Abstract
Objectives
Menstrual hygiene management (MHM) is a critical area of daily living skills for neurodiverse menstruators in which few evidence-based interventions exist. This study evaluated the acceptability and social validity of a caregiver-mediated intervention for youth on the autism spectrum utilizing behavior skills training, animated video modeling, task analysis, and telehealth services to improve changing a menstrual pad.
Methods
The consultant recruited three youth and caregiver dyads to test the intervention and collect acceptability and social validity assessments. Materials varied based on the phase of the study; however, a typical trial required data collection sheets, youth’s underwear, a menstrual pad, and, during intervention, the video model and hardware technology. A multiple baseline design across participants and reversal design were used to demonstrate experimental effects. Due to the sensitive nature of the study, independence and accuracy data were collected by caregivers and analyzed later by the consultant through visual analysis.
Results
Overall, youth participants improved their percentage of independent and accurate steps of changing a menstrual pad. Furthermore, caregivers reported moderate to high levels of acceptability of the telehealth service delivery and animated video modeling, as well as the overall MHM training program measured by the Technology Acceptability Model-Fast Form (FF-TAM) and the Behavior Intervention Rating Scale (BIRS), respectively. Youth reported high levels of acceptability of the MHM training program as measured by the Child Intervention Rating Profile (CIRP).
Conclusions
Results suggest that a technology-based, caregiver-mediated MHM intervention for neurodiverse youth would be considered acceptable and socially valid by caregiver and youth participants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Persons on the autism spectrum experience marked challenges in their ability to independently perform daily living skills (DLS), an important part of everyday adaptive functioning (Pugliese et al., 2015). DLS includes a wide range of self-care tasks such as bathing, eating, dressing, and managing menstrual hygiene. While numerous evidence-based techniques exist to support neurodiverse persons, those exploring menstrual hygiene management (MHM) are less prevalent (Ersoy et al., 2009). According to the Global Menstrual Collective, menstrual health consists of five essential elements: (1) access to punctual, developmentally appropriate, and evidence-based information; (2) fulfillment of bodily-related care through personal preferences, hygiene, comfort, privacy, and safety; (3) prompt and adequate treatment for menstrual-related discomforts or disorders; (4) a supportive community that provides key resources with the aim of empowerment; and (5) active and voluntary participation throughout life without fear of menstrual-related bias or violence (Hennegan et al., 2021). Without these components, neurodiverse individuals may experience an elevated risk of infection, difficulty concentrating, bodily discomfort, feelings of shame and embarrassment, and reduced rates of school participation during their menstrual cycle (Hennegan et al., 2016; Torondel et al., 2018).
To maintain proper MHM, menstruators on the autism spectrum may face a unique and heightened set of challenges in the form of sensory sensitivity and restricted and repetitive behaviors and movements, where one or more of these can cause significant disruption to a menstruator’s daily functioning (Burke et al., 2010; Lee, 2004; Steward et al., 2018). Neurodiverse menstruators may also start puberty before their neurotypical peers and have a greater chance of gynecological disorders; common examples include heavier periods (menorrhagia), painful abdominal/pelvic cramps (dysmenorrhea), and irregular cycles (Burke et al., 2010; Corbett et al., 2020; Hamilton et al., 2011). Caregivers of neurodiverse youth have expressed concerns related to puberty and menstruation, such as how to best support their youth in managing related challenges and navigating the scarcity of maturation education available in their school (Cridland et al., 2013; Nichols & Blakeley-Smith, 2009). With the potential risks for menstruators on the autism spectrum, there is a dire need for caregivers, educators, and/or service providers to supply supports (i.e., comprehensive educational materials and MHM training opportunities) in advance of menses (Steward et al., 2018).
Several strategies are available to support neurodiverse menstruators with MHM. A task analysis of these skills is a common approach and involves breaking an entire task into smaller, more manageable steps (Wong et al., 2015). A task analysis explicitly includes the unstated components associated with the task, such as going into the bathroom, standing near the toilet, pulling pants and underwear below the knees, and sitting on the toilet. MHM task analyses have demonstrated positive results when taking the form of a social story (Ariyanti & Royanto, 2017; Klett & Turan, 2012), or a visual list (Richman et al., 1984; Veazey et al., 2016), while using simulation on different models including humans (Ariyanti & Royanto, 2017) and dolls (Altundağ & Çalbayram, 2016; Ersoy et al., 2009; Kırbaş et al., 2020). Task analyses have also evolved over time; they vary in form, model, and individual conducting the training. The person providing the MHM support has shifted away from mostly researchers (Ariyanti & Royanto, 2017; Ersoy et al., 2009; Kırbaş et al., 2020; Richman et al., 1984; Veazey et al., 2016), to nurses (Altundağ & Çalbayram, 2016), caregivers (Klett & Turan, 2012), and peers (Kırbaş et al., 2020). Researchers have also explored task analyses in combination with other behavioral strategies such as chaining procedures (Richman et al., 1984; Veazey et al., 2016) and prompting (Ersoy et al., 2009). Succinctly, a task analysis is a socially acceptable and effective intervention to increase MHM independence for neurodiverse persons (Ersoy et al., 2009; Klett & Turan, 2012).
Another strategy available to support MHM is video modeling (Ariyanti & Royanto, 2017). Rooted in Bandura’s social learning theory, video modeling extends the possibilities of learning that result from watching a live model perform a skill by utilizing technology to record individuals modeling the desired skill (Bellini & Akullian, 2007). Despite being recognized as an effective instructional method for a wide variety of skills, the sensitive nature of certain DLS, like MHM, makes traditional video modeling an unsuitable strategy (Darden-Brunson et al., 2008; de Bruin et al., 2013). Therefore, incorporating animation into video models for MHM is a strong alternative to address this challenge in a more socially valid way (Drysdale et al., 2015; Mclay et al., 2015). Learning through modeling is more salient when the viewer perceives the model as similar to themselves in some way (Bandura, 1977). Animated video characters can be customized to match the model’s appearance to that of the learner, increasing the possibility that the viewer engages with the video. In contrast to typical video modeling, video animation offers a more entertaining and aesthetically pleasing modality for learning new skills; furthermore, this creativity has demonstrated success in minimizing escape-maintained behavior and promoting effective learning environments (Geiger et al., 2010).
Many of the current studies targeting MHM for this population have yet to explore telehealth as an additional means of service delivery. Telehealth describes the utilization of technology to provide medical and mental health services to clients synchronously (e.g., videoconferencing) or asynchronously (e.g., email, mobile apps, websites; American Psychological Association, 2014). At the start of the millennium, approximately 2% of psychologists had provided telehealth services via internet, satellite, or closed-circuit television in their professional careers (VandenBos & Williams, 2000). Presently, the extent of research on telehealth has spiked, in particular after the start of the COVID-19 pandemic, with 96% of psychologists treating patients remotely (Canady, 2020; Ellison et al., 2021). The application of telehealth now yields access to a growing variety of services, such as diagnostic and other related health assessments, intervention, consultation, supervision, and training (Fischer et al., 2019; Ore, 2021; Sutherland et al., 2019), across a greater number of remote and rural communities (Little et al., 2018; Ore, 2021; Simacek et al., 2020; Tsami et al., 2019). Caregivers found telehealth acceptable for its ease of use, reduced financial costs, fewer disruptions to daily routine, increased flexibility, and minimal to no transportation concerns (Ellison et al., 2021; Little et al., 2018; Ore, 2021; Tomlinson et al., 2018). The use of telehealth resulted in less stress for caregivers and neurodiverse youth, as well (White et al., 2021).
