Abstract
Introduction
Clinical remission is a relatively new concept in asthma but recent research initiatives suggest it could be an ambitious and achievable therapeutic target for patients with asthma.
Methods
In this modified Delphi study (comprising two online surveys, completed either side of a virtual scientific workshop), the opinions of a panel of respiratory physicians were evaluated to summarize perspective statements on key therapeutic outcomes and criteria for on-treatment clinical remission in patients with moderate asthma. An agreement threshold was pre-defined as agreement by ≥ 75% of participants.
Results
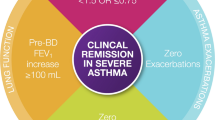
Surveys 1 and 2 were completed by 20 and 18 participants, respectively. Most participants (95%) agreed with the concept of clinical remission in moderate asthma and that this should be a desirable treatment goal (90%). Based on a composite measure of 4–6 desirable therapeutic outcomes, current understanding of clinical remission was considered as 12 months with no exacerbations, no oral corticosteroids, no daytime or night-time asthma symptoms (Asthma Control Test score ≥ 20 or Asthma Control Questionnaire score ≤ 0.75), stable lung function, and no treatment-related adverse events. No agreement was reached on the role of relievers in defining therapeutic outcomes or on the wider use of biomarkers and airway hyperresponsiveness for defining asthma remission in clinical practice.
Conclusions
In line with recent consensus statements from the United States and Europe, there was a high level of agreement on the elements of clinical remission among a panel of respiratory physicians from Asia, the Middle East, and South America. Extension of the concept of clinical remission to patients with moderate asthma was considered aligned with the potential of clinical remission as a goal of therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Clinical remission on treatment is a new concept in asthma that aims to meet a higher standard than the current goal of asthma control. |
Recent research in patients with either severe asthma who are treated with biologics or in those with moderate-to-severe asthma who are treated with inhaled therapy alone, suggests clinical remission could be an ambitious and achievable goal of therapy. |
Using a modified eDelphi procedure, this study aimed to identify the current understanding of clinical remission and how it may apply to patients with moderate asthma, not treated with biologics. |
What was learned from the study? |
There was a high level of agreement on the current concept of asthma remission and its potential as a future goal of therapy in patients with moderate asthma. |
In this group of physicians, current understanding of clinical remission was 12 months with no exacerbations, no oral corticosteroids, no daytime or night-time asthma symptoms (Asthma Control Test score≥20 or Asthma Control Questionnaire score ≤0.75), stable lung function, and no treatment-related adverse events. |
•Patients with moderate asthma on regular controller medication should achieve desirable therapeutic outcomes to target a goal of clinical remission. |
Further research is required to evaluate clinical remission as a goal of therapy. |
Introduction
Treatment-induced remission is a well-defined therapeutic target in some chronic inflammatory disorders such as rheumatoid arthritis (RA) [1,2,3], ulcerative colitis [4], and systemic lupus erythematosus [5], but is a relatively new concept in asthma and it is not yet a target of therapy. The current goals of asthma treatment are to achieve prolonged asthma control and to minimize future asthma-related risks and side effects of treatment [6]. Randomized controlled trials demonstrate that regular treatment with inhaled corticosteroid (ICS)-containing therapies can achieve guideline-defined asthma control and reduce asthma exacerbations [7, 8]. In the real world, however, guidelines are not always fully implemented in clinical practice, even when physicians agree that regular ICS-containing treatments are the most appropriate maintenance treatment for patients with asthma [9, 10]. In addition, patient adherence to asthma medications is frequently low, putting them at increased risk of asthma exacerbations and poor asthma control [11].
Research in patients with severe asthma treated with biologics has suggested that clinical remission could be a plausible and achievable future therapeutic target in severe asthma cases [12,13,14,15,16]. A recent post hoc analysis of the CAPTAIN trial demonstrated that clinical remission could also be achieved in patients with moderate-to-severe asthma treated with inhaled therapy alone, i.e., which is not yet considered for biologics [17]. In this analysis, clinical remission while on treatment was defined as no severe exacerbations, no systemic corticosteroids use, controlled asthma symptoms (Asthma Control Questionnaire (ACQ)-5 score ≤ 1.5) and change from baseline in trough forced expiratory volume in 1 s (FEV1) ≥ 100 ml [17]. These criteria for clinical remission generally aligned with the previous definitions developed using expert opinion and medical literature review [16, 18]. A recent expert working group definition of clinical remission representing American professional respiratory bodies included additional factors such as no missed work or school due to asthma-related symptoms, continued controller therapy (ICS, ICS/long-acting beta agonist (LABA), leukotriene receptor antagonist) only at low-to-medium doses of ICS, and one-time reliever use for no more than once a month [19].
