Abstract
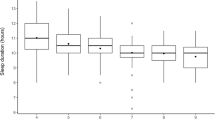
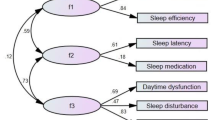
Central hypersomnia (HS) and delayed sleep–wake phase disorder (DSWPD) appear commonly in adolescents, and they severely reduce quality of life and have an enormous impact on academic performance and other aspects of development. Although these disorders are thought to be considerably different in etiology, it is sometimes difficult to distinguish them because of their similar clinical features. This study aimed to compare psychosocial factors and sleep study findings between HS and DSWPD in teenagers. The clinical data of 89 teenagers who visited the psychiatric section of the Sleep Medicine Center of Nihon University Itabashi Hospital from January 2013 to December 2019 were analyzed. Psychosocial factors were evaluated at the first visit, and polysomnography (PSG) and the multiple sleep latency test (MSLT) were performed for patients deemed to require definitive diagnosis. Compared with patients with HS, those with DSWPD had a higher rate of mother’s employment, introversion, adjustment problems, events that triggered the disorder, concurrent mental disorders, habitual lateness, and difficulty attending school or work. PSG did not show any differences in sleep parameters between the two disorders, except for sleep latency. On the MSLT, sleep latency was shorter in those with HS on the second, third, and fourth tests. The present results suggest that focusing on psychosocial factors could be useful for differential diagnosis of the two disorders that appear commonly in adolescents.

Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Scammell TE. Narcolepsy. N Engl J Med. 2015;373:2654–62.
Trotti LM. Idiopathic hypersomnia. Sleep Med Clin. 2017;12:331–44.
Nesbitt AD. Delayed sleep–wake phase disorder. J Thorac Dis Suppl. 2018;10:S103–11.
Kansagra S. Sleep disorders in adolescents. Pediatr Suppl. 2020;145:2019–56.
Inocente CO, Gustin MP, Lavault S, Guignard Perret A, et al. Quality of life in children with narcolepsy. CNS Neurosci Ther. 2014;20:763–71.
Jennum P, Knundsen S, Kjellberg J. The economic consequences of narcolepsy. J Clin Sleep Med. 2009;5:240–5.
Flores NM, Villa KF, Black J, Chervin RD, et al. The humanistic and economic burden of narcolepsy. J Clin Sleep Med. 2016;12:401–7.
Longstreth WT Jr, Koepsell TD, Ton TG, Hendrickson AF, et al. The epidemiology of narcolepsy. Sleep. 2007;30:13–26.
Billiard M, Sonka K. Idiopathic hypersomnia. Sleep Med Rev. 2016;29:23–33.
Pizza F, Moghadam KK, Vandi S, Detto S, et al. Daytime continuous polysomnography predicts MSLT results in hypersomnias of central origin. J Sleep Res. 2013;22:32–40.
Khan Z, Trotti LM. Central disorders of hypersomnolence focus on the narcolepsies and idiopathic hypersomnia. Chest. 2015;148:262–73.
Okawa M, Uchiyama M, Ozaki S, Shibui K, et al. Circadian rhythm sleep disorders in adolescents. Psychiatry Clin Neurosci. 1998;52:483–90.
Wilhelmsen-Langeland A, Saxvig IW, Johnsen EH, Marszalek MA, Wiig Andersen MI, Sætre VK, et al. Patients with delayed sleep-wake phase disorder show poorer executive functions compared to good sleepers. Sleep Med. 2019;54:244–9.
Sivertsen B, Glozier N, Harvey AG, Hysing M. Academic performance in adolescents with delayed sleep phase. Sleep Med. 2015;16:1084–90.
Schrader H, Bovim G, Sand T. The prevalence of delayed and advanced sleep phase syndromes. J Sleep Res. 1993;2:51–5.
Millman RP. Excessive sleepiness in adolescents and young adults: causes, consequences, and treatment strategies. Pediatrics. 2005;115:1774–86.
Frauscher B, Ehrmann L, Mitterling T, Gabelia D, et al. Delayed diagnosis, range of severity, and multiple sleep comorbidities: a clinical and polysomnographic analysis of 100 patients of the Innsbruck Narcolepsy Cohort. J Clin Sleep Med. 2013;9:805–12.
Liblau SR, Vassalli A, Seifinejad A, Tafti M. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 2015;14:318–28.
Micic G, Lovato N, Gradisar M, Lack LC. Personality differences in patients with delayed sleep-wake phase disorder and non-24-h sleep-wake rhythm disorder relative to healthy sleepers. Sleep Med. 2017;30:128–35.
Shirayama M, Shirayama Y, Iida H, Kato M, et al. The psychological aspects of patients with delayed sleep phase syndrome (DSPS). Sleep Med. 2003;4:427–33.
Phillips AJK, Clerx WM, O’Brien CS, Sano A, Barger LK, Picard RW, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-03171-4.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien: American Academy of Sleep Medicine; 2014.
Berry RB, Albertario CL, Harding SM, Lloyd RM, for the American Academy of Sleep Medicine, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Version 2.5. Darien: American Academy of Sleep Medicine; 2018.
Komada Y, Inoue Y, Hayashida K, Nakajima T, et al. Clinical significance and correlates of behaviorally induced insufficient sleep syndrome. Sleep Med. 2008;9:851–6.
Wakastuki Y, Kubo T, Shibata S. Constant light housing during nursing causes human DSPS (delayed sleep phase syndrome) behaviour in Clock-mutant mice. Eurosci. 2007;25:2413–24.
A study by the Cabinet Office of Japan: Comprehensive research survey of cause delinquency 4th edition May 2010 assistant in policy of director general for policies on cohesive society:74–7.
Lee MJ, Lee SY, Yuan SS, Yang CJ, et al. Comorbidity of narcolepsy and depressive disorders: a nationwide population-based study in Taiwan. Sleep Med. 2017;39:95–100.
Zamarian L, Hogl B, Delazer M, Hingerl K, et al. Subjective deficits of attention, cognition and depression in patients with narcolepsy. Sleep Med. 2015;16:45–51.
Kamiyama Y. Polysomnography and contextual factors characteristics with hypersomnia and circadian rhythm sleep-wake disorders in teenagers. Dissertation, Nihon University. 2021.
Acknowledgements
This article is a part of Yayumi Kamiyama's dissertation, which has been submitted to the university’s institutional repository [29].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kamiyama, Y., Kaneko, Y., Saitoh, K. et al. Differences in psychosocial factors and sleep study findings between delayed sleep–wake phase disorder and hypersomnia in teenagers. Sleep Biol. Rhythms 21, 241–247 (2023). https://doi.org/10.1007/s41105-022-00441-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-022-00441-1