Telehealth, when used in the delivery of behavior skills training (BST) to support skill acquisition, has demonstrated promising levels of social validity and acceptability by both practitioners and caregivers (Boutain et al., 2020; Carnett et al., 2021; Dogan et al., 2017; Rios et al., 2020). Providers have widely used BST to teach youth new skills and train both caregivers (Schaefer & Andzik, 2020) and practitioners (Rios et al., 2020) on intervention procedures and strategies. BST typically consists of verbal or written instruction, modeling, rehearsal, and feedback components (Sarokoff & Sturmey, 2004). In a systematic review that explored using BST to train caregivers as primary interventionists, Schaefer and Andzik (2020) found that BST was a favorable tool for incurring positive behavioral change. Other studies have outlined caregivers’ effective contributions and support in communication and language development (Brown & Woods, 2016; Simacek et al., 2017), feeding interventions (Diaz & Cosbey, 2018; Mueller et al., 2003), and menstrual care (Klett & Turan, 2012). While maintaining procedural fidelity, caregivers have contributed to the generalization of target skills (Brown & Woods, 2016; Klett & Turan, 2012) and have also influenced the maintenance of skills within the naturalistic setting (Buschmann et al., 2008; Roberts & Kaiser, 2011; Simacek et al., 2017). While research should continue to explore BST, delivery via telehealth is an effective method that could be applied to MHM interventions and allow families the opportunity to address private and sensitive concerns (Kırbaş et al., 2020).
Existing research clearly highlights that many of the previously mentioned strategies have improved different domains of DLS in neurodiverse persons. However, these strategies (i.e., task analysis, animated video modeling, BST, and telehealth) together have yet to be examined to address MHM. While this study intends to expand previous research on task analyses and MHM, it also aims to contribute to the existing literature by evaluating the acceptability and social validity of a caregiver-led intervention, using animated video modeling, telehealth service delivery, and BST to improve changing a menstrual pad. Research questions and hypotheses are as follows: (1) Is there a functional relation between the implementation of a technology-based MHM program and an increase in the percentage of independent and accurate steps completed in the task analysis for changing a menstrual pad; (2) Is there a functional relation between the level of prompting required within the treatment training and an increase in level of MHM skill acquisition; (3) Is there a functional relation between treatment training and the percentage of training steps completed by the caregiver; (4) To what extent do caregivers find the MHM program training and consultation delivered via telehealth and the technology-based task analysis (i.e., animated video) acceptable as measured by the Technology Acceptability Model-Fast Form (FF-TAM); (5) To what extent do caregivers and youth find the total MHM program acceptable as measured by the Behavior Intervention Rating Scale (BIRS) and the Child Intervention Rating Profile (CIRP), respectively.
Method
Participants
Eligible youth criteria included an age limit of 14 years of age or younger; documentation of a clinical diagnosis of ASD; and indication of menarche and independence on several prerequisite skills to changing a menstrual pad (e.g., using a toilet for bladder movements and cleaning oneself after, dressing/undressing). Caregivers and youth participants had to provide voluntary verbal and written consent to participate in the study and research procedures. Last, participants needed access to the internet and a teleconferencing device (e.g., laptop, desktop, tablet, phone) to engage in telehealth services. The total sample size was six (i.e., three caregivers and three youth participants).
Caregiver
Each youth worked closely with their caregiver. All caregivers for this study identified as a biological parent, female assigned at birth, and had experienced or were experiencing menstruation. The consultant interviewed caregivers using the Developmental Profile, Fourth Edition (DP4) to measure the youth’s developmental levels across cognitive, adaptive behavior, social-emotional, physical, and communication domains. Additionally, each caregiver reported their youth’s independence level with hygiene-related tasks and support required for completing multi-step (2–3) directions.
Youth
The names of the following participants are pseudonyms. Amanda, an 11-year-old female assigned at birth who presented with average scores across all DP4 domains, was a member of the first cohort of participants. Amanda demonstrated the ability to complete all hygiene-related tasks and multi-step directions independently. Reportedly, Amanda presented no behavioral problems when engaging in hygiene-related tasks. Amanda experienced her menarche during baseline data collection procedures. Attrition occurred due to personal circumstances after the collection of three treatment training data points. Another member of the first cohort of participants, Annie was an 11-year-old female assigned at birth who presented with average DP4 domain scores for adaptive behavior, social-emotional, cognitive, and communication, and below average for the physical domain. Annie’s caregiver reported that she had not started menstruating, could complete all hygiene-related tasks independently, and required minimal support for multi-step directions. Reportedly, Annie presented no behavioral problems associated with hygiene-related tasks, but did experience significant anxiety when discussing puberty-related topics (i.e., menstruation). Anxious behaviors included observable physiological responses such as becoming pale in the face, increased sweating, quickened breathing, and leaning her body against her caregiver.
A member of the second cohort of participants, Mallory was a 12-year-old female assigned at birth who presented with delayed scores on all DP4 domains. Reportedly, Mallory could independently complete some hygiene-related tasks (e.g., using the toilet for bladder movements, and dressing/undressing), but required substantial support with completing multi-step directions. Her caregiver reported that Mallory had not started menstruating and exhibited elopement and tantrum-like behaviors with hygiene-related tasks.
Consultant
The consultant was a graduate student in an APA-accredited doctoral program in school psychology. At the time of the study, the consultant had 2 years of direct experience providing feeding therapy and behavioral intervention services via telehealth to neurodiverse youth and adolescents. In preparation for this study, the consultant attended sexuality education webinars, which incorporated effective teaching methods for MHM to youth, adolescents, and adults across all ability levels.
Procedures
Video Technology, Hardware, and Software
The consultant and research team used personal laptop computers (MacBook Pro 2017) to create animated videos as well as implement all procedures with participants via Chrome and Safari search engines. They created the animated videos through the web-based application Vyond, which enables users to build animated videos for a variety of topics with vectored animation and drag-and-drop functionality. For this study, researchers developed two animated videos: the Introduction to Menstruation Video (see Fig. 1), which gives a brief overview of menstruation; and the Training Video (see Fig. 2), which provides the task analysis of changing a menstrual pad. Both videos utilized laptop microphone technology to provide voice-overs to the subtitles. The consultant set the training video in the first-person point-of-view (i.e., youth) and personalized it to each youth and caregiver by modeling the animated characters to resemble their real-life counterparts. To facilitate later training implementation, the consultant spliced the video into eighteen segments (to reflect the task analysis) and inserted it into a slideshow, where each segment had its own slide. To access the two videos, visit the University of Utah’s Technology in Training, Education, and Consultation (U-TTEC) Lab’s website (https://www.u-tteclab.com/tools-and- resources.html).
In accordance with the BST protocol for the study, the consultant and research team created an instructional video using a video camera and video editing software (Sony Vegas Pro 11) on personal laptop computers (MacBook Pro 2017) to provide caregivers with an appropriate, virtual model for both data collection and MHM treatment training implementation. The instructional video incorporated a recording of the consultant modeling the steps of MHM treatment training and directions on further support for the youth if they did not comply or responded incorrectly during a trial. This footage also employed a separate recording that instructed caregivers on collecting independence, accuracy, and integrity data.