Moderate asthma is defined as asthma that is well controlled with low or medium doses of ICS/LABA [6]. This study aimed to identify the current understanding of desirable therapeutic outcomes and criteria for on-treatment clinical remission in patients with moderate asthma among a panel of respiratory physicians in Latin America, the Middle East, and Southeast Asia. The results will help inform future research evaluating clinical remission as a goal of therapy.
Methods
Study Design
This study used a modified Delphi procedure to elicit views on clinical remission criteria in patients treated for moderate asthma. The study comprised two online surveys and an online scientific workshop, conducted between April and October 2023 (Supplementary Materials, Figure S1).
The survey questionnaires were developed by a research team comprising industry sponsor authors (BA, GL, AP) and an external respiratory expert with a research background in clinical remission in asthma (author PGG). These authors did not contribute to the survey responses. An independent Vendor administered the virtual surveys with Decipher software (version Compact = 153) and performed the data analysis. All survey results gathered from participants were kept anonymous and confidential. The research strictly followed the UK Data Protection Law (GDPR), the British Healthcare Business Intelligence Association’s (BHBIA) Legal & Ethical Guidelines, and the European Pharmaceutical Market Research Association’s (EphMRA) code of conduct [20, 21]. No formal ethical approval was required for this study, as it was a non-interventional physician survey that fell outside the remit of the governance arrangements for research ethics committees [20].
Participants
Twenty-five respiratory physicians from seven countries representing different healthcare systems across Latin America, the Middle East, and Southeast Asia (Argentina, Arabian Gulf, India, Mexico, Philippines, Thailand, and Vietnam) were invited to participate. Participants were invited to participate based on their expert knowledge of asthma and fulfilled at least three of the following criteria: (a) key opinion leaders with at least 10 years of experience in managing patients with asthma, (b) research interest in asthma especially clinically remission, (c) multiple publications in asthma, (d) involved in diverse scientific activities related to asthma in national and/or international congresses, (e) membership in a respiratory society, (f) member of an international or national asthma guideline committee, (g) interested in improving the care and outcomes of patients with asthma. All participants provided their informed consent for each survey and were aware of the objectives of the study prior to participation in the surveys. Participants were also aware of the intention to publish the results of the study. Based on previous studies in the respiratory field [22,23,24,25], a panel of 25 experts was deemed sufficient to elicit meaningful agreements.
Delphi Procedure
The Delphi technique uses structured questionnaires to elicit the views of an expert panel. The major characteristics of this method are anonymity, controlled feedback, and group responses [25, 26]. Participants completed the questionnaires independently and did not know the specific answers given by other participants. Anonymized group responses were shared between the two rounds of questionnaires.
Development of the Delphi Surveys
Questions for the first survey were developed following a literature review using the search terms “moderate”, “asthma”, “therapeutic outcomes”, “clinical remission”, and “complete remission”. This survey included 101 questions (81 close-ended and 20 open-ended questions), covering three main themes in relation to moderate asthma: desirable therapeutic outcomes (in terms of treatment goals), the definition of clinical remission, and the potential future goals beyond clinical remission (termed complete remission in the survey questionnaire) (see Supplementary Materials, Appendix 1).
The second survey questionnaire comprised questions that did not reach agreement during survey 1 and that had been discussed/modified following the scientific meeting. This survey consisted of 39 close-ended questions followed by three open-ended questions (Supplementary Materials, Appendix 2).
Execution of Delphi Surveys and Scientific Workshop
The first survey was sent out in April 2023 and was completed before the scientific workshop. All participants in the first online Delphi survey were invited to a virtual scientific workshop for presentations and discussions about the results, including being asked to share their opinions where agreement had not been met. The meeting was arranged and facilitated by the sponsor and moderated by an external expert (PGG). The second survey was sent out following the scientific workshop. All participants in the second survey had received feedback of anonymized group responses prior to receiving survey 2, following the standard practice of a Delphi process [25, 26]. Following completion of both surveys, the responses were collected and checked for data consistency and anomalies.
Rating of Survey Responses
A 0-to-9-point Likert scale was used to phrase questions and rate the responses. Participants rated their level of agreement with each statement, ranging from 0 (completely disagree) to 9 (completely agree). These scores were categorized into three groups: agree (7–9 points), neither agree nor disagree (4–6 points) and disagree (0–3 points).
Data Analysis
Response data from completed questionnaires were considered for descriptive analysis. Data were presented as the mean, standard deviation (SD), median, and range. For each question, an agreement threshold was pre-defined as at least 75% of participants who answered within the agreement range (7–9 points), in line with previous Delphi studies [27,28,29]. Open-ended questions were summarized descriptively and listed together.
