24. https://doi.org/10.32872/cpe.4165
Mittal, V. A., & Wakschlag, L. S. (2017). Research domain criteria (RDoC) grows up: Strengthening neurodevelopment investigation within the RDoC framework. Journal of Affective Disorders, 216, 30–35. https://doi.org/10.1016/j.jad.2016.12.011
O’Dea, ÁE., Coote, S., & Robinson, K. (2021). Occupational therapy practice with children with developmental coordination disorder: An online qualitative vignette survey. British Journal of Occupational Therapy, 84(5), 307–316. https://doi.org/10.1177/0308022620944100
Polatajko, H. J., Fox, A. M., & Missuna, C. (1995). An international consensus on children with developmental coordination disorder. Canadian Journal of Occupational Therapy, 62(1), 3–6. https://doi.org/10.1177/000841749506200101
Purcell, C., Scott-Roberts, S., & Kirby, A. (2015). Implications of DSM-5 for recognising adults with developmental coordination disorder (DCD). British Journal of Occupational Therapy, 78(5), 295–302. https://doi.org/10.1177/0308022614565113
Tal Saban, M., & Kirby, A. (2018). Adulthood in developmental coordination disorder (DCD): A review of current literature based on ICF perspective. Motor Disorders, 5(1), 9–17. https://doi.org/10.1007/s40474-018-0126-5
Tal Saban, M., Ornoy, A., & Parush, S. (2016). Participation and quality of life of young adults with developmental coordination disorder: A longitudinal study. The American Journal of Occupational Therapy, 70(4_Supplement_1). https://doi.org/10.5014/ajot.2016.70S1-PO4108
Tamplain, P., & Miller, H. L. (2020). What can we do to promote mental health among individuals with developmental coordination disorder? Current Developmental Disorders Reports, 8, 24–31. https://doi.org/10.1007/s40474-020-00209-7
Thornton, A., Licari, M., Reid, S., Armstrong, J., Fallows, R., & Elliott, C. (2016). Cognitive orientation to (daily) occupational performance intervention leads to improvements in impairments, activity and participation in children with developmental coordination disorder. Disability and Rehabilitation, 38(10), 979–986. https://doi.org/10.3109/09638288.2015.1070298
Van der Linde, B. W., van Netten, J. J., Otten, B., Postema, K., Geuze, R. H., & Schoemaker, M. M. (2015). Activities of daily living in children with developmental coordination disorder: Performance, learning, and participation. Physical Therapy, 95(11), 1496–1506. https://doi.org/10.2522/ptj.20140211
Weyers, L., Zemp, M., & Alpers, G. W. (2019). Impaired interparental relationships in families of children with attention-deficit/hyperactivity disorder (ADHD). Zeitschrift für Psychologie, 227(1), 31–41. https://doi.org/10.1027/2151-2604/a000354
Wilson, B. N., Neil, K., Kamps, P. H., & Babcock, S. (2012). Awareness and knowledge of developmental co-ordination disorder among physicians, teachers and parents. Child: Care Health and Development, 39(2), 296. https://doi.org/10.1111/j.1365-2214.2012.01403.x
World Health Organization. (2022). ICD-11: International classification of diseases (11th revision). https://icd.who.int/
Zwicker, J. G., Suto, M., Harris, S. R., Vlasakova, N., & Missuna, C. (2018). Developmental coordination disorder is more than a motor problem: Children describe the impact of daily struggles on their quality of life. British Journal of Occupational Therapy, 81(2), 65–73. https://doi.org/10.1177/0308022617735046
Acknowledgments
The authors would like to thank the anonymous participants for their time taking part in the present study. This project was supported by the Graduate School of Economics and Social Sciences at the University of Mannheim.
Funding
Open access funding provided by University of Basel
Author information
Authors and Affiliations
Contributions
EJM, HM, and GWA were involved in the conception and design of the work, data interpretation, critical revision of article, and approval of the version submitted for publication. EJM and HM independently coded case study responses and then deliberated on inconsistencies in coding. EJM performed final data analysis included in the manuscript, conducted the literature review, formulated the initial draft of the manuscript, and acquired funding for the project. HM prepared the study questionnaires for testing, translated the case study, recruited participants, and conducted preliminary data cleaning and analysis. GWA supervised EJM and HM.
Corresponding author
Ethics declarations
Ethics Statement
The University of Mannheim Ethics Committee reviewed and approved of the study.
Informed Consent Statement
All participants provided informed consent before participation.
Conflict of Interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 32.2 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meachon, E.J., Melching, H. & Alpers, G.W. The Overlooked Disorder: (Un)awareness of Developmental Coordination Disorder Across Clinical Professions. Adv Neurodev Disord 8, 253–261 (2024). https://doi.org/10.1007/s41252-023-00334-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-023-00334-5