Other Materials
For baseline procedures, the consultant requested that caregivers have a blank baseline data collection and integrity form accessible to track progress during trials (see Supplementary Materials). Caregivers collected baseline data via a paper and pencil/pen method. Additional material requirements included a clean pair of the youth’s underwear and menstrual pad placed within the underwear lining, extra menstrual pads in the bathroom, and a trash can positioned next to the toilet. During treatment training, the consultant instructed caregivers to prepare all baseline materials (e.g., a menstrual pad placed in underwear, pencil/pen, clipboard, extra menstrual pads in the bathroom, and trash can) and treatment training data collection and fidelity forms (see Supplementary Materials). Last, caregivers needed a camera to take photos of specific steps and a device to stream the animated video situated on a stable surface (i.e., phone, tablet, or laptop).
Setting
The consultant held meetings with the caregiver or youth via telehealth (i.e., Zoom video conferencing software), where each member engaged from a setting of their choice (e.g., bedroom, office). The only exception to this was for baseline, treatment training, and treatment trials which occurred within the youth and caregiver’s home bathroom.
Design
For the first cohort, the consultant used a multiple baseline design (MBD) across participants. Due to participant attrition, the MBD was incomplete and limited from a lack of data points. For the second cohort, the sole participant (Mallory) was shifted to a reversal design (ABAB). The first phase of this design was the baseline, followed by treatment training, treatment, and a second treatment training. Although learning is irreversible, the reversal phase (treatment) was identical to the baseline condition regarding the prompts that were available.
Recruitment
For an illustration of the procedural timeline (see Fig. 3). Recruitment for the study included the consultant approaching local behavioral clinics that offered Applied Behavior Analysis (ABA) services to youth and adolescents on the autism spectrum. Clinic coordinators received an email from the consultant with information related to the study (e.g., procedures, contact information, inclusion criteria). If requested, the consultant met in person or virtually to discuss study details in greater depth. Relevant clinic personnel disseminated study information to clients and/or families they believed would benefit from the study. Following, interested caregivers filled out an online form and, if caregiver responses met the study’s criteria, the consultant contacted them to discuss details and coordinate the initiation of study procedures.
Puberty Education
The consultant provided separate puberty training to both the caregiver and youth, including a slideshow with informative videos, helpful tips, talking points, and resources. First, the consultant met with the caregiver to deliver training covering relevant puberty topics such as anatomy and terminology, physical and social-emotional changes, increased hygiene responsibilities, and public versus private boundaries. Following this, the consultant delivered complementary puberty training to the youth. The consultant offered to provide the puberty training to the youth exclusively, or with the caregiver present. Prior to the youth’s training, the consultant reviewed the training with the caregiver to filter and add content that could cause distress or be of potential benefit to the youth, respectively. The standard topics for this training included expected physical and emotional changes accompanied by puberty, public versus private boundaries, and period information (i.e., MHM products, premenstrual signs, and symptoms). The consultant and youth then considered ways the youth could advocate for their menstrual needs across specific settings. After both training sessions, the consultant shared additional menstrual-related resources with the caregiver and youth.
Baseline
The consultant discussed baseline procedures with each caregiver after puberty training. The consultant reviewed the procedural guidelines, which listed the necessary steps to conduct a baseline trial and complete baseline data collection and fidelity forms. Throughout, the consultant provided ample opportunity for caregivers to ask questions or voice concerns.
During baseline procedures, the caregiver prepared all necessary materials and inserted the clean menstrual pad within the lining of the youth’s underwear. Next, caregivers requested the youth to put on the underwear with a menstrual pad already in place and then change the menstrual pad. While the youth changed the pad, the caregiver observed and recorded any steps the youth completed correctly or incorrectly on the data collection form. The caregiver avoided feedback, prompts, or guidance during this process. The only exception occurred when the youth was attempting to discard a menstrual pad and/or its packaging into the toilet, at which point the caregiver directed the youth to put the menstrual pad and/or its packaging in the trash can. Regardless of whether the youth refused, attempted, or completed the task, the caregiver thanked them for their effort. Immediately after, the caregiver completed the baseline fidelity form and shared a scanned copy or photo of both the baseline data collection and fidelity forms with the consultant via email.
Behavior Skills Training
Upon collecting all baseline data, the consultant prepared the caregiver to implement the MHM treatment training procedures with the youth using BST (Sarokoff & Sturmey, 2004). First, the consultant reviewed the steps involved in implementing MHM treatment training and additional instruction on the types of prompts (i.e., verbal, video model, partial physical, and full physical) delivered to support the youth. Next, the consultant provided the video model of proper MHM treatment training. The caregiver then recorded a practice trial of themselves implementing MHM treatment training with a confederate, who could be either a separate youth, adult, or research team member. The caregiver later submitted the practice trial video to the consultant, who assessed their practice for fidelity using a treatment training fidelity form and provided feedback in a separate meeting. The caregiver practiced the rehearsal and feedback process until they reached 80% or higher in fidelity.
MHM Treatment Training
The treatment training procedural guidelines specified the necessary steps involved in trial procedures, where the caregiver prepared all necessary materials (see section on Other Materials) and pressed the menstrual pad into the lining of the underwear. Afterwards, the caregiver requested the youth put on the underwear and change their menstrual pad. Before the youth’s return, the caregiver opened the slideshow with animated video clips on a device and situated it in a stable location near the trial setting.
For the first treatment training trial, the caregiver showed the full Training Video to the youth before starting data collection. After viewing the video, the caregiver observed if the youth engaged in the first step of the task analysis within 5s of their prompt to change the pad; if the youth responded independently and accurately, the caregiver immediately provided verbal praise (e.g., “Good job”). In the absence of an independent and accurate response after 5s, the caregiver provided a verbal prompt or stated the step for completion (e.g., “Shut the door,” “Flush the toilet”). The caregiver allowed the youth an additional 5s to complete this step accurately. If the youth did not respond correctly, then the caregiver played the first step of the animated video and, once the step finished, verbally prompted the youth to do the action (e.g., “Now you do it”). The caregiver waited 5 more seconds for a correct response from the youth. However, if the youth did not respond or responded incorrectly, the caregiver delivered a partial physical prompt with an additional verbal prompt of repeating the step (e.g., “Shut the door”). A similar process would occur if the youth did not respond or responded incorrectly after the partial physical prompt, where the caregiver delivered a full physical prompt and verbal prompt of the step (e.g., “Shut the door”) so that the youth completed the action.
With the completion of each step, the caregiver noted on the treatment training data collection sheet the accuracy of the youth’s first attempt at completing the step and the level of prompting required, if any. Some steps also had a camera icon, which prompted the caregiver to take a photo of the result for pre-determined non-private steps. Non-private steps were defined as steps that involved only trial materials or did not require the youth to expose their private body parts (e.g., “Stand near the toilet,” “Throw wrapping in the trash”). Private steps were those that the youth engaged in more private behaviors (e.g., “Pull pants/skirt, underwear, and menstrual pad down below knees,” “Wipe vagina with toilet paper”). Once the youth had practiced all steps, the caregiver praised the youth for practicing the skill and filled out the treatment training fidelity form. The caregiver then shared copies of the forms and pictures of specific steps with the consultant via email.