Results
Participants
Twenty-five respiratory physicians were invited to participate in this study and 20 completed the first survey (response rate 80%) (Supplementary Materials, Figure S1, Table S1). All participants were invited to the scientific workshop and ten attended; the remainder were unable to participate due to conflicting appointments and/or time zones. The scientific workshop was non-compulsory; however, all participants received the follow-up minutes from these discussions prior to completion of survey 2. Eighteen participants completed the post-workshop second survey (Table S1). Participants had been working in the respiratory field for an average of 23 years (range, 3–47 years).
Delphi Survey 1
Desirable Therapeutic Outcomes
When participants were asked their opinions on the importance of specific individual desirable outcomes, most (≥ 80%) agreed that for patients with moderate asthma these would include, having no moderate/severe exacerbations, no requirement for oral corticosteroids (OCS), achieving asthma control (measured by Asthma Control Test (ACT) or ACQ), having stable lung function over 1 year, no treatment-related adverse effects requiring a treatment change, and demonstrating no on-treatment bronchodilator reversibility (Fig. 1a). No agreement was reached on the cut-off for rescue medication use (rescue inhaler ≤ 2 days and ≤ 4 occasions per week) (65%), quality of life measures (70%) or measures of airway hyperresponsiveness (AHR) (70%) and airway inflammation (based on availability of fractional exhaled nitric oxide (FeNO) assessment) (65–70%) in defining desirable outcomes (Fig. 1a). Although participants did agree that many months or even years of continued treatment is required to ensure improvement of underlying AHR (90% agreed) (Supplementary Materials, Figure S2a), and that normalizing AHR may be important for exacerbation prevention and long-term outcomes, no agreement was reached on the importance of measuring AHR in patients with either mild or moderate asthma in a clinical practice setting (Supplementary Materials, Figure S3a). Participants did agree that desirable outcomes should be considered as being achieved without changing treatment and after a sufficiently long period (85%), which most physicians thought should be at least 6–12 months (Supplementary Materials, Figure S4).
All participants agreed that patients with moderate asthma should be managed with regular controller treatment and most agreed that therapeutic outcomes should be measured using a composite measure (90%) (Supplementary Materials, Figure S5a). Participants also agreed that therapy should continue until this measure is achieved (85%). When asked how many individual measures should be included in a composite outcomes measure, the most commonly chosen category was between 4 and 6. The top three individual outcomes, considered the most important components of a composite measure were, having no exacerbations, achieving asthma control (measured by asthma control tool), and no use of OCS (Supplementary Materials, Figure S6).
The panel did not reach an agreement when asked if the step 3/4 Global Initiative for Asthma [GINA] recommendations on outcomes for moderate asthma are supported by scientific consensus (50%) (Supplementary Materials, Figure S5a). There was also no agreement on whether desirable therapeutic outcomes are achievable with a symptom-driven treatment approach (45%) (Supplementary Materials, Figure S5a), or if the concept of desirable outcomes applies only to patients who are adherent to treatment (70%) (Supplementary Materials, Figure S2a). While all participants agreed that continuing regular controller treatment is required even when clinical goals have been normalized, 80% also agreed that patients who achieved desirable therapeutic outcomes should be assessed for having their treatment de-escalated without losing any desirable therapeutic outcomes (Supplementary Materials, Figure S2a).
Clinical Remission (on Treatment) in Moderate Asthma
The majority of participants (95%) agreed with the concept of clinical remission in moderate asthma and that a definition of clinical remission should be stringent (80%) and validated (100%) (Fig. 2). They also agreed that clinical remission in moderate asthma, based on objective measures, should be a desirable treatment goal (90%), and 80% thought this should be based on at least 12 months of treatment. Nearly all the participants (95%) understood that clinical remission of patients with asthma on treatment would not mean a cure.
Participants reached agreement on the following outcomes being considered in a definition of clinical remission: no daytime or night-time asthma symptoms (ACT ≥ 20 or ACQ ≤ 0.75), no exacerbations, no OCS, and no treatment-related adverse events requiring a change in therapy (Fig. 3a and Supplementary Materials, Figure S7). Although 90% of physicians agreed that no reliever use could be considered in a definition of clinical remission (Fig. 3a), some practical limitations in relation to identifying acceptable amounts of use were highlighted in the workshop. The participants did not agree that having normal lung function (FEV1) or reduced levels of inflammatory biomarkers should be considered as criteria for clinical remission (Fig. 3a and Supplementary Materials, Figure S7).
Outcomes that could be included in a definition of clinical remission on treatment in a) Survey 1 and b) Survey 2. BEC blood eosinophil count, FeNO fractional exhaled nitric oxide, FEV1 forced expiratory volume in 1 s, FEV1p FEV1 percent of predicted, ICS inhaled corticosteroids, PEF peak expiratory flow
Approximately half of the participants in survey 1 thought that the individual components of clinical remission could be implemented in primary care practice, providing that physicians understood and used the relevant clinical parameters, with the remainder of participants less sure about its applicability in primary care. Most participants (90%) believed in the need to evaluate data from previous or planned clinical studies to better understand clinical remission as an endpoint.
Biological Confirmation
There was agreement among participants (75% agreed) that a future goal of asthma treatment beyond clinical remission may include the criteria for clinical remission plus the absence of airway inflammation, and that this should be based on at least 12 months of measures on treatment (90%) (Supplementary Materials, Figure S8a). Although there was agreement among participants that the criteria for clinical remission plus the measurement of FeNO may meet this definition (75%) (Supplementary Materials, Figure S9a), no agreement was reached on which objective anti-inflammatory measures would be suitable measures in moderate asthma in terms of AHR (45%), blood eosinophils (35%), or FeNO cut-offs (≤ 40 ppb or ≤ 25 ppb) (65%) (Fig. 4a).
When considering the criteria for a goal beyond clinical remission, participants did not agree that healthcare provider and patient concurrence should be considered to meet these criteria (70%), or that achieving this goal would eliminate the risk of severe and even fatal asthma events (60%) (Supplementary Materials, Figure S8a).
Scientific Workshop
Ten participants were able to attend the scientific workshop (Table S1). These participants represented countries in all participating regions. At the meeting, the participants were given some background on previous research in clinical remission in asthma, including studies evaluating remission with biologics in severe asthma. In addition, the results of survey 1 were presented. Among participants, it was considered that demonstrating stable lung function was more appropriate than normal lung function, and that a medical history of sub-optimal lung function should not preclude a patient from meeting the criteria for remission if their lung function is stable. There was also agreement that some objective measure of inflammation (FeNO, AHR, blood eosinophil count) could be an important outcome in patients with moderate asthma, but this would be limited by their availability in primary care clinical practice. Although survey 1 responses suggested that reliever use should be limited, it was acknowledged at the workshop that setting limits for reliever use would be challenging in clinical practice.
Important points identified as worthy of future consideration or research were: what the term remission would mean for patients and physicians and how this could be more widely applied, and the concept of clinical remission in mild asthma.
Delphi Survey 2
Following the scientific workshop and completion of survey 2, some additional agreement statements to those agreed after survey 1 were reached. The majority of participants now agreed that a good quality of life (94%) and no time missed at work or school due to asthma (78%) should be considered desirable therapeutic outcomes, but there was still no agreement on the cut-off for rescue medication use (Fig. 1b).
The panel agreed (89%) that stable lung function would be the most appropriate lung function measurement in defining clinical remission (Fig. 3b). There was also agreement that the measurement of FeNO to indicate controlled airway inflammation could be a desirable therapeutic outcome and a useful indicator of clinical remission, if this test was available in clinical practice (Figs. 1b, 3b). Although 78% of participants considered that a reduction in blood eosinophil count could be a biological confirmation of clinical remission (Supplementary Materials Figure S9b), there was discord about the practicalities of assessing inflammatory measures in clinical practice (Fig. 4b, Supplementary Materials, Figure S3b).
In survey 2, 78% of participants agreed that there is still no scientific consensus to support desirable therapeutic outcomes in moderate asthma (in steps 3 and 4 of the GINA recommendations) (Supplementary Materials, Figure S5b). The majority (83%) also agreed that a symptom-driven approach (without regular controller treatment) is insufficient to achieve composite therapeutic outcomes in patients with moderate-to-severe asthma (Supplementary Materials, Figure S5b). The panel also agreed that the concept of desirable outcomes in terms of treatment goals should apply only to patients who are adherent to treatment (89%), and that any definition should include the risk of future relapses (exacerbation or an ACT score of ≤ 20) in patients who have achieved therapeutic goals (Supplementary Materials, Figure S2b).
There was agreement among participants that healthcare provider and patient concordance should be required when considering a goal of treatment beyond clinical remission (78%) (Supplementary Materials, Figure S8b). Eighty-three percent of participants also agreed that being in clinical remission would not eliminate the risk of severe and even fatal asthma events (Supplementary Materials, Figure S8b).