During the treatment training phase, the caregiver met weekly with the consultant to discuss progress with changing a menstrual pad. The consultant presented a graph of the youth’s independence and accuracy with the task as well as the caregiver’s fidelity in conducting the training. The consultant reviewed both the youth and caregiver’s performances and formulated a plan for any remaining data collection. If the caregiver had any questions or concerns, the consultant addressed those during the meeting. For those in the MBD, if the youth reached mastery, the consultant discontinued training and discussed the next steps for treatment.
Treatment
Treatment assessed how well the youth could change a menstrual pad without assistance from their caregiver and animated video model. For this, caregivers implemented the same procedures as a baseline using similar data collection and fidelity forms, with the exception of title changes (“17”). If the youth did not maintain mastery, the consultant moved the youth and caregiver back to the MHM treatment training phase. However, if they did maintain mastery, the consultant discontinued treatment and discussed next steps for acceptability and social validity survey completion.
Measures
Dependent Variable
The primary dependent variable for this study was the percentage of independent and accurate steps completed in the task analysis (see Table 1), where mastery was 100% across five consecutive data points during the training and treatment phases. The caregiver collected and recorded step independence and accuracy throughout baseline, treatment training, and treatment. A single trial consisted of the percentage of all steps completed independently and accurately out of the total number of steps of the task analysis. For treatment training alone, caregivers collected a second dependent variable on the percentage of prompting (i.e., verbal, video model, partial physical, or full physical) provided across total task analysis steps.
Due to the private nature of intervention skills, the dependent variable limited interobserver agreement (IOA). During treatment training, the caregiver included pictures of five task analysis steps, carefully chosen to protect the youth’s privacy, with their data collection sheets. Each picture acted as evidence of step completion, even if the youth needed assistance. The consultant collected IOA across 33% of treatment training trials for Amanda, 35% for Annie, and 14% for Mallory. The consultant then reviewed the pictures and compared them to their accompanying data collection sheets for agreement, resulting in 100% for Amanda, 97% for Annie, and 60% for Mallory. Mallory’s caregiver was unable to collect as many complete trials for IOA due to the high chance of privacy violation.
Consultant Procedural Integrity and Caregiver Treatment Integrity
Procedural integrity measures how well the consultant followed the steps of a specific phase (i.e., baseline, treatment training, treatment) and sessions (e.g., puberty education, BST, consultation) within a phase. The consultant recorded data using a behaviorally anchored checklist, which varied across different sessions and phases, outlining the necessary steps to facilitate participants’ progress (see Supplementary Materials). For example, during sessions in the treatment training phases, some steps for the consultant to complete included: (1) review the results of the intervention data with the caregiver using a graph; (2) offer feedback on youth’s and caregiver’s performance; (3) collaborate on next steps for study implementation. After each session, the consultant self-assessed their own procedural integrity in order to ascertain whether a step had been missed. Overall, the consultant’s procedural integrity was acceptable across all recorded sessions with participants: Amanda (M = 93%), Annie (M = 95%), and Mallory (M = 96%). Following, the consultant saved the recorded session for another team member to view and assess IOA by dividing the agreements of steps completed over the total agreements and disagreements of steps completed. The other team member completed IOA across a third of all sessions and was acceptable for Amanda (M = 92%), Annie (M = 87%), and Mallory (M = 98%).
The caregiver self-recorded treatment integrity after each data collection trial using a behaviorally anchored checklist (see Supplementary Materials). Similar to the consultant procedural integrity, the number of steps varied based on the demands of the specific phase (i.e., baseline, treatment training, treatment). For example, during treatment training, the caregiver had to prepare their video technology and provide behavioral prompting strategies, which was not needed at baseline. The steps were based on the observable behaviors needed to complete a trial with their youth, which may include (1) prepare youth’s underwear with a menstrual pad inside the lining; (2) provide verbal prompts to start a practice trial; and (3) verbally praise and thank the youth for their effort in changing a pad. The consultant was unable to take IOA data on caregiver treatment integrity, due to the private nature of the dependent variable, and thus relied on caregiver report. Overall, caregivers reported high levels of treatment integrity across all data collection trials, see Table 2.
Acceptability and Social Validity
The consultant used an adapted version of the Technology Acceptability Model-Fast Form (FF-TAM) to assess the acceptability of the animated video model and telehealth services based on usefulness, ease of use, and predicted usage by caregivers. The FF-TAM utilizes a 12-item scale and rates on a semantic differential (range from − 3 to + 3) with higher ratings indicating higher levels of acceptability (maximum total score = 36; maximum average score = 3.0). Previous research indicated adequate internal consistency across all three factors (α = 0.93–0.97; Chin et al., 2008). For this study, the consultant changed the language of the FF-TAM to fit the context of MHM.
To measure the social validity of the entire intervention, the consultant administered an adapted version of the Behavior Intervention Rating Scale (BIRS) to caregivers. The BIRS is a reliable and internally consistent 24-item scale rated on a six-point Likert scale from “strongly disagree” to “strongly agree,” with higher scores corresponding to higher levels of treatment acceptability (Elliot & Treuting, 1991). The consultant modified the language of the BIRS to examine the perceptions of treatment acceptability, perceived effectiveness, and timeliness of the effect for the MHM intervention.
Last, the consultant provided a modified Children’s Intervention Rating Profile (CIRP) to youth upon completing the study. The CIRP is a reliable experimental rating scale developed to assess youth’s reactions concerning the acceptability of a given intervention (Witt & Elliot, 1985). The CIRP is a seven-item questionnaire, written at a fifth-grade reading level, which uses a six-point Likert scale (1 = strongly disagree and 6 = strongly agree; Elliot, 1986). Total scores range from 7 to 42, after reflecting negatively worded items, with scores of 24.5 or higher considered acceptable (Turco & Elliot, 1986). The consultant modified the language of the CIRP to assess increasing MHM independence rather than performance in school.
Data Analyses
The consultant utilized visual inspection to analyze the data (Cooper et al., 2006).
Results
Independence and Accuracy of MHM Task Analysis
Amanda: Amanda and her caregiver participated fully in the baseline phase and partially in the treatment training phase (see Fig. 4). Amanda’s baseline data indicated increasing independence and accuracy of task analysis steps, reaching 100% on the final two trials (M = 90%, range = 78–100%). Treatment training data was 100% across the 3 data points.
Annie: Annie completed the study in its entirety (see Fig. 4). Annie’s baseline data indicated some variability with an initial increasing trend, followed by a decrease in independence and accuracy of task analysis steps (M = 63%, range = 39–89%). There was an immediate drop in the level of accuracy and independence at the beginning of the treatment training phase. At the sixth data point, there was another decrease in independence and accuracy. Following a steady increasing trend, Annie met mastery criteria at the 17th treatment training trial (M = 75%, range = 11–100%). Annie’s average during the treatment phase remained at 100%, demonstrating continued mastery.
Mallory: Mallory completed the study in its entirety (see Fig. 5), with baseline data indicating some initial variability, followed by low and stable levels of independence and accuracy (M = 4%, range = 0–17%) of task analysis steps. During the initial treatment training, Mallory’s performance continued at this level until the third treatment training session, where there was an increase in accuracy and independence. Beyond the third treatment training data point, Mallory’s performance levels varied (M = 37%, range = 0–67%). Across the reversal phase, the first three data points remained high, followed by a decreasing trend in independence and accuracy for the last two data points (M = 60%, range = 39–72%). After re-introducing the treatment training phase, Mallory’s independence and accuracy immediately increased and continued to display an increasing trend for the last two data points (M = 74%, range = 67–83%).