Summary
At the end of the Delphi process, the top 4 (‘major’) desirable outcomes that participants currently agree are both desirable outcomes and a criterion for clinical remission were no exacerbations, no OCS, no symptoms (ACT ≥ 20 or ACQ ≤ 0.75) and stable lung function (Figs. 1, 3, Supplementary Materials, Figure S6). Participants also agreed that having no adverse events requiring a change in treatment was a desirable outcome (95%) and may be considered a criterion for clinical remission (90%) although this was not rated as one of the most important desirable outcomes (Supplementary Materials, Figure S6). Participant responses and discussions around reliever use suggested that reliever use should be limited but no agreement was reached on acceptable amounts of use. A summary of overall results from this Delphi study is shown in Fig. 5.
Understanding and agreement of criteria for desirable outcomes, clinical remission, and biological confirmation of remission (on treatment)a. aReliever use ≤ 2 days ≤ 4 occasions per week was one of the top 4 criteria for desirable therapeutic outcomes (Figure S6) but did not achieve pre-defined agreement threshold (Fig. 1). ACQ Asthma Control Questionnaire, ACT Asthma Control Test, FeNO fractional exhaled nitric oxide, FEV1 forced expiratory volume in 1 s, QOL quality of life, OCS oral corticosteroids
Discussion
This study demonstrated a high level of agreement on the concept of clinical remission and the potential for its future development as a goal of treatment in patients with moderate asthma. The view of this panel was that a definition of clinical remission based on desirable therapeutic outcomes would comprise 12 months with no exacerbations, no OCS, no daytime or night-time asthma symptoms (assessed using ACT or ACQ), stable lung function, and no treatment-related adverse events requiring a change in treatment. The panel view was also that biological confirmation of asthma remission would comprise the criteria for clinical remission plus the absence of airway inflammation confirmed by an objective measure of FeNO. The main area of non-agreement in this process centered around the measurement of markers of airway inflammation, mainly related to the practical issues of measuring them in primary care clinical practice. Most participants agreed that further research aimed at evaluating clinical remission as a goal of therapy would be an important step in corroborating a definition of clinical remission in moderate asthma.
Clinical remission in asthma is a relatively new and emerging concept and several expert groups/respiratory societies/guidelines have proposed definition criteria for clinical remission [12, 16, 18, 19], some of which define clinical remission without categorizing for which severity group they apply [16, 19]. In common with our Delphi findings, all previous definitions have specified an absence of asthma symptoms (measured by a validated tool), no exacerbations, and no OCS use. These are consistent with current treatment guidelines which have been developed around concepts of controlling symptoms and mitigating future risks [6, 30, 31]. Other components considered for clinical remission have not been consistent across articles. For example, Pavord et al. recommended a criterion of clinical remission to be normalized lung function in a severe asthma population treated with biologics [12]. Whereas other articles based on expert opinion proposed an outcome of optimized or stable lung function [16, 18, 19]. The latter definition recognizes that some patients may never attain normal lung function thresholds and achieving stable lung function may be a desirable outcome for these patients. Although participants in this study considered one criterion of on-treatment remission could be reliever use in the past 12 months, there were differing opinions on what would constitute acceptable levels of reliever use and workshop discussions centered on how this would be difficult to measure. This is consistent with other definitions that have not considered or not agreed upon a reliever criterion [12, 16, 18]. Blaiss et al., on the other hand, recommended one-time reliever therapy (inhaled short-acting beta-agonists (SABA), inhaled corticosteroids (ICS)-SABA, ICS-LABA) no more than once a month in their definition of clinical remission [19], highlighting the challenge of including reliever use as an objective measure when defining remission. This reflects discussions in the literature about the role of SABAs as relievers, where some authors have suggested limiting the access to as-needed SABAs [32, 33] while others have provided evidence for the safety and appropriate use of SABA relievers to complement ICS-based maintenance treatments [34, 35]. The participants in this Delphi survey were of the opinion that one criterion for remission would be no treatment-related adverse events requiring a change in treatment which differs from previous definitions [16, 18, 19]. Any change in regular asthma treatment, i.e., initiation of a different/additional controller, indicates a failure of previous therapy and on-treatment remission criteria requires continuous treatment for ≥ 12 months, providing a rationale for this finding.
Only one expert working group has stipulated that no school or work should be missed over the last 12 months as part of their clinical remission criteria [19]. In this study, participants recognized the importance of achieving a good quality of life and no time missed from work or school as desirable therapeutic outcomes, but neither are considered under the current understanding of clinical remission. The impacts of asthma on patients’ daily activities and health-related quality of life are important to patients but may be a secondary consideration for physicians compared with managing asthma control and future risks [36].
A change in focus towards goals of remission would need to be accommodated in management guidelines and involve retraining physicians to consider these outcomes. To successfully implement clinical remission as a target of therapy, it must be measurable and implementable in clinical practice (including primary care), meaningful for patients, and would ideally be associated with reduced disease progression. The ideal remission framework would encompass the outcomes of clinical remission and include biological confirmation of an altered disease state. A challenge of including biological confirmation of clinical remission in any remission framework is the assessment of objective inflammatory measures, and this topic was the subject of some debate among the Delphi panel. After the second survey, although the panel agreed that a FeNO threshold could be considered if it was available in clinical practice, it is not widely available or routinely measured in current clinical practice. Therefore, this measure is not one that could be currently included in a definition of clinical remission, consistent with other expert groups [12, 16–19]. Alignment between previous definitions of well- or totally controlled asthma, guideline recommendations and expert opinion papers for desirable therapeutic outcomes and clinical remission will be needed. The extent of this challenge was recently highlighted by an expert Delphi panel that concluded there is, as yet, not even a standard and universally accepted definition of asthma control, having identified 19 different composite consensus/guideline definitions and/or validated measures of control [37].
The participants in this survey agreed that there is still no scientific consensus to support desirable therapeutic outcomes for clinical remission in moderate asthma (as per step 3/4 GINA recommendations [6]), possibly supporting the idea of a different approach to achieve desirable outcomes across all severities of asthma. To aspire to a goal of clinical remission in all patients with asthma may require earlier, regular long-term intervention with controller therapy to address early underlying airway inflammation and remodeling, even in patients with mild asthma [38]. A recent workgroup definition of clinical remission in asthma allows for continued use of ICS-containing controller treatment (at low-to-medium doses of ICS or less) in order to differentiate remission criteria from just achieving control [19]. Lommatzsch et al. recently proposed that by adopting the model used in RA, an overarching term of disease-modifying anti-asthmatic drugs for all ICS-containing inhalation schemes, biologics, and allergen immunotherapy strategies could be used in conjunction with defining asthma remission as a target of therapy [39]. This is supported by a proportion of patients with either severe asthma [16] or moderate-to-severe asthma [17], achieving clinical remission while receiving medium and high doses of ICS/ICS-containing treatments.
Strengths and Limitations
The Delphi technique used in this study had several strengths; namely, the research problem was clearly identified, the respiratory specialists had knowledge and specific interest in the topic of research, and an independent specialist team oversaw the Delphi process. A limitation of this study is that all participants were respiratory specialists and the findings may not represent the views of physicians generally or primary care physicians specifically who are responsible for managing many patients with moderate asthma. As such, the views represented may not be reproducible by a different panel of experts. However, participants represented variable healthcare systems in Latin America, the Middle East, and Southeast Asia, and their responses were not homogenous, suggesting a wide range of views were represented. Another limitation is that we focused on moderate asthma and did not consider mild asthma in this survey. This would be a topic of future research.
Conclusions
The physicians from Asia, the Middle East, and South America who participated in this study reached a high level of agreement on the current understanding of clinical remission in patients with moderate asthma and agreed that any future changes to the definition must be stringent, validated, and should be achievable in primary care clinical practice.
Data Availability
Information on GlaxoSmithKline R&D’s data sharing commitments and requesting access can be found at: https://www.clinicalstudydatarequest.com.
References
NICE guideline. Rheumatoid arthritis in adults: management; 2020. Available at: www.nice.org.uk/guidance/ng100. Last Accessed 2 Nov 2023.
Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2021;73:924–39.
Smolen JS, Landewé RBM, Bergstra SA, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann Rheum Dis. 2023;82(1):3–18.
Vuitton L, Peyrin-Biroulet L, Colombel JF, et al. Defining endoscopic response and remission in ulcerative colitis clinical trials: an international consensus. Aliment Pharmacol Ther. 2017;45:801–13.
van Vollenhoven R, Voskuyl A, Bertsias G, et al. A framework for remission in SLE: consensus findings from a large international task force on definitions of remission in SLE (DORIS). Ann Rheum Dis. 2017;76:554–61.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2023. Available from: https://ginasthma.org/gina-reports/. Accessed 29 Nov 2023.
Bateman ED, Boushey HA, Bousquet J, GOAL Investigators Group, et al. Can guideline-defined asthma control be achieved? The gaining optimal asthma control study. Am J Respir Crit Care Med. 2004;170:836–44.
Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD005533.pub2.
Aggarwal B, Shantakumar S, Hinds D, Mulgirigama A. Asia-Pacific survey of physicians on asthma and allergic rhinitis (ASPAIR): physician beliefs and practices about diagnosis, assessment, and treatment of coexistent disease. J Asthma Allergy. 2018;11:293–307.