Prompting Required Across Treatment Training
Amanda: Amanda required no support from her caregiver during treatment training (see Figure 6).
Annie: At the start of treatment training, the caregiver provided considerable support in the form of video modeling (see Fig. 6). The first four data points showed high levels of video modeling usage with some partial physical prompting. Annie required partial physical prompts in the second and third data points to dispose of the menstrual pad since the trash can was a few feet from the toilet. For the subsequent data points, Annie needed minimal verbal prompting until she achieved mastery across the last six data points (M = 24%, range = 0–89%).
Mallory: Across the first and second treatment training phases, Mallory’s caregiver provided mostly verbal prompts (see Fig. 6). At the beginning of the first treatment training phase, Mallory required support to complete all steps; but this decreased beginning at the third data point (M = 63%, range = 33–100%). In addition to verbal prompts, Mallory required video and partial physical prompts for the first, second, and third data points, and partial physical prompts for the fifth and sixth. The level of prompting remained stable and moderate for the last data points in this training phase. With the re-introduction to treatment training after reversal, Mallory required a reduced level of overall prompting to complete the task; across the five data points, her caregiver provided solely verbal prompts (M = 24%, range = 17–33%).
Behavior Skills Training Fidelity and Treatment Integrity
Amanda: Amanda’s caregiver completed 100% of the treatment steps with fidelity during BST (see Table 2). During baseline, Amanda’s caregiver demonstrated 100% treatment integrity, which she also exhibited during the treatment training phase.
Annie: During the BST fidelity check, Annie’s caregiver demonstrated 100% fidelity (see Table 2). Annie’s caregiver also had 100% treatment integrity for all trials across the study.
Mallory: When teaching the intervention steps during the rehearsal fidelity check, Mallory’s caregiver completed 100% of the treatment steps (see Table 2). Across baseline, Mallory’s caregiver demonstrated an average of integrity for 94% of treatment procedures. During the first treatment training phase, Mallory’s caregiver demonstrated a 92% mean for treatment integrity. Her treatment integrity increased to an average of 98% across the following two phases (i.e., reversal and the final treatment training).
Acceptability and Social Validity
Three caregiver respondents completed the FF-TAM social validity measure. The first and second caregivers both responded to the question of the acceptability of telehealth with high total sum scores of 32 (M = 2.67, range = 0–3), while the third caregiver answered with a high total sum score of 36 (M = 3, range = 3). On the acceptability of the animated video model as a method for intervention, the first respondent yielded a moderate total sum score of 30 (M = 2.5, range = 0–3), while the second and third respondents both had a high total sum score of 36 (M = 3; range = 3).
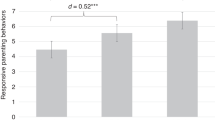
On the BIRS, all three respondents found the intervention to be highly acceptable (M = 5.29, 5.0, 6.0). Overall acceptability index scores were high (M = 5.0, 5.0, 6.0); perceived effectiveness was also highly acceptable (M = 5.0, 5.0, 6.0); and time of effect received high acceptability ratings (M = 5.5, 5.0, 6.0).
One respondent completed the CIRP. The respondent’s scores indicated that they found the MHM training program acceptable, with a high total sum score of 39. Of note, the respondent selected “strongly agree” for the questions about the fairness of the program, and its potential usefulness for other kids and learning skills to be more independent. Furthermore, the respondent selected “strongly disagree” for questions about caregiver harshness and problems caused by the program.
Discussion
This pilot investigation offers preliminary support and direction for the acceptability and social validity of an intervention that incorporates BST, animated video modeling, task analysis, and telehealth services to facilitate positive change in a neurodiverse youth’s MHM. Of the three participants, Amanda’s performance data reflected mastery criteria prior to treatment training; whereas Annie’s and Mallory’s data showed increases in performance over time, with the addition of the intervention. Their data also demonstrated they required less prompting across treatment training trials, indicating improved independence and accuracy. Overall, study results suggest that a technology-based, caregiver-mediated MHM intervention is considered highly acceptable and socially valid by caregivers and youth, as measured through the FF-TAM, BIRS, and CIRP.
Additionally, caregivers’ high percentage of accurate treatment steps completed during the rehearsal fidelity check preceded high levels of treatment integrity. However, two of three caregivers’ treatment fidelity data demonstrated ceiling effects, which may suggest that the training steps appeared less complex and allowed for caregivers to implement them effectively with minimal guidance and still attain maximum treatment integrity. Due to a lack of IOA data on caregiver treatment integrity, the impact of caregiver accuracy cannot be determined. Nonetheless, achieving a high percentage of steps accurately during caregiver training may have contributed to subsequent integrity of treatment procedures.
Specifically, these findings expand previous literature by demonstrating that caregivers can achieve high rates of fidelity in MHM treatment implementation and data collection procedures before and after receiving training over telehealth (Kırbaş et al., 2020). Acceptable ratings of telehealth procedures by caregivers, as shown by the results on the FF-TAM, support the utility of telehealth for MHM caregiver-implemented interventions in the future. This is promising for increased training opportunities as telehealth provides the opportunity to reach a broader audience.
In addition, study results extend previous literature by demonstrating that animated video modeling is a useful and socially valid tool to improve MHM for individuals on the autism spectrum (Ariyanti & Royanto, 2017). In comparison to live video modeling, video animation takes away the necessity of human models and the associated requirements to engage in intimate and sensitive behaviors on camera. Caregivers rated the animated video model as effective and acceptable on the FF-TAM, further supporting its utility in MHM-targeted interventions.
Limitations and Future Research
The consultant modeled this study after previous studies examining similar research questions that were somewhat reflective of the current study’s purpose. This study should be regarded as a pilot investigation and can provide direction to help address a range of drawbacks to potential future applications (i.e., alternative designs, and participant attrition).
Of note, Amanda, Annie, and Mallory’s data demonstrated hindrances with internal validity. First, Amanda studied how to correctly complete the menstrual task via web searches outside of the practice trials with her caregiver. This may have impacted Amanda’s baseline results as indicated in an increasing trend towards the end of the phase. Second, Annie’s data showed a significant drop in level at the start of the treatment training phase, which can be attributed to her caregiver allowing her to view the respective animation step prior to performing the skill.
This took away the opportunity for Annie to respond independently, thereby impacting the initial trials of the respective phase. While this was later corrected by the consultant, a true representation of Annie’s MHM independence and accuracy with the introduction of the intervention remains inconclusive. During the initial treatment training phase, Mallory’s performance remained at zero independence and accuracy across the first two trials. This lack of progress was attributed to the novelty of the task by her caregiver and does not support the immediate efficacy of the intervention. Given the various circumstances with each participant’s data, readers should use caution when inferring a functional relation from the independence and accuracy data of the intervention.
Further limitations are demonstrated via the caregiver treatment integrity. When Annie’s caregiver provided considerable support in the form of video modeling, her opportunity to demonstrate independence was diminished. Due to the consultant’s omission, Annie’s caregiver’s treatment integrity scores did not reflect total errors; otherwise, there may have been a decreased level in overall integrity (see Table 2). This mistake negatively impacted the internal validity of the caregiver treatment integrity, as well as the possible demonstration of experimental effect. Therefore, future investigations should consider incorporating this option into the integrity forms.