Chapman KR, Canonica GW, Lavoie KL, et al. Patients’ and physicians’ perspectives on the burden and management of asthma: results from the APPaRENT 2 study. Respir Med. 2022;201: 106948.
Bårnes CB, Ulrik CS. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir Care. 2015;60:455–68.
Pavord I, Gardiner F, Heaney LG, et al. Remission outcomes in severe eosinophilic asthma with mepolizumab therapy: analysis of the REDES study. Front Immunol. 2023;14:1150162.
Thomas D, McDonald VM, Stevens S, et al. Biologics (mepolizumab and omalizumab) induced remission in severe asthma patients. Allergy. 2024;79:384–92.
Sposato B, Bianchi F, Ricci A, Scalese M. Clinical asthma remission obtained with biologics in real life: Patients’ prevalence and characteristics. J Pers Med. 2023;13:1020.
Lugogo NL, Mohan A, Arbor A, et al. Are we ready for asthma remission as a clinical outcome? Chest. 2023;164:831–4.
Menzies-Gow A, Bafadhel M, Busse WW, et al. An expert consensus framework for asthma remission as a treatment goal. J Allergy Clin Immunol. 2020;145(3):757–65.
Lugogo N, Oppenheimer J, Crawford J, et al. Is asthma clinical remission achievable by inhaled therapy? A post-hoc analysis of single inhaler triple therapy with FF/UMEC/VI in the CAPTAIN trial. J Allergy Clin Immunol. 2024;153(supplement issue 2):AB266.
Canonica GW, Blasi F, Carpagnano GE, et al. Severe Asthma Network Italy definition of clinical remission in severe asthma: a Delphi consensus. J Allergy Clin Immunol Pract. 2023;S2213–2198(23):00816–24.
Blaiss M, Oppenheimer J, Corbett M, et al. Consensus of an American College of Allergy, Asthma, and Immunology, American Academy of Allergy, Asthma, and Immunology, and American Thoracic Society workgroup on definition of clinical remission in asthma on treatment. Ann Allergy Asthma Immunol. 2023;131:782–5.
Association BHBI. BHBIA legal and ethical guidelines for healthcare market research. Hertfordshire, UK: British Healthcare Business Intelligence Association 2024. https://www.bhbia.org.uk/guidelines-and-legislation/legal-and-ethical-guidelines. Accessed 26 April 2024.
European Pharmaceutical Market Research Association’s (EphMRA) code of conduct 2023. https://www.ephmra.org/code-conduct-aer. Accessed 26 April 2024.
Bousquet J, Winchester C, Papi A, et al. Global allergy and asthma European network (GA2LEN). Inhaled corticosteroid/long-acting β2-agonist combination therapy for asthma: attitudes of specialists in Europe. Int Arch Allergy Immunol. 2012;157:303–10.
Harding G, Leidy NK, Meddis D, Kleinman L, Wagner S, O’Brien CD. Interpreting clinical trial results of patient-perceived onset of effect in asthma: methods and results of a Delphi panel. Curr Med Res Opin. 2009;25:1563–71.
Sheikh A, Major P, Holgate ST. Developing consensus on national respiratory research priorities: key findings from the UK respiratory research Collaborative’s e-Delphi exercise. Respir Med. 2008;102:1089–92.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15.
Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE. 2011;6: e20476.
Slade SC, Dionne CE, Underwood M, Buchbinder R. Standardised method for reporting exercise programmes: protocol for a modified Delphi study. BMJ Open. 2014;4: e006682.
Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E. A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes (Lond). 2019;43:2573–86.
Domingo C, Garcia G, Gemicioglu B, et al. Consensus on mild asthma management: results of a modified Delphi study. J Asthma. 2023;60:145–57.
The British Thoracic Society. BTS/SIGN British guideline on the management of asthma, 2019. <https://www.brit-thoracic.org.uk/standards-of-care/guidelines/btssign-british-guideline-on-the-management-of-asthma/>. Accessed 29 Nov 2023.
Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI) administered and coordinated National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC), Cloutier MM, Baptist AP, Blake KV, et al. 2020 Focused updates to the asthma management guidelines: a report from the national asthma education and prevention program coordinating committee expert panel working group. J Allergy Clin Immunol. 2020;146(6):1217–70.
Charriot J, Gaga M, Suehs C, Bourdin A. Asthma rescue treatments, time to reboot. Eur Respir J. 2020;55:2000542.
Volpe FM. Cause or consequence? Eur Respir J. 2022;59(6):2103107.