Researchers should also consider recruiting more participants than necessary and choose a design with reduced participant demand. The study’s original design, MBD, required considerable response effort (e.g., fidelity, IOA, data collection, and caregiver BST rehearsal procedures) that may have impacted participant attrition and the possibility of demonstrating experimental control. Some participants withdrew at the start of the youth’s academic school year due to shifts in schedules and responsibilities. Therefore, conducting the study during summer break may provide increased availability for youth and caregivers.
While telehealth has many benefits, conducting the rehearsal portion of BST required considerable preparation by the caregiver (i.e., having materials ready, prepping the confederate, implementing the procedures, and managing technology). In future renditions, researchers would be wise to apply simpler rehearsal strategies. Also, the consultant was not able to conduct follow-up trials to assess the maintenance of the skills learned by the youth. If possible, later studies should attempt to collect follow-up data, to better guide other MHM development programs.
Unlike traditional procedures that used highly trained researchers to obtain IOA data, this study utilized highly trained caregivers to both collect IOA and conduct experimental procedures with the youth participant. The consultant assigned caregivers dual roles due to the intimate and sensitive nature of the study and to avoid any discomfort from a third-party researcher. However, with all the responsibilities assigned to caregivers, IOA data collection did not adhere to the recent standards by What Works Clearinghouse (WWC, 2020). Thus, future researchers should consider feasible and appropriate methods to attain IOA without violating a participant’s privacy.
Researchers should attempt this intervention with menstruators of different age groups, ability levels, disability categories, and menstrual experience. The current study included youth between 11 and 12 years of age on the autism spectrum who had recently experienced menarche (within 6 months) or had not started menstruating. It could be valuable to service providers and caregivers to evaluate the appropriateness of this strategy for a wider age group and those with differing disabilities (e.g., cerebral palsy, intellectual disability, Down’s syndrome). Additionally, previous researchers have suggested the field consider recruiting participants with varied adaptive capabilities, such as those related to self-care and bathroom routines (Klett & Turan, 2012; Veazey et al., 2016).
Finally, little is known about the acceptability of menstrual products for neurodiverse youth and adolescents. While this study focused on menstrual pads, other products may have led to quicker skill acquisition and even higher acceptability ratings from caregiver and youth participants. Evaluating the overall acceptability and preference of menstrual products from the perspective of neurodiverse menstruators will likely increase the relevance of future MHM interventions.
Change history
11 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s41252-023-00321-w
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th edition). https://doi.org/10.1176/appi.books.9780890425596
American Psychological Association. (2014). What are telehealth and telepsychology? Retrieved July 20, 2021, from https://www.apa.org/pi/disability/resources/publications/telepsychology
Altundağ, S., & Çalbayram, N. Ç. (2016). Teaching menstrual care skills to intellectually disabled female students. Journal of Clinical Nursing, 25(13–14), 1962–1968. https://doi.org/10.1111/jocn.13215
Ariyanti, T. D., & Royanto, L. R. (2017). The effectiveness of social stories and video modeling in improving self-care skills in female adolescents with mild intellectual disabilities during menstrual periods. Advances in Social Science, Education and Humanities Research, 135, 15–16. https://doi.org/10.2991/iciap-17.2018.16
Bandura, A. (1977). Social learning theory. Prentice-Hall.
Bellini, S., & Akullian, J. (2007). A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism spectrum disorders. Exceptional Children, 73(3), 264–287. https://doi.org/10.1177/001440290707300301
Bernard-Opitz, V., Sriram, N., & Nakhoda-Sapuan, S. (2001). Enhancing social problem solving in children with autism and normal children through computer-assisted instruction. Journal of Autism and Developmental Disorders, 31(4), 377–384. https://doi.org/10.1023/A:1010660502130
Bosseler, A., & Massaro, D. W. (2003). Development and evaluation of a computer-animated tutor for vocabulary and language learning in children with autism. Journal of Autism and Developmental Disorders, 33(6), 653–672. https://doi.org/10.1023/B:JADD.0000006002.82367.4f
Boutain, A. R., Sheldon, J. B., & Sherman, J. A. (2020). Evaluation of a telehealth parent training program in teaching self-care skills to children with autism. Journal of Applied Behavior Analysis, 53(3), 1259–1275. https://doi.org/10.1002/jaba.743
Brown, J. A., & Woods, J. J. (2016). Parent-implemented communication intervention. Topics in Early Childhood Special Education, 36(2), 115–124. https://doi.org/10.1177/0271121416628200
Burke, L. M., Kalpakjian, C. Z., Smith, Y. R., & Quint, E. H. (2010). Gynecologic issues of adolescents with down syndrome, autism, and cerebral palsy. Journal of Pediatric and Adolescent Gynecology, 23(1), 11–15. https://doi.org/10.1016/j.jpag.2009.04.005
Buschmann, A., Jooss, B., Rupp, A., Feldhusen, F., Pietz, J., & Philippi, H. (2008). Parent based language intervention for 2-year-old children with specific expressive language delay: A randomized controlled trial. Archives of Disease in Childhood, 94(2), 110–116. https://doi.org/10.1136/adc.2008.141572
Canady, V. A. (2020). APA survey finds spike in treatment demand, telehealth use. Mental Health Weekly, 30(45), 4–5. https://doi.org/10.1002/mhw.32596
Carnett, A., Hansen, S., Tullis, C., & Machalicek, W. (2021). Using behavioral skills training via telehealth to increase teachers use of communication interventions and increase student use of speech-generating devices in a high school functional skills classroom. Journal of Intellectual Disability Research, 65(2), 133–148. https://doi.org/10.1111/jir.12794
Charman, T., Pickles, A., Simonoff, E., Chandler, S., Loucas, T., & Baird, G. (2010). IQ in children with autism spectrum disorders: Data from the special needs and autism project (SNAP). Psychological Medicine, 41(3), 619–627. https://doi.org/10.1017/s0033291710000991
ChinSchwarz, J. (2008). A fast form approach to measuring technology acceptance and other constructs. MIS Quarterly, 32(4), 687. https://doi.org/10.2307/25148867
Cooper, J. O., Heron, T. E., & Heward, W. L. (2006). Applied behavior analysis (2nd edition). Pearson Prentice Hall.