Amirav I, Garcia G, Le BK, Barria P, Levy G, Aggarwal B, Fahrbach K, Martin A, Phansalkar A, Sriprasart T. SABAs as reliever medications in asthma management: evidence-based science. Adv Ther. 2023;40:2927–43.
Sriprasart T, Waterer G, Garcia G, Rubin A, Andrade MAL, Roguska A, Phansalkar A, Fulmali S, Martin A, Mittal L, Aggarwal B, Levy G. Safety of SABA monotherapy in asthma management: a systematic review and meta-analysis. Adv Ther. 2023;40:133–58.
Juniper EF. Assessing asthma quality of life: its role in clinical practice. Breathe. 2005;1:192–204.
Canonica GW, Spanevello A, de Llano LP, Domingo Ribas C, Blakey JD, Garcia G, Inoue H, Dalcolmo M, Yang D, Mokashi S, Kurne A, Butta AK. Is asthma control more than just an absence of symptoms? An expert consensus statement. Respir Med. 2022;202: 106942.
Ward C, Pais M, Bish R, et al. Airway inflammation, basement membrane thickening and bronchial hyperresponsiveness in asthma. Thorax. 2002;57:309–16.
Lommatzsch M, Brusselle GG, Canonica GW, Jackson DJ, Nair P, Buhl R, Virchow JC. Disease-modifying anti-asthmatic drugs. Lancet. 2022;399:1664–8.
Acknowledgements
The authors thank all participants who completed the surveys and contributed to discussions in the scientific workshop. The authors also thank the team at EVERSANA who administered the questionnaires and performed the data analysis.
Medical writing/Editorial assistance: Editorial support in the form of writing assistance (draft preparation and copyediting) was provided by Kate Hollingworth of Continuous Improvement Ltd, UK, and was funded by GSK.
Funding
This work was supported by GSK. The Rapid Service Fee for publication was funded by GSK.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: Bhumika Aggarwal, Abhay Phansalkar, Gur Levy, Maximilian Plank, Peter Gibson. Data acquisition and/or data interpretation: All authors. Data analyses: Bhumika Aggarwal, Abhay Phansalkar, Gur Levy supported by EVERSANA. All authors contributed to drafting, reviewing, and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Kittipong Maneechotesuwan has received honoraria for lectures, presentations, speakers’ bureaus or educational events from AstraZeneca, Boehringer Ingelheim, GSK, Novartis, and Sanofi. Gabriel Garcia has received speaker and advisory board honoraria from AstraZeneca, GSK, and Sanofi, and support for travel/attending meetings from AstraZeneca and Sanofi. Hugo Neffen has received honoraria for lectures from AstraZeneca and Casasco, for manuscript writing from Elea, and support for travel/attending meetings from AstraZeneca and Casasco. Mona Al-Ahmad has received speaker and advisory board honoraria from AstraZeneca, GSK, and Sanofi, and support for travel/attending meetings from AstraZeneca and Sanofi. Mousa Khadadah has received advisory board and speaker’s fees from AstraZeneca, Boehringer Ingelheim, and GSK, and support for travel/attending a conference from MundiPharma. Vu Tran Thien Quan has received honoraria for lectures, presentations, speakers’ bureaus from AstraZeneca, Boehringer Ingelheim, DKSH, and GSK. Krittika Teerapuncharoen has received lectures/speakers honoraria from AstraZeneca, Boehringer Ingelheim, and GSK, and support for travel/attending meetings from Boehringer Ingelheim. Mario Soto Ramos has received honoraria from GSK for speaking in educational events. Peter Gibson has received funding for education lectures from AstraZeneca, GSK, and Novartis, and his institution has received grants from AstraZeneca and GSK, all unrelated to the current paper. Bhumika Aggarwal, Gur Levy, Maximilian Plank, and Abhay Phansalkar are GSK employees and hold GSK shares. Daniel Tan and Ramon Javier have no competing interests to declare.
Ethical Approval
The research strictly followed the UK Data Protection Law (GDPR), the British Healthcare Business Intelligence Association’s (BHBIA) Legal & Ethical Guidelines, and the European Pharmaceutical Market Research Association’s (EphMRA) code of conduct. No formal ethical approval was required for this study as it was a non-interventional physician survey that fell outside the remit of the governance arrangements for research ethics committees [20]. All participants provided their informed consent for each survey and were aware of the objectives of the study prior to participation in the surveys. Participants were also aware of the intention to publish the results of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Maneechotesuwan, K., Aggarwal, B., Garcia, G. et al. Exploring Clinical Remission in Moderate Asthma – Perspectives from Asia, the Middle East, and South America. Pulm Ther (2024). https://doi.org/10.1007/s41030-024-00262-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41030-024-00262-2