Corbett, B. A., Vandekar, S., Muscatello, R. A., & Tanguturi, Y. (2020). Pubertal timing during early adolescence: Advanced pubertal onset in females with autism spectrum disorder. Autism Research, 13(12), 2202–2215. https://doi.org/10.1002/aur.2406
Cridland, E. K., Jones, S. C., Caputi, P., & Magee, C. A. (2013). Being a girl in a boys’ world: Investigating the experiences of girls with autism spectrum disorders during adolescence. Journal of Autism and Developmental Disorders, 44(6), 1261–1274. https://doi.org/10.1007/s10803-013-1985-6
Darden-Brunson, F., Green, A., & Goldstein, H. (2008). Video-based instruction for children with autism. In J. K. Luiselli, D. C. Russo, W. P. Christian, & S. M. Wilczynski (Eds.), Effective practices forchildren with autism (pp. 241–268). Oxford. https://doi.org/10.1093/med:psych/9780195317046.003.0012
de Bildt, A., Sytema, S., Kraijer, D., Sparrow, S., & Minderaa, R. (2005). Adaptive functioning and behavior problems in relation to level of education in children and adolescents with intellectual disability. Journal of Intellectual Disability Research, 49(9), 672–681. https://doi.org/10.1111/j.1365-2788.2005.00711.x
de Bruin, C. L., Deppeler, J. M., Moore, D. W., & Diamond, N. T. (2013). Public school–based interventions for adolescents and young adults with an autism spectrum disorder. Review of Educational Research, 83(4), 521–550. https://doi.org/10.3102/0034654313498621
Diaz, J., & Cosbey, J. (2018). A systematic review of caregiver-implemented mealtime interventions for children with autism spectrum disorder. OTJR Occupation, Participation and Health, 38(3), 196–207. https://doi.org/10.1177/1539449218765459
Dogan, R. K., King, M. L., Fischetti, A. T., Lake, C. M., Mathews, T. L., & Warzak, W. J. (2017). Parent-implemented behavioral skills training of social skills. Journal of Applied Behavior Analysis, 50(4), 805–818. https://doi.org/10.1002/jaba.411
Drysdale, B., Lee, C. Y. Q., Anderson, A., & Moore, D. W. (2015). Using video modeling incorporating animation to teach toileting to two children with autism spectrum disorder. Journal of Developmental and Physical Disabilities, 27(2), 149–165. https://doi.org/10.1007/s10882-014-9405-1
Elliott, S. N. (1986). Children’s ratings of the acceptability of classroom interventions for misbehavior: Findings and methodological considerations. Journal of School Psychology, 24(1), 23–35. https://doi.org/10.1016/0022-4405(86)90039-7
Elliott, S. N., & Treuting, M. V. B. (1991). The behavior intervention rating scale: Development and validation of a pretreatment acceptability and effectiveness measure. Journal of School Psychology, 29(1), 43–51. https://doi.org/10.1016/0022-4405(91)90014-i
Ellison, K. S., Guidry, J., Picou, P., Adenuga, P., & Davis, T. E. (2021). Telehealth and autism prior to and in the age of COVID-19: A systematic and critical review of the last decade. Clinical Child and Family Psychology Review, 24(3), 599–630. https://doi.org/10.1007/s10567-021-00358-0
Ersoy, G., Tekin-Iftar, E., & Kircaali-Iftar, G. (2009). Effects of antecedent prompt and test procedure on teaching simulated menstrual care skills to females with developmental disabilities. Education and Training in Developmental Disabilities, 44(1), 54–66. Retrieved November 14, 2021, from http://www.jstor.org/stable/24233463
G Yakubova BB Chen 2021 Examining the effects of parent-created and parent-implemented video prompting to teach daily living skills to an adolescent with autism Journal of Autism and Developmental Disorders 1–13 https://doi.org/10.1007/s10803-021-04913-0
Farley, M. A., McMahon, W. M., Fombonne, E., Jenson, W. R., Miller, J., Gardner, M., Block, H., Pingree, C. B., Ritvo, E. R., Ritvo, R. A., & Coon, H. (2009). Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research, 2(2), 109–118. https://doi.org/10.1002/aur.69
Fischer, A. J., Collins, T. A., Dart, E. H., & Radley, K. C. (2019). Technology applications in school psychology consultation, supervision, and training. Routledge.
Geiger, K. B., Carr, J. E., & LeBlanc, L. A. (2010). Function-based treatments for escape-maintained problem behavior: A treatment-selection model for practicing behavior analysts. Behavior Analysis in Practice, 3(1), 22–32. https://doi.org/10.1007/BF03391755
Hamilton, A., Marshal, M. P., & Murray, P. J. (2011). Autism spectrum disorders and menstruation. Journal of Adolescent Health, 49(4), 443–445. https://doi.org/10.1016/j.jadohealth.2011.01.015
Hennegan, J., Dolan, C., Wu, M., Scott, L., & Montgomery, P. (2016). Measuring the prevalence and impact of poor menstrual hygiene management: a quantitative survey of schoolgirls in rural Uganda. Global Health Research, 6(12). https://doi.org/10.1136/bmjopen-2016-012596
Hennegan, J., Winkler, I. T., Bobel, C., Keiser, D., Hampton, J., Larsson, G., Chandra-Mouli, V., Plesons, M., & Mahon, T. (2021). Menstrual health: A definition for policy, practice, and research. Sexual and Reproductive Health Matters, 29(1), 1911618. https://doi.org/10.1080/26410397.2021.1911618
JM Schaefer NR Andzik 2020 Evaluating behavioral skills training as an evidence-based practice when training parents to intervene with their children Behavior Modification 1–24. https://doi.org/10.1177/0145445520923996
Kellems, R. O., Charlton, C., Kversøy, K. S., & Győri, M. (2020). Exploring the use of virtual characters (Avatars), live animation, and augmented reality to teach social skills to individuals with autism. Multimodal Technologies and Interaction, 4(3), 48. https://doi.org/10.3390/mti4030048
Kırbaş, Z. Ö., Kahriman, I., & Kaşko Arıcı, Y. (2022). Training female adolescent students with intellectual disabilities about genital hygiene skills using peer training. International Journal of Developmental Disabilities, 68(3), 332–341. https://doi.org/10.1080/20473869.2020.1774224
Klin, A., Saulnier, C. A., Sparrow, S. S., Cicchetti, D. V., Volkmar, F. R., & Lord, C. (2006). Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders, 37(4), 748–759. https://doi.org/10.1007/s10803-006-0229-4
Klett, L. S., & Turan, Y. (2012). Generalized effects of social stories with task analysis for teaching menstrual care to three young girls with autism. Sexuality and Disability, 30(3), 319–336. https://doi.org/10.1007/s11195-011-9244-2
KS Guidry J Picou P Adenuga P Davis, T. E., 3rd, 2021 Telehealth and autism prior to and in the age of COVID-19: A systematic and critical review of the last decade Clinical Child and Family Psychology Review 24 3 599 630. https://doi.org/10.1007/s10567-021-00358-0
Lee, D. O. (2004). Menstrually related self-injurious behavior in adolescents with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 43(10), 1193–1193. https://doi.org/10.1097/01.chi.0000135624.89971.d1
Little, L. M., Wallisch, A., Pope, E., & Dunn, W. (2018). Acceptability and cost comparison of a telehealth intervention for families of children with autism. Infants & Young Children, 31(4), 275–286. https://doi.org/10.1097/IYC.0000000000000126
McLay, L., Carnett, A., van der Meer, L., & Lang, R. (2015). Using a video modeling-based intervention package to toilet train two children with autism. Journal of Developmental and Physical Disabilities, 27(4), 431–451. https://doi.org/10.1007/s10882-015-9426-4
Mueller, M. M., Piazza, C. C., Moore, J. W., Kelley, M. E., Bethke, S. A., Pruett, A. E., Oberdorff, A. J., & Layer, S. A. (2003). Training parents to implement pediatric feeding protocols. Journal of Applied Behavior Analysis, 36(4), 545–562. https://doi.org/10.1901/jaba.2003.36-545
Nichols, S., & Blakeley-Smith, A. (2009). “I’m not sure we’re ready for this …”: Working with families toward facilitating healthy sexuality for individuals with autism spectrum disorders. Social Work in Mental Health, 8(1), 72–91. https://doi.org/10.1080/15332980902932383
Ore, T. (2021). How effective is the use of telehealth for children with autism spectrum disorders? International Journal of Psychiatry Research, 4(1), 1–4.
Pugliese, C. E., Anthony, L. G., Strang, J. F., Dudley, K., Wallace, G. L., Naiman, D. Q., & Kenworthy, L. (2015). Longitudinal examination of adaptive behavior in autism spectrum disorders: Influence of executive function. Journal of Autism and Developmental Disorders, 46(2), 467–477. https://doi.org/10.1007/s10803-015-2584-5
Richman, G. S., Reiss, M. L., Bauman, K. E., & Bailey, J. S. (1984). Teaching menstrual care to mentally retarded women: Acquisition, generalization, and maintenance. Journal of Applied Behavior Analysis, 17(4), 441–451. https://doi.org/10.1901/jaba.1984.17-441
Rios, D., Schenk, Y. A., Eldridge, R. R., & Peterson, S. M. (2020). The effects of remote behavioral skills training on conducting functional analyses. Journal of Behavioral Education, 29(2), 449–468. https://doi.org/10.1007/s10864-020-09385-3
Roberts, M. Y., & Kaiser, A. P. (2011). The effectiveness of parent-implemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology, 20(3), 180–199. https://doi.org/10.1044/1058-0360(2011/10-0055)
Sarokoff, R. A., & Sturmey, P. (2004). The effects of behavioral skills training on staff implementation of discrete-trial teaching. Journal of Applied Behavior Analysis, 37(4), 535–538. https://doi.org/10.1901/jaba.2004.37-535
Simacek, J., Dimian, A. F., & McComas, J. J. (2017). Communication intervention for young children with severe neurodevelopmental disabilities via telehealth. Journal of Autism and Developmental Disorders, 47(3), 744–767. https://doi.org/10.1007/s10803-016-3006-z
Kanne, S. M., Gerber, A. J., Quirmbach, L. M., Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2010). The role of adaptive behavior in autism spectrum disorders: Implications for functional outcome. Journal of Autism and Developmental Disorders, 41(8), 1007–1018. https://doi.org/10.1007/s10803-010-1126-4
Simacek, J., Elmquist, M., Dimian, A. F., & Reichle, J. (2020). Current trends in telehealth applications to deliver social communication interventions for young children with or at risk for autism spectrum disorder. Current Developmental Disorders Reports, 8(1), 15–23. https://doi.org/10.1007/s40474-020-00214-w
Steward, R., Crane, L., Mairi Roy, E., Remington, A., & Pellicano, E. (2018). “Life is much more difficult to manage during periods”: Autistic experiences of menstruation. Journal of Autism and Developmental Disorders, 48(12), 4287–4292. https://doi.org/10.1007/s10803-018-3664-0
Sutherland, R., Trembath, D., Hodge, M. A., Rose, V., & Roberts, J. (2019). Telehealth and autism: Are telehealth language assessments reliable and feasible for children with autism? International Journal of Language & Communication Disorders, 54(2), 281–291. https://doi.org/10.1111/1460-6984.12440
Tomlinson, S. R. L., Gore, N., & McGill, P. (2018). Training individuals to implement applied behavior analytic procedures via telehealth: A systematic review of the literature. Journal of Behavioral Education, 27(2), 172–222. https://doi.org/10.1007/s10864-018-9292-0
Torondel, B. Sinha, S. Mohanty, JR. Swain, T. Sahoo, P. Panda, B. Nayak, A. Bara, M. Bilung, B. Cumming, O. Panigrahi, P. Das, P. 2018 Association between unhygienic menstrual management practices and prevalence of lower reproductive tract infections: A hospital-based cross-sectional study in Odisha, India. BMC Infectious Diseases 18(1). https://doi.org/10.1186/s12879-018-3384-2
Tsami, L., Lerman, D., & Toper-Korkmaz, O. (2019). Effectiveness and acceptability of parent training via telehealth among families around the world. Journal of Applied Behavior Analysis, 52(4), 1113–1129. https://doi.org/10.1002/jaba.645
Turco, T. L., & Elliott, S. N. (1986). Assessment of students’ acceptability ratings of teacher-initiated interventions for classroom misbehavior. Journal of School Psychology, 24(3), 277–283. https://doi.org/10.1177/073428298600400404
VandenBos, G. R., & Williams, S. (2000). The internet versus the telephone: What is telehealth anyway? Professional Psychology: Research and Practice, 31(5), 490–492. https://doi.org/10.1037/0735-7028.31.5.490
Veazey, S. E., Valentino, A. L., Low, A. I., McElroy, A. R., & LeBlanc, L. A. (2016). Teaching feminine hygiene skills to young females with autism spectrum disorder and intellectual disability. Behavior Analysis in Practice, 9(2), 184–189. https://doi.org/10.1007/s40617-015-0065-0
What Works Clearinghouse. (2020). What works clearinghouse standards handbook, Version 4.1. U.S. Department of education, institute of education sciences, national center for education evaluation and regional assistance. Retrieved November 14, 2021, from https://ies.ed.gov/ncee/wwc/handbooks
White, S. W., Stoppelbein, L., Scott, H., & Spain, D. (2021). It took a pandemic: Perspectives on impact, stress, and telehealth from caregivers of people with autism. Research in Developmental Disabilities, 113, 103938. https://doi.org/10.1016/j.ridd.2021.103938
Witt, J. C., & Elliott, S. N. (1985). Acceptability of classroom intervention strategies. Advances in School Psychology, 4, 251–288.
Wong, C., Odom, S. L., Hume, K. A., Cox, A. W., Fettig, A., Kucharczyk, S., Brock, M. E., Plavnick, J. B., Fleury, V. P., & Schultz, T. R. (2015). Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism and Developmental Disorders, 45(7), 1951–1966. https://doi.org/10.1007/s10803-014-2351-z
Funding
Partial financial support was received from the Autism Council of Utah (ACU) to conduct this research.
Author information
Authors and Affiliations
Contributions
K. L. designed and executed the study, conducted data analyses, and wrote the paper. M. W. assisted in the development of training materials and fidelity forms, conducted IOA for procedural integrity, and collaborated in the writing and editing of the final manuscript. C. I. supervised and supported study planning and execution, and collaborated in the writing and editing of the final manuscript. A. F. supervised and supported study planning and execution, and collaborated in the writing and editing of the final manuscript. M. F. wrote part of the introduction and method section, and assisted in the development of the animated videos and BST instructional videos. R. J. analyzed data and wrote part of the results, and collaborated in the writing and editing of the final manuscript. A. M. analyzed data and wrote part of the results and collaborated in the writing and editing of the final manuscript. S. M. analyzed data and wrote part of the results, and collaborated in the writing and editing of the final manuscript. J. M. wrote part of the introduction and supported data collection. H. H. wrote part of the “2” section.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University of Utah (April 19, 2021).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
All participants provided consent to the submission of their study data to a scientific journal.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct the spelling in the names of the authors in reference section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lundy, K.M., Wenzbauer, M.A., Illapperuma, C.R. et al. Evaluating the Acceptability and Social Validity of a Caregiver-Led Technology-Based Menstrual Hygiene Management Intervention for Youth on the Autism Spectrum. Adv Neurodev Disord 6, 315–330 (2022). https://doi.org/10.1007/s41252-022-00261-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-022-00